Abstract
Background and aims
Studies examining predictors of survival among the oldest-old have primarily focused on objective measures, such as physical function and health status. Only a few studies have examined the effect of personality traits on survival, such as optimism. The aim of this study was to examine whether an optimistic outlook predicts survival among the oldest-old.
Methods
The Danish 1905 Cohort Survey is a nationwide, longitudinal survey comprising all individuals born in Denmark in 1905. At baseline in 1998, a total of 2,262 persons aged 92 or 93 agreed to participate in the intake survey. The baseline in-person interview consisted of a comprehensive questionnaire including physical functioning and health, and a question about whether the respondent had an optimistic, neutral or pessimistic outlook on his or her own future.
Results
During the follow-up period of 12 years (1998–2010) there were 2,239 deaths (99 %) in the 1905 Cohort Survey. Univariable analyses revealed that optimistic women and men were at lower risk of death compared to their neutral counterparts [HR 0.82, 95 % CI (0.73–0.93) and 0.81, 95 % CI (0.66–0.99), respectively]. When confounding factors such as baseline physical and cognitive functioning and disease were taken into account the association between optimism and survival weakened in both sexes, but the general pattern persisted. Optimistic women were still at lower risk of death compared to neutral women [HR 0.85, 95 % CI (0.74–0.97)]. The risk of death was also decreased for optimistic men compared to their neutral counterparts, but the effect was non-significant [HR 0.91, 95 % CI (0.73–1.13)].
Conclusion
An optimistic outlook appears to be a significant predictor of survival among the oldest-old women. It may also be a significant predictor for men but the sample size is small.
Keywords: Predictors of mortality, Survival, Optimism, Oldest-old
Introduction
Do optimists live longer than pessimists? Since ancient times, negative emotions have been thought to play an essential role in the etiology of physical disease. Empirically, a number of studies have linked negative psychological states to adverse health outcomes. For example, depression and anxiety are associated with a higher risk of coronary heart disease (CHD), disability, or all cause mortality [1–5]. In recent decades, the interest in “positive psychology”, i.e., the relation between positive psychological well-being and physical health, has increased substantially [6, 7].
To have a positive outlook or to be optimistic may pose an independent health benefit to the individual [8, 9]. A recent review examining the link between optimism and various physical health outcomes such as mortality, survival, pain, cardiovascular and cancer outcomes, and physiological markers (including immune function) indicates that optimism is a significant predictor of positive physical health outcomes [8]. Specifically, prospective epidemiological studies have related optimism to a reduced risk of all cause [10, 11] and cardiovascular mortality [12], CHD [13, 14], and depression [15] in healthy populations. In diseased populations, optimism is associated with a lower level of re-hospitalization following coronary artery bypass grafting [16], better long-term psychological well-being after treatment for early stage breast cancer in women [17], and a better survival in a group of head- and neck cancer patients [18] and self-referred medical patients [19].
Optimism is conceptualized in two rather different ways, as explanatory style optimism [20, 21], and as dispositional optimism [22, 23]. Explanatory style optimism refers to the way an individual explains the causes of uncontrollable bad life events, whereas dispositional optimism refers to the generalized positive expectation that good things rather than bad things will happen in the future. The two different measures of optimism do not seem to correlate strongly with each other [24] and thus may represent different aspects of psychological well-being.
Studies examining predictors of survival among the oldest-old have primarily focused on objective measures, such as socio-demographic variables, physical and cognitive function, and health status [25–27]. In contrast, only few studies have examined personality traits as predictors of survival, such as optimism [8, 10, 12]. In this study we focused on a measure of dispositional optimism. The objective was to test whether optimistic individuals had a survival advantage compared to less optimistic individuals among 2,262 nonagenarians in the Danish 1905 Cohort Survey, controlling for baseline health and function.
Methods
Study population
The Danish 1905 Cohort Survey is a nationwide longitudinal survey comprising all individuals born in Denmark in 1905 identified through the Danish Civil Registration System (CRS). At baseline in 1998 a total of 3600 individuals aged 92–93 were still alive in the cohort, and of these 2,262 agreed to participate in the baseline interview (63 %). A non-response analysis showed no differences with respect to housing, marital status or hospitalization patterns between responders and non-responders. The baseline in-person interview consisted of a comprehensive questionnaire covering socio-demographic variables, health behavior, self-reported diseases, cognitive testing and self-reported activities of daily living (ADL), and a question about whether the respondent had an optimistic, neutral or pessimistic outlook on his or her own future. The question about optimism was previously used in the Cambridge Mental Disorders of the Elderly Examination (CAMDEX) interview schedule [28]. Among the 2,262 participants at baseline, 448 participated via a proxy. Because proxy information was not available for the question about optimism only 1,814 participants (80.2 %) were approached about that particular item. The 1905 Cohort Survey has been described in greater detail by Nybo et al. [29]. The Ethical committee system in Denmark approved the study (trial number VF20040240).
Measures
Predictors of survival during the first 15 months of follow-up have previously been examined in the 1905 Cohort Survey [25]. Results showed that otherwise well-known predictors of death in younger age groups such as socio-demographic factors (educational attainment and marital status) and health behavior (smoking, obesity, and alcohol consumption) did not prove to be significant risk factors for death among the oldest-old. However, a high disability level, poor physical and cognitive performance, and poor self-rated health (only in women) continued to be important predictors of mortality. The variables included in this study as confounders were based on the previous findings by Nybo et al. [25] and on knowledge about covariates of a priori importance for the association under study. Baseline socio-demographic characteristics in the 1905 Cohort Survey are described elsewhere [30].
Dispositional optimism was measured by one question: “How do you feel about your own future?” Answer categories were “optimistic”, “neutral” or “pessimistic”. Respondents who answered “neutral” to this question served as the reference group in the regression analyses.
Disability was assessed using a modified version of the Katz Index of Activities of Daily Living (Katz ADL) [31] that includes basic ADLs such as bathing, dressing, toileting, transferring, continence and feeding. The question about continence was not included in the 1905 Cohort Survey and therefore excluded from the present analysis. The remaining five ADL items were coded as binary variables identifying respondents who were able to perform the particular item independently with or without the use of assistive devices but with no guidance or personal assistance. A disability score was calculated reflecting how many ADL items the respondent was able to perform independently. Respondents were categorized as “Independent” if they could perform all of the five ADL items independently, “Moderately disabled” if they were independent in 3–4 items, and “Severely disabled” if they were independent in 0–2 items.
Cognitive function was measured using the Mini Mental State Examination (MMSE) developed by Folstein et al. [32]. The MMSE assesses different areas of cognitive function: orientation, registration, calculation, recall, and language. The correct scores of each area are summed to a maximum score of 30 points. In the present study, the summary scores were divided into three categories reflecting “No cognitive impairment” (24–30 points), “Mild cognitive impairment” (18–23 points), and “Severe cognitive impairment” (0–17 points) following the conventions established in the Epidemiologic Catchment Area Studies in the USA [33]. Missing information due to non-response or refusal in the MMSE was scored as zero points following the recommendations by Fillenbaum et al. [34].
Self-reported diseases were assessed according to a list of 31 chronic conditions and diseases, and respondents were asked whether they were ever told by a physician that they suffered from any of them. The diseases included in this study were divided into five categories: (1) osteoar-thritis, rheumatoid arthritis, osteoporosis, cataract, and glaucoma, categorized as “Non-fatal chronic disease”; (2) chronic bronchitis and asthma, categorized as “Chronic lung disease”; and (3) stroke, heart attack, angina pectoris, irregular heart rhythm, treatment for hypertension with prescription medicine, other heart problems, heart failure, and insufficient blood circulation in the legs, categorized as “Circulatory disease”. The fourth category was cancer (except for skin cancer) and the fifth category was diabetes. Each disease category was a binary variable identifying respondents who had been diagnosed with at least one of the diseases included in the particular disease category.
Vital statistics data
A total of 3,600 individuals were still alive in the 1905 birth cohort at intake in 1998. Date of death was retrieved for the total cohort through the Danish CRS. By the end of follow-up on 31 December 2009 only 38 (1 %) individuals were still alive in the cohort, and of these 22 participated in the baseline interview. Two persons emigrated since intake but before the end of follow-up, and one of these participated in the baseline survey. Thus, of the 2,262 persons participating in the baseline survey 2,239 persons (99 %) had died during the 12-year follow-up, and one was lost to follow-up due to emigration. For the 22 individuals still alive at follow-up right censoring was done on 31 December 2009, and for the person who emigrated on the day of emigration (12 April 1999). Respondents in the 1905 Cohort Survey were followed up from the day of the baseline interview until death, emigration or end of follow-up on 31 December 2009, whichever occurred first. For three respondents the interview date was missing. Further examination revealed that one was interviewed in March and two in May 1998. Consequently, the missing interview dates were replaced by 15 March 1998, and 15 May 1998, respectively.
Statistical analyses
The Kaplan–Meier method was used to examine crude survival proportions within the groups of optimistic, neutral and pessimistic individuals, and the Log rank test was applied to test if survival distributions differed significantly between groups. Differences between groups on categorical variables were tested using the Pearson Chi Square test. Multivariable Cox regression models were used to derive hazard ratios (HR) and corresponding 95 % confidence intervals (95 % CI) of death according to optimism controlling for relevant confounders. All analyses were stratified by sex to detect any gender differences. To determine the effect of each covariate on survival mortality rates and their corresponding 95 % confidence intervals were computed. The final multivariable Cox regression model included adjustment for cognitive function, ADL, and self-reported diseases, and all variables were treated as categorical. The assumption of proportional hazards was assessed by martingale residuals [35] and was satisfied for optimism in both men and women. Time varying effects of ADL and non-fatal chronic disease for men and of MMSE, ADL and diabetes for women were detected but subsequent correction did not change estimates. Therefore, only the uncorrected results are presented in the following. Potential interaction between optimism and the remaining covariates in the model were tested using the Likelihood Ratio test, and this revealed a weak interaction between optimism and ADL for women: optimism appeared to be less important for survival in women who were independent in ADL, although nonsignificant. Statistical tests of the regression estimates were based on Wald statistics and a p value of <0.05 was considered statistically significant. Robust standard errors were used to derive corresponding 95 % CI for each regression estimate. Analyses were performed using STATA, version 11.1, STATA Corporation [36].
Results
Information about optimism was available for 1,682 respondents in the 1905 Cohort Survey, of these 1,229 were women and 453 were men. A total of 546 (32.5 %) respondents reported themselves as optimistic, 942 (56.0 %) were neutral, and 194 (11.5 %) were pessimistic. Men were more optimistic than women (37.1 % vs. 30.8 %, p = 0.048). Still, men incurred higher mortality rates than their female counterparts (Table 1). The highest prevalence of chronic disease at baseline was found for non-fatal chronic disease (68.3 %) and circulatory disease (58.5 %) and in both disease categories women accounted for the highest proportion. With respect to chronic lung disease, cancer (except for skin cancer) and diabetes the prevalence was much lower in the total study population, 13.1, 7.4 and 7.2 %, respectively. As expected, mortality rates were higher among both pessimistic and diseased respondents (except for those with non-fatal chronic disease), and in those who were cognitively impaired or physically disabled (Table 1).
Table 1.
Mortality rates according to optimism and confounders (The Danish 1905 Cohort Survey)
| Participants (n) | Women |
Men |
Total | ||
|---|---|---|---|---|---|
| 1,678 | 584 | 2,262 | |||
| Variable | n (%) | Mortality rate per 100 person years (95 % CI) |
n (%) | Mortality rate per 100 person years (95 % CI) |
n (%) |
| Optimism | |||||
| Optimistic | 378 (22.5) | 22.3 (20.1–24.7) | 168 (28.8) | 28.4 (24.4–33.0) | 546 (24.1) |
| Neutral | 705 (42.0) | 25.8 (23.9–27.8) | 237 (40.6) | 33.3 (29.3–37.9) | 942 (41.6) |
| Pessimistic | 146 (8.7) | 31.9 (27.1–37.5) | 48 (8.2) | 37.8 (28.5–50.1) | 194 (8.6) |
| Missing | 449 (26.8) | 131 (22.4) | 580 (25.6) | ||
| Activities of daily living† | |||||
| Non-disabled | 518 (30.9) | 20.6 (18.9–22.5) | 252 (43.1) | 26.4 (23.3–29.9) | 770 (34.1) |
| Moderately disabled | 719 (42.8) | 28.5 (26.5–30.6) | 202 (34.6) | 39.4 (34.3–45.2) | 921 (40.7) |
| Severely disabled | 441 (26.3) | 50.9 (46.4–55.9) | 130 (22.3) | 67.4 (56.7–80.1) | 571 (25.2) |
| Missing | Nil | Nil | Nil | ||
| Mini Mental State Examination (MMSE) | |||||
| 24–30 points | 562 (33.5) | 21.8 (20.0–23.7) | 254 (43.5) | 27.4 (24.2–31.0) | 816 (36.1) |
| 18–23 points | 422 (25.2) | 25.6 (23.3–28.2) | 148 (25.3) | 34.5 (29.3–40.5) | 570 (25.2) |
| 0–17 points | 332 (19.8) | 35.2 (31.6–39.2) | 92 (15.8) | 51.5 (42.0–63.2) | 424 (18.7) |
| Missing | 362 (21.5) | 90 (15.4) | 452 (20.0) | ||
| Chronic disease | |||||
| Non-fatal chronic disease‡ | |||||
| No | 482 (28.7) | 29.4 (26.9–32.2) | 228 (39.0) | 38.6 (33.9–44.0) | 710 (31.4) |
| Yes | 1,177 (70.1) | 28.1 (26.5–29.7) | 352 (60.3) | 33.3 (30.0–37.0) | 1,529 (67.6) |
| Missing | 19 (1.1) | 4 (0.7) | 23 (1.0) | ||
| Chronic lung disease# | |||||
| No | 1448 (86.3) | 28.1 (26.7–29.6) | 505 (86.5) | 35.0 (32.1–38.2) | 1,953 (86.3) |
| Yes | 217 (12.9) | 31.0 (27.1–35.4) | 77 (13.2) | 36.1 (28.8–45.2) | 294 (13.0) |
| Missing | 13 (0.8) | 2 (0.3) | 15 (0.7) | ||
| Circulatory disease§ | |||||
| No | 676 (40.3) | 28.3 (26.2–30.5) | 255 (43.7) | 32.4 (28.6–36.7) | 931 (41.2) |
| Yes | 986 (58.8) | 28.5 (26.8–30.4) | 326 (55.8) | 38.0 (34.1–42.4) | 1312 (58.0) |
| Missing | 16 (0.9) | 3 (0.5) | 19 (0.8) | ||
| Cancer (except for skin cancer) | |||||
| No | 1530 (91.2) | 28.3 (27.0–29.8) | 551 (94.4) | 34.8 (32.0–37.8) | 2,081 (92.0) |
| Yes | 135 (8.1) | 30.2 (25.5–35.8) | 31 (5.3) | 45.0 (31.7–64.0) | 166 (7.3) |
| Missing | 13 (0.7) | 2 (0.3) | 15 (0.7) | ||
| Diabetes | |||||
| No | 1548 (92.3) | 28.0 (26.6–29.5) | 546 (93.5) | 35.1 (32.2–38.1) | 2,094 (92.6) |
| Yes | 125 (7.4) | 36.2 (30.4–43.2) | 37 (6.3) | 37.6 (27.2–51.9) | 162 (7.1) |
| Missing | 5 (0.3) | 1 (0.2) | 6 (0.3) | ||
Number of ADL items performed independently according to a modified version of Katz ADL: bathing, dressing, toileting, transferring and eating. “Not disabled” defined as independent in all five items, “Moderately disabled” defined as independent in 3–4 items, and “Severely disabled” defined as independent in 0–2 items
Yes indicates one or more of the following diseases: osteoarthrosis, rheumatoid arthritis, osteoporosis, cataract or glaucoma
Yes indicates chronic bronchitis and/or asthma
Yes indicates one or more of the following diseases/conditions: stroke, heart attack, angina pectoris, irregular heart rhythm, treatment for hypertension with prescription medicine, other heart problems, heart failure, insufficient blood circulation in the legs
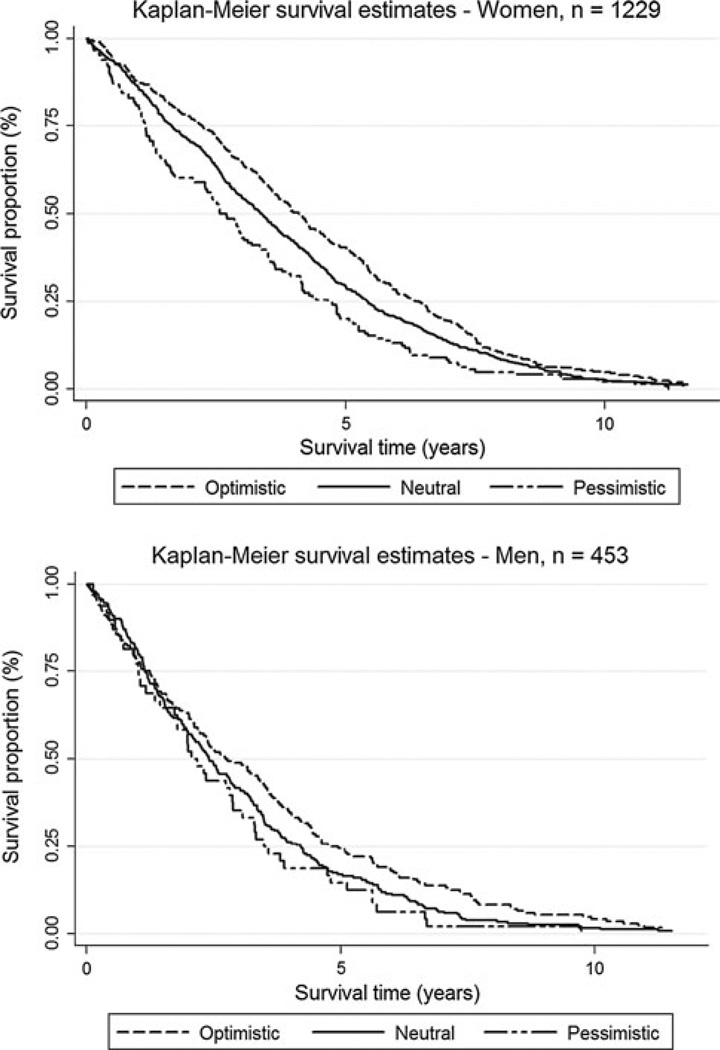
Figure 1 displays the Kaplan–Meier survival curves for optimistic, neutral and pessimistic respondents, stratified by sex. In both sexes, optimists lived longer than did neutral or pessimistic respondents, although more pronounced in women than men. The median survival time in optimistic women was 4.1 years (95 % CI, 3.7–4.4) compared to 3.4 (95 % CI, 3.1–3.6) and 2.6 years (95 % CI, 2.3–3.1) among neutral and pessimistic women, respectively. The corresponding figures for men were 2.7 years (95 % CI, 2.2–3.5), 2.4 years (95 % CI, 2.1–2.8), and 2.1 years (95 % CI, 1.4–2.9), respectively.
Fig. 1.
Kaplan–Meier analysis of survival according to different levels of optimism, stratified by sex. Optimistic individuals had a survival advantage compared to neutral and pessimistic individuals in both women (Log rank test, p < 0.001) and men (Log rank test, p = 0.031)
Univariable analyses revealed that women and men who had an optimistic outlook on their future were at lower risk of death compared to their neutral counterparts [HR 0.82, 95 % CI (0.73–0.93) and 0.81, 95 % CI (0.66–0.99), respectively] (Table 2). When ADL, cognitive functioning and self-reported disease were taken into account the association between optimism and survival weakened in both sexes, but the general pattern persisted. Women who were optimistic were still at lower risk of death compared to neutral women [HR 0.85, 95 % CI (0.74–0.97)]. In optimistic men, the corresponding hazard ratio was also decreased, but the effect was non-significant [HR 0.91, 95 % CI (0.73–1.13)].
Table 2.
Crude and adjusted hazard ratios (95 % CI) for mortality according to optimism
| Women |
Men |
|||||
|---|---|---|---|---|---|---|
| Crude model* HR (95 % CI) |
Multivariable model† HR (95 % CI) |
p value | Crude model* HR (95 % CI) |
Multivariable model† HR (95 % CI) |
p value | |
| Optimistic | 0.82 (0.73–0.93) | 0.85 (0.74–0.97) | 0.01 | 0.81 (0.66–0.99) | 0.91 (0.73–1.13) | 0.39 |
| Neutral | 1 | 1 | 1 | 1 | ||
| Pessimistic | 1.31 (1.08–1.59) | 1.06 (0.87–1.30) | 0.56 | 1.17 (0.88–1.57) | 1.06 (0.78–1.43) | 0.71 |
| p value‡ | p < 0.001 | p = 0.02 | p = 0.03 | p = 0.56 | ||
Non-adjusted crude model. Robust standard errors were used to derive 95 % CI. Women: n = 1,229. Men: n = 453
Hazard ratios adjusted for MMSE, ADL, circulatory disease, cancer (except for skin cancer), diabetes, non-fatal chronic disease, and lung disease. Robust standard errors were used to derive 95 % CI. Women: n = 1214. Men: n = 448
Based on Wald statistics
Pessimistic women and men compared to their neutral counterparts had an increased risk of death in crude analyses (Table 2). Adjustment for confounding variables attenuated the association in both women and men, and the effect of being pessimistic was non-significant [HR 1.06, 95 % CI (0.87–1.30) and 1.06, 95 % CI (0.78–1.43), respectively].
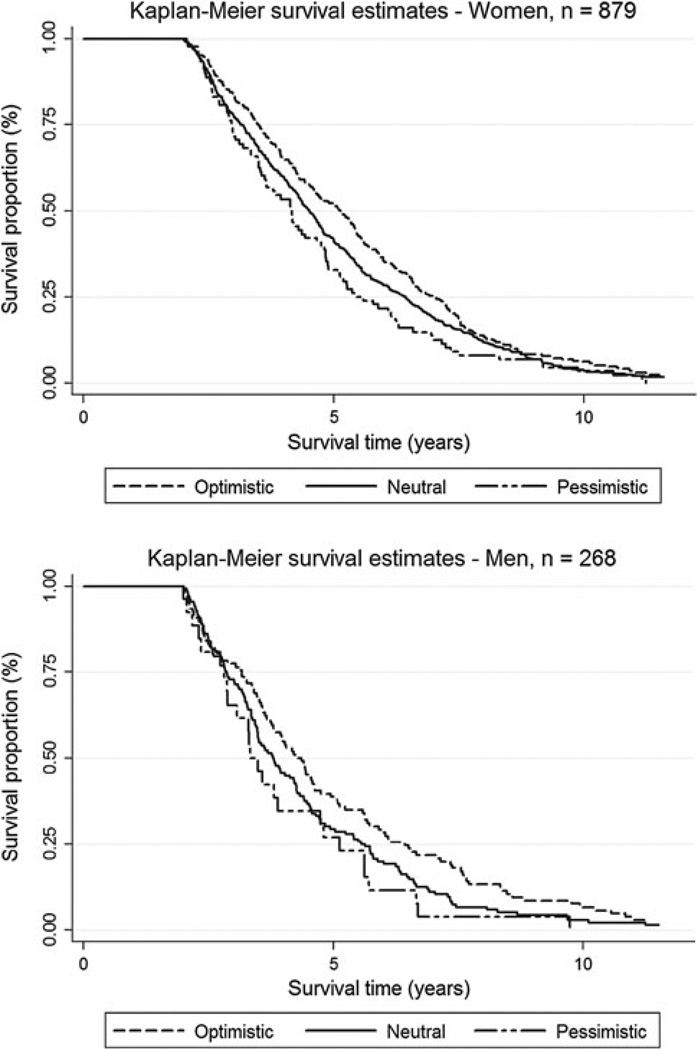
Figure 2 displays the Kaplan–Meier survival curves according to a sensitivity analysis where all deaths in the first 2 years after baseline were discarded to rule out residual confounding from serious chronic disease at baseline. Still, beyond 2 years of observation time, optimistic respondents had a survival advantage compared to neutral and pessimistic individuals in both women (Log rank test, p = 0.009) and men (Log rank test, p = 0.041) (Fig. 2).
Fig. 2.
Sensitivity analysis to explore if residual confounding accounts for the displayed associations. Kaplan–Meier analysis of survival according to different levels of optimism, stratified by sex. After discarding all deaths during the first 2 years after baseline, optimistic individuals still had a survival advantage compared to neutral and pessimistic individuals in both women (Log rank test, p = 0.009) and men (Log rank test, p = 0.041)
The total number of missing responses to the question about optimism was 580 (25.6 %) (449 women and 131 men), of which 448 (358 women and 90 men) were due to proxy interviews where the question about optimism was not asked. The main reason for carrying out a proxy interview was dementia [29]. Proxy respondents were also significantly more severely disabled than those who went through a personal interview (65.6 vs. 15.3 %, p < 0.001). Of the 1,814 non-proxy respondents 132 persons (7.3 %) provided no information about optimism (of which 90 persons responded “do not know” to the question). Compared to the 1,682 respondents who answered the question about optimism, these 132 persons were significantly more severely cognitively impaired (46.1 vs. 21.7 %, p < 0.001) and severely disabled (28.8 vs. 14.2 %, p < 0.001). The MMSE had a total of 452 missing responses, of which 448 were due to proxy interviews. Missing responses to the remaining variables included in the study ranged from 0 to 1 %.
Discussion
These prospective data demonstrate an association between optimism and survival in the oldest-old segment of the population even when health and function is controlled for. In a cohort of Danish nonagenarians followed up over a 12-year period, optimistic nonagenarians lived longer than their more neutral counterparts, although more pronounced in women than men. Similarly, pessimists were at increased risk of death in both sexes, but this association did not reach statistical significance.
Our findings are consistent with those from other prospective studies carried out in younger cohorts [10–12]. Optimism appeared to be a significant predictor of survival, although more pronounced in women than men. This may be explained by the small sample size of men compared to women, i.e., a matter of study power, but the gender differences in the association between optimism and survival also could suggest optimism to be a more important predictor of survival among oldest-old women compared to oldest-old men. This is in agreement with the observation of a “Male–Female Health-Survival Paradox”, i.e., despite better self-reported health and functioning, males have higher mortality [37]. To our knowledge, only one other study focused on sex differences in the association between optimism and survival in a cohort of elderly men and women aged 65–85 years [10]. Contrary to our results, this study found a more pronounced effect of optimism on all cause mortality among men when adjustment was made for age, health behavioral factors and socio-demographic variables [10]. Another study examined sex differences as part of their preliminary analysis, but concluded that the association between optimism and survival was not materially different between men and women in their sample [11]. The less pronounced effect of pessimism on survival in our study may be explained by the low proportion of pessimistic respondents (11.5 %).
Our study had important strengths. First, no exclusion criteria were employed in the 1905 Cohort Survey, i.e., every person born in 1905, including individuals who were living in nursing homes, were approached as potential respondents. Also, the response rate at baseline was relatively high for this age group (63 %), and the non-response analysis showed no difference between responders and non-responders with respect to housing, marital status or hospitalization patterns [29]. Second, due to the completeness of the Danish CRS the follow-up for vital status was complete (only one person was lost to follow-up due to emigration). Third, to our knowledge, no previous study has employed a follow-up period of 12 years in a population of nonagenarians.
The measure of optimism employed in this study was a one-item measure. Other studies examining the effect of optimism on survival utilized different scales, such as the Optimism–Pessimism Scale (PSM) of the Minnesota Multiphasic Personality Inventory (MMPI) measuring explanatory style optimism [38] or the life orientation test (LOT) measuring dispositional optimism [22]. We did not validate our measure of optimism against other specific scales, but the results of our study show that the simple question about the respondents’ outlook on their own future is predictive of survival.
The question is whether the association between optimism and survival in this study is genuine, or if residual confounding accounts for the displayed associations. The risk of substantial residual confounding was minimized by the adjustment for factors previously shown to predict survival in this population. However, potential residual confounding concerning chronic disease may be present, even after adjustment for prevalent disease at baseline. For example, if a respondent suffers from cancer at baseline this would only add a single count to the self-reported disease score and probably not have much effect on either the physical disability or cognitive disability measures. Yet it could depress the sense of optimism. To examine the robustness of our analyses and to rule out that our results could be explained by residual confounding from the presence of serious chronic disease at baseline, we discarded all deaths during the first 2 years after the baseline interview. Still, beyond 2 years of observation time, optimistic respondents had a survival advantage compared to neutral and pessimistic individuals in both women and men (Fig. 2).
Consistent with earlier studies, the present study showed optimism to be a possible predictor of survival even after adjustment for a number of baseline confounding factors. Whether the association between optimism and survival is causal or whether the effect of optimism is mediated through underlying pathways remains, however, an unresolved question. Behavioral differences between optimists and pessimists may exert their effect in favor of better survival. For example, optimists compared to pessimists appear to adopt more favorable and effective coping strategies in the face of adversity [39, 40], and optimists are more likely than pessimists to proactively engage in health promoting behavior [41, 42]. Such important behavioral differences between optimists and pessimists may act as mediators in the association between optimism and survival, and thus may represent key variables to include and explore in future studies examining optimism as a predictor of physical health.
Conclusions
In conclusion, we found an inverse relationship between optimism and mortality in a Danish cohort of oldest-old women. Optimists enjoyed increased longevity whereas pessimists incurred higher death rates compared to neutral individuals.
Acknowledgments
The study was supported by U.S. National Institute on Aging Research Grant PO1AG08761. The Danish Aging Research Center is supported by a grant from the VELUX foundation.
Footnotes
The work was carried out at The Danish Aging Research Center, Institute of Public Health, University of Southern Denmark, J. B. Winsløwsvej 9B, 5000 Odense C, Denmark.
Conflict of interest The authors declare that they have no conflict of interest regarding the paper.
Contributor Information
Henriette Engberg, Department of Epidemiology, The Danish Aging Research Center, Institute of Public Health, University of Southern Denmark, Odense, Denmark; Research Unit of Clinical Epidemiology, Institute of Clinical Research, University of Southern Denmark and Centre for National Clinical Databases, South, Odense University Hospital, Sdr. Boulevard 29, Entrance 101, 4th floor, 5000 Odense C, Denmark engbergh@gmail.com.
Bernard Jeune, Department of Epidemiology, The Danish Aging Research Center, Institute of Public Health, University of Southern Denmark, Odense, Denmark.
Karen Andersen-Ranberg, Department of Epidemiology, The Danish Aging Research Center, Institute of Public Health, University of Southern Denmark, Odense, Denmark.
Torben Martinussen, Department of Biostatistics, University of Copenhagen, Copenhagen, Denmark.
James W. Vaupel, Department of Epidemiology, The Danish Aging Research Center, Institute of Public Health, University of Southern Denmark, Odense, Denmark Max Planck Institute for Demographic Research, Rostock, Germany; Max Planck Odense Center on the Biodemography of Aging, Odense, Denmark.
Kaare Christensen, Department of Epidemiology, The Danish Aging Research Center, Institute of Public Health, University of Southern Denmark, Odense, Denmark; Department of Clinical Biochemistry and Pharmacology, Odense University Hospital, Odense, Denmark; Department of Clinical Genetics, Odense University Hospital, Odense, Denmark.
References
- 1.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72:227–236. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- 2.Kuper H, Marmot M, Hemingway H. Systematic review of prospective cohort studies of psychosocial factors in the etiology and prognosis of coronary heart disease. Semin Vasc Med. 2002;2:267–314. doi: 10.1055/s-2002-35401. [DOI] [PubMed] [Google Scholar]
- 3.Kubzansky LD, Cole SR, Kawachi I, Vokonas P, Sparrow D. Shared and unique contributions of anger, anxiety, and depression to coronary heart disease: a prospective study in the normative aging study. Ann Behav Med. 2006;31:21–29. doi: 10.1207/s15324796abm3101_5. [DOI] [PubMed] [Google Scholar]
- 4.Schillerstrom JE, Royall DR, Palmer RF. Depression, disability and intermediate pathways: a review of longitudinal studies in elders. J Geriatr Psychiatry Neurol. 2008;21:183–197. doi: 10.1177/0891988708320971. [DOI] [PubMed] [Google Scholar]
- 5.Dalle CL, Maggi S, Noale M, et al. Physical disability and depressive symptomatology in an elderly population: a complex relationship. The Italian Longitudinal Study on Aging (ILSA) Am J Geriatr Psychiatry. 2009;17(2):144–154. doi: 10.1097/jgp.0b013e31818af817. [DOI] [PubMed] [Google Scholar]
- 6.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70:741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 7.Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131:925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- 8.Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: a meta-analytic review. Ann Behav Med. 2009;37:239–256. doi: 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Forgeard MJC, Seligman MEP. Seeing the glass half full: a review of the causes and consequences of optimism. Pratiques Psychologiques. 2012;18:107–120. [Google Scholar]
- 10.Giltay EJ, Geleijnse JM, Zitman FG, Hoekstra T, Schouten EG. Dispositional optimism and all-cause and cardiovascular mortality in a prospective cohort of elderly Dutch men and women. Arch Gen Psychiatry. 2004;61:1126–1135. doi: 10.1001/archpsyc.61.11.1126. [DOI] [PubMed] [Google Scholar]
- 11.Brummett BH, Helms MJ, Dahlstrom WG, Siegler IC. Prediction of all-cause mortality by the Minnesota Multiphasic Personality Inventory Optimism-Pessimism Scale scores: study of a college sample during a 40-year follow-up period. Mayo Clin Proc. 2006;81:1541–1544. doi: 10.4065/81.12.1541. [DOI] [PubMed] [Google Scholar]
- 12.Giltay EJ, Kamphuis MH, Kalmijn S, Zitman FG, Kromhout D. Dispositional optimism and the risk of cardiovascular death: the Zutphen Elderly Study. Arch Intern Med. 2006;166:431–436. doi: 10.1001/archinte.166.4.431. [DOI] [PubMed] [Google Scholar]
- 13.Kubzansky LD, Sparrow D, Vokonas P, Kawachi I. Is the glass half empty or half full? A prospective study of optimism and coronary heart disease in the normative aging study. Psychosom Med. 2001;63:910–916. doi: 10.1097/00006842-200111000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Tindle HA, Chang YF, Kuller LH, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s health initiative. Circulation. 2009;120:656–662. doi: 10.1161/CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giltay EJ, Zitman FG, Kromhout D. Dispositional optimism and the risk of depressive symptoms during 15 years of follow-up: the Zutphen Elderly Study. J Affect Disord. 2006;91:45–52. doi: 10.1016/j.jad.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 16.Scheier MF, Matthews KA, Owens JF, et al. Optimism and rehospitalization after coronary artery bypass graft surgery. Arch Intern Med. 1999;159:829–835. doi: 10.1001/archinte.159.8.829. [DOI] [PubMed] [Google Scholar]
- 17.Carver CS, Smith RG, Antoni MH, Petronis VM, Weiss S, Derhagopian RP. Optimistic personality and psychosocial well-being during treatment predict psychosocial well-being among long-term survivors of breast cancer. Health Psychol. 2005;24:508–516. doi: 10.1037/0278-6133.24.5.508. [DOI] [PubMed] [Google Scholar]
- 18.Allison PJ, Guichard C, Fung K, Gilain L. Dispositional optimism predicts survival status 1 year after diagnosis in head and neck cancer patients. J Clin Oncol. 2003;21:543–548. doi: 10.1200/JCO.2003.10.092. [DOI] [PubMed] [Google Scholar]
- 19.Maruta T, Colligan RC, Malinchoc M, Offord KP. Optimists vs pessimists: survival rate among medical patients over a 30-year period. Mayo Clin Proc. 2000;75:140–143. doi: 10.4065/75.2.140. [DOI] [PubMed] [Google Scholar]
- 20.Peterson C, Seligman ME. Explanatory style and illness. J Pers. 1987;55:237–265. doi: 10.1111/j.1467-6494.1987.tb00436.x. [DOI] [PubMed] [Google Scholar]
- 21.Peterson C, Seligman ME, Vaillant GE. Pessimistic explanatory style is a risk factor for physical illness: a thirty-five-year longitudinal study. J Pers Soc Psychol. 1988;55:23–27. doi: 10.1037//0022-3514.55.1.23. [DOI] [PubMed] [Google Scholar]
- 22.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4:219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 23.Scheier MF, Carver CS. Dispositional optimism and physical well-being: the influence of generalized outcome expectancies on health. J Pers. 1987;55:169–210. doi: 10.1111/j.1467-6494.1987.tb00434.x. [DOI] [PubMed] [Google Scholar]
- 24.Isaacowitz DM, Seligman ME. Cognitive style predictors of affect change in older adults. Int J Aging Hum Dev. 2002;54:233–253. doi: 10.2190/J6E5-NP5K-2UC4-2F8B. [DOI] [PubMed] [Google Scholar]
- 25.Nybo H, Petersen HC, Gaist D, et al. Predictors of mortality in 2,249 nonagenarians—the Danish 1905-Cohort Survey. J Am Geriatr Soc. 2003;51:1365–1373. doi: 10.1046/j.1532-5415.2003.51453.x. [DOI] [PubMed] [Google Scholar]
- 26.Bravell ME, Berg S, Malmberg B. Health, functional capacity, formal care, and survival in the oldest old: a longitudinal study. Arch Gerontol Geriatr. 2008;46:1–14. doi: 10.1016/j.archger.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Xie J, Matthews FE, Jagger C, Bond J, Brayne C. The oldest old in England and Wales: a descriptive analysis based on the MRC Cognitive Function and Ageing Study. Age Ageing. 2008;37:396–402. doi: 10.1093/ageing/afn061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roth M, Tym E, Mountjoy CQ, et al. CAMDEX. A standardised instrument for the diagnosis of mental disorder in the elderly with special reference to the early detection of dementia. Br J Psychiatry. 1986;149:698–709. doi: 10.1192/bjp.149.6.698. [DOI] [PubMed] [Google Scholar]
- 29.Nybo H, Gaist D, Jeune B, et al. The Danish 1905 cohort: a genetic-epidemiological nationwide survey. J Aging Health. 2001;13:32–46. doi: 10.1177/089826430101300102. [DOI] [PubMed] [Google Scholar]
- 30.Nybo H, Gaist D, Jeune B, McGue M, Vaupel JW, Christensen K. Functional status and self-rated health in 2,262 nonagenarians: the Danish 1905 Cohort Survey. J Am Geriatr Soc. 2001;49:601–609. doi: 10.1046/j.1532-5415.2001.49121.x. [DOI] [PubMed] [Google Scholar]
- 31.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 32.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 33.George LK, Blazer DF, Winfield-Laird I, et al. Psychiatric disorders and mental health service use in later life: evidence from the Epidemiologic Catchment Area Program. In: Brody J, Maddox G, editors. Epidemiology and Aging. New York: Springer; 1988. pp. 189–219. [Google Scholar]
- 34.Fillenbaum GG, George LK, Blazer DG. Scoring nonresponse on the Mini-Mental State Examination. Psychol Med. 1988;18:1021–1025. doi: 10.1017/s0033291700009946. [DOI] [PubMed] [Google Scholar]
- 35.Lin DY, Wei LJ, Ying Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika. 1993;80:557–572. [Google Scholar]
- 36.STATA Corporation STATA Statistical Software Release 11.1. College Station TX 77845 USA: STATA Corporation; [Google Scholar]
- 37.Oksuzyan A, Juel K, Vaupel JW, Christensen K. Men: good health and high mortality. Sex differences in health and aging. Aging Clin Exp Res. 2008;20:91–102. doi: 10.1007/bf03324754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malinchoc M, Offord KP, Colligan RC. PSM-R: Revised Optimism-Pessimism Scale for the MMPI-2 and MMPI. J Clin Psychol. 1995;51:205–214. doi: 10.1002/1097-4679(199503)51:2<205::aid-jclp2270510210>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 39.Nes LS, Segerstrom SC. Dispositional optimism and coping: a meta-analytic review. Pers Soc Psychol Rev. 2006;10:235–251. doi: 10.1207/s15327957pspr1003_3. [DOI] [PubMed] [Google Scholar]
- 40.Rasmussen HN, Wrosch C, Scheier MF, Carver CS. Self-regulation processes and health: the importance of optimism and goal adjustment. J Pers. 2006;74:1721–1747. doi: 10.1111/j.1467-6494.2006.00426.x. [DOI] [PubMed] [Google Scholar]
- 41.Salovey P, Rothman AJ, Detweiler JB, Steward WT. Emotional states and physical health. Am Psychol. 2000;55:110–121. doi: 10.1037//0003-066x.55.1.110. [DOI] [PubMed] [Google Scholar]
- 42.Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev. 2010;30:879–889. doi: 10.1016/j.cpr.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]