Abstract
Introduction
Older adults are generally considered to be at greater risk for medication non-adherence due to factors such as medication complexity, side effects, cost, and cognitive decline. However, this generalization may not apply to older adults with human immunodeficiency virus (HIV). Regardless of age, suboptimal adherence to antiretroviral therapy (ART) can lead to increased viral load, immunosuppression, drug-resistant viral strains, co-morbidities, and opportunistic infections. Understanding trends of adherence to ART among older adults is critical, especially as the population of people living with HIV grows older.
Objectives
The purpose of this systematic review and meta-analysis is to determine if older individuals with HIV are less likely to be non-adherent to antiretroviral therapy than younger individuals with HIV.
Design
A systematic search in PubMed, Embase, and PsycINFO was conducted to identify peer-reviewed articles evaluating adherence to ART in older adults. Two independent reviewers screened abstracts, applied inclusion criteria, and appraised study quality. The bibliographies of qualifying studies were searched. Data were abstracted from studies by two independent authors. Meta-analyses were conducted, and adherence levels were reported as the relative risk of non-adherence in older individuals compared to younger individuals.
Results
The systematic search yielded 1,848 abstracts. Twelve studies met full inclusion criteria. The overall meta-analysis found that older age reduced risk for non-adherence by 27% (Relative Risk (RR) 0.72, 95% Confidence Interval (CI) 0.64–0.82). Studies assessing both short-term and long-term adherence demonstrated a significant reduction in non-adherence among older patients (RR 0.75, 95% CI 0.64–0.87 and RR 0.65, 95% CI 0.50–0.85, respectively).
Conclusions
Older adults with HIV have a reduced risk for non-adherence to ART than their younger counterparts. Future studies should seek to elucidate contributing factors of adherence among older individuals with HIV.
Keywords: Aged, human immunodeficiency virus, adherence, antiretroviral medications, meta analysis
1. Introduction
In an aging world, older adults comprise a significant and growing portion of the HIV-positive population. The "graying" of the HIV epidemic is more evident than ever, with more than half of the United States’ HIV population over the age of 50 by 2015 [1–4].
Aging of the HIV population is a result of both a growing incidence of HIV in older adults and a dramatically improved life expectancy from advances in antiretroviral therapy (ART). These medications have changed management of HIV from a terminal disease model to a chronic disease model of care. This care requires an interdisciplinary approach using principles of geriatrics and chronic disease management [5]. Older adults living with HIV experience increased co-morbidities in addition to accelerated physical and cognitive aging. By convention initiated by the Centers for Disease Control and Prevention (CDC), the HIV literature uses the age of 50 to describe the ‘aging’ HIV-positive population. Treatment strategies have been published to guide providers in the care of these older, HIV-infected individuals [6]. As the prevalence of older individuals living with HIV/AIDS continues to increase, adherence to antiretroviral therapy within this cohort must be carefully examined.
Medication adherence is critical to the success of HIV disease management. Although newer regimens may be effective despite suboptimal adherence, past work demonstrates that for the majority of regimens, patients must adhere to HIV treatment at nearly perfect rates in order to counter disease progression, multi-drug resistance, and immunologic failure [7, 8]. Adherence can be challenging as a consequence of age-related co-morbidities, memory loss, changes in body composition, and adverse effects and drug toxicity due to age related physiological decline in renal and hepatic functions. While older patients with more medications are considered to be at increased risk of non-adherence, some studies show that older adults with HIV may actually achieve greater adherence to therapy than their younger counterparts [7–15]. This particular population may be more organized and experienced in their daily lives, or possibly more motivated after experiencing the initial devastating outcomes of the AIDS epidemic. However, some studies have concluded that age is not associated with improved adherence rates, and many older individuals demonstrate suboptimal adherence to treatment [16–18]. As older adults have been found to have reduced survival rates after HIV diagnosis, and non-adherence may increase risk for progression, determining rates of non-adherence is important to understand risk factors and improve successful treatment [1]. The purpose of this systematic review is to investigate differences in non-adherence to ART between younger and older adults.
2. Methods
2.1 Systematic Search Strategy
We conducted a systematic search in July 2012 to identify peer-reviewed articles evaluating adherence to ART in older adults. We searched Medline, EMBASE and PsychINFO in order to obtain a broad search of relevant peer-reviewed articles. Major keyword and subject terms referring to HIV, older age, and adherence were utilized in a Boolean search (See Electronic Supplementary Method (ESM) for complete search statement) [19].
2.2 Eligibility Criteria
Two independent reviewers screened titles and abstracts of all articles. Articles were excluded if they were non-human studies; case reports or review articles; studies that predated the initial use of ART in 1996; included any participants not currently on ART; lacked a control group; or specifically focused on psychiatric disorders, substance abuse, or adherence in children. In addition, bibliographies of full text articles were reviewed for additional titles to be included in the full text review.
2.3 Study Selection and Data Extraction
Two authors reviewed full text articles to determine if studies included adherence findings for older and younger groups of participants. While age over 50 years is conventionally considered “older” in the HIV literature, research studies do not consistently use 50 years old as the cutoff for studies, therefore articles were included in the full text review if participants in the older classification were at least 45 years of age. Given the various definitions and measures of adherence in the literature, studies were excluded if the cut-off for adequate adherence was non-specific or below 80%. Previous meta-analyses have limited studies to those that define adherence at or above 80%. The optimal adherence level remains difficult to determine due to the heterogeneity of ART regimens and patient characteristics, [20–22] along with the inherent difficulty of measuring adherence. Reviewers abstracted follow-up times, definition of adherence, data collection methodologies, sample size, adherence rates, percentage of participants using ART, and control group data. One reviewer abstracted study information and a second reviewer confirmed the accuracy of this data.
Two independent reviewers appraised the quality of evidence in the selected articles using the United States Preventative Services Task Force (USPSTF) criteria for internal and external validity, using categories of poor, fair, and good [23]. In the case of disagreement, a third author independently graded studies. Using the USPSTF definition of external validity, we excluded manuscripts if they were from developing countries.
2.4 Data Analysis
Meta-analysis was conducted using STATA 11.0 (Stata, Inc. College Station, TX) with random effects modeling. The overall outcome is reported as the relative risk (95% Confidence Interval-95%CI) for non-adherence in the older population, compared to the younger population. Heterogeneity is measured with the I2, an approximation of variability in the point estimates attributable to heterogeneity [24]. The significance of the heterogeneity is quantified using a Chi-square test. To identify publication bias, funnel plots were visually examined for asymmetry and quantified using the method of Peter [25].
3. Results
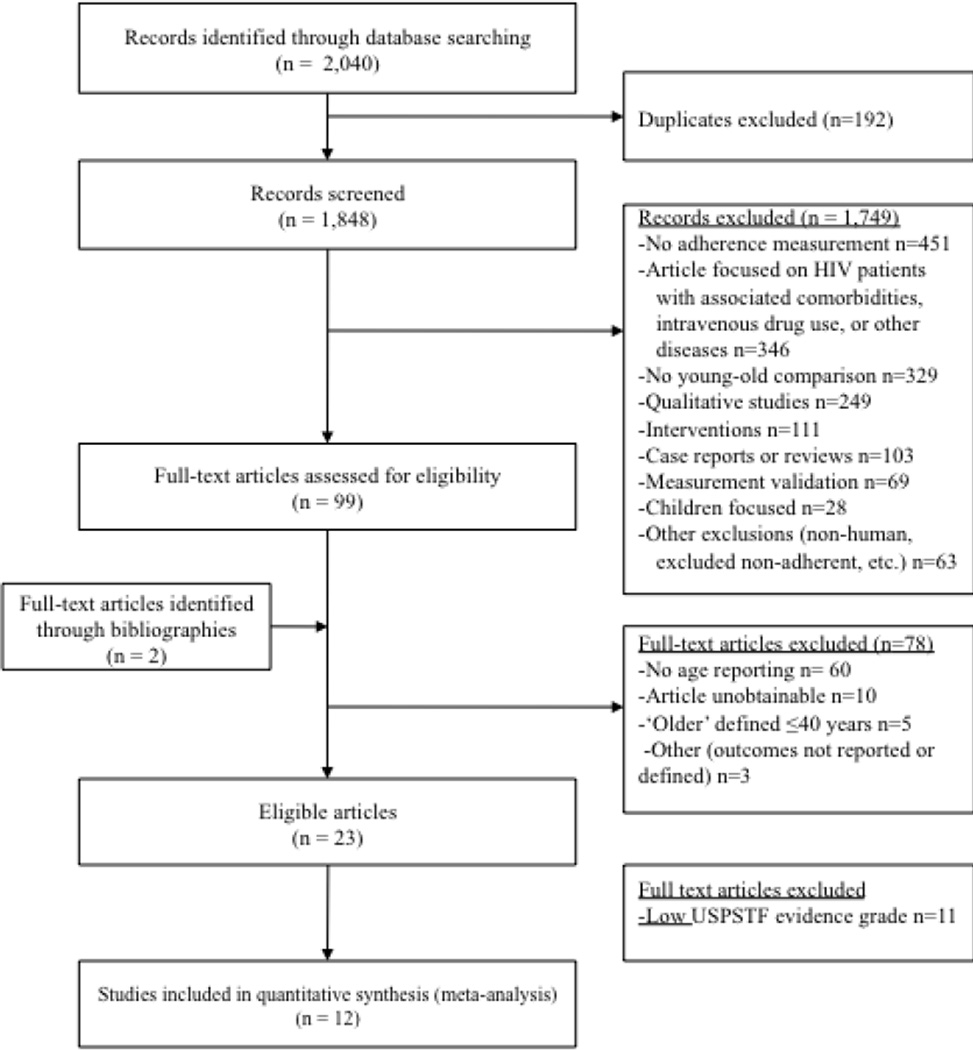
Figure 1 describes the search results and study flow diagram. The systematic search yielded 1,848 articles using no restrictions. 1,749 irrelevant studies were eliminated based on review of title and abstract, with 101 studied for full text review. Of these, 78 studies were excluded because they lacked control groups, defined older age as less than 40, or used adherence measurements that were ambiguous, or not included in the specified criteria. The remaining 23 articles were further assessed for validity and 12 studies ultimately met eligibility criteria for inclusion in the meta-analysis.
Figure 1.
PRIMSA Study Flow Diagram of the Systematic Review: The systematic literature review identified 1,848 abstracts, 101 of which were reviewed to identify the 12 included studies. PRISMA – Preferred Reporting for Items for Systematic Review and Meta Analysis; USPSTF – Unites States Preventative Services Task Force;
Table 1 describes the sample of included studies. Overall, there were 3 cross-sectional studies, 4 prospective studies, 2 retrospective studies, and 3 case controls. Follow up time also varied substantially: 6 studies used a follow up of fewer than eight days, 2 followed patients for 28 days, and the remaining 4 authors followed patients for 180 days or longer. The number of participants completing follow up in the studies ranged from 67.5–100%.
Table 1.
Studies included in the analyses
| Author, Year (references) |
Country | Type of Study |
Total Final Sample |
Length of Follow Up (days) |
Definition of older age |
Adherence Measure |
Definition of Adherence* (%) |
Adherence Young % (n/N) |
Adherence Older % (n/N) |
Internal Validity Grade |
External Validity Grade |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Manfredi, 2000[49] | Italy | Case-control | 105 | 365 | 55 | Pharmacy Refill | 90 | 93 (84) | 90 (21) | Good | Fair |
| Kleeberger, 2001[32] | U.S. | Retrospective cohort | 539 | 4 | 45 | Self Report | 80 | 77 (271) | 78 (268) | Good | Good |
| Pinheiro, 2002[44] | Brazil | Cross sectional | 195 | 2 | 45 | Self Report | 95 | 58 (164) | 52 (31) | Good | Fair |
| Wellons, 2002[45] | U.S. | Retrospective case-control | 269 | 196 | 50 | Chart Review | 100 | 74 (176) | 89 (93) | Fair | Good |
| Johnson, 2003[14] | U.S. | Cross sectional | 2765 | 3 | 50 | Self Report | 90 | 67 (2317) | 74 (441) | Good | Good |
| Tumbarello, 2004[38] | Italy | Case-control | 243 | 183 | 50 | Self Report | 80 | 73 (162) | 84 (81) | Fair | Good |
| Hinkin, 2004[28] | U.S. | Prospective | 148 | 28 | 50 | MEMS | 95 | 26 (109) | 54 (39) | Good | Good |
| Barclay, 2007[16] | U.S. | Prospective | 185 | 28 | 50 | MEMS | 95 | 32 (141) | 77 (44) | Good | Good |
| Silverberg, 2007[29] | U.S. | Retrospective-cohort | 5090 | 365 | 50 | Pharmacy Refill | NR | 85 (4093) | 89 (997) | Fair | Good |
| Sherr, 2010[50] | U.K. | Cross sectional | 479 | 7 | 55 | Self Report | 100 | 37 (333) | 56 (153) | Fair | Good |
| Kyser, 2011[27] | U.S. | Prospective | 528 | 3 | 48 | Self Report | 100 | 83 (399) | 88 (129) | Good | Good |
| Raboud 2011[42] | Canada | Prospective | 779 | 4 | 50 | Self Report | 100 | 83 (447) | 88(332) | Good | Good |
MEMS - Medication Event Monitoring System; NR- not reported
Adherence was defined by each study as the percentage of doses taken as prescribed, and each study set specific cutoffs as a definition of adherence.
Adherence was either measured subjectively by patient self-reported questionnaires, or by system-based measures such as pill counts, record extraction, prescription refill records, or electronic monitoring (i.e. pill bottle cap openings called the Medication Event Monitoring System (MEMS)). Most studies (n=7) collected participant adherence rates by means of self-report questionnaires. However, 2 studies used MEMS, 2 studies used pharmacy re-fill records, and 1 study conducted a chart review [26]. The definition of adequate adherence varied from taking 80% to 100% of prescribed doses of ART.
The definition of “older age” was variable, ranging from at least 45 to 55 years old. Fifty-eight percent (n=7) defined “older age” as at least 50 years old, while 25% (n=3) used a 45 years of age cutoff. One study used 55 years of age, and in another study the older group was defined as the cohort 48 years of age and older [27].
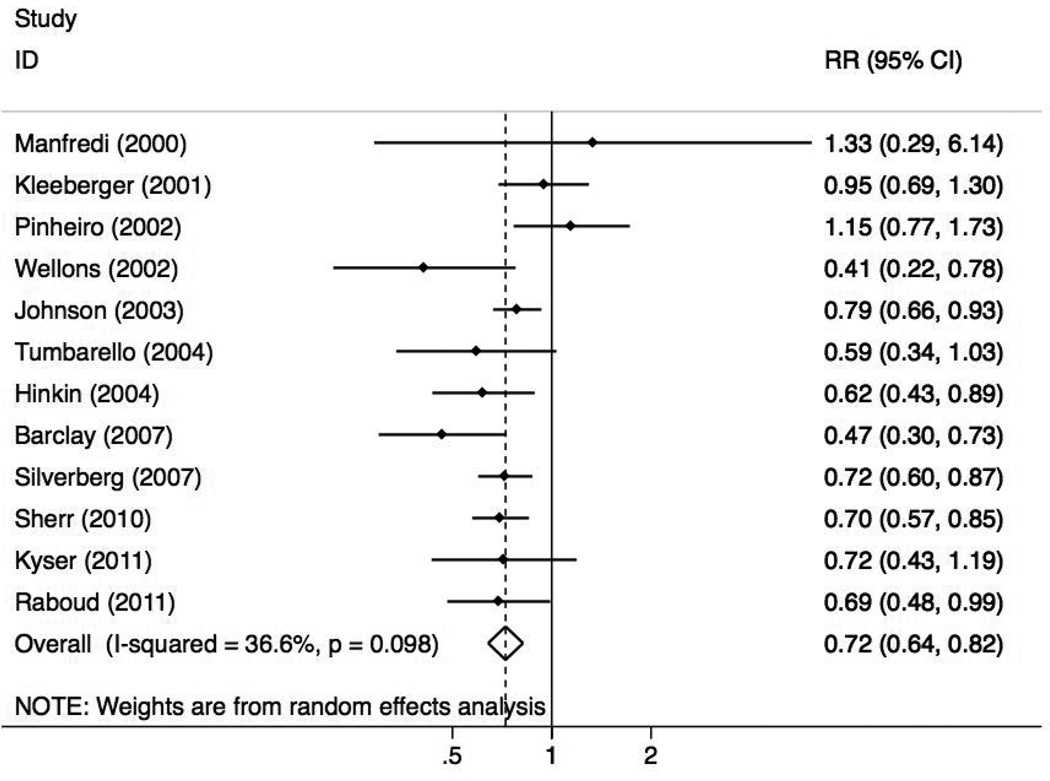
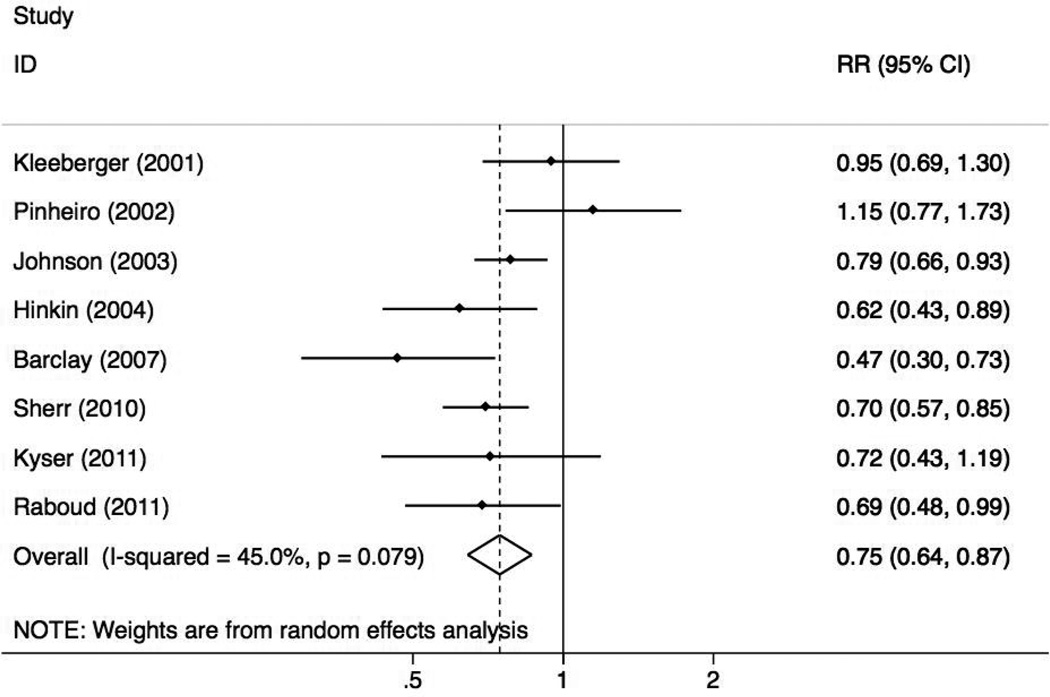
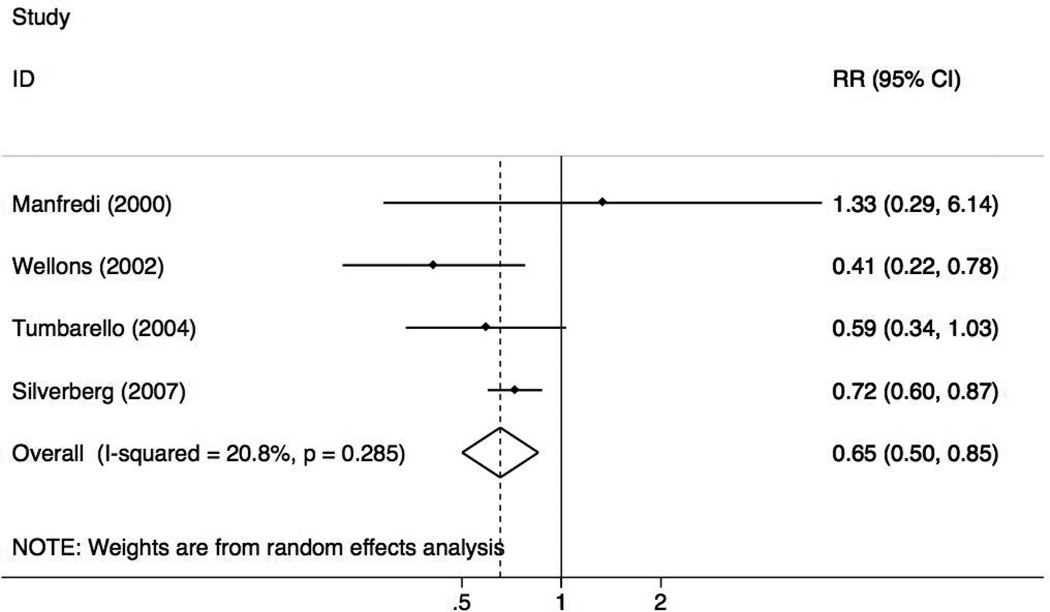
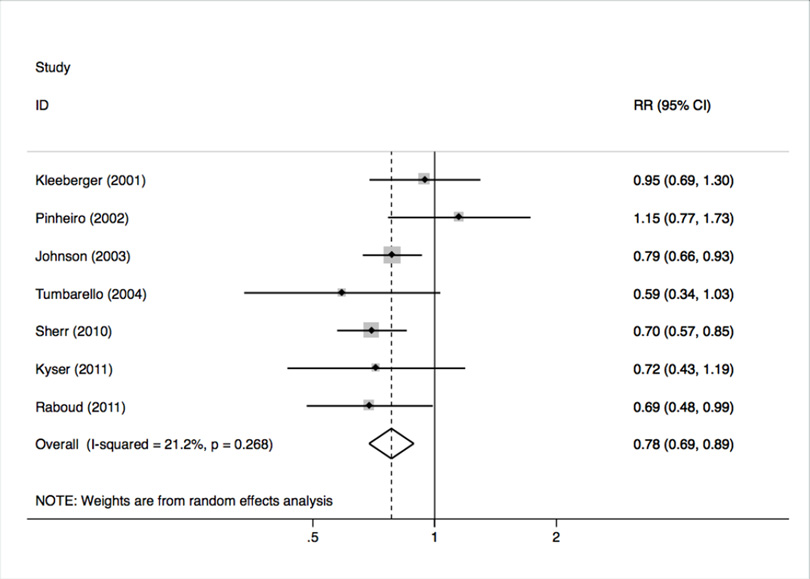
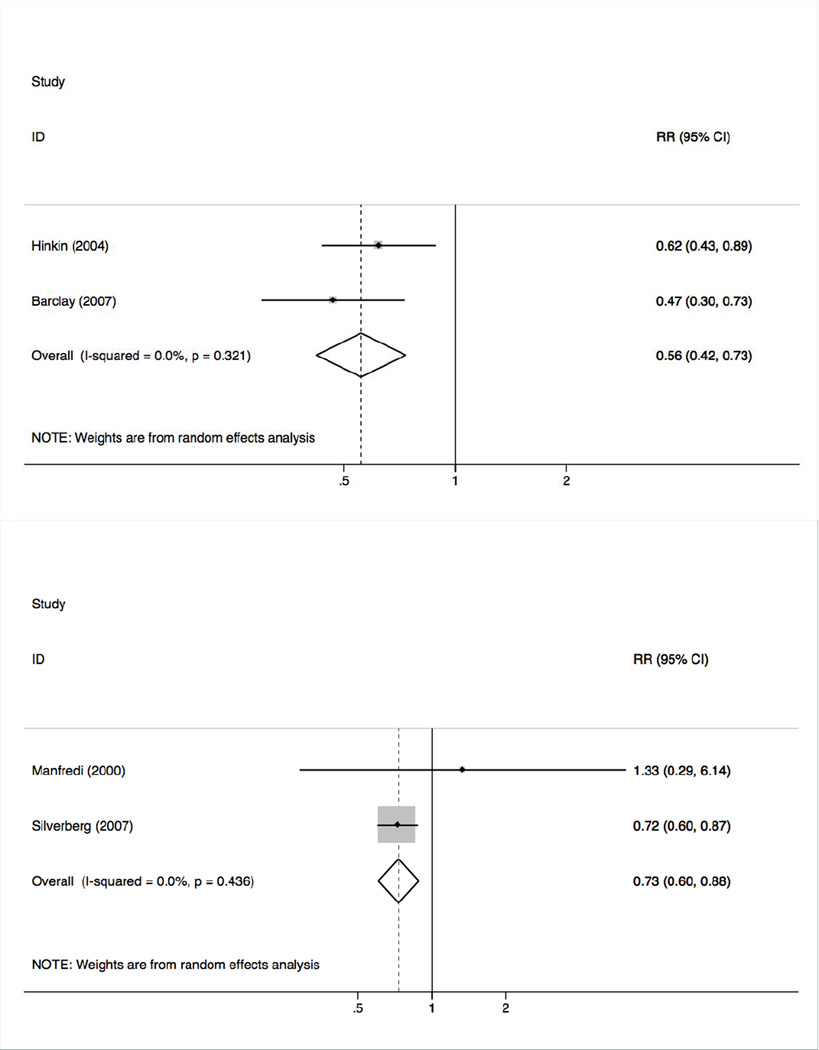
Figure 2 illustrates the three forest plots for the meta-analysis, which demonstrate that older age reduced the risk for non-adherence by 27%, (RR 0.72, 95% CI 0.64–0.82). Heterogeneity was not a significant factor in this analysis (I2=37%, p=0.10). Table 2 describes the meta-analyses, which examined short-term (less than or equal to one month) and long-term (greater than one month) follow up time. Older age reduces the risk for non-adherence by 25% in the short-term (RR 0.75, 95%CI 0.64–0.87) and 35% in the longer-term assessments (RR 0.65, 95%CI 0.50–0.85). Studies measuring non-adherence with patient self-report show an overall significant reduction in non-adherence according to age (RR 0.78, 95% CI 0.69–0.89). Studies utilizing MEMS caps and pharmacy records demonstrated an even greater reduction in non-adherence (RR 0.56, 95% CI 0.42–0.74 & RR 0.73, 95% CI 0.61–0.88, respectively), though this analysis is limited by a small number of studies [16, 28]. In general, the magnitude of risk reduction remains consistent across studies and adherence methods (Figure 3). In analyses of publication bias, the visual scan of the funnel plots demonstrated no bias and no significant small study effects were found in the analyses.
Figure 2.
Forest Plots for the Overall Analysis and Sub-analyses of Measurement Time Frames. Panel A is a plot of the risk for non-adherence in older patients relative to younger patients across all studies. Panel B includes those studies that measured adherence for one month or less. Panel C includes those studies measuring adherence for longer than 1 month.
Table 2.
Risk for Non-Adherence in Older Patients
| Number of studies (n) (reference numbers) |
RR | 95%CI | Heterogeneity | ||
|---|---|---|---|---|---|
| I2 | p- value |
||||
| All Studies | 12 [14, 16, 27–29, 32, 38, 42, 44, 45, 49, 51] |
0.72 | 0.64, 0.82 | 37% | .10 |
| Measurement Follow-Up | |||||
| Long-term (>1 month) | 4 [29, 38, 45, 49] |
0.65 | 0.50, 0.85 | 21% | .29 |
| Short-term (≤1 month) | 8 [14, 16, 27, 28, 32, 42, 44, 51] |
0.75 | 0.64, 0.87 | 45% | .08 |
| Measurement Method | |||||
| Self Report | 7 [14, 27, 32, 38, 42, 44, 51] |
0.78 | 0.69, 0.89 | 27% | .21 |
| MEMS Caps | 2 [16, 28] |
0.56 | 0.42, 0.74 | 0% | .32 |
| Pharmacy Refill | 2 [29, 49] |
0.73 | 0.61, 0.88 | 0% | .44 |
RR is relative risk for non adherence in the older participants relative to the younger
95%CI - 95% Confidence Interval
I2 is the variation in RR attributable to heterogeneity (lower is better)
n is the number of studies included
Figure 3.
Forest Plots for the Sub-analyses of Measurement Type. Panel A are those studies that utilized a self report system. Panel B are those studies that used the Medication Event Monitoring System (MEMS Caps) which electronically record when a medication bottle is opened. Panel C is are those studies using pharmacy refill records to measure medication adherence.
4. Discussion
This systematic review and meta-analysis was conducted to determine if older age was associated with adherence to ART. We found that older individuals over the age of 50 on ART regimens have a reduced risk of non-adherence when compared to younger individuals. These findings serve as a call for increased understanding of the age, anthropological, and cultural factors associated with adherence.
Medication adherence translates to improved HIV suppression and health outcomes. Two studies found older patients have an increased probability of achieving low HIV viral load. However, this effect disappeared after adjusting for adherence, indicating that adherence may have been a contributor. Another study found non-adherence predicts an inability to suppress viral load, explaining why older individuals with good adherence may be more likely to achieve better viral load suppression [29, 30]. Based on the literature, older adults can achieve successful HIV disease management similar to younger adults if they adhere optimally to ART, despite facing many age-related challenges such as diminished immune system function, cognitive impairment, and coronary artery disease at an earlier age [8, 31].
We found that older age carries a lower risk of non-adherence, however, based on our review we cannot determine the specific causative factors for this increased adherence. Several factors have been shown to affect adherence and could therefore create confounding. By identifying age as a factor that impacts adherence, clinicians can better identify and target younger adults who may be at greater risk of non-adherence, and researchers can better study the specific factors associated with aging that results in better adherence to ART.
4.1 Patient Factors
Studies have suggested multiple patient factors that might affect age-related adherence. Barclay et al, and Kleeberger et al, found non-adherence in younger HIV individuals to be associated with financial dependence on others (e.g. family and government programs), while non-adherence in older individuals was associated with an annual income greater than $10,000 [16, 32]. Financial dependence is a predictor for adherence in younger individuals, creating a possible relationship between income and adherence, as finances and income relate to the ability to purchase medications. Moreover, a recent article reviewing medical care for youth with HIV/AIDS found the leading reasons for non-adherence in youth to be lack of insurance in addition to social and psychological factors. Other factors of adherence for youth included inconsistent daily routine, fear of disclosure, simply forgetting, adverse effects of the medication, and not understanding the need to take medication when one feels well [33].
Additionally, sexual orientation may play a role, but results to-date are inconclusive. Prior research demonstrated that homosexuals might be more likely to adhere to ART than heterosexuals [14, 16]. While the specific reason is unknown, others have suggested the specific impact of the HIV epidemic on the gay community, awareness of the increased risk for HIV transmission in men who have sex with men and the generational experience of those who experienced the devastating effects of the emergence of the HIV epidemic.
Interestingly, older adults show higher tolerance to treatment, because they express fewer reasons, such as nausea and pill burden, to switch treatment [18, 30]. Older individuals may have more experience with taking medications, following more complex regimens, or have more co-morbidities than younger patients, leading to fewer treatment complaints or perceived burdens. Medication complexity is a significant component of adherence, as is age, and multiple other psychosocial factors [34–36].
Some studies included in this review identified psychosocial factors as determinants of adherence, yet it was unclear whether these factors were specific to younger or older individuals with HIV. In evaluating psychosocial models to improve adherence among HIV-positive older adults, Johnson et al. found negative affect to be the mediator among maladaptive coping, social support, and adherence[37]. Factors of adherence, including affect and attitude to HIV and ART, may differ among older adults newly infected with HIV and those affected by HIV in years preceding widely available, effective therapy.
4.2 Medical Factors
Our finding of better adherence to ART among older adults is interesting and somewhat unexpected based on the greater presence of traditional risk factors that could impair adherence in older adults. Our meta-analysis found improved adherence despite studies that show older adults are more likely to have greater co-morbidity, cognitive decline, and pill-burden, which may all impact adherence (14–35)
Changes in body composition may be exacerbated by long-term use of ART. In addition to differences in age, older cohorts include participants with a greater co-morbidity score, increased mortality, and higher severity of illness [29, 38]. Cognitive impairment, specifically executive function, memory, and psychomotor speed, confers 2.5 times greater risk for non-adherence specifically for older adults with HIV [16, 28]. Hinkin et al, found that 74% of older HIV-positive adults with impairments in executive function, 78% of those with psychomotor slowing, and 67% of those with memory impairment were poor adherers [28]. Barclay et al, found no psychiatric variables associated with adherence in older individuals, although apathy predicted non-adherence in younger individuals [16]. Shah et al, cited lack of reminders, confusion, adverse effects, and pain to be correlates of poor adherence for all participants [39].
Barriers to medication adherence in the elderly have been previously explored in a systematic review. While the review included patients over 65 years old with any medical condition, it also reports on medical-related factors associated with adherence. Cognitive impairment was associated with non-adherence in one of the five studies measuring cognitive impairment[40]. The study by Hinkin et al, in this systematic review found an association with cognitive impairment and medication adherence. This may be capturing a factor unique to HIV patients since HIV/AIDS is a disease that can directly affect cognitive function. There is significant heterogeneity in the studies, making a definitive conclusion challenging. Of note, one of the studies that did not find a relationship between adherence and cognitive impairment in the general elderly found non-adherence was associated with independent medication management[40].
Additionally, age-related disease burden often increases pill burden. Our analysis found conflicting results on this issue. Some studies found poor adherence for all ages is not associated with amount of time on ART, pill burden, number of prior ART regimens, or duration of HIV illness [14, 27, 39, 41, 42]. Conversely, other studies found higher numbers of daily doses, HIV-related symptoms, lower self-efficacy, and being “tired of taking medications” to be predictive of poorer adherence [14, 27, 42, 43]. Kyser found a diagnosis of HIV greater than 5 years was associated with non-adherence [27]. Kleeberger identified a direct correlation between number of ART medications, and adherence [32]. Although Pinheiro did not find an association between adherence and age, the number of times per day ART was taken significantly correlated with adherence across all ages [44]. The ability of regimen complexity to predict adherence remains unclear. In fact, this may be unique to each patient based on his or her prior medication experiences and individual perception of complexity.
4.3 Study-Related Factors
Four distinct study designs- cross-sectional, prospective cohort, retrospective cohort, and case control- are included among the 12 articles. Each study design employed unique methods to enroll participants. Many of the initially enrolled participants were lost to follow up or died, which may lead to an underestimation of the reduced risk of non-adherence seen in older adults.
Adherence assessment methods of self-report and MEMS may be subject to reporting bias. Self-reporting methods may overestimate adherence rates due to participant recall and social desirability [45]. This reporting bias may differ in older and younger patients [46]. While MEMS caps are considered a more objective standard, self-reports may be sufficiently reliable. A recent study found that an Adult AIDS Clinical Trial Group (AACTG) 4-day recall instrument, and a 1-month recall instrument, both significantly correlate to MEMS caps measurement [47]. Additionally, an ACTG randomized control study demonstrated self-reporting methods are able to predict HIV viral load response [48]. Nonetheless, adherence is a complex behavior that occurs along a spectrum, and is difficult to measure and study.
In addition to age, health and social factors may play a role in adherence. Further investigation of these factors would be important for a deeper understanding of adherence in HIV-positive patients, and may translate to adherence in the general population.
4.4 Strengths/Limitations
This systematic review and meta-analysis possesses several significant strengths. We had two independent reviewers conduct the comprehensive literature search by independently deciding study selection, manuscript review, USPSTF study grading, and data abstraction. Furthermore, by including studies with comparison groups, it was possible to perform a more rigorous comparison of age groups. The meta-analysis demonstrated limited heterogeneity and a consistent effect size across studies, allowing for the conclusion that older adults with HIV are more likely to take their medications when compared with their younger counterparts.
Limitations to this work include variable study designs and follow up times of the included studies, although we are unable to determine the directionality of this bias. Findings are also limited by variability in adherence definitions. This is due to the numerous ART regimens, conflicting cutoffs for adequate adherence, and the inconsistent consideration of timing and food requirements for adherence. Furthermore, an arbitrary age definition for ‘older’ individuals with HIV had to be chosen due to lack of uniformity across studies, though most age-cutoffs were consistent with the HIV literature convention of 50 years old for HIV-positive older adults [6, 8].
5. Conclusion
Understanding ART adherence predictors and outcomes is particularly important for providers caring for HIV-positive individuals. We found that older adults with HIV were less likely than younger adults to be non-adherent to ART. This is the first systematic review and meta-analysis to our knowledge to show that older adults with HIV are less likely to be non-adherent to ART than younger adults. While better adherence to ART in older adults has often been postulated to play a role in better virologic response rates to ART, this finding is nonetheless surprising, given the various patient and medical factors that affect adherence. Many factors that affect adherence traditionally worsen adherence for older adults, such as co-morbidities, medication complexity and cognitive impairment. Yet, despite these challenges, older adults with HIV are better at following and taking their ART regimens. Information about the health, cultural, and measurement-related factors that influence ART adherence in older adults is lacking and further research to explore this is needed. We hypothesize that one factor related to the improved adherence of older adults is somewhat of a selection bias; in other words, if a significant portion of the older population with HIV has been living with HIV/AIDS for many years, then perhaps the reason they have successfully survived to older age is by virtue of better adherence throughout their lives. Thus, perhaps there is a subgroup that was more adherent in youth, and as a result was more likely to survive to older age and continue to be more adherent despite the additional challenges common with aging. However, there are likely additional factors that we have not identified, and our findings help point out the need for further investigation into this importance question. We also note that the incidence of new infections with HIV in older adults is rising, and perhaps future research will identify whether adherence in older adults who contract HIV later in life is different than the adherence of those you contracted HIV when younger. Adherence to ART is critical for the successful treatment of HIV, and as long as adherence rates remain less than 100%, clinicians need to better understand the factors that impact adherence and also need to be able to identify, and target those at greater risk.
Supplementary Material
Acknowledgements
We would like to thank Dr. Paul Bain of the Countway Library of Medicine, for his guidance provided for the systematic review and Mrs. Elizabeth Archambault for her editing.
Funding:
This work was funded by Dr Simone’s HRSA Geriatric Academic Career Award Grant No. K01HP23811 and the NIH T35-AG038027-02 grant awarded to Dr Rudolph and Ms Ghidei. Dr Kostas is partially supported by a John A. Hartford Center of Excellence Award. Dr Rudolph is supported by a VA Rehabilitation Research Career Development Award and a VA Patient Safety Center of Inquiry award. Drs Kostas, Salow, and Rudolph receive funding from a T21 alternative to non-institutional long term care grant. Drs Salow, Paquin, Skarf, Kostas, and Rudolph are employees of the Veterans Health Administration. The views expressed are those of the authors, and do not reflect the official policies of the Veterans Health Administration or U.S. Government.
Footnotes
Statement of COI:
Dr Simone received an honorarium from the American Academy of HIV Medicine / American Geriatrics Society for participation in the HIV and Aging Guidance Project. Drs Ghidei, Salow, Zimmerman, Paquin, Skarf, Kostas and Rudolph have no conflicts of interest to declare.
Author Contributions
Conception and design: Ghidei, Simone, Rudolph, Bain
Acquisition of data: Ghidei, Simone, Salow, Rudolph
Analysis: Ghidei, Simone, Salow, Rudolph
Interpretation of data: Ghidei, Simone, Salow, Zimmerman, Paquin, Skarf, Kostas, Rudolph
Drafting the article: Ghidei, Simone, Salow, Zimmerman, Rudolph
Critical revision: Ghidei, Simone, Salow, Zimmerman, Paquin, Skarf, Kostas, Rudolph, Archambault
Final approval of the manuscript: Ghidei, Simone, Salow, Zimmerman, Paquin, Skarf, Kostas, Rudolph
References
- 1.Brooks JT, Buchacz K, Gebo KA, Mermin J. HIV Infection and Older Americans: The Public Health Perspective. Am J Public Health. 2012;102:1516–1526. doi: 10.2105/AJPH.2012.300844. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention. [Accessed 20 July 2012];HIV/AIDS Surveillance Report, 2010. vol 22 http://www.cdc.gov/hiv/pdf/statistics_surveillance_report_vol_22.pdf. [Google Scholar]
- 3.Center for Disease Control and Prevention. [Accessed 10 Dec 2012];HIV/AIDS Surveillance Report, 2011. vol 23 http://www.cdc.gov/hiv/topics/surveillance/resources/reports. [Google Scholar]
- 4.Center for Disease Control and Prevention. [Accessed 20 July 2012];HIV/AIDS among Persons Aged 50 and Older. 2008 http://www.cdc.gov/hiv/topics/over50/.
- 5.Collaboration TATC. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372:293–299. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abrass CK, Appelbaum JS, Boyd CM, Braithwaite RS, Broudy VC, Covinsky K, et al. HIV and Aging Consensus Project; Recommended Treatment Strategies for Clinicians Managing Older Patients with HIV. J Am Geriatr Soc. 2012;60:974–979. doi: 10.1111/j.1532-5415.2012.03948.x. [DOI] [PubMed] [Google Scholar]
- 7.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453–472. doi: 10.2147/cia.s2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wood E, Hogg RS, Yip B, Harrigan PR, O'Shaughnessy MV, Montaner JS. The impact of adherence on CD4 cell count responses among HIV-infected patients. J Acquir Immune Defic Syndr. 2004;35:261–268. doi: 10.1097/00126334-200403010-00006. [DOI] [PubMed] [Google Scholar]
- 10.Maggiolo F, Ripamonti D, Arici C, Gregis G, Quinzan G, Camacho GA, et al. Simpler regimens may enhance adherence to antiretroviral in HIV-infected patients. HIV Clin Trials. 2002;3:371–378. doi: 10.1310/98b3-pwg8-pmyw-w5bp. [DOI] [PubMed] [Google Scholar]
- 11.Dunham PJ, Karkula JM. Effects of a pharmacy-care program on adherence and outcomes. Am J of Pharm Benefits. 2012;4:e8–e14. [Google Scholar]
- 12.Viswanathan H, Anderson R, Thomas J., Iii Evaluation of an antiretroviral medication attitude scale and relationships between medication attitudes and medication nonadherence. AIDS Patient Care STDS. 2005;19:306–316. doi: 10.1089/apc.2005.19.306. [DOI] [PubMed] [Google Scholar]
- 13.Ruppar TM, Conn VS, Russell CL. Medication adherence interventions for older adults: literature review. Res Theory Nurs Pract. 2008;22:114–147. [PubMed] [Google Scholar]
- 14.Johnson MO, Catz SL, Remien RH, Rotheram-Borus MJ, Morin SF, Charlebois E, et al. Theory-Guided, Empirically Supported Avenues for Intervention on HIV Medication Nonadherence: Findings from the Healthy Living Project. AIDS Patient Care STDS. 2003;17:645–656. doi: 10.1089/108729103771928708. [DOI] [PubMed] [Google Scholar]
- 15.Holodniy M, Hornberger J, Rapoport D, Robertus K, MaCurdy TE, Lopez J, et al. Relationship between antiretroviral prescribing patterns and treatment guidelines in treatment-naive HIV-1-infected US veterans (1992–2004) J Acquir Immune Defic Syndr. 2007;44:20–29. doi: 10.1097/01.qai.0000248354.63748.54. [DOI] [PubMed] [Google Scholar]
- 16.Barclay TR, Hinkin CH, Castellon SA, Mason KI, Reinhard MJ, Marion SD, et al. Age-associated predictors of medication adherence in HIV-positive adults: health beliefs, self-efficacy, and neurocognitive status. Health Psychol. 2007;26:40–49. doi: 10.1037/0278-6133.26.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cuzin L, Delpierre C, Gerard Sp, Massip P, Marchou B. Immunologic and Clinical Responses to Highly Active Antiretroviral Therapy in Patients with HIV Infection Aged 150 Years. Clin Infect Dis. 2007;45:654–657. doi: 10.1086/520652. [DOI] [PubMed] [Google Scholar]
- 18.Sherr L, Harding R, Lampe F, Johnson M, Anderson J, Zetler S, et al. Clinical and behavioural aspects of aging with HIV infection. Psychol Health Med. 2009;14:273–279. doi: 10.1080/13548500902865964. [DOI] [PubMed] [Google Scholar]
- 19.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 20.Elema R, Mills C, Yun O, Lokuge K, Ssonko C, Nyirongo N, et al. Outcomes of a remote, decentralized health center-based HIV/AIDS antiretroviral program in Zambia, 2003 to 2007. J Int Assoc Physicians AIDS Care (Chic) 2009;8:60–67. doi: 10.1177/1545109709331472. [DOI] [PubMed] [Google Scholar]
- 21.Mathes TPD, Antoine SL, Eikermann M. Adherence-enhancing interventions for highly active antiretroviral therapy in HIV-infected patients - a systematic review. HIV medicine. 2013 doi: 10.1111/hiv.12051. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 22.Mills EJNJ, Buchan I, Orbinski J, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006 Aug 9;296:679–690. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- 23. [Accessed 10 July 2012];U.S. Preventive Services Task Force Procedure Manual. AHRQ Publication No. 08-05118-EF; July, 2008. Available at URL: http://www.uspreventiveservicestaskforce.org/uspstf08/methods/procmanual.htm.
- 24.Higgins J. Heterogeneity in meta-analyses should be expected and appropriately quantified. Int J Epidemiol. 2008:1158–1160. doi: 10.1093/ije/dyn204. [DOI] [PubMed] [Google Scholar]
- 25.Sterne JAC, Bradburn MJ, Egger M. In: Meta– Analysis in Stata™, in Systematic Reviews in Health Care: Meta-Analysis in Context, Second Edition. Egger M, Smith GD, Altman DG, editors. London, UK: BMJ Publishing Group; 2008. [Google Scholar]
- 26.Lyimo R, van den Boogarden J, Msoka E, et al. Measuring adherence to antiretroviral therapy in northern Tanzania: feasibility and acceptability of the Medication Event Monitoring System. BMC Public Health. 2011;11:1–20. doi: 10.1186/1471-2458-11-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kyser M, Buchacz K, Bush TJ, et al. Factors associated with non-adherence to antiretroviral therapy in the SUN study. AIDS Care. 2011;23:601–611. doi: 10.1080/09540121.2010.525603. [DOI] [PubMed] [Google Scholar]
- 28.Hinkin CH, Hardy DJ, Mason KI, et al. Medication adherence in HIV-infected adults: effect of patient age, cognitive status, and substance abuse. AIDS. 2004;18:S19–S25. doi: 10.1097/00002030-200418001-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silverberg MJ, Leyden W, Horberg MA, et al. Older age and the response to and tolerability of antiretroviral therapy. Arch Intern Med. 2007;167:684–691. doi: 10.1001/archinte.167.7.684. [DOI] [PubMed] [Google Scholar]
- 30.Sherr L, Lampe FC, Clucas C, et al. Self-reported non-adherence to ART and virological outcome in a multiclinic UK study. AIDS Care. 2010;22:939–945. doi: 10.1080/09540121.2010.482126. [DOI] [PubMed] [Google Scholar]
- 31.Simone MJ, Appelbaum J. HIV in older adults. Geriatrics. 2008;63:6–12. [PubMed] [Google Scholar]
- 32.Kleeberger CA, Phair JP, Strathdee SA, et al. Determinants of heterogeneous adherence to HIV-antiretroviral therapies in the Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr. 2001;26:82–92. doi: 10.1097/00126334-200101010-00012. [DOI] [PubMed] [Google Scholar]
- 33.Dowshen N, D’Angelo L. Health Care Transition for Youth Living With HIV/AIDS. Pediatrics. 2011;128(4):762–771. doi: 10.1542/peds.2011-0068. [DOI] [PubMed] [Google Scholar]
- 34.Greene M, Justice AC, Valcour V, et al. Management of Human Immunodeficiency Virus Infection in Advanced Age. JAMA. 2013;309:1397–1405. doi: 10.1001/jama.2013.2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Justice AC. HIV and aging: time for a new paradigm. Current HIV/AIDS reports. 2010 May;7:69–76. doi: 10.1007/s11904-010-0041-9. [DOI] [PubMed] [Google Scholar]
- 36.Working Group on HIV and Aging. HIV and aging: state of knowledge and areas of critical need for research. A report to the NIH Office of AIDS Research by the HIV and Aging Working Group. J Acquir Immune Defic Syndr. 2012;60:S1–S18. doi: 10.1097/QAI.0b013e31825a3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johnson CJ, Heckman TG, Hansen NB, et al. Adherence to antiretroviral medication in older adults living with HIV/AIDS: A comparison of alternative models. AIDS Care - Psychological and Socio-Medical Aspects of AIDS/HIV. 2009;21(5):541–551. doi: 10.1080/09540120802385611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tumbarello MRR, de Gaetano Donati K, Bertagnolio S, et al. Older age does not influence CD4 cell recovery in HIV-1 infected patients receiving highly active antiretroviral therapy. BMC Inferctious Diseases. 2004;4:1–32. doi: 10.1186/1471-2334-4-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shah B, Walshe L, Saple DG, et al. Adherence to antiretroviral therapy and virologic suppression among HIV-infected persons receiving care in private clinics in Mumbai, India. Clin Infect Dis. 2007;44:1235–1244. doi: 10.1086/513429. [DOI] [PubMed] [Google Scholar]
- 40.Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: Looking beyond cost and regimen complexity. Am J Geriatr Pharmacotherapy. 2011;9:11–23. doi: 10.1016/j.amjopharm.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ladefoged K, Andersson M, Koch A, et al. Living conditions, quality of life, adherence and treatment outcome in Greenlandic HIV patients. Int J Circumpolar Health. 2012;71:1–8. doi: 10.3402/ijch.v71i0.18639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Raboud J, Li M, Walmsley S, et al. Once daily dosing improves adherence to antiretroviral therapy. AIDS Behav. 2011;15:1397–1409. doi: 10.1007/s10461-010-9818-5. [DOI] [PubMed] [Google Scholar]
- 43.Kunutsor S, Evans M, Thoulass J, et al. Ascertaining baseline levels of antiretroviral therapy adherence in Uganda: a multimethod approach. J Acquir Immune Defic Syndr. 2010;55:221–224. doi: 10.1097/QAI.0b013e3181e255ec. [DOI] [PubMed] [Google Scholar]
- 44.Pinheiro CA, de-Carvalho-Leite JC, Drachler ML, et al. Factors associated with adherence to antiretroviral therapy in HIV/AIDS patients: a cross-sectional study in Southern Brazil. Braz J Med Biol Res. 2002;35:1173–1181. doi: 10.1590/s0100-879x2002001000010. [DOI] [PubMed] [Google Scholar]
- 45.Wellons MF, Sanders L, Edwards LJ, et al. HIV infection: Treatment outcomes in older and younger adults. J Am Geriatr Soc. 2002;50:603–607. doi: 10.1046/j.1532-5415.2002.50152.x. [DOI] [PubMed] [Google Scholar]
- 46.Watt MH, Maman S, Golin CE, et al. Factors associated with self-reported adherence to antiretroviral therapy in a Tanzanian setting. AIDS Care. 2010;22:381–389. doi: 10.1080/09540120903193708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Buscher AHC, Kallen MA, Giordano TP. Validity of self-report measures in assessing antiretroviral adherence of newly diagnosed, HAART-naïve, HIV patients. HIV Clin Trials. 2011;12:244–254. doi: 10.1310/hct1205-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fletcher M, Brundage R, Chesney M, et al. Four Measures of Antiretroviral Medication Adherence and Virologic Response in AIDS Clinical Trials Group Study 359. J Acq Immune Defic Synd. 2005;40:301–306. doi: 10.1097/01.qai.0000180078.53321.6a. [DOI] [PubMed] [Google Scholar]
- 49.Manfredi R, Chiodo F. A case-control study of virological and immunological effects of highly active antiretroviral therapy in HIV-infected patients with advanced age. AIDS. 2000;14:1475–1477. doi: 10.1097/00002030-200007070-00034. [DOI] [PubMed] [Google Scholar]
- 50.Hinkin CH, Barclay TR, Castellon SA, et al. Drug use and medication adherence among HIV-1 infected individuals. AIDS Behav. 2007;11:185–194. doi: 10.1007/s10461-006-9152-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sherr L, Lampe FC, Clucas C, et al. Self-reported non-adherence to ART and virological adherence to ART and virological outcome in a multiclinic UK study. AIDS care. 2010;22:939–945. doi: 10.1080/09540121.2010.482126. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.