Abstract
Background
Escalating rates of prescription opioid use and abuse have occurred in the context of efforts to improve the treatment of non-malignant pain.
Objectives
To characterize the diagnosis and management of non-malignant pain in ambulatory, office-based settings in the United States between 2000 and 2010.
Design, setting, and participants
Serial cross-sectional and multivariate regression analyses of the National Ambulatory Medical Care Survey (NAMCS), a nationally representative audit of office-based physician visits.
Measures
(1) Annual visits volume among adults with primary pain symptom or diagnosis; (2) receipt of any pain treatment; and (3) receipt of prescription opioid or non-opioid pharmacologic therapy in visits for new musculoskeletal pain.
Results
Primary symptoms or diagnoses of pain consistently represented one-fifth of visits, varying little from 2000 through 2010. Among all pain visits, opioid prescribing nearly doubled from 11.3% to 19.6%, whereas non-opioid analgesic prescribing remained unchanged (26%–29% of visits). One-half of new musculoskeletal pain visits resulted in pharmacologic treatment, though the prescribing of non-opioid pharmacotherapies decreased from 38% of visits (2000) to 29% of visits (2010). After adjusting for potentially confounding covariates, few patient, physician or practice characteristics were associated with a prescription opioid rather than a non-opioid analgesic for new musculoskeletal pain, and increases in opioid prescribing generally occurred non-selectively over time.
Conclusions
Increased opioid prescribing has not been accompanied by similar increases in non-opioid analgesics or the proportion of ambulatory pain patients receiving pharmacologic treatment. Clinical alternatives to prescription opioids may be underutilized as a means of treating ambulatory non-malignant pain.
INTRODUCTION
Chronic pain affects approximately 100 million adults in the United States1 and pain is the most common reason patients seek health care.2,3 The medical and lost productivity costs of chronic pain are enormous, estimated at $635 billion dollars annually.1 Over the past thirty years, a growing awareness of the prevalence and disability associated with pain has prompted a variety of initiatives to improve its identification and management.4,5,6,7
These efforts have also coincided with a sharp increase in opioid use and abuse in the United States.8,9,10,11 By 2010, approximately 5.1 million individuals’ ages 12 years and older reported current nonmedical use of pain relievers12, which has contributed to consistent increases in number of emergency department visits and deaths associated with illicit prescription opioid use.13,14 By 2008, the annual number of fatal drug poisonings surpassed those of motor vehicle deaths15 and overdose deaths attributable to prescription drugs exceeded those of cocaine and heroin combined.16
The epidemic of prescription drug abuse in the United States has renewed the challenge of appropriate identification and management of pain in ambulatory settings. Despite efforts to better identify and treat patients in pain5,6,17, campaigns to improve pain management may have unintended consequences.18,19,20,21 We examined the diagnosis and management of non-malignant pain in ambulatory settings between 2000 and 2010 using a large, nationally representative federal survey of physicians. In addition to examining secular trends, we were especially interested in whether increases in opioid utilization have been accompanied by similar increases in the use of non-opioid analgesics.
METHODS
Data
We analyzed data from the 2000–2010 National Ambulatory Medical Care Survey (NAMCS)22, a nationally representative, annual sample of outpatient office visits that provides data on patient and physicians.23 The NAMCS requests physicians and office staff to complete a one-page form for a systematic random sample of office visits that occur during a one-week period. These data include information about the physician, patient, reason for visit, diagnoses, and prescribed and over-the-counter medications. Masked sampling design variables are included to adjust for non-participation and non-response and allow for national projections.
Cohort derivation
The NAMCS patient record includes up to three patient-reported symptoms and three physician-reported diagnoses for each visit. We used medical coding software24, manual keyword searches and clinical judgment to identify visits with a primary patient self-reported symptom or physician-reported diagnosis related to pain or, in subset analyses, new musculoskeletal pain. In all analyses, we excluded individuals less than 18 years of age (19% of all visits) and those with a diagnosis of cancer from all analyses (6% of adult visits). A total of 7.8 million weighted visit records were analyzed.
Outcomes
We focused on pharmacologic treatments including opioids, non-opioids, and adjuvant therapies. We used the 2010 NAMCS survey documentation, which classifies drugs using the Multum drug ontology23, to group pharmacologic therapies into mutually exclusive subclasses. We excluded analgesic antitussives and expectorants. We used a similar approach to identify and group non-opioid pharmacologic therapies, such as non-steroidal inflammatory therapies, acetaminophen and aspirin. In some analyses, we examined the prescribing of select adjunctive therapies used to manage pain, including anti-convulsants, tricyclic anti-depressants, and in the case of musculoskeletal pain, muscle relaxants, injectable and topical treatments, and non-pharmacologic therapies such as acupuncture.
Analysis
We used descriptive statistics to compare the patient, provider and practice characteristics of patients with a primary symptom or diagnosis of pain and their counterparts. Next, we examined the prevalence of pain during each year. We then focused on patients with a new symptom or diagnosis of musculoskeletal pain, examining the proportion of patients who received different therapies. To do so, we categorized each visit as one of two (or, in the case of new musculoskeletal pain, three) types: (1) opioid visit, which we defined as any visit where an opioid was dispensed; (2) non-opioid pharmacologic visit, which we defined as any visit where a non-opioid analgesic was used without any opioid therapy; and, in the case of musculoskeletal pain, (3) non-medicine visits, which we defined as any visit where complementary and alternative or physical therapy was used regardless of any analgesic medicine.
To build our regression models, we defined our outcome as the receipt of an opioid rather than non-opioid analgesic for new musculoskeletal pain. First, we quantified the bivariate associations. We then conducted multivariate logistic regression, including variables that were basic demographic characteristics, of at least borderline statistical significance on bivariate analysis (p<0.10) or in which we had a substantive a priori interest. To examine how the likelihood of opioid receipt varied across different groups of patients, providers and visits we used the coefficients from the multivariate models to derive the predicted probability of opioid receipt for the period 2000–2002 and the period 2006–2010, calculating these at the mean levels of other variables in the models. We accounted for the complex survey design of NAMCS using study design parameters and sample weights provided by the National Center for Health Statistics. All analyses were done using SAS version 9.2.
Sensitivity Analyses
We included several analyses to assess our results under different assumptions, including: (1). examining visits with symptoms of pain separately from diagnoses of pain and including visits with secondary or tertiary symptoms or diagnoses; (2) quantifying how our findings varied when including subjects in our denominator who received a non-pharmacologic therapy for musculoskeletal pain; (3) identifying predictors of opioid utilization among all pain visits rather than new musculoskeletal visits; (4) considering the potential interaction between year of observation and several patient characteristics, including age, race and payment source; and (5) repeating analyses excluding over-the-counter medications due to potential underestimation of these drugs in the NAMCS survey.
RESULTS
Patient, provider and practice characteristics associated with visits for pain
From 2000 to 2010, approximately 20.7% of visits (1,616 of 7,802 million office visits) were associated with a primary symptom or diagnosis of pain (Table 1). Overall, patient, provider and visit characteristics were generally similar between those associated with pain and those that were not.
Table 1.
Patient and Physician Characteristics Stratified by Presence of Non-malignant Pain, 2000–2010.
| No pain symptoms or diagnosis (N=6,186 million visits) | Pain symptoms or diagnosis (N=1,616 million visits) | Total (N=7,802 million visits) | |
|---|---|---|---|
| Total visits | 79.29 | 20.71 | 100.00 |
|
| |||
| Age, % | |||
| 18–24 years | 6.85 | 6.29 | 6.73 |
| 25–44 years | 26.43 | 29.56 | 27.08 |
| 45–64 years | 34.41 | 38.63 | 35.28 |
| 65–74 years | 15.66 | 13.34 | 15.18 |
| >75 years | 16.65 | 12.18 | 15.72 |
|
| |||
| Female sex, % | 61.94 | 61.56 | 61.87 |
|
| |||
| Race/ethnicity, % | |||
| White (Non-hispanic) | 85.47 | 85.62 | 85.50 |
| Black (Non-hispanic) | 9.92 | 10.10 | 9.95 |
| Other race/ethnicity | 4.62 | 4.29 | 4.55 |
|
| |||
| Ethnicity, % | |||
| Hispanic | 9.32 | 10.41 | 9.54 |
| Non-hispanic | 90.68 | 89.59 | 90.46 |
|
| |||
| Comorbid conditions, % | |||
| None | 2.09 | 1.21 | 1.91 |
| One | 47.69 | 47.82 | 47.72 |
| Two | 26.86 | 28.09 | 27.11 |
| Three or more | 23.35 | 22.88 | 23.26 |
|
| |||
| Mental illness, % | |||
| No | 89.15 | 94.14 | 90.18 |
| Yes | 10.85 | 5.86 | 9.82 |
|
| |||
| Payment source, % | |||
| Private | 52.62 | 55.20 | 53.15 |
| Medicare | 28.84 | 23.31 | 27.70 |
| Medicaid | 6.22 | 6.66 | 6.31 |
| Self Pay | 4.89 | 4.10 | 4.73 |
| Other payment source | 7.43 | 10.73 | 8.11 |
|
| |||
| Type of provider(s) seen at visit, % | |||
| Physician | 95.99 | 96.89 | 96.17 |
| Physician assistant | 3.42 | 3.79 | 3.50 |
| Nurse | 22.45 | 21.00 | 22.15 |
| Other provider type | 10.63 | 9.95 | 10.49 |
|
| |||
| Physician Specialty, % | |||
| General/Family Practice | 24.05 | 32.17 | 25.73 |
| Internal Medicine | 18.73 | 21.38 | 19.28 |
| Surgeon | 19.01 | 20.61 | 19.34 |
| Neurologist | 1.23 | 3.22 | 1.64 |
| Other specialty | 36.98 | 22.62 | 34.01 |
|
| |||
| Type of Physician, % | |||
| Allopathic (MD) | 92.74 | 89.14 | 92.00 |
|
| |||
| Time Spent with physician, minutes | 19.46±0.21 | 19.36±0.15 | 19.44±0.18 |
|
| |||
| Patient new to physician, % | 52.32 | 47.26 | 51.27 |
|
| |||
| Patient new to practice, % | 12.04 | 16.52 | 12.97 |
|
| |||
| Region, % | |||
| Northeast | 19.74 | 20.12 | 19.82 |
| Midwest | 21.75 | 22.44 | 21.89 |
| South | 37.38 | 35.87 | 37.07 |
| West | 21.13 | 21.58 | 21.23 |
Source: National Ambulatory Medical Care Survey, 2000–2010
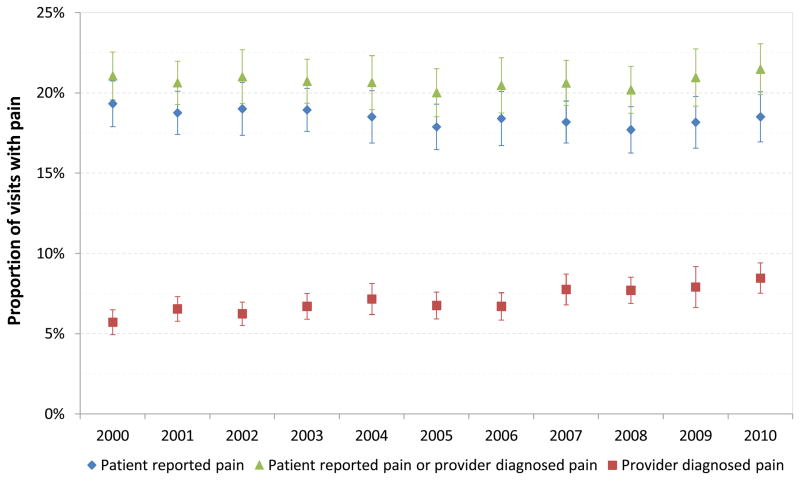
Trends in patient symptoms and provider diagnoses of pain
Absolute rates of reported pain as a primary symptom or diagnosis fluctuated less than 2% during the period examined and consistently represented approximately one-fifth of visits (Figure 1). Rates of pain including cases where it was reported as a secondary or tertiary symptom or diagnosis were somewhat greater (Appendix Table 1). Patient-reported pain as a primary symptom was consistently approximately 17% to 19% of visits, whereas provider reported pain increased nearly 50% from 2000 (5.7% of visits with pain as a primary diagnosis, 95% confidence intervals [CI] 4.96%–6.49%) to 2010 (8.5%, CI 7.53%–9.42%). Musculoskeletal pain represented about half of all non-malignant pain visits from 2000 through 2010.
Figure 1.
Ambulatory prevalence of patient and provider reported non-malignant pain in the United States, 2000-2010.
Source: National Ambulatory Medical Care Survey, 2000-2010
Appendix Table 1.
National trends in provider and patient reported non-malignant pain, 2000–2010.
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pain reported from patient or provider | |||||||||||
| As primary code, % | 21.06 | 20.63 | 21.01 | 20.73 | 20.65 | 20.02 | 20.47 | 20.62 | 20.20 | 20.97 | 21.48 |
| As any code, % | 27.61 | 27.36 | 27.75 | 27.72 | 27.25 | 26.42 | 27.63 | 27.63 | 27.08 | 28.65 | 28.87 |
|
| |||||||||||
| Provider reported pain | |||||||||||
| As primary diagnosis, % | 5.72 | 6.55 | 6.25 | 6.71 | 7.17 | 6.77 | 6.71 | 7.76 | 7.71 | 7.91 | 8.47 |
| As any diagnosis, % | 8.61 | 9.76 | 9.74 | 10.03 | 10.87 | 10.23 | 10.54 | 11.71 | 11.65 | 12.70 | 12.78 |
|
| |||||||||||
| Patient reported pain | |||||||||||
| As primary symptom, % | 19.33 | 18.76 | 19.01 | 18.95 | 18.51 | 17.89 | 18.41 | 18.19 | 17.71 | 18.17 | 18.51 |
| As any symptom, % | 25.14 | 24.70 | 24.66 | 25.09 | 23.99 | 23.44 | 24.29 | 24.12 | 23.42 | 24.64 | 24.73 |
|
| |||||||||||
| Musculoskeletal pain reported from patient or provider | |||||||||||
| As primary code, % | 10.02 | 10.77 | 10.49 | 10.41 | 11.14 | 10.40 | 10.43 | 10.84 | 10.18 | 10.86 | 11.48 |
| As any code, % | 12.93 | 13.57 | 13.70 | 13.55 | 14.28 | 13.21 | 13.43 | 14.26 | 13.55 | 14.11 | 14.74 |
|
| |||||||||||
| Provider reported musculoskeletal pain | |||||||||||
| As primary diagnosis, % | 2.19 | 2.93 | 2.51 | 2.85 | 3.12 | 3.07 | 2.93 | 3.24 | 3.18 | 3.36 | 4.13 |
| As any diagnosis, % | 3.39 | 4.12 | 4.13 | 4.29 | 4.81 | 4.64 | 4.63 | 5.15 | 5.28 | 5.30 | 6.07 |
|
| |||||||||||
| Patient reported musculoskeletal pain | |||||||||||
| As primary diagnosis, % | 9.32 | 9.90 | 9.63 | 9.81 | 10.17 | 9.48 | 9.52 | 9.86 | 9.19 | 9.69 | 10.02 |
| As any diagnosis, % | 11.89 | 12.36 | 12.07 | 12.50 | 12.83 | 11.91 | 11.95 | 12.75 | 11.71 | 12.49 | 12.89 |
Source: National Ambulatory Medical Care Survey, 2000–2010
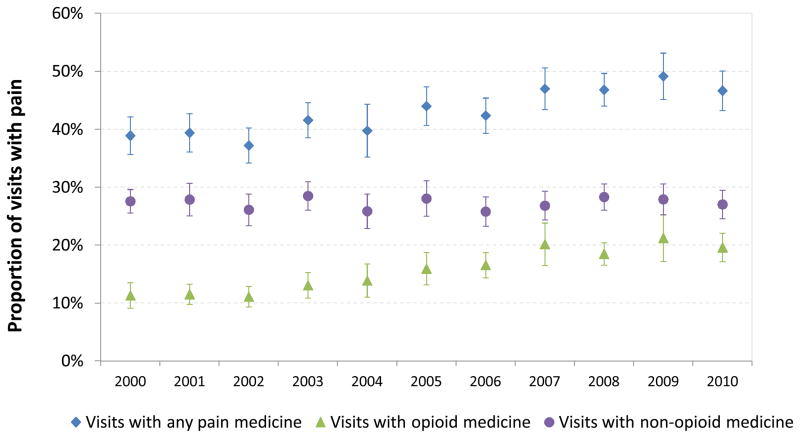
Pharmacologic treatment of pain
Figure 2 and Appendix Table 2 depict the prevalence and treatment of pain among patient visits from 2000 through 2010. In 2000, there were 130 million patient visits where pain was either a primary symptom or diagnosis, and of these, opioids were prescribed in 11% (CI 9.11%–13.53%), while approximately 60% (CI 57.86%–64.33%) had no pharmacologic treatment. There were modest declines in the proportion of visits with no pharmacologic pain treatment from 2000 (61.10% of visits) to 2010 (53.35% of visits).
Figure 2.
Ambulatory treatment of non-malignant pain with opioid and non-opioid analgesics in the United States, 2000-2010.
Source: National Ambulatory Medical Care Survey, 2000-2010
Appendix Table 2.
Trends in treatment of non-malignant pain among ambulatory visits in the United States, 2000–2010.*
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| All pain visits | |||||||||||
| Treated with pain medicines** | 38.90 | 39.40 | 37.22 | 41.58 | 39.76 | 43.99 | 42.37 | 46.99 | 46.82 | 49.15 | 46.65 |
| No pharmacotherapy | 61.10 | 60.60 | 62.78 | 58.42 | 60.24 | 56.01 | 57.63 | 53.01 | 53.18 | 50.85 | 53.35 |
|
| |||||||||||
| Visits treated with opioids | 11.32 | 11.53 | 11.10 | 13.08 | 13.90 | 15.94 | 16.56 | 20.17 | 18.51 | 21.24 | 19.61 |
| Fixed-dose combination visits | 8.80 | 9.31 | 9.59 | 10.76 | 10.72 | 11.77 | 12.05 | 14.54 | 13.02 | 15.23 | 14.01 |
| Opioid only visits | 2.87 | 2.63 | 1.88 | 2.94 | 4.14 | 5.30 | 5.58 | 7.46 | 6.73 | 8.10 | 6.68 |
| NSAIDs visits | 3.72 | 3.22 | 3.10 | 4.78 | 4.41 | 4.24 | 4.39 | 4.41 | 5.33 | 5.40 | 5.16 |
| Acetaminophen visits | .48 | .19 | .34 | .33 | .26 | .50 | .39 | .61 | .81 | .57 | .62 |
| Adjunctive treatment visits | 2.90 | 3.34 | 3.70 | 4.25 | 4.83 | 4.73 | 4.87 | 7.29 | 6.70 | 8.76 | 7.14 |
|
| |||||||||||
| Visits treated with non-opioids only | 27.58 | 27.87 | 26.11 | 28.50 | 25.86 | 28.05 | 25.80 | 26.82 | 28.31 | 27.90 | 27.04 |
| NSAIDs visits | 21.37 | 21.36 | 19.80 | 20.74 | 18.75 | 19.96 | 18.70 | 18.49 | 19.40 | 19.39 | 19.57 |
| Acetaminophen visits | 2.69 | 2.65 | 3.42 | 3.63 | 3.06 | 3.72 | 2.81 | 3.41 | 3.62 | 3.57 | 3.07 |
| Adjunctive treatment visits | 6.79 | 7.79 | 6.63 | 8.51 | 8.19 | 8.81 | 8.90 | 9.80 | 10.18 | 9.79 | 9.51 |
|
| |||||||||||
| Total visits | |||||||||||
| Opioid (millions), N | 14.7 | 16.1 | 15.6 | 18.9 | 19.7 | 23.1 | 23.0 | 21.1 | 27.6 | 35.9 | 32.1 |
| Non-opioids only (millions), N | 35.8 | 38.8 | 36.7 | 41.2 | 36.7 | 40.6 | 35.8 | 41.4 | 42.3 | 47.2 | 44.2 |
| No pharmacotherapy (millions), N | 79.3 | 84.5 | 88.2 | 84.5 | 85.4 | 81.1 | 80.0 | 81.8 | 79.4 | 86.0 | 87.3 |
|
| |||||||||||
| All pain visits (millions), N | 129.8 | 139.4 | 140.5 | 144.6 | 141.8 | 144.9 | 138.8 | 154.3 | 149.4 | 169.1 | 163.6 |
Except where otherwise indicated values represent column percents;
Pain medicines include opioids, non-steroidal anti-inflammatory agents (NSAIDs), acetaminophen, and adjunctive treatments (gabapentin, pregabalin, tricyclic antidepressants, local injectable anesthetics, muscle relaxants and topical therapies)
Source: National Ambulatory Medical Care Survey, 2000–2010
Over the period examined, two-fifths to one-half (40%–50%) of pain visits were associated with an analgesic use. Although rates of opioid use increased 73% from 11.3% of visits (2000) to 19.6% of visits (2010), prescribing rates of non-opioid pharmacotherapies remained relatively constant (26%–29%). In 2010, the final year of observation, of 164 million pain visits, approximately one-half (47%; 43.24%–50.06%) were treated with a pain medicine, one-fifth with an opioid (20%; 17.17%–22.06%), and one-quarter (27%; 24.59%–29.49%) with a non-opioid pharmacotherapy such as an NSAID, acetaminophen or adjuvant therapy.
The concomitant use of opioids with non-opioids analgesics increased during the time period examined. Among all pain visits, opioid with NSAID prescribing increased 39%, from 3.7% of visits (2000) to 5.2% of visits (2010). There were also increases in use of acetaminophen (from 0.5% to 0.6% of visits) and adjunctive therapies (from 2.9% to 7.1% of visits) with opioids, though patients receiving these combinations of therapies still represented a small proportion of all pain visits.
Pharmacological treatment of new musculoskeletal pain
From 2000 to 2010, ambulatory care visits where new musculoskeletal pain was either a primary symptom or diagnosis increased from 62 million visits to 87 million visits (Table 2). Approximately one-half of visits in a given year were treated with analgesics. During 2005–2010, the years that information regarding non-pharmacologic treatments such as complementary and alternative therapies was available, such treatments were used among 13–18% of visits.
Table 2.
Trends in pharmacologic treatment among visits for musculoskeletal pain, 2000–2010.*
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| All visits | |||||||||||
| Treated with pain medicines** | 52.65 | 49.90 | 46.47 | 51.71 | 46.60 | 51.88 | 50.83 | 54.77 | 53.85 | 54.74 | 53.44 |
| Treated with non-medicines | --- | --- | --- | --- | --- | 15.80 | 15.41 | 13.38 | 15.39 | 17.35 | 18.23 |
| No pharmacotherapy | --- | --- | --- | --- | --- | 39.52 | 42.51 | 37.45 | 39.28 | 37.23 | 37.29 |
|
| |||||||||||
| Visits treated with opioids | 15.08 | 15.18 | 15.99 | 17.98 | 18.43 | 21.15 | 22.33 | 27.19 | 24.11 | 26.78 | 24.43 |
| Fixed-dose combination visits | 12.31 | 12.13 | 14.09 | 15.07 | 14.80 | 16.18 | 16.87 | 20.68 | 17.61 | 20.04 | 17.88 |
| Opioid only visits | 3.10 | 3.58 | 2.45 | 3.61 | 5.04 | 6.73 | 6.96 | 8.85 | 8.05 | 9.42 | 8.10 |
| NSAIDs visits | 6.18 | 3.81 | 5.36 | 7.17 | 6.74 | 6.05 | 6.40 | 6.50 | 7.34 | 7.00 | 7.18 |
| Acetaminophen visits | .39 | 0.12 | .41 | .45 | .37 | .74 | .45 | .75 | .57 | 0.53 | .56 |
| Muscle relaxants, injectables, or topical | 3.50 | 3.92 | 5.07 | 5.73 | 6.32 | 5.70 | 6.16 | 7.85 | 7.39 | 9.91 | 7.90 |
|
| |||||||||||
| Visits treated with non-opioids only | 37.57 | 33.72 | 30.48 | 33.72 | 28.17 | 30.74 | 28.50 | 27.58 | 29.73 | 27.96 | 29.01 |
| NSAIDs visits | 32.23 | 27.08 | 24.86 | 36.60 | 23.18 | 24.18 | 22.19 | 20.90 | 23.10 | 21.19 | 23.00 |
| Acetaminophen visits | 2.17 | 3.15 | 1.79 | 2.31 | 2.02 | 2.85 | 2.16 | 2.64 | 3.11 | 2.83 | 1.90 |
| Muscle relaxants, injectables, or topical | 7.71 | 8.50 | 7.69 | 10.29 | 8.27 | 7.75 | 10.04 | 9.27 | 9.04 | 9.12 | 8.78 |
|
| |||||||||||
| Total visits | |||||||||||
| Opioid (millions), N | 9.3 | 11.0 | 11.2 | 13.1 | 14.1 | 15.9 | 15.8 | 22.1 | 18.1 | 23.4 | 21.4 |
| Non-opioids only (millions), N | 23.2 | 24.5 | 21.4 | 24.5 | 21.5 | 23.1 | 20.2 | 22.4 | 22.4 | 24.5 | 25.4 |
| No pharmacotherapy (millions), N | 28.6 | 37.1 | 37.5 | 35.1 | 40.1 | 29.7 | 30.1 | 30.4 | 29.6 | 32.6 | 32.6 |
|
| |||||||||||
| Total pain visits (millions), N | 61.8 | 72.7 | 70.1 | 72.6 | 76.5 | 75.3 | 70.7 | 81.1 | 75.3 | 87.5 | 87.4 |
Except where otherwise indicated values represent column percents;
Pain medicines include opioids, non-steroidal anti-inflammatory agents (NSAIDs), acetaminophen, muscle relaxants, local injectable anesthetics, and topical therapies; Elipses indicate years where data is unavailable
Source: National Ambulatory Medical Care Survey, 2000–2010
Although opioid prescribing increased 62% from 15.1% (CI 11.77%–18.39%) of visits (2000) to 24.4% (CI 20.80%–28.04%) of visits (2010), the prescribing of non-opioid medications for musculoskeletal pain visits decreased from 38% (CI 34.09%–41.06%) of visits in 2000 to 29% (CI 25.55%–32.48%%) of visits in 2010. These declines were primarily driven by reductions in the use of NSAIDs.
Patient, provider and practice characteristics associated with non-opioid use
Few patient, practice and physician characteristics were associated with the likelihood of receiving an opioid versus a non-opioid analgesic for a new primary symptom or diagnosis of musculoskeletal pain. For example, on bivariate analysis, rates of opioid receipt were similar among subjects of different ages, nor did opioid receipt differ based on patients’ sex, number of comorbid conditions, or whether the patient was new to the practice or physician. On multivariate analysis, the likelihood of opioid receipt was lower among older patients, Hispanics, those on fewer medicines, individuals with a private insurance, and those who whose self-identified race was neither White nor Black, as compared with their counterparts (Table 3). Over the period examined, increases in opioid use generally occurred non-selectively rather than being concentrated in particular subpopulations of visits.
Table 3.
Multivariate association between patient, physician and practice characteristics and opioid receipt for new musculoskeletal pain.
| Predicted probability of opioid receipt | ||||
|---|---|---|---|---|
|
|
||||
| Odds ratio | 95% Confidence Intervals | 2000–2002 | 2006–2010 | |
| PATIENT CHARACTERISTICS
| ||||
| Age, years | ||||
| 18–24 | 1.11 | 0.79–1.57 | 0.33 (0.26–0.41) | 0.39 (0.31–0.47) |
| 25–44 | 1.12 | 0.92–1.38 | 0.33 (0.29–0.38) | 0.39 (0.35–0.43) |
| 45–64 | REF | REF | 0.31 (0.27–0.35) | 0.36 (0.32–0.40) |
| 65–74 | 0.63 | 0.45–0.87 | 0.22 (0.17–0.28) | 0.26 (0.21–0.33) |
| 75 or more | 0.59 | 0.43–0.81 | 0.21 (0.16–0.26) | 0.25 (0.20–0.31) |
|
| ||||
| Sex | ||||
| Male | REF | REF | 0.30 (0.26–0.35) | 0.35 (0.32–0.39) |
| Female | 0.94 | 0.79–1.12 | 0.29 (0.26–0.32) | 0.34 (0.31–0.37) |
|
| ||||
| Race/ethnicity | ||||
| White | REF | REF | 0.30 (0.27–0.34) | 0.35 (0.32–0.39) |
| Black | 0.90 | 0.70–1.15 | 0.28 (0.23–0.34) | 0.33 (0.28–0.39) |
| Other | 0.51 | 0.30–0.88 | 0.18 (0.11–0.28) | 0.22 (0.14–0.32) |
|
| ||||
| Ethnicity | ||||
| Hispanic | 0.75 | 0.57–0.98 | 0.24 (0.19–0.30) | 0.29 (0.24–0.35) |
| Non-Hispanic | REF | REF | 0.30 (0.27–0.34) | 0.35 (0.32–0.38) |
|
| ||||
| Number of medications | ||||
| One | 0.33 | 0.26–0.42 | 0.18 (0.15–0.21) | 0.21 (0.18–0.25) |
| Two | 0.76 | 0.62–0.94 | 0.33 (0.29–0.38) | 0.38 (0.34–0.43) |
| Three | 1.05 | 0.82–1.34 | 0.41 (0.35–0.47) | 0.46 (0.41–0.52) |
| Four or more | REF | REF | 0.39 (0.34–0.45) | 0.45 (0.41–0.49) |
|
| ||||
| PROVIDER CHARACTERISTICS
| ||||
| Type of provider(s) seen at visit | ||||
| Non-nurse | REF | REF | 0.30 (0.26–0.33) | 0.35 (0.32–0.38) |
| Nurse | 0.98 | 0.81–1.19 | 0.29 (0.25–0.34) | 0.34 (0.30–0.39) |
|
| ||||
| VISIT CHARACTERISTICS
| ||||
| Payment Source | ||||
| Private | REF | REF | 0.27 (0.24–0.31) | 0.31 (0.28–0.34) |
| Medicare | 1.62 | 1.19–2.20 | 0.38 (0.30–0.46) | 0.42 (0.36–0.48) |
| Medicaid | 1.46 | 1.08–1.99 | 0.35 (0.28–0.44) | 0.39 (0.32–0.47) |
| Self-Pay | 1.70 | 1.20–2.41 | 0.39 (0.31–0.48) | 0.43 (0.35–0.52) |
| Other | 1.39 | 1.08–1.79 | 0.34 (0.28–0.41) | 0.38 (0.32–0.44) |
|
| ||||
| Year | ||||
| 2000–2002 | 0.79 | 0.64–0.98 | 0.29 (0.26–0.33) | |
| 2003–2005 | 0.86 | 0.68–1.08 | 0.31 (0.27–0.36) | |
| 2005–2010 | REF | REF | 0.35 (0.32–0.38) | |
Source: National Ambulatory Medical Care Survey, 2000–2010
Bold denotes statistical significance at p<.05
Sensitivity analyses
Sensitivity analyses supported our analytic approach and the robustness of our results. Although the prevalence of pain was greater when examining subjects with a postoperative visit or with any symptom rather than a primary symptom or diagnosis of pain, the substantive results and their interpretation were unchanged. Multivariate analyses including subjects in our denominator who received a non-pharmacologic therapy for musculoskeletal pain also yielded substantively similar results, as did models that examined all subjects with pain rather than those with new musculoskeletal pain. In most cases, the year of observation did not modify the independent association between these patient characteristics and the likelihood of opioid receipt, and interactions terms were excluded from the final model. Finally, in analyses that excluded over-the-counter medications from analysis due to their potential for systematic under capture and the differential impact of this over the period examined, our results showed even larger decreases in NSAIDs prescribing for all pain and new musculoskeletal pain.
DISCUSSION
Using nationally representative data on ambulatory practice in the United States, the overall prevalence of patient-reported pain has not changed during the past decade, although providers’ diagnoses of pain as a primary complaint nearly doubled. Despite large increases in opioid use, there were not similar increases in the prescribing of alternative analgesics, such as non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen and other therapies that may serve as alternatives to prescription opioids. These results are important given epidemic rates of prescription opioid abuse that have occurred in the context of efforts to improve the identification and treatment of non-malignant pain. While escalating opioid utilization has been well described11,13, 25 our analyses represent some of the most comprehensive to date examining trends in the ambulatory diagnosis and treatment of pain.
Our findings have implications for patients, providers and policy-makers and highlight the need for more evidence demonstrating the safety and effectiveness of opioid compared to other analgesics. Despite greater recognition of pain by providers and a remarkable increase in opioid prescribing, there was no commensurate increase in the prescribing of non-opioid therapies. This is particularly important because of the variety of alternative pharmacologic treatments available to treat non-malignant pain, including selective and non-selective non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, some anti-convulsants, tricyclic anti-depressants, and in the case of musculoskeletal pain, muscle relaxants, topical analgesics and local injections.1,26 The removal of rofecoxib from the market in 2004 may have increased providers’ awareness of adverse events related to NSAIDs, and thus contributed to the decreases in NSAID use for the treatment of musculoskeletal pain. However, there is little evidence to support any greater safety or effectiveness of opioids over many of these alternative analgesics, particularly with respect to functional outcomes and longer term use.27 Indeed, despite large escalations in clinical adoption, trials of opioids have generally been placebo-controlled, examined only short-term outcomes and excluded patients with a history of substance abuse, depression or other mental illness.28 Although our results suggest the need for greater evidence about the comparative effectiveness of opioids and alternative treatments29, clinicians and policy-makers should use caution in extrapolating the findings of the current evidence regarding opioids to clinical populations that differ considerably from the contexts in which they have been most studied.
In multivariate analyses, some patient or visits characteristics were associated with the likelihood of opioid receipt rather than non-opioid analgesic receipt for new musculoskeletal pain. Despite this, the overall clinical and policy magnitude of these differences was modest, findings which persisted when examining all pain rather than new musculoskeletal pain. In addition, we found that in general, increases in opioid use have occurred non-selectively, rather than being focused within a particular group of patients, clinicians, or types of office visits.
While approximately one-fifth of office visits were associated with a primary symptom or diagnosis of pain, there were large increases in the total number of ambulatory pain visits, from 616 million in 2000 to 761 million in 2010. We also found an approximate 50% increase in provider diagnoses of pain, which may reflect the impact of campaigns such as the “Pain as the fifth vital sign” initiative30,31 and the World Health Organization pain ladder32, as well as an increasing number of therapies that have been marketed and promoted for its treatment. Nevertheless, there is still considerable discordance between patient and provider reports of pain, which may be due to a variety of factors, such as clinicians’ tendency to diagnose underlying causes of pain rather than pain itself1, and is worthy of further investigation. This discordance, as well as the large proportion of pain visits that did not result in analgesic use, are both worthy of further study, though neither should be used alone to infer insufficient pain treatment. For example, a prospective observational study of pain-related visits in the emergency department setting yielded results suggesting approximately one-half of patients may not desire pharmacological analgesia.33
Our study has several important limitations. First, although the NAMCS is uniquely well suited for the current analysis, its cross-sectional structure excludes some information of interest such as indication, pain chronicity, dosing, drug intolerance, treatment failures and health outcomes, which limits our ability to judge the quality of pain management among these patients. Second, the NAMCS data may underestimate provider mentions of some over-the-counter therapies such as acetaminophen, however prior analyses have demonstrated that the NAMCS captures a substantial proportion of these drug mentions.34 Such under capture would primarily be of concern if it was systematically impacted by secular changes such as the market withdrawal of rofecoxib in 2004, however, our sensitivity analyses suggested substantive findings when excluding over-the-counter therapies from analysis. Finally, there are additional adjunctive pharmacological therapies (e.g. selective serotonin reuptake inhibitors, beta-blockers, anti-convulsants, steroids) that may be prescribed off-label to treat pain; we conservatively excluded most of these therapies from our primary analyses because they are also used for a variety of non-analgesic indications.
CONCLUSION
Many factors contribute to the complexity of the epidemic of prescription opioid abuse and diversion. One is that historically, pain has been undertreated in some settings. Despite this, our data suggest that the rapidly rising rates of opioid use have not been accompanied by increases in the proportion of ambulatory pain patients receiving pharmacologic treatment, nor have large increases in the ambulatory prescribing of opioids been accompanied by similar increases in the prescribing of non-opioid analgesics. Policy-makers, professional organizations, and providers should reevaluate prior efforts to improve the identification, treatment and management of non-malignant pain and promote approaches that adequately reflect the importance of non-opioid and non-pharmacologic treatments.
Supplementary Material
Acknowledgments
Support
Dr. Alexander is supported by the Agency for Healthcare Research and Quality (RO1 HS0189960). These funding sources had no role in the design and conduct of the study, analysis or interpretation of the data; and preparation or final approval of the manuscript prior to publication.
Footnotes
Disclosures
Dr Alexander is an ad hoc member of the FDA’s Drug Safety and Risk Management Advisory Committee, serves as a paid consultant to IMS Health, and serves on an IMS Health scientific advisory board. This arrangement has been reviewed and approved by the Johns Hopkins University in accordance with its conflict of interest policies. Dr. Kruszewski has served as general and case-specific expert for multiple plaintiff litigation involving OxyContin, Neurontin and Zyprexa and has had false claims settled as co-plaintiff with the United States against Southwood Psychiatric Hospital, Pfizer (Geodon) and AstraZeneca (Seroquel).
COMPLETE AUTHOR INFORMATION
| Matthew Daubresse, MHS Johns Hopkins Bloomberg School of Public Health Department of Epidemiology 615 N. Wolfe Street W6023 Baltimore, MD 21205 Phone: 410 955 9052; Fax:410 955 0863 Email: mdaubres@jhsph.edu |
Nilay D. Shah, PhD Mayo Clinic Division of Health Care Policy and Research 200 First Street SW Rochester, MN 55905 Phone: 507 266 7890; Fax: 507 266 7890 Email: Shah.Nilay@mayo.edu |
| Hsien-Yen Chang, PhD Johns Hopkins Bloomberg School of Public Health Department of Health Policy and Management 624 N. Broadway Street Baltimore, Maryland 21205 Phone: 410 614 5812; Fax: 410 955 0863 Email: hchang2@jhsph.edu |
Randall S. Stafford MD, PhD Stanford Prevention Research Center Stanford University 1265 Welch Road Palo Alto, CA 94305-5411 Phone: 650 724 2400; Fax: 650 725 6906 Email: rstafford@stanford.edu |
| Yuping Yu, PharmD Johns Hopkins Bloomberg School of Public Health Center for Drug Safety and Effectiveness 615 N. Wolfe Street W6035 Baltimore, MD 21205 Phone: 410 955 8168; Fax: 410 955 0863 Email: yupingph@yahoo.com |
Stefan P. Kruszewski Stefan P. Kruszewski, M.D. & Associates 133 Linglestown Road Harrisburg, Pennsylvania 17110 Phone: 717 234 2684 Fax: 717 234 2686 Email: SKruszewski@spkmd.com |
| Shilpa Viswanathan, MS Johns Hopkins Bloomberg School of Public Health Department of Epidemiology 615 N. Wolfe Street W6023 Baltimore, MD 21205 Phone: 410 512 0014; Fax: 410 955 0863 Email: sviswana@jhsph.edu |
G. Caleb Alexander, MD, MS Johns Hopkins Bloomberg School of Public Health Department of Epidemiology 615 N. Wolfe Street W6035 Baltimore, MD 21205 Phone: 410 955 8168; Fax:410 955 0863 Email: galexand@jhsph.edu |
References
- 1.IOM (Institute of Medicine) Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 2.Fox CD, Berger D, Fine PG, et al. A position statement from the American Pain Society. Glenview, IL: American Pain Society; 2000. Pain assessment and treatment in the managed care environment. [DOI] [PubMed] [Google Scholar]
- 3.McCarberg BH. Pain management in primary care: strategies to mitigate opioid misuse, abuse, and diversion. Postgrad Med. 2011;123:119–30. doi: 10.3810/pgm.2011.03.2270. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Agency for Health Care Policy and Research. Acute Pain Management: Operative or Medical Procedures and Trauma. (AHCPR Pub. No. 92-0032) Rockville, MD: U.S. Department of Health and Human Services; 1992. [Google Scholar]
- 5.American Pain Society. Principles of Analgesic Use in the Treatment of Acute Pain and Cancer Pain. Vol. 4. Glenview, IL: American Pain Society; 1999. [Google Scholar]
- 6.American Pain Society Quality of Care Committee. Quality improvement guidelines for the treatment of acute pain and cancer pain. JAMA. 1995;274:1874–80. doi: 10.1001/jama.1995.03530230060032. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. [Accessed January 2, 2013];WHO’s Pain Relief Ladder. 2009 Available at: www.who.int/cancer/palliative/painladder/en/
- 8.Sullivan MD, Edlund MJ, Fan MY, DeVries A, Braden JB, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000–2005 in Commercial and Medicaid insurance plans: The TROUP study. Pain. 2008;138:440–449. doi: 10.1016/j.pain.2008.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martell BA, O’Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, Fiellin DA. Systematic Review: Opioid Treatment for Chronic Back Pain: Prevalence, Efficacy, and Associations with Addiction. Annals of Internal Medicine. 2007;146:116–27. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 10.Chou R, Clark E, Helfand M. Comparative Efficacy and Safety of Long-Acting Oral Opioids for Chronic Non-Cancer Pain: A systematic review. Journal of Pain and Symptom Management. 2003;26:1026–48. doi: 10.1016/j.jpainsymman.2003.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Manchikanti L, Singh A. Therapeutic opioids: A ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician. 2008;11:S63–S88. [PubMed] [Google Scholar]
- 12.Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-41, HHS Publication No. (SMA) 11-4658. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011. [Google Scholar]
- 13.Alexander GC, Kruszewski SP, Webster DW. Rethinking Opioid Prescribing to Protect Patient Safety and Public Health. JAMA. 2012;308:1865–1866. doi: 10.1001/jama.2012.14282. [DOI] [PubMed] [Google Scholar]
- 14.Manchikanti L, Fellows B, Ailinani H, Pampati V. Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain Physician. 2010;13(5):401–435. [PubMed] [Google Scholar]
- 15.Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. [Accessed January 2, 2013];NCHS Data Brief. 2011 (81):1–8. Available at: http://www.cdc.gov/nchs/data/databriefs/db81.pdf. [PubMed]
- 16.CDC. Vital Signs: Overdoses of Prescription Opioid Pain Relievers—United States, 1999–2008. [Accessed January 2, 2013];MMWR. 2011 60:1–6. Available at : http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm?s_cid=mm6043a4_w. [PubMed] [Google Scholar]
- 17.Kalso E, Allan L, Dellemijn PL, Faura CC, Illias WK, Jensen TS, Perrot S, Plaghki LW, Zenz M. Recommendations for using opioids in chronic non-cancer pain. European Journal of Pain. 2003;7:381–386. doi: 10.1016/S1090-3801(02)00143-X. [DOI] [PubMed] [Google Scholar]
- 18.Mularski RA, et al. Measuring Pain as the 5th vital sign does not improve pain management. Journal of general internal medicine. 2006;21:607–612. doi: 10.1111/j.1525-1497.2006.00415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lucas Charles E, Vlahos Angie L, Ledgerwood Anna M. Kindness Kills: The Negative Impact of Pain as the Fifth Vital Sign. Journal of the American College of Surgeons, Volume. 2007;205:101–107. doi: 10.1016/j.jamcollsurg.2007.01.062. [DOI] [PubMed] [Google Scholar]
- 20.Lorenz KA, Sherbourne CD, Shugarman LV, Rubenstein LW, Cohen A, Goebel JR, Hagenmeier E, Simon B, Lanto A, Asch SM. How Reliable in Pain as the fifth vital sign? J Am Board Fam Med. 2009;22:291–298. doi: 10.3122/jabfm.2009.03.080162. [DOI] [PubMed] [Google Scholar]
- 21.Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs. 2000. Pain. 2004;109:514–519. doi: 10.1016/j.pain.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Hsiao CJ, Cherry DK, Beatty PC, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2007 summary. National Health Statistics Report. 2010;3:1–32. [PubMed] [Google Scholar]
- 23.NCHS. [Accessed January 2, 2013];NAMCS 2010 Micro-data file documentation. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc2010.pdf.
- 24. [Accessed January 2, 2013];Flash Code Medical Coding Software. Available at: http://flashcode.com.
- 25.Olsen Y, Daumit GL, Ford DE. Opioid prescriptions by U.S. primary care physicians from 1992 to 2001. J Pain. 2006;7:225–35. doi: 10.1016/j.jpain.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 26.Turk DC, Wilson HD, Cahana A. Treatment of chronic non-cancer pain. Lancet. 2011;377:2226–2235. doi: 10.1016/S0140-6736(11)60402-9. [DOI] [PubMed] [Google Scholar]
- 27.Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E. Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ. 2006;174:1589–1594. doi: 10.1503/cmaj.051528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grady D, Berkowitz SA, Katz MH. Opioids for Chronic Pain. Arch Intern Med. 2011;171:1426–1427. doi: 10.1001/archinternmed.2011.213. [DOI] [PubMed] [Google Scholar]
- 29.Alexander GC, Stafford RS. Does comparative effectiveness have a comparative edge? JAMA. 2009;301:2488–2490. doi: 10.1001/jama.2009.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Pain Society. Principles of Analgesic Use in the Treatment of Acute Pain and Cancer Pain. Vol. 4. Glenview, IL: American Pain Society; 1999. [Google Scholar]
- 31.American Pain Society Quality of Care Committee. Quality improvement guidelines for the treatment of acute pain and cancer pain. JAMA. 1995;274:1874–80. doi: 10.1001/jama.1995.03530230060032. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization. WHO’s Pain Relief Ladder. 2009 www.who.int/cancer/palliative/painladder/en/
- 33.Singer AJ, Garra G, Chohan JK, Dalmedo C, Thode HC., Jr Triage pain scores and the desire for and use of analgesics. Ann Emerg Med. 2008;52:689–95. doi: 10.1016/j.annemergmed.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 34.Stafford RS. Aspirin use is low among United States outpatients with coronary artery disease. Circulation. 2000;101:1097–1101. doi: 10.1161/01.cir.101.10.1097. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.