Abstract
Nasopharyngeal carcinoma (NPC) is rare globally but common in China and exhibits a distinct ethnic and geographic distribution. In 2009, the National Central Cancer Registry in China provided real-time surveillance information on NPC. Individual NPC cases were retrieved from the national database based on the ICD-10 topography code C11. The crude incidence and mortality of NPC were calculated by sex and location (urban/rural). China's population in 1982 and Segi's world population structures were used to determine age-standardized rates. In regions covered by the cancer registries in 2009, the crude incidence of NPC was 3.61/100,000 (5.08/100,000 in males and 2.10/100,000 in females; 4.19/100,000 in urban areas and 2.42/100,000 in rural areas). Age-standardized incidences by Chinese population (ASIC) and Segi's world population (ASIW) were 2.05/100,000 and 2.54/100,000, respectively. The crude mortality of NPC was 1.99/100,000 (2.82/100,000 in males and 1.14/100,000 in females; 2.30/100,000 in urban areas and 1.37/100,000 in rural areas). The age-standardized mortalities by Chinese population (ASMC) and world population (ASMW) were 1.04/100,000 and 1.35/100,000, respectively. The incidence and mortality of NPC were higher in males than in females and higher in urban areas than in rural areas. Both age-specific incidence and mortality were relatively low in persons younger than 30 years old, but these rates dramatically increased. Incidence peaked in the 60-64 age group and mortality peaked in the over 85 age group. Primary and secondary prevention, such as lifestyle changes and early detection, should be carried out in males and females older than 30 years of age.
Keywords: Nasopharyngeal carcinoma, cancer registry, incidence, mortality, China
Nasopharyngeal carcinoma (NPC) is a rare malignancy in most parts of the world but is particularly frequent in China, especially in the South[1]. The average incidence of NPC worldwide is less than 1/100,000 population[2]. However, in endemic areas of China, its incidence reaches 20/100,000[3]–[5]. In the past three decades, NPC incidence has declined among the Chinese residing in Southeast Asia, including Taiwan, Hong Kong, and Singapore[5]—areas with lifestyles distinct from that of mainland China. The National Central Cancer Registry (NCCR) of China, responsible for data collection, evaluation, analysis, and publication from population-based cancer registries, has organized three retrospective mortality surveys on the causes of cancer death, which provide sex- and age-specific mortality for major cancers among areas in mainland China. Recent population-based studies in China show that the incidence of NPC in some areas has remained stable in males and even slightly decreased in females[6],[7]. Additionally, although rates are still higher in persons over 50 years of age, the age-specific mortality in the high risk age group has followed a downward trend over a 30-year period.
The NCCR of China established the Chinese Cancer Registry annual report system to comprehensively promote cancer registration. The Chinese Cancer Registry Annual Report has been published since 2008 and has provided the scientific basis for cancer prevention and control in China. In 2012, the NCCR collected data for the calendar year 2009 from 104 registries. After comprehensive quality evaluation, data from 72 registries were selected as sources of the annual report to reflect cancer incidence and mortality in the registration areas. In this study, NPC cases were retrieved from the national database for analysis to show the updated NPC burden in Chinese population.
Materials and Methods
Data source
All new cancer cases diagnosed in 2009 were reported to cancer registries from all hospitals, community health centers, and other institutions, including centers of township medical insurance and the New-type Rural Cooperative Medical System. The death record database was linked and matched with the cancer registration database for identifying cancer deaths and missed cases.
Totally 104 cancer registries (covering 46 cities and 58 counties in 27 provinces) reported cancer registration data to NCCR. The overall population coverage was 109,476,347, accounting for 8.2% of the whole population. The cancer registries coded cancer site and histology according to the International Classification of Diseases for Oncology, third edition (ICD-03) and tenth edition (ICD-10). Invasive cases of NPC (topography code C11) were retrieved and analyzed from the overall cancer database. Demographic information was provided by the National Statistics Bureau.
Quality control
Based on the guideline of Chinese cancer registration[8] and the standard of data inclusion in Cancer Incidence in Five Continents Volume IX[9], cancer registration data were evaluated by several quality indicators: proportion of morphologic verification (MV%), percentage of cancer cases identified with death certification only (DCO%), and mortality/incidence ratio (M/I)[10]–[12]. The detailed standard for data inclusion was shown previously[13]. Generally, data with DCO% less than 20%, an overall MV% more than 55%, and M/I between 0.55 and 0.95 were considered acceptable.
Statistical analysis
Crude incidence and mortality of NPC were prepared by sex, area, and 19 total age groups (<1, 1–4, 5–9,…80–84, ≥85 years). Age-standardized rates were calculated using the Chinese population from 1982 and Segi's World population. The cumulative risk of developing or dying from cancer for persons young than 75 years (in the absence of competing causes of death) was calculated and presented as a percentage. Software including MS-FoxPro, MS-Excel, and IARCcrgTools issued by the International Agency for Research on Cancer (IARC) and the International Association of Cancer Registration (IACR) were used for data checkup. SAS software (version 9.0) was used to calculate incidence and mortality.
Results
Pooled data
After evaluating all submitted information, data from 72 population-based cancer registries were accepted for the annual report. The population covered by these cancer registries was 85,470,522, including 43,231,554 males and 42,238,968 females, accounting for 6.4% of the whole population. A total of 31 registries were from urban areas, covering a total population of 57,489,009, whereas 41 registries were from rural areas, covering a total population of 27,981,513. The MV%, DCO%, and M/I for the national pooled data were 71.99%, 3.05%, and 0.55, respectively, in urban areas and 70.65%, 3.54%, and 0.56, respectively, in rural areas. There were 3,085 new cases of NPC (2,197 males and 888 females) and 1,702 overall NPC cancer deaths (1,219 males and 483 females) in 2009. Detailed information for the covered population, including NPC incidence and deaths in each cancer registry, is shown in Table 1.
Table 1. Population and number of new nasopharyngeal carcinoma (NPC) cases and deaths in cancer registries in 2009.
| Registry | Areaa | Population |
New NPC cases |
NPC deaths |
||||||
| Both | Males | Females | Both | Males | Females | Both | Males | Females | ||
| Beijing | 1 | 7,645,186 | 3,859,586 | 3,785,600 | 81 | 64 | 17 | 76 | 56 | 20 |
| Qianxi | 2 | 361,312 | 182,138 | 179,174 | 1 | 1 | 0 | 0 | 0 | 0 |
| Shexian | 2 | 394,944 | 205,168 | 189,776 | 2 | 2 | 0 | 2 | 2 | 0 |
| Cixian | 2 | 634,333 | 322,621 | 311,712 | 6 | 5 | 1 | 2 | 2 | 0 |
| Baoding | 1 | 948,612 | 478,051 | 470,561 | 11 | 5 | 6 | 4 | 2 | 2 |
| Yangquan | 1 | 683,165 | 346,023 | 337,142 | 2 | 2 | 0 | 2 | 1 | 1 |
| Yangcheng | 2 | 383,165 | 192,119 | 191,046 | 5 | 3 | 2 | 2 | 0 | 2 |
| Chifeng | 1 | 1,203,006 | 613,725 | 589,281 | 10 | 6 | 4 | 7 | 4 | 3 |
| Shenyang | 1 | 3,497,815 | 1,722,976 | 1,774,839 | 56 | 41 | 15 | 34 | 19 | 15 |
| Dalian | 1 | 2,266,224 | 1,136,772 | 1,129,452 | 36 | 26 | 10 | 18 | 14 | 4 |
| Zhuanghe | 2 | 915,660 | 461,826 | 453,834 | 15 | 11 | 4 | 5 | 1 | 4 |
| An'shan | 1 | 1,471,775 | 731,916 | 739,859 | 22 | 14 | 8 | 14 | 10 | 4 |
| Benxi | 1 | 955,409 | 475,113 | 480,296 | 13 | 11 | 2 | 6 | 5 | 1 |
| Dandong | 1 | 767,011 | 378,794 | 388,217 | 14 | 8 | 6 | 10 | 5 | 5 |
| Donggang | 2 | 640,853 | 323,798 | 317,055 | 22 | 18 | 4 | 3 | 2 | 1 |
| Dehui | 2 | 943,395 | 479,486 | 463,909 | 21 | 17 | 4 | 8 | 5 | 3 |
| Yanji | 2 | 440,957 | 215,260 | 225,697 | 0 | 0 | 0 | 2 | 1 | 1 |
| Daoli District, Harbin | 1 | 713,264 | 351,071 | 362,193 | 12 | 10 | 2 | 6 | 5 | 1 |
| Nangang District, Harbin | 1 | 1,020,233 | 508,921 | 511,312 | 13 | 9 | 4 | 10 | 8 | 2 |
| Shangzhi | 2 | 616,046 | 314,864 | 301,182 | 3 | 0 | 3 | 0 | 0 | 0 |
| Shanghai | 1 | 6,181,334 | 3,084,496 | 3,096,838 | 220 | 167 | 53 | 189 | 152 | 37 |
| Jintan | 2 | 545,000 | 26,2407 | 282,593 | 11 | 7 | 4 | 11 | 8 | 3 |
| Suzhou | 1 | 2,392,087 | 1,183,716 | 1,208,371 | 79 | 55 | 24 | 51 | 37 | 14 |
| Haian | 2 | 936,785 | 463,612 | 473,173 | 16 | 10 | 6 | 16 | 9 | 7 |
| Qidong | 2 | 1,114,951 | 548,805 | 566,146 | 38 | 25 | 13 | 25 | 17 | 8 |
| Haimen | 2 | 1,016,228 | 501,407 | 514,821 | 32 | 18 | 14 | 13 | 11 | 2 |
| Lianyungang | 1 | 886,862 | 452,358 | 434,504 | 16 | 12 | 4 | 10 | 6 | 4 |
| Donghai | 2 | 1,117,858 | 579,751 | 538,107 | 17 | 9 | 8 | 11 | 9 | 2 |
| Guanyun | 2 | 1,015,229 | 534,502 | 480,727 | 19 | 13 | 6 | 16 | 14 | 2 |
| Chuzhou District, Huai'an | 1 | 1,174,877 | 609,088 | 565,789 | 14 | 9 | 5 | 11 | 7 | 4 |
| Huaiyin District, Huai'an | 1 | 900,027 | 465,502 | 434,525 | 13 | 10 | 3 | 2 | 0 | 2 |
| Xuyi | 2 | 759,450 | 388,180 | 371,270 | 29 | 20 | 9 | 7 | 4 | 3 |
| Jinhu | 2 | 352,292 | 176,689 | 175,603 | 11 | 9 | 2 | 5 | 4 | 1 |
| Sheyang | 2 | 965,817 | 494,682 | 471,135 | 24 | 18 | 6 | 15 | 9 | 6 |
| Jianhu | 2 | 805,465 | 410,369 | 395,096 | 9 | 7 | 2 | 9 | 7 | 2 |
| Dafeng | 2 | 724,147 | 363,326 | 360,821 | 11 | 7 | 4 | 7 | 4 | 3 |
| Yangzhong | 2 | 272,046 | 134,758 | 137,288 | 9 | 8 | 1 | 2 | 2 | 0 |
| Taixing | 2 | 1,128,840 | 613,199 | 515,641 | 17 | 12 | 5 | 10 | 7 | 3 |
| Hangzhou | 1 | 6,753,509 | 3,403,893 | 3,349,616 | 363 | 240 | 123 | 110 | 80 | 30 |
| Jiaxing | 1 | 509,367 | 253,819 | 255,548 | 16 | 14 | 2 | 12 | 8 | 4 |
| Jiashan | 2 | 382,475 | 189,692 | 192,783 | 15 | 12 | 3 | 10 | 8 | 2 |
| Haining | 2 | 653,957 | 322,969 | 330,988 | 31 | 22 | 9 | 8 | 7 | 1 |
| Shangyu | 2 | 771,321 | 383,462 | 387,859 | 21 | 17 | 4 | 16 | 15 | 1 |
| Xianju | 2 | 490,070 | 255,438 | 234,632 | 14 | 12 | 2 | 7 | 6 | 1 |
| Feixi | 2 | 858,895 | 449,882 | 409,013 | 18 | 14 | 4 | 8 | 6 | 2 |
| Maanshan | 1 | 633,477 | 323,834 | 309,643 | 35 | 24 | 11 | 6 | 4 | 2 |
| Tongling | 1 | 433,545 | 221,375 | 212,170 | 8 | 6 | 2 | 5 | 5 | 0 |
| Changle | 2 | 673,717 | 355,091 | 318,626 | 21 | 17 | 4 | 14 | 13 | 1 |
| Xiamen | 1 | 1,160,135 | 583,873 | 576,262 | 89 | 63 | 26 | 26 | 19 | 7 |
| Zhanggong District, Ganzhou | 1 | 420,759 | 212,159 | 208,600 | 30 | 18 | 12 | 14 | 10 | 4 |
| Linqu | 2 | 817,857 | 417,434 | 400,423 | 7 | 7 | 0 | 5 | 4 | 1 |
| Wenshang | 2 | 762,828 | 388,454 | 374,374 | 3 | 2 | 1 | 1 | 0 | 1 |
| Feicheng | 2 | 733,501 | 358,739 | 374,762 | 6 | 2 | 4 | 7 | 4 | 3 |
| Yanshi | 2 | 602,266 | 306,192 | 296,074 | 1 | 1 | 0 | 2 | 1 | 1 |
| Linzhou | 2 | 108,0241 | 557,392 | 522,849 | 3 | 0 | 3 | 3 | 3 | 0 |
| Xiping | 2 | 858,002 | 434,899 | 423,103 | 6 | 4 | 2 | 1 | 0 | 1 |
| Wuhan | 1 | 4,832,174 | 2,484,622 | 2,347,552 | 173 | 122 | 51 | 98 | 73 | 25 |
| Yunmeng | 2 | 524,801 | 261,237 | 263,564 | 13 | 10 | 3 | 8 | 7 | 1 |
| Hengdong | 2 | 713,458 | 373,923 | 339,535 | 33 | 23 | 10 | 13 | 7 | 6 |
| Guangzhou | 1 | 3,968,216 | 2,014,580 | 1953,636 | 662 | 480 | 182 | 374 | 267 | 107 |
| Sihui | 2 | 413,363 | 211,351 | 202,012 | 122 | 79 | 43 | 79 | 53 | 26 |
| Zhongshan | 1 | 1,468,391 | 732,333 | 736,058 | 263 | 189 | 74 | 139 | 91 | 48 |
| Liuzhou | 1 | 1,038,208 | 533,050 | 505,158 | 68 | 52 | 16 | 42 | 30 | 12 |
| Fusui | 2 | 444,332 | 236,000 | 208,332 | 19 | 15 | 4 | 12 | 11 | 1 |
| Jiulongpo District, Chongqing | 1 | 798,618 | 402,961 | 395,657 | 25 | 21 | 4 | 12 | 10 | 2 |
| Qingyang District, Chengdu | 1 | 534,701 | 277,154 | 257,547 | 29 | 25 | 4 | 12 | 8 | 4 |
| Ziliujing District, Zigong | 1 | 357,600 | 179,873 | 177,727 | 14 | 11 | 3 | 4 | 2 | 2 |
| Yanting | 2 | 610,103 | 316,499 | 293,604 | 20 | 12 | 8 | 13 | 8 | 5 |
| Jingtai | 2 | 233,609 | 119,953 | 113,656 | 2 | 1 | 1 | 2 | 1 | 1 |
| Liangzhou District, Wuwei | 1 | 990,583 | 524,276 | 466,307 | 10 | 5 | 5 | 8 | 4 | 4 |
| Xining | 1 | 882,839 | 439,175 | 443,664 | 10 | 6 | 4 | 8 | 4 | 4 |
| Xinyuan | 2 | 271,944 | 138,895 | 133,049 | 5 | 2 | 3 | 2 | 1 | 1 |
| Total | 85,470,522 | 43,231,554 | 42,238,968 | 3,085 | 2,197 | 888 | 1,702 | 1,219 | 483 | |
a 1, urban area; 2, rural area.
Incidence
The crude incidence of NPC was 3.61/100,000 in 2009, accounting for 1.26% of all new cancer cases. The age-standardized incidences by Chinese population (ASIC) and world population (ASIW) were 2.05/100,000 and 2.54/100,000, respectively. Among persons under the age of 75, the cumulative incidence was 0.28%.
NPC occurred more frequently among males than females. For males, the crude incidence of NPC was 5.08/100,000, whereas the ASIC and ASIW were 2.89/100,000 and 3.60/100,000, respectively. For females, the crude incidence of NPC was 2.10/100,000, whereas the ASIC and ASIW were 1.21/100,000 and 1.47/100,000, respectively. The crude incidence in urban areas (4.19/100,000) was higher than that in rural areas (2.42/100,000). After age standardization, incidence in urban areas was still higher than that in rural areas (ASIW, 2.88/100,000 vs. 1.80/100,000; Table 2).
Table 2. NPC incidence by sex and area in regions covered by the cancer registries in 2009.
| Location | Sex | No. of cases | Crude rate (1/105) | Ratio | ASIC (1/105) | ASIW (1/105) | Cumulative rate (%) Age 0–74 |
| All areas | Both | 3,085 | 3.61 | 1.26 | 2.05 | 2.54 | 0.28 |
| Males | 2,197 | 5.08 | 1.60 | 2.89 | 3.60 | 0.40 | |
| Females | 888 | 2.10 | 0.83 | 1.21 | 1.47 | 0.16 | |
| Urban | Both | 2,407 | 4.19 | 1.38 | 2.33 | 2.88 | 0.32 |
| Males | 1,725 | 5.95 | 1.80 | 3.32 | 4.12 | 0.46 | |
| Females | 682 | 2.39 | 0.87 | 1.35 | 1.65 | 0.18 | |
| Rural | Both | 678 | 2.42 | 0.97 | 1.44 | 1.80 | 0.19 |
| Males | 472 | 3.31 | 1.13 | 1.97 | 2.48 | 0.28 | |
| Females | 206 | 1.50 | 0.73 | 0.90 | 1.09 | 0.11 |
ASIC, age-standardized incidence by Chinese population; ASIW, age-standardized incidence by world population.
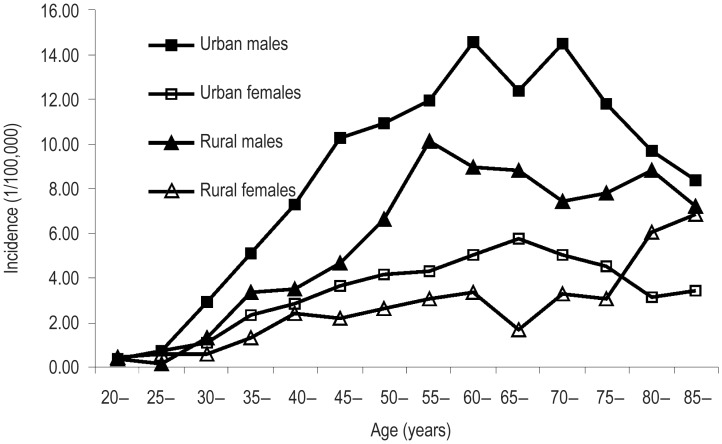
Age-specific incidence of NPC for both sexes and areas was compared. Overall, the age-specific incidence was relatively low in persons under 30 years old but dramatically increased in those over 30 years old, peaking in the 60–64 age group in males and urban areas, in 80-84 age group in rural areas, and in 70-74 age group in females. For persons over 30 years old, NPC age-specific incidence was more than 2-fold greater in males than in females, although there were slight differences among those under 30 years old. The age-specific incidence of NPC in urban areas was generally higher than that in rural areas both in males and females, especially in older age groups (Table 3, Figure 1).
Table 3. Age-specific incidence of NPC in regions covered by the cancer registries in 2009 (1/105).
| Age group | All areas |
Urban areas |
Rural areas |
||||||
| Both | Males | Females | Both | Males | Females | Both | Males | Females | |
| All | 3.61 | 5.08 | 2.10 | 4.19 | 5.95 | 2.39 | 2.42 | 3.31 | 1.50 |
| <1 | 0.16 | 0.00 | 0.34 | 0.26 | 0.00 | 0.55 | 0.00 | 0.00 | 0.00 |
| 1-4 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 5-9 | 0.06 | 0.05 | 0.06 | 0.09 | 0.09 | 0.10 | 0.00 | 0.00 | 0.00 |
| 10-14 | 0.04 | 0.04 | 0.05 | 0.04 | 0.07 | 0.00 | 0.05 | 0.00 | 0.11 |
| 15-19 | 0.18 | 0.18 | 0.19 | 0.20 | 0.22 | 0.17 | 0.16 | 0.10 | 0.22 |
| 20-24 | 0.38 | 0.37 | 0.39 | 0.37 | 0.37 | 0.36 | 0.42 | 0.37 | 0.47 |
| 25-29 | 0.61 | 0.54 | 0.68 | 0.72 | 0.70 | 0.73 | 0.36 | 0.18 | 0.55 |
| 30-34 | 1.63 | 2.33 | 0.91 | 1.98 | 2.87 | 1.08 | 0.97 | 1.34 | 0.60 |
| 35-39 | 3.23 | 4.47 | 1.98 | 3.69 | 5.06 | 2.30 | 2.32 | 3.31 | 1.32 |
| 40-44 | 4.38 | 6.02 | 2.70 | 5.10 | 7.30 | 2.85 | 2.93 | 3.47 | 2.37 |
| 45-49 | 5.89 | 8.52 | 3.16 | 6.99 | 10.23 | 3.61 | 3.41 | 4.63 | 2.15 |
| 50-54 | 6.73 | 9.67 | 3.70 | 7.55 | 10.90 | 4.12 | 4.65 | 6.58 | 2.62 |
| 55-59 | 7.67 | 11.41 | 3.91 | 8.09 | 11.96 | 4.27 | 6.67 | 10.13 | 3.04 |
| 60-64 | 8.63 | 12.75 | 4.50 | 9.75 | 14.57 | 5.03 | 6.21 | 8.95 | 3.32 |
| 65-69 | 7.73 | 11.11 | 4.42 | 8.96 | 12.33 | 5.75 | 5.27 | 8.78 | 1.65 |
| 70-74 | 8.27 | 12.34 | 4.54 | 9.50 | 14.44 | 5.03 | 5.32 | 7.42 | 3.30 |
| 75-79 | 7.20 | 10.71 | 4.09 | 7.95 | 11.80 | 4.50 | 5.26 | 7.81 | 3.04 |
| 80-84 | 6.42 | 9.47 | 4.00 | 6.09 | 9.71 | 3.16 | 7.24 | 8.84 | 6.04 |
| ≥85 | 5.79 | 8.04 | 4.36 | 5.34 | 8.34 | 3.38 | 6.96 | 7.20 | 6.82 |
Figure 1. Age-specific incidence of nasopharyngeal carcinoma (NPC) in males and females in urban and rural areas in 2009.
The age-specific incidence increased as age increased and peaked in the 60-64 age group in urban males, in the 55-59 age group in rural males, in the 65-69 age group in urban females, and in the 85 and over age group in rural females. Incidences in urban areas were higher than those in rural areas except among females over the age of 75, and incidences in males were higher than those in females in any age group.
Mortality
The mortality of NPC was higher in males than in females. The crude mortality, the age-standardized mortalities by Chinese population (ASMC) and world population (ASMW) were 2.82/100,000, 1.51/100,000, and 1.97/100,000, respectively, for males and 1.14/100,000, 0.57/100,000, and 0.74/100,000, respectively, for females. These values were 2.30/100,000, 1.15/100,000, and 1.50/100,000, respectively, in urban areas and 1.37/100,000, 0.78/100,000, and 1.00/100,000, respectively, in rural areas. NPC was confirmed to be a fatal disease in both males and females, and in urban and rural areas (Table 4).
Table 4. NPC mortality by sex and area in regions covered by the cancer registries in 2009.
| Location | Sex | No. of cases | Crude rate (1/105) | Ratio | ASMC (1/105) | ASMW (1/105) | Cumulative rate (%) Age 0-74 |
|
| All areas | Both | 1,702 | 1.99 | 1.10 | 1.04 | 1.35 | 0.15 | |
| Males | 1,219 | 2.82 | 1.26 | 1.51 | 1.97 | 0.22 | ||
| Females | 483 | 1.14 | 0.84 | 0.57 | 0.74 | 0.09 | ||
| Urban | Both | 1,320 | 2.30 | 1.26 | 1.15 | 1.50 | 0.17 | |
| Males | 946 | 3.26 | 1.46 | 1.69 | 2.21 | 0.25 | ||
| Females | 374 | 1.31 | 0.94 | 0.63 | 0.82 | 0.10 | ||
| Rural | Both | 382 | 1.37 | 0.77 | 0.78 | 1.00 | 0.11 | |
| Males | 273 | 1.92 | 0.85 | 1.12 | 1.42 | 0.17 | ||
| Females | 109 | 0.79 | 0.62 | 0.43 | 0.56 | 0.06 | ||
ASMC, age-standardized mortality by Chinese population; ASMW, age-standardized mortality by world population.
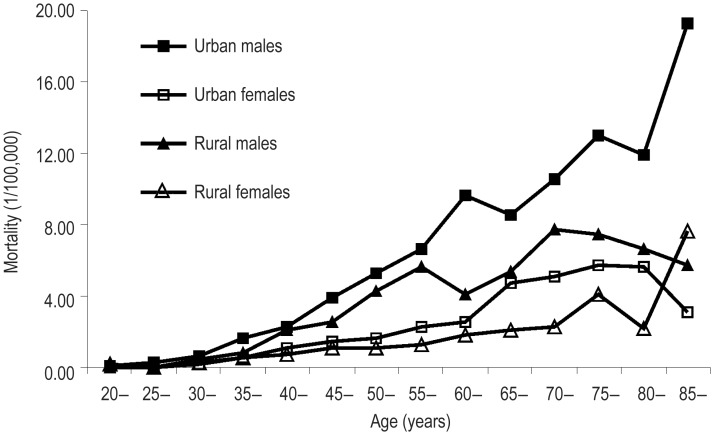
Age-specific mortality by sex and area is shown in Table 5 and Figure 2. The mortality was relatively low in age groups under 40 years old and peaked in the over 85 year age group. However, in urban females, the mortality in the 75–79 age group was the highest among all groups and in rural males, the 70–74 age group had the highest mortality of NPC. The age-specific mortality of NPC in urban areas was generally higher than that in rural areas in both males and females.
Table 5. Age-specific mortality of NPC in regions covered by the cancer registries in 2009 (1/105).
| Age group | All areas |
Urban areas |
Rural areas |
||||||
| Both | Males | Females | Both | Males | Females | Both | Males | Females | |
| All | 1.99 | 2.82 | 1.14 | 2.30 | 3.26 | 1.31 | 1.37 | 1.92 | 0.79 |
| <1 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 1-4 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 5-9 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 10-14 | 0.04 | 0.08 | 0.00 | 0.04 | 0.07 | 0.00 | 0.05 | 0.10 | 0.00 |
| 15-19 | 0.06 | 0.07 | 0.04 | 0.03 | 0.06 | 0.00 | 0.11 | 0.10 | 0.11 |
| 20-24 | 0.07 | 0.05 | 0.08 | 0.06 | 0.07 | 0.04 | 0.09 | 0.00 | 0.19 |
| 25-29 | 0.11 | 0.19 | 0.03 | 0.16 | 0.27 | 0.04 | 0.00 | 0.00 | 0.00 |
| 30-34 | 0.38 | 0.54 | 0.21 | 0.40 | 0.60 | 0.19 | 0.34 | 0.42 | 0.26 |
| 35-39 | 0.97 | 1.36 | 0.58 | 1.11 | 1.63 | 0.58 | 0.69 | 0.81 | 0.58 |
| 40-44 | 1.60 | 2.17 | 1.01 | 1.69 | 2.23 | 1.13 | 1.42 | 2.06 | 0.76 |
| 45-49 | 2.43 | 3.50 | 1.33 | 2.71 | 3.92 | 1.44 | 1.82 | 2.53 | 1.08 |
| 50-54 | 3.27 | 5.01 | 1.47 | 3.48 | 5.30 | 1.62 | 2.72 | 4.29 | 1.09 |
| 55-59 | 4.16 | 6.32 | 1.98 | 4.42 | 6.61 | 2.26 | 3.52 | 5.67 | 1.27 |
| 60-64 | 5.08 | 7.85 | 2.30 | 6.05 | 9.66 | 2.51 | 2.99 | 4.08 | 1.82 |
| 65-69 | 5.66 | 7.48 | 3.89 | 6.62 | 8.57 | 4.76 | 3.75 | 5.39 | 2.06 |
| 70-74 | 6.90 | 9.71 | 4.32 | 7.72 | 10.58 | 5.14 | 4.93 | 7.69 | 2.29 |
| 75-79 | 8.16 | 11.46 | 5.23 | 9.14 | 12.99 | 5.69 | 5.62 | 7.42 | 4.06 |
| 80-84 | 7.22 | 10.48 | 4.64 | 8.46 | 11.93 | 5.64 | 4.09 | 6.63 | 2.20 |
| ≥85 | 8.75 | 15.70 | 4.36 | 9.44 | 19.29 | 3.05 | 6.96 | 5.76 | 7.67 |
Figure 2. Age-specific mortality of NPC in cancer registration areas in 2009.
The age-specific mortality increased as age increased. However, a decline was observed starting in the 70-74 age group in rural males and the 80-84 age group in urban females. Mortalities in urban areas were higher than those in rural areas except among females over 85 years of age, and mortalites in males were higher than those in females in any age group.
Discussion
For this analysis of NPC incidence and mortality in 2009, 72 registries were qualified as sources of the annual report on cancer burden in 2009. The data in this report covered 85.47 million people (about 57.49 million from 31 urban areas), which is the largest population coverage to date. We analyzed NPC cases including 3,085 newly diagnosed patients and 1,702 deaths—data that might be representative of the whole country.
Compared with other studies in China during past decades, the incidence of NPC has remained stable[14] or slightly decreased[7] in females in low-risk regions, or has slightly increased in males in some high-risk regions[15]. NCCR data analysis revealed that the crude incidence and mortality fluctuated slightly in 2009 due to different population coverage. Additionally, NCCR results showed that incidence was higher in males than in females. The crude incidence in urban areas was also slightly higher than that in rural areas for both males and females. After age standardization, incidences were still higher in males and in urban areas compared to females and rural areas, respectively. The results showed that the age-specific incidence of persons in the 60–64 year old age group in urban areas was 1–2 times higher than that in rural areas, both in males and females.
Although a rare disease worldwide, NPC shows a relatively high incidence among the Chinese, probably because of Epstein-Barr virus (EBV) infection, lifestyle, or smoking-related factors[16]. In endemic areas in China, NPC remains a common and fatal disease. The prevention strategy in China focuses mainly on secondary prevention, with a goal of improving rates of early detection and diagnosis in NPC patients and thereby giving high-risk populations a clinically valuable survival advantage[17]. Since the 1970s, NPC screening tests and studies for high-risk areas in southern China, such as Sihui, have included monitoring for EBV using anti-EBV serum biomarkers[18]–[22], but there is still no confirmed screening scheme for a larger sample size nationwide. Nevertheless, screening for plasma EBV DNA[22] in persons in high-risk age ranges[6], [19], as well as health education and promotion should become standard practice for high-risk areas in China.
In conclusion, although the incidence of NPC remains stable and low in most age groups, especially in the young generation, it is still a major public issue in high-risk regions in China, especially among persons in high-risk age ranges. The cancer registry provides timely and dynamic information for making national, regional, and local policies for cancer control. As NCCR continues to expand the national cancer registry system, primary and secondary prevention of NPC is expected to improve.
Acknowledgments
We thank all staff from local cancer registries for sharing their cancer registration databases.
References
- 1.Huang TR, Zhang SW, Chen WQ, et al. Trends in nasopharyngeal carcinoma mortality in China, 1973-2005. Asian Pac J Cancer Prev. 2012;13:2495–2502. doi: 10.7314/apjcp.2012.13.6.2495. [DOI] [PubMed] [Google Scholar]
- 2.Black RJ, Bray F, Ferlay J, et al. Cancer incidence and mortality in the European Union: cancer registry data and estimates of national incidence for 1990. Eur J Cancer. 1997;33:1075–1107. doi: 10.1016/s0959-8049(96)00492-3. [DOI] [PubMed] [Google Scholar]
- 3.Yu MC, Yuan JM. Epidemiology of nasopharyngeal carcinoma. Semin Cancer Biol. 2002;12:421–429. doi: 10.1016/s1044579x02000858. [DOI] [PubMed] [Google Scholar]
- 4.Ren JS, Chen WQ, Shin HR, et al. A comparison of two methods to estimate the cancer incidence and mortality burden in China in 2005. Asian Pac J Cancer Prev. 2010;11:1587–1594. [PubMed] [Google Scholar]
- 5.Chang ET, Adami HO. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2006;15:1765–1777. doi: 10.1158/1055-9965.EPI-06-0353. [DOI] [PubMed] [Google Scholar]
- 6.Cao SM, Simons MJ, Qian CN. The prevalence and prevention of nasopharyngeal carcinoma in China. Chin J Cancer. 2011;30:114–119. doi: 10.5732/cjc.010.10377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang WS, Yang C, Zheng JW, et al. Time trend analysis of incidence rate for nasopharyngeal carcinoma in urban Shanghai. Zhonghua Liu Xing Bing Xue Za Zhi. 2009;30:1171–1174. [in Chinese] [PubMed] [Google Scholar]
- 8.Beijing: The Peking Union Medical College Press; 2004. National Office for Cancer Prevention and Control & National Central Cancer Registry. The guideline of Chinese cancer registration. [in Chinese] [Google Scholar]
- 9.Cancer incidence in five continents. Volume IX. IARC Sci Publ. 2008:1–837. [PubMed] [Google Scholar]
- 10.Curado MP, Edwards B, Shin HR, et al. Lyon: IARC; 2007. Cancer incidence in five continents, vol. LX. Scientific Publications 160. [Google Scholar]
- 11.Parkin DM. Lyon: IARC; 1994. Comparability and quality control in cancer registration. [Google Scholar]
- 12.Ferlay J, Burkhard C, Whelan S, et al. Lyon: IARC; 2005. Check and conversion programs for cancer registries. [Google Scholar]
- 13.Vol. 2 Beijing: Military Medical Science Press; 2011. National Office for Cancer Prevention and Control, National Center for Cancer Registry, Disease Prevnetion and Control Bureau, MOH. Chinese cancer registry annual report (2010) [Google Scholar]
- 14.Xie SH, Gong J, Yang NN, et al. Time trends and age-period-cohort analyses on incidence rates of nasopharyngeal carcinoma during 1993-2007 in Wuhan, China. Cancer Epidemiol. 2012;36:8–10. doi: 10.1016/j.canep.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Jia WH, Huang QH, Liao J, et al. Trends in incidence and mortality of nasopharyngeal carcinoma over a 20-25 year period (1978/1983-2002) in Sihui and Cangwu counties in southern China. BMC Cancer. 2006;6:178. doi: 10.1186/1471-2407-6-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arnold M, Wildeman MA, Visser O, et al. Lower mortality from nasopharyngeal cancer in the netherlands since 1970 with differential incidence trends in histopathology. Oral Oncol. 2013;49:237–243. doi: 10.1016/j.oraloncology.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 17.Ng WT, Choi CW, Lee MC, et al. Outcomes of nasopharyngeal carcinoma screening for high risk family members in Hong Kong. Fam Cancer. 2010;9:221–228. doi: 10.1007/s10689-009-9296-y. [DOI] [PubMed] [Google Scholar]
- 18.Rao DP, Liu Q, Cao SM. Cost-effectiveness evaluation of seven screening strategies for nasopharyngeal carcinoma. Zhonghua Zhong Liu Za Zhi. 2012;34:549–553. doi: 10.3760/cma.j.issn.0253-3766.2012.07.015. [in Chinese] [DOI] [PubMed] [Google Scholar]
- 19.Liu Y, Huang Q, Liu W, et al. Establishment of VCA and EBNA1 IgA-based combination by enzyme-linked immunosorbent assay as preferred screening method for nasopharyngeal carcinoma: a two-stage design with a preliminary performance study and a mass screening in southern China. Int J Cancer. 2012;131:406–416. doi: 10.1002/ijc.26380. [DOI] [PubMed] [Google Scholar]
- 20.Chen F, Huang QH, Fang F, et al. Interval cancers in naso-pharyngeal carcinoma screening: comparing two screening intervals after a negative initial screening result. J Med Screen. 2012;19:195–200. doi: 10.1258/jms.2012.012068. [DOI] [PubMed] [Google Scholar]
- 21.Cao SM, Liu Z, Jia WH, et al. Fluctuations of Epstein-Barr virus serological antibodies and risk for nasopharyngeal carcinoma: a prospective screening study with a 20-year follow-up. PLoS One. 2011;6:e19100. doi: 10.1371/journal.pone.0019100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan KC, Hung EC, Woo JK, et al. Early detection of nasopharyngeal carcinoma by plasma Epstein-Barr virus DNA analysis in a surveillance program. Cancer. 2013;119:1838–1844. doi: 10.1002/cncr.28001. [DOI] [PubMed] [Google Scholar]