Abstract
The female sex is traditionally considered a favorable prognostic factor for nasopharyngeal carcinoma (NPC). However, no particular study has reported this phenomenon. To explore the prognostic impact of gender on patients with NPC after definitive radiotherapy, we reviewed the clinical data of 2063 consecutive patients treated between 1st January 2000 and 31st December 2003 in the Sun Yat-sen University Cancer Center. The median follow-up for the whole series was 81 months. The female and male patients with early stage disease comprised 49.4% and 28.1% of the patient population, respectively. Both the 5-year overall survival (OS) and disease-specific survival (DSS) rates of female patients were significantly higher than those of male patients (OS: 79% vs. 69%, P < 0.001; DSS: 81% vs. 70%, P < 0.001). For patients with locoregionally advanced NPC, the 5-year OS and DSS rates of female vs. male patients were 74% vs. 63% (P < 0.001) and 76% vs. 64%, respectively (P < 0.001). A multivariate analysis showed that gender, age, and TNM stage were independent prognostic factors for the 5-year OS and DSS of NPC patients. The favorable prognosis of female patients is not only attributed to the early diagnosis and treatment but might also be attributed to some intrinsic factors of female patients.
Keywords: Nasopharyngeal carcinoma, female, prognosis, radiotherapy
Nasopharyngeal carcinoma (NPC) is a leading malignancy of the head and neck in southern China. NPC has an annual incidence as high as 25–50 per 100,000[1]. However, NPC differs from other head and neck carcinomas in terms of its high rate of distant metastasis, undifferentiated histology, radiosensitivity, and chemosensitivity[2]. Due to the deep-seated location of the nasopharynx, 60%–70% of patients present with loco-regionally advanced disease at diagnosis. Radiotherapy is the mainstay treatment for NPC[3],[4]. The 5-year overall survival (OS) rate for patients with early stage (I + II) disease is approximately 80%–90% with radiotherapy alone[5] but drops to 37%–59% for patients with loco-regionally advanced (III + IV) disease[6],[7]. Over the past 2 decades, attempts have been made to improve the prognosis of NPC patients by combining chemotherapy with radiotherapy[8]. As a result of this combined treatment modality, a 6% survival benefit has been gained for locoregionally advanced disease, resulting in an improved 5-year OS rate (65%–75% ) for NPC patients[3],[9]–[11].
Prognostic factors for NPC have been reported in many studies. The impact of the primary and nodal stage on survival is well established. In addition, many reports have shown controversial results with regard to the prognostic impact of gender. Larger series from the Surveillance, Epidemiology, and End Results (SEER) database or the EUROCARE database revealed that there was a borderline or no significant difference between female and male NPC patients in OS (performed by multivariate analysis)[12],[13]. However, female gender was reported as a favorable factor for OS in some Chinese series. Lee et al.[10] reported that the male sex was associated with significantly higher progression rates compared to the female sex. The 5-year disease-specific survival (DSS) rates of females and males were 84% and 78%, respectively. Despite the gender difference noted, no research focused exclusively on female NPC patients has ever been reported. Do female NPC patients have a better prognosis in the NPC epidemic area? What might contribute to their favorable prognosis? To have a comprehensive understanding of these issues, we conducted this retrospective study to analyze the treatment outcomes of Chinese female NPC patients and identify their prognostic features.
Materials and Methods
Patient selection criteria
The patient eligibility criteria were the following: no contraindications for chemotherapy and radiotherapy; stage I to IVa–b disease (by the 2002 UICC staging system); hospitalized and treated in the Sun Yat-sen University Cancer Center between January 2000 and December 2003; no chemotherapy, surgery, or radiotherapy before diagnosis; and a Karnofsky (KPS) score of ≥ 80. All patients had undergone routine checkups, including head and neck magnetic resonance imaging (MRI), chest X-ray, abdominal ultrasonography, and bone scan before treatment.
Treatment strategy
All patients were treated with continuous conventional radiotherapy applying a two-dimensional technique. The radiation doses to the nasopharynx, lymph node–positive areas, and lymph node-negative areas were 60–78 Gy, 60–70 Gy, and 50–60 Gy, respectively. The NPC patients with stage III, IVa, or IVb disease underwent concurrent induction or adjuvant chemotherapy. Platinum-based chemotherapy was used.
Follow-up
The patients were followed every 3 months for the first 2 years. The follow-up intervals gradually increased to 6 months to 1 year. All patients were followed until January 2010.
Statistical analysis
Survival was counted from the date of treatment commencement. Death due to any cause was assessed as the endpoint of OS; locoregional failure and distant metastasis were assessed as the endpoints of DSS.
The Statistical Package for the Social Sciences (SPSS 16.0) program (IBM, Armonk, NY, USA) was used for statistical analysis. Survival rates were calculated using the Kaplan-Meier method, and the differences were compared with the log-rank test. Multivariate analysis was performed with the Cox regression model to identify independent factors. All statistical tests were two-sided, and P < 0.05 was considered significant.
Results
Patient characteristics and follow-up
Clinical data of 2,063 consecutive patients with newly diagnosed, non-metastatic NPC were reviewed. All patients were ethnic Chinese. Their ages ranged from 11 to 86 years (median, 46 years). The pathologic diagnosis was WHO type I in 9 cases, WHO type II in 84 cases, and WHO type III in 1,970 cases. According to the 2002 UICC staging system of NPC, 91 patients were at stage I, 592 at stage II, 796 at stage III, and 584 at stage IVa-b.
All patients completed radical radiotherapy. More than 1 course of platinum-based chemotherapy was given to 145 female and 667 male patients with locoregionally advanced disease. All patients were followed for 2 to 116 months (median, 81 months). Of the 2,063 patients, 98.9%, 95.2%, and 89.6% had complete follow-up data available at 1, 3, and 5 years, respectively. During the follow-up, 760 patients died: 681 died of NPC, 36 died of treatment-related toxicities, 18 died of incidental diseases, and 25 died of unknown causes.
The relationship between gender and clinical characteristics of NPC
With regards to age and WHO pathologic classification, no significant differences were found between female and male patients. However, the female sex was positively associated with an early T category, early N category, early clinical stage, less disease progression, and fewer cancer-related deaths. The female and male patients with early clinical stage disease were 49.4% and 28.1%, respectively. The characteristics of these patients are shown in Table 1.
Table 1. The relationship between gender and clinical characteristics in patients with nasopharyngeal carcinoma (NPC).
| Characteristic | No. of patients | Gender |
P | |
| Female | Male | |||
| Total | 2,063 | 484 | 1,579 | |
| Age (years) | 0.055 | |||
| <46 | 953 (46.2%) | 242 | 711 | |
| ≥ 46 | 1,110 (53.8%) | 242 | 868 | |
| WHO pathologic classification | 0.181 | |||
| Type I | 9 (0.4%) | 4 | 5 | |
| Type II | 84 (4.1%) | 24 | 60 | |
| Type III | 1,970 (95.5%) | 460 | 1,514 | |
| T category | <0.001 | |||
| T1 +T2 | 990 (48.0%) | 317 | 673 | |
| T3 + T4 | 1,073 (52.0%) | 167 | 906 | |
| N category | 0.001 | |||
| N0 + N1 | 1,343 (65.3%) | 347 | 996 | |
| N2 + N3 | 720 (34.7%) | 137 | 583 | |
| Clinical stage | <0.001 | |||
| I + II | 683 (33.1%) | 239 | 444 | |
| III + IV | 1,380(66.9%) | 245 | 1,135 | |
| Disease progression | <0.001 | |||
| No | 1,358 (65.8%) | 372 | 986 | |
| Yes | 705 (34.2%) | 112 | 593 | |
| Cancer-related death | <0.001 | |||
| No | 1,346(65.2%) | 393 | 953 | |
| Yes | 717 (34.8%) | 91 | 626 | |
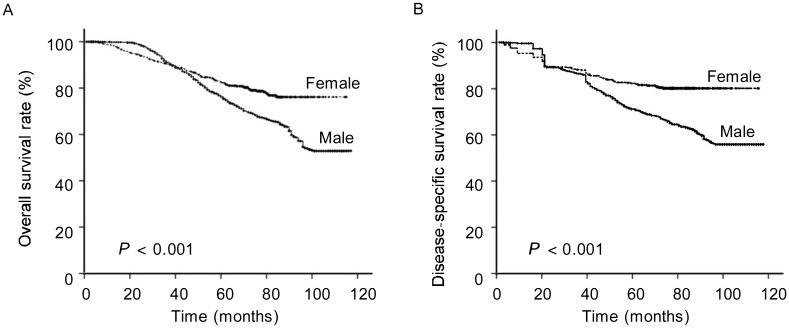
A better OS and DFS in female NPC patients than in male NPC patients
The 5-year OS rates of female and male NPC patients were 79% and 69% (P < 0.001), respectively (Figure 1A). The 5-year DSS rates of female and male NPC patients were 80% and 64% (P< 0.001), respectively (Figure 1B).
Figure 1. The survival curves according to gender for the whole series.
A, overall survival (OS); B, disease-specific survival (DSS).
To confirm that the increased survival rate of females was not a result of only the early stage disease, we further compared the 5-year OS and DSS of patients with the same advanced TNM classification. The results showed that the 5-year OS and DSS of female patients in stages III–IVa-b, T3–4, and N2–3 were all significantly higher than those of the male patients (P < 0.001) (Table 2).
Table 2. The 5-year overall survival (OS) and disease-specific survival (DSS) rates of female and male NPC patients with the same TNM classification.
| Classification | No. of patients | 5-year OS (%) | P | 5-year DSS (%) | P |
| TNM stage | |||||
| Stage I–II | 683 | 0.837 | 0.754 | ||
| Female | 239 | 85 | 86 | ||
| Male | 444 | 85 | 85 | ||
| Stage III–IVa,b | 1,380 | 0.001 | <0.001 | ||
| Female | 245 | 74 | 76 | ||
| Male | 1,135 | 63 | 64 | ||
| T category | 0.021 | 0.012 | |||
| T1+2 | 990 | 84 | |||
| Female | 317 | 83 | 78 | ||
| Male | 673 | 77 | 0.021 | 0.007 | |
| T3+4 | 1,073 | ||||
| Female | 167 | 73 | 75 | ||
| Male | 906 | 64 | 64 | ||
| N category | 0.001 | <0.001 | |||
| N0+1 | 1,343 | ||||
| Female | 347 | 83 | 84 | ||
| Male | 996 | 75 | 76 | ||
| N2+3 | 720 | 0.040 | 0.011 | ||
| Female | 137 | 70 | 73 | ||
| Male | 583 | 60 | 60 |
Multivariate Cox risk model analysis
To distinguish the independent prognostic factors of NPC patients, we used a multivariate analysis to examine the effects of gender, age (≤46 vs. >46), WHO pathologic classification, T category, N category, and TNM stage on the OS and DSS. The results showed that in addition to age, T category, N category, and TNM stage, gender was among the independent prognostic factors for the OS and DSS of NPC patients (Table 3).
Table 3. The multivariate analysis of Cox proportional hazards model for 5-year OS and DSS rates.
| Variate | Wald | Sig. | Exp (B) | 95% confidence interval |
| OS | ||||
| Gender | 7.878 | 0.005 | 1.357 | 1.096–1.679 |
| Age | 50.847 | 0.000 | 1.719 | 1.481–1.995 |
| WHO pathology | 0.091 | 0.763 | 0.952 | 0.691–1.312 |
| T category | 3.060 | 0.080 | 1.130 | 0.985–1.296 |
| N category | 13.115 | 0.000 | 1.194 | 1.085–1.313 |
| TNM stage | 17.232 | 0.000 | 1.445 | 1.215–1.720 |
| DSS | ||||
| Gender | 10.434 | 0.001 | 1.445 | 1.156–1.807 |
| Age | 40.061 | 0.000 | 1.646 | 1.413–1.917 |
| WHO pathology | 0.218 | 0.641 | 0.923 | 0.659–1.292 |
| T category | 3.026 | 0.082 | 1.132 | 0.984–1.303 |
| N category | 13.909 | 0.000 | 1.206 | 1.093–1.331 |
| TNM stage | 17.079 | 0.000 | 1.457 | 1.219–1.743 |
Discussion
NPC differs from other head and neck carcinomas in numerous ways. The most notable difference is its substantial responsiveness to both radiotherapy and chemotherapy. With the combined treatment modality, the 5-year OS rate of all NPC patients reported in our hospital or other institutions is 65%–75%, with the rates of 15%–20% for locoregional recurrence and 19%–23% for distant metastasis [3],[10],[11]. The female sex is traditionally considered a favorable prognostic factor. However, no particular study has reported this difference. In this study, we first reported the impact of gender on the survival status of NPC patients. The results show that both the 5-year OS and DSS rates of female patients were significantly higher than those of male patients. These results suggest that female patients had a better prognosis than male patients.
In the last 40 years, there have been several studies that mention the gender-related outcomes of NPC patients[1],[14]–[17]. As shown in Table 4, the efficacy of radiation was greatly improved with advances in imaging and radiotherapy techniques. However, the survival rate of female patients was always better than male patients during the same period. In our study, the 5-year survival rate of female NPC patients was similar to that reported by Yi et al.[18]. It is well known that TNM stage is undoubtedly the most important prognostic factor for predicting the survival of NPC patients[18]. Studies including patients of both genders reported that 60%–70% of NPC patients had locoregionally advanced disease due to the deep and hidden anatomic location of the nasopharynx[3],[4]. To explain the favorable outcomes of female NPC patients, we first analyzed the clinical characteristics of both female and male patients in our study. We found that only 50.6% of female patients had locoregionally advanced disease, which was much lower than the 71.9% of male patients who had locoregionally advanced NPC. Hence, the relatively low proportion of locoregionally advanced stage in female NPC patients, in part, might result in a better outcome compared to male patients.
Table 4. The 5-year survival rates of males and females with NPC reported by previous studies.
| Reference | Treatment period | Gender | No. | OS |
DFS |
||
| % | P | % | P | ||||
| Qin et al.[15] | 1958–1978 | Male | 1,067 | 39.9 | <0.05 | NA | NA |
| Female | 312 | 46.4 | |||||
| Altun et al.[1] | 1960–1991 | Male | 226 | 58 | NA | 44 | NA |
| Female | 82 | 65 | 57 | ||||
| Erkal et al.[16] | 1979–1996 | Male | 322 | 34 | 0.001 | 34 | 0.006 |
| Female | 125 | 53 | 48 | ||||
| Yeh et al.[17] | 1983–1998 | Male | 568 | 55 | <0.001 | 48 | 0.001 |
| Female | 281 | 68 | 61 | ||||
| Yi et al.[18] | 1990–1999 | Male | 669 | 74.7 | 0.09 | 56.2 | 0.01 |
| Female | 236 | 80.3 | 64.7 | ||||
NA, not available.
However, we found that early stage disease was not the only reason for the favorable prognosis in female NPC patients. We further stratified the patients by early and advanced stages and analyzed the survival of patients with advanced disease. The results showed that even with the same tumor burden, female patients still had better prognoses than male patients. This result suggested that some intrinsic factors might play important roles in the prognosis of NPC. It is not clear why female NPC patients present a better prognosis than males, even with the same tumor burden. In human colon cancer, it had been reported that testosterone negatively affected the immune function of male patients. Furthermore, female sex steroids could have a protective immune role, which might contribute to the increased survival of female patients compared to the corresponding male patients[19]. In addition, because female patients have a better outcome when compared with males, investigators have explored the role of hormonal therapy for patients with advanced melanoma[20],[21]. It is also reasonable to assume that gonadal hormones and their related receptors may play an important part in regulating the biological behavior of NPC. This hypothesis deserves more research to delineate the influence of these factors.
Conclusions
This study showed that female NPC patients had favorable treatment outcomes, with 5-year survival rates exceeding 80%. The favorable prognosis of female NPC patients was not only attributed to early diagnosis and treatment but might also be attributed to some intrinsic factors of female patients. These intrinsic factors may play an important role in the prognosis of NPC.
Acknowledgments
This project has been funded by the National Natural Science Foundation of China (No. 81172041) and Natural Science Foundation of Guangdong Province (No. S2011010005312).
References
- 1.Altun M, Fandi A, Dupuis 0, et al. et al. Undifferentiated nasopharyngeal cancer (UCNT): current diagnostic and therapeutic aspects. Int J Radiat Oncol Biol Phys. 1995;32:859–877. doi: 10.1016/0360-3016(95)00516-2. [DOI] [PubMed] [Google Scholar]
- 2.Ho J. An epidemiological and clinical study of nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 1978;4:183–197. [PubMed] [Google Scholar]
- 3.Liu MZ, Tang LL, Zong JF, et al. et al. Evaluation of sixth edition of AJCC staging system for nasopharyngeal carcinoma and proposed improvement. Int J Radiat Oncol Biol Phys. 2008;70:1115–1123. doi: 10.1016/j.ijrobp.2007.07.2353. [DOI] [PubMed] [Google Scholar]
- 4.Min H, Hong M, Ma J, et al. et al. A new staging system for nasopharyngeal carcinoma in China. Int J Radiat Oncol Biol Phys. 1994;30:1037–1042. [PubMed] [Google Scholar]
- 5.Xiao WW, Han F, Lu TX, et al. et al. Treatment outcomes after radiotherapy alone for patients with early-stage nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2009;74:1070–1076. doi: 10.1016/j.ijrobp.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Lin JC, Jan JS, Hsu CY, et al. et al. Phase III study of concurrent chemoradiotherapy versus radiotherapy alone for advanced nasopharyngeal carcinoma: positive effect on overall and progression-free survival. J Clin Oncol. 2003;21:631–637. doi: 10.1200/JCO.2003.06.158. [DOI] [PubMed] [Google Scholar]
- 7.Chan AT, Leung SF, Ngan RK, et al. et al. Overall survival after concurrent cisplatin-radiotherapy compared with radiotherapy alone in locoregionally advanced nasopharyngeal carcinoma. J Natl Cancer Inst. 2005;97:536–539. doi: 10.1093/jnci/dji084. [DOI] [PubMed] [Google Scholar]
- 8.Krstevska V, Stojkovski I. Chemotherapy in locoregionally advanced nasopharyngeal carcinoma—a review. J Buon. 2008;13:495–503. [PubMed] [Google Scholar]
- 9.Baujat B, Audry H, Bourhis J, et al. et al. Chemotherapy in locally advanced nasopharyngeal carcinoma: an individual patient data meta-analysis of eight randomized trials and 1753 patients. Int J Radiat Oncol Biol Phys. 2006;64:47–56. doi: 10.1016/j.ijrobp.2005.06.037. [DOI] [PubMed] [Google Scholar]
- 10.Lee AW, Sze WM, Au JS, et al. et al. Treatment results for nasopharyngeal carcinoma in the modern era: the Hong Kong experience. Int J Radiat Oncol Biol Phys. 2005;61:1107–1116. doi: 10.1016/j.ijrobp.2004.07.702. [DOI] [PubMed] [Google Scholar]
- 11.Palazzi M, Guzzo M, Tomatis S, et al. et al. Improved outcome of nasopharyngeal carcinoma treated with conventional radiotherapy. Int J Radiat Oncol Biol Phys. 2004;60:1451–1458. doi: 10.1016/j.ijrobp.2004.05.059. [DOI] [PubMed] [Google Scholar]
- 12.Ou SH, Zell JA, Ziogas A, et al. et al. Epidemiology of nasopharyngeal carcinoma in the United States: improved survival of Chinese patients within the keratinizing squamous cell carcinoma histology. Ann Oncol. 2007;18:29–35. doi: 10.1093/annonc/mdl320. [DOI] [PubMed] [Google Scholar]
- 13.Sun LM, Li CI, Huang EY, et al. et al. Survival differences by race in nasopharyngeal carcinoma. Am J Epidemiol. 2007;165:271–8. doi: 10.1093/aje/kwk008. [DOI] [PubMed] [Google Scholar]
- 14.Qin DX, Hu YH, Yan JH, et al. et al. Analysis of 1379 patients with nasopharyngeal carcinoma treated by radiation. Cancer. 1988;61:1117–1124. doi: 10.1002/1097-0142(19880315)61:6<1117::aid-cncr2820610611>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 15.Erkal HS, Serin M, Cakmak A. Nasopharyngeal carcinomas: analysis of patient, tumor and treatment characteristics determining outcome. Radiother Oncol. 2001;61:247–256. doi: 10.1016/s0167-8140(01)00448-0. [DOI] [PubMed] [Google Scholar]
- 16.Yeh SA, Tang Y, Lui CC, et al. et al. Treatment outcomes and late complications of 849 patients with nasopharyngeal carcinoma treated with radiotherapy alone. Int J Radiat Oncol Biol Phys. 2005;62:672–679. doi: 10.1016/j.ijrobp.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Yi JL, Gao L, Huang XD, et al. et al. Nasopharyngeal carcinoma treated by radical radiotherapy alone: ten-year experience of a single institution. Int J Radiat Oncol Biol Phys. 2006;65:161–168. doi: 10.1016/j.ijrobp.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 18.Wei WI, Sham JS. Nasopharyngeal carcinoma. Lancet. 2005;365:2041–2054. doi: 10.1016/S0140-6736(05)66698-6. [DOI] [PubMed] [Google Scholar]
- 19.Derwinger K, Gustavsson B. A study of aspects on gender and prognosis in synchronous colorectal cancer. Clin Med Insights Oncol. 2011;5:259–64. doi: 10.4137/CMO.S7871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McClay EF, McClay ME, Monroe L, et al. et al. The effect of tamoxifen and cisplatin on the disease-free and overall survival of patients with high risk malignant melanoma. Br J Cancer. 2000;83:16–21. doi: 10.1054/bjoc.1999.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chiarion SV, Nortilli R, Aversa SM, et al. et al. Phase II randomized study of dacarbazine, carmustine, cisplatin and tamoxifen versus dacarbazine alone in advanced melanoma patients. Melanoma Res. 2001;11:189–196. doi: 10.1097/00008390-200104000-00015. [DOI] [PubMed] [Google Scholar]