Abstract
Colorectal cancer screening has been shown to be a cost-effective intervention, but uncertainty remains over the most cost-effective methods for increasing screening rates.
We used data from a pragmatic randomized controlled trial to estimate the cost-effectiveness of an automated telephone intervention from a managed care perspective. Intervention group patients received calls for fecal occult blood testing (FOBT) screening.
Electronic medical records confirmed whether a patient had completed screening. We searched patient’s electronic medical record for any screening (defined as FOBT, flexible sigmoidoscopy, double contrast barium enema, or colonoscopy) during follow-up.
Intervention costs included project implementation and management, telephone calls, patient identification and tracking. Costs of screening included FOBT (kits, mailing and processing) and any completed screening tests during follow-up. We estimated the incremental cost-effectiveness ratio (ICER) of the cost per additional screen.
Results
At 6 months average costs per patient in the intervention group were $37 (25% screened) and $34 (19% screened) in the control groups. The ICER at 6 months was $40 per additional screen. The probability of cost-effectiveness was 0.49, 0.84 and 0.99 for willingness to pay thresholds of $40, $100 and $200, respectively. Similar results were seen at 9 months.
Screening rates and cost-effectiveness differed by age. A greater increase in FOBT testing was seen for patients aged 70 years and over (45 per 100 intervention, 33 per 100 control) compared with younger patients (25 per 100 intervention, 21 per 100 control). The intervention was dominant (lower costs and greater proportion of patients screened) for patients aged 70 years and over and was $73 per additional screen for younger patients.
Discussion
A patient-directed, automated phone calling increased screening rates by about 6% and costs by $3 per patient. The ICER we report is less than half what other studies have reported. The intervention was especially good value for money in older patients. At a willingness to pay of $100 or higher per additional screening test our study suggests an automated telephone reminder intervention can be an optimal use of resources.
Introduction
Colorectal cancer (CRC) is a common and often lethal disease with a lifetime risk of about 1 in 20; it causes more than 51,000 deaths annually in the US. When diagnosed at late stages the 5-year survival is less than 12%, but patients with localized tumors have a 5-year survival greater than 90%. 1 Early detection is clearly a key to improving survival, and screening has been shown to be cost-effective (for example, at a commonly used threshold of $50,000 per year of life gained), with some analyses even suggesting screening to be cost-saving.2 While CRC screening rates have increased in recent years, they are still below 60% for people aged <64 years, and below 75% for those aged over 65 years.3
Because the favorable cost-effectiveness of CRC screening is now established, attention has shifted to optimizing methods for increasing adherence with CRC screening. The cost-effectiveness of several intervention types has been reported including mailing stool cards, with and without targeted calls, where the cost per additional patient screened has ranged from about $100 to over $6,000 depending on the intensity of the intervention 4,5 and physician education efforts6,7where the cost per additional patient screened has ranged from about $100 to $1,000.
Automated telephone calls have been used in several disease areas to remind and inform patients about a wide range of preventive and therapeutic health care interventions.8-11 A recently reported pragmatic trial by our group showed that automated telephone reminders significantly improved CRC screening rates.9 Using data from that randomized control trial (RCT), this report focuses on the cost-effectiveness per additional patient screened of telephone reminders relative to usual care.
Methods
We used findings from a practical RCT that enrolled patients due for colorectal cancer screening (due, as defined by National Council for Quality Assurance [NCQA]) to estimate the cost-effectiveness of an automated telephone intervention relative to usual care on colorectal cancer screening. The cost analysis focuses on replication costs12 from the perspective of an HMO and included any method of screening (not just fecal occult blood testing (FOBT)). Our follow-up was less than one year, so costs and effects were not discounted; costs were inflated to reflect 2008 dollars.13
Trial design
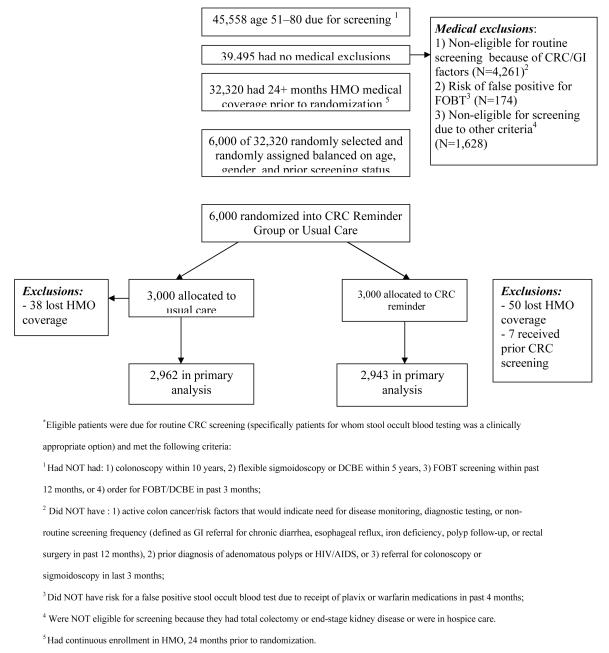
A complete description of the trial has been reported elsewhere.9 The trial was conducted at Kaiser Permanente Northwest, a not-for-profit, group-model HMO and was approved by its institutional review board. Figure 1 details how patients were selected in the RCT; 6000 patients (out of 32,320) were randomly allocated to automated telephone contact or usual care. Consistent with United States Preventive Services Task Force (USPSTF) in place at the time of trial initiation14 CRC screening guidelines, we selected average risk patients aged 51-80 years who were eligible for screening (e.g. had no evidence of relevant screening in the HMO’s records, and did not have risk factors indicating need for disease monitoring).
Figure 1.
Study design and population selection* (used with permission)
Intervention group
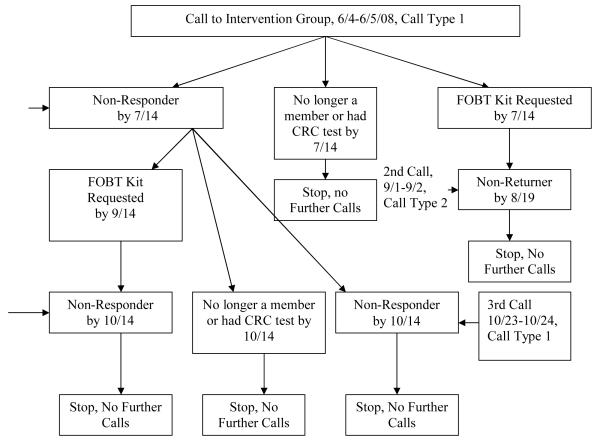
Intervention group patients were exposed to calls prompting FOBT screening (call type 1) and FOBT return reminder calls (call type 2); while these calls were not personalized they were directed toward specific individuals. Figure 2 details the timing of these calls. Call type 1 was brief (1 minute) and provided information about the benefits of CRC screening, and encouraged FOBT as a relatively simple and low-risk method of cancer screening. Recipients who answered could immediately request a mailed FOBT kit by touch-tone. A detailed message which included a telephone number to call for FOBT kit requests was left via voice mail for unanswered calls. Anyone who did not screen received up to 2 “general” automated reminder calls, 6 weeks apart. One additional reminder call (call type 2) was made to patients who had requested an FOBT kit but did not return it within 5 weeks from the date of request; those patients were given the opportunity to request an additional FOBT kit. All FOBT kits used the guaiac method (Hemoccult II; Beckman Coulter, Inc.), which required samples from 3 consecutive stools, and were delivered via standard mail.
Figure 2.
Type and Timing of Calls to Intervention Group
Usual Care
Patients randomized to usual care did not receive the telephone contact intervention. Their CRC screening, if any, occurred via normal care processes. At the time of the study, clinicians had access to national guidelines, Intranet-based screening guidelines, and a “panel support tool” (an electronic prompt system embedded in the electronic medical record that informed clinicians which patients were due for preventive services, including CRC screening). For usual care patients FOBT kits were obtained after a clinician order by either picking it up from the laboratory at the clinic where they received their care, or from the HMO’s influenza immunization service, located in primary care clinics.
Outcome measures
We used the HMO’s electronic data systems to identify patient outcomes. We specified two outcomes for the analysis; the cost per “any completed screen,” and the cost per “positive FOBT screen.” Even though the intervention promoted FOBT, we defined a “completed screen” as a patient with a record of any USPSTF recognized screening test (FOBT, flexible sigmoidoscopy, double contrast barium enema [DCBE], or colonoscopy) during follow-up. For both outcomes a patient was counted as screened only once, even if they had multiple tests; but as detailed below, costs for all screening tests during follow-up were included. We used the term ‘non-fecal tests’ to collectively refer to those more invasive testing methods including flexible sigmoidoscopy, DCBE, and colonoscopy. We examined the effect of the intervention on both FOBT and nonfecal tests separately.
Costs
We estimated staff costs associated with the intervention from clinical trial records and study staff time estimates. These costs included project management time to oversee the entire process, and computer programming efforts for patient identification, electronic file preparation for the automated telephone call vendor, and patient tracking (e.g. for repeat calls to nonresponders). To improve generalizability to other systems, salary costs were taken from the Bureau of Labor and Statistics.15 To fully allocate the costs we added a fringe benefit rate of 30% and overhead rate of 20%. The cost of the calls and their content was based on vendor charges. The cost of developing and maintaining the automated telephone system was embedded in the vendor charge to the HMO. FOBT kit mailing costs were estimated based on bulk mailing rates.
For patients in both groups, the costs associated with the FOBT testing kit, processing and reporting was estimated from the HMO’s laboratory charges to non-members. Clinician time and cost associated with FOBT laboratory result review and follow-up with patients was estimated from a previous economic evaluation in laboratory medicine16 and from interviews with those doing the work. Costs for other types of testing, including DCBE, flexible sigmoidoscopy, and endoscopy came from the HMOs accounting database. While a patient was counted as “screened” only one time, all CRC testing-related costs during the follow-up were enumerated and assigned to that patient. We did this because the intervention may have had knock-on effects for other types of colorectal cancer testing, including both diagnostic (e.g. following a positive FOBT) and screening (e.g. encouraging patient request for colonoscopy screening) and we wanted to more fully account for the economic consequences of the intervention. For example, if a patient was screened with FOBT at month 1 and then subsequently had a colonoscopy during month 8, the cost of both tests was counted in the 9-month analysis. We made no attempt to discern the clinical rationale for a given screening test (e.g. a screening vs. a diagnostic colonoscopy), rather we conservatively included all tests for both outcomes and costs. Usual care patients may have gotten their screening advice at an office visit, but we assumed CRC screening advice was unlikely to be the chief reason for visit, so we did not attempt to include those costs. Any resulting bias from that decision would make usual care appear less costly.
Clinical trial findings
In the clinical trial, the mean age in both groups was about 60 years, with an even female/male split. There were 2,943 patients in the intervention group, and 2,962 patients in the usual care group. In the intervention group, 22.5% completed FOBT within 6 months, compared with 16.0% in the UC group. Screening by any method was completed for 23.9% in the intervention versus 17.6% in the UC group. In the intervention group, 2943 (100%) received the initial call type 1 (general reminder), 2406 (81.8%) received a second type 1 call, and 1632 (55.5%) received a total of 3 calls of type 1. Call type 2 (FOBT return reminder) was made to 18.3% of the intervention group.
Statistical Analysis
We calculated the incremental cost-effectiveness ratio (ICER) as (costi – costc)/(effecti – effectc, where i = intervention, c = control, and effect = number of patients with a screening test. We used net benefit regression methods17-19 to estimate the intervention’s probability of being cost-effective. We report the probability of the intervention being cost-effective at several relevant thresholds of willingness to pay for an additional outcome (e.g. additional screen) to aid decision maker’s translation of the results to their own setting and specific considerations. We also computed bootstrapped 95% confidence intervals on total costs using the percentile method.
The parent clinical trial revealed a significant intervention effect that depended on patient age, so we undertook a similar subgroup analysis. As did the clinical trial, we followed patients for 6 months in our primary analysis. Since fecal screening is recommended annually the health plan encourages screening on that basis, so we additionally wanted to examine a time period more compatible with that interval. To accomplish this, and to avoid the potential overlapping effects from the next annual screening efforts, we undertook a secondary analysis and followed patients for completed tests up to 9 months after their index date. SAS [version 9.1] and STATA versions 10 and 11 were used for all analyses.
Results
Table 1 enumerates the resources necessary to implement and sustain the automated calling program in the intervention arm, and to carry out all types of CRC screening tests in both arms. Table 2 shows the resource use and average cost per person in both groups, at 6 and 9 months and by age. Accounting for the staff time associated with project management, computer programming, patient tracking and reporting, and the calls themselves, the intervention cost was about $4.20 per person.
Table 1.
Resource and Unit Costs
| Resource use category | Unit cost |
Source | Comment |
|---|---|---|---|
| Project management-related staff time (intervention group) |
$0.42 per person |
Clinical trial, HMO Costs, Bureau of Labor and Statistics |
Coordination effort required to maintain the program |
| Patient identification, tracking, and reporting-related staff time (intervention group) |
0.66 per person |
Clinical trial, HMO Costs, Bureau of Labor and Statistics |
Analyst time to write and maintain programs, transfer to phone vendor, reporting and tracking |
| Automated telephone call (intervention group) |
$0.54 per person |
Clinical trial | Estimated cost from in house vendor of phone messaging services |
| FOBT kit, including mailing to patient (intervention group patients that requested one; usual care group patients with a completed test) |
$0.84 per test |
Clinical trial | HMO non member charge |
| FOBT test processing (both groups) | $1.77 per test |
Laboratory charge |
HMO non member charge |
| Clinician follow-up for positive FOBT test (both groups) |
$12 per person |
Expert opinion | 5 minutes. Review chart, refer and contact patient for follow-up testing |
| DCBE (both groups) | $277 per test |
HMO Cost | Scheduling, performing and interpreting the test |
| Flexible sigmoidoscopy (both groups) | $374 per test |
HMO Cost | Scheduling, performing and interpreting the test |
| Endoscopy (both groups) | $745 per test |
HMO Cost | Scheduling, performing test interpretation |
Table 2.
Mean per patient costs at 6- and 9-month follow-up
| Type of service | Intervention group | Usual care group |
|---|---|---|
| All Ages | n=2943 | n=2962 |
| 6-month follow up | mean (sd) | mean (sd) |
| Intervention cost * | $4.2 ($0.4) | NA |
| FOBT testing and follow-up | $0.7 ($1.9) | $0.6 ($1.8) |
| Non-fecal tests** and follow-up | $32.1 ($142.7) | $33.8 ($148.4) |
| Total Cost (95% CI) | $37.0 ($31.9, $42.3) | $34.4 ($29.7, $39.8) |
| 9-month follow up | ||
| Intervention cost * | $4.2 ($0.4) | NA |
| FOBT testing and follow-up | $0.9 ($2.1) | $0.8 ($2.0) |
| Non-fecal tests** and follow-up | $46.9 ($178.8) | $49.1 ($180.8) |
| Total Cost (95% CI) | $52.0 ($45.7, $58.5) | $49.9 ($44.0, $56.4) |
|
| ||
| Age <70 years | n=2568 | n=2589 |
| 6-month follow up | mean (sd) | mean (sd) |
| Intervention cost * | $4.1 ($0.4) | NA |
| FOBT testing and follow-up | $0.7 ($1.8) | $0.5 ($1.7) |
| Non-fecal tests** and follow-up | $33.2 ($145.4) | $34.4 ($150.8) |
| Total Cost (95% CI) | $37.9 ($32.7, $44.1) | $34.9 ($28.7, $40.8) |
| 9 month follow-up | ||
| Intervention cost * | $4.1 ($0.4) | NA |
| FOBT testing and follow-up | $0.8 ($2.0) | $0.7 ($1.9) |
| Non-fecal tests** and follow-up | $48.7 ($182.6) | $49.2 ($181.2) |
| Total Cost (95% CI) | $53.6 ($46.5, $60.5) | $49.9 ($41.9, $56.1) |
|
| ||
| Age 70 years and older | n=375 | n=373 |
| 6 month follow-up | mean (sd) | mean (sd) |
| Intervention cost * | $4.3 ($0.4) | NA |
| FOBT testing and follow-up | $1.3 ($2.4) | $0.8 ($2.2) |
| Non-fecal tests** and follow-up | $24.6 ($122.5) | $30.0 ($130.5) |
| Total Cost (95% CI) | $30.1 ($17.9, $43.0) | $30.8 ($18.7, $46.9) |
| 9 month follow-up | ||
| Intervention cost * | $4.3 ($0.4) | NA |
| FOBT testing and follow-up | $1.5 ($2.6) | $1.2 ($2.5) |
| Non-fecal tests** and follow-up | $34.6 ($150.3) | $48.7 ($178.9) |
| Total Cost (95% CI) | $40.4 ($26.6, $55.0) | $49.9 ($32.0, $67.9) |
includes all components needed to deliver the intervention
endoscopy, DCBE, flexible sigmoidoscopy
FOBT = fecal occult blood testing
For patients of all ages, the average cost per patient for FOBT testing (kits and their processing) was slightly higher in the intervention group while the per-patient cost associated with non-fecal tests (endoscopy, DCBE, and flexible sigmoidoscopy) were slightly higher in the usual care group. We found that the number of FOBT tests completed at 9 months was markedly higher in the intervention group (e.g. 812 vs. 669). On the other hand, we observed similar overall proportions of patients with non-fecal tests (3.2% intervention and 3.0% usual care, data not shown). But there were differences by age; for patients aged 70 years and over there were 5.6 non-fecal tests per 100 persons in the intervention group compared to 7.8 per 100 in usual care. However, for patients aged <70 years non-fecal test use was similar in both group (7.9 and 8.0 non-fecal tests per 100 persons in the intervention and usual care groups, respectively). FOBT increased in both age groups, but the FOBT increase was greater in the older age group (45 per 100 intervention and 33 per 100 control) than for those at younger ages (25 per 100 intervention and 21 per 100 control). As shown in Table 2, these observed differences by age in the use of FOBT and non-fecal tests translated into notable differences in costs at both 6 and 9 months. For example, at 9 months the average cost of FOBT and non-fecal tests were similar for patients aged <70 years in the intervention and usual care groups. However, at 9 months, for patients aged 70 years and over, the costs of FOBT were 25% higher in the intervention group ($1.50 vs $1.20), while the costs for non-fecal tests were more than 40% lower in the intervention group ($34.60 vs. $48.70). While these component costs showed some variation, total costs were similar in both groups as evidenced by the overlapping confidence limits.
Table 3 shows the cost-effectiveness at 6 and 9 months by age using each of the two measures of effectiveness: ‘any completed screen’ analysis, and the ‘positive FOBT screen.’ Overall, we found that the cost for an additional screened patient was $42 at 6 months and $40 at 9 months. At 6 months, the chance of the intervention being cost effective was about 50% at a willingness to pay of $40 for an additional patient screened. It increased to 84% for a willingness to pay of $100, and 99% for a willingness to pay of $200.
Table 3.
Incremental Cost Effectiveness per 100 patients at 6- and 9-month post-intervention: Any Completed Screen* and Positive FOBT Screen
| Total cost |
Total screens |
Incremental costs |
Incremental screens |
ICER | Probability of cost- effectiveness for maximum willingness to pay |
|||
|---|---|---|---|---|---|---|---|---|
|
6 months post
intervention |
||||||||
| Any Completed Screen Analysis | $40 | $100 | $200 | |||||
| Intervention group |
$3,701 | 25.076 | ||||||
| Usual care group | $3,438 | 18.805 | $263 | 6.27 | $42 | 0.49 | 0.84 | 0.99 |
| Age 70 and older | ||||||||
| Intervention group |
$3,014 | 38.667 | ||||||
| Usual care group | $3,084 | 24.397 | −$69 | 14.27 | Intervention Dominant |
0.75 | 0.97 | 1.00 |
| Age <70 | ||||||||
| Intervention group |
$3,793 | 22.555 | ||||||
| Usual care group | $3,449 | 17.860 | $344 | 4.69 | $73 | 0.35 | 0.64 | 0.95 |
| Positive FOBT Screen | ||||||||
| Intervention group |
$3,701 | 1.053 | ||||||
| Usual care group | $3,438 | 1.047 | $263 | 0.006757 | $38,924 | NC | NC | NC |
|
| ||||||||
|
9 months post
intervention |
||||||||
| Any Completed Screen Analysis | $40 | $100 | $200 | |||||
| Intervention group |
$5,196 | 30.751 | ||||||
| Usual care group | $4,990 | 25.625 | $206 | 5.13 | $40 | 0.51 | 0.76 | 0.97 |
| Age 70 and older | ||||||||
| Intervention group |
$4,036 | 46.400 | ||||||
| Usual care group | $4,990 | 34.316 | -$954 | 12.08 | Intervention Dominant |
0.88 | 0.97 | 1.00 |
| Age <70 | ||||||||
| Intervention group |
$5,337 | 27.984 | ||||||
| Usual care group | $4,875 | 24.194 | $462 | 3.79 | $122 | 0.26 | 0.42 | 0.74 |
|
|
||||||||
| Positive FOBT Screen | $1,000 | $3,000 | $7,000 | |||||
| Intervention group |
$5,196 | 1.495 | ||||||
| Usual care group | $4,990 | 1.317 | $206 | 0.18 | $1,156 | 0.47 | 0.64 | 0.70 |
The Any Completed Screen analysis counts any type of screening (i.e. FOBT, DCBE, flexible sigmoidoscopy, or colonoscopy) as a successful screen.
The FOBT Screen analysis counts only FOBT as a successful screen
Patients could have had more than one screen, but only the first test per person was counted as a successful screen
Costs included all types of CRC screening (FOBT, DCBE, flexible sigmoidoscopy, or colonoscopy) undertaken during followup
NA = not applicable
NC = not calculated
The intervention was dominant (i.e. lower costs with a greater proportion of patients screened) at 6 months for patients aged 70 years or more, but had an ICER of $73 for younger patients. Both age groups had a high probability (>=95%) of being cost effective at a willingness to pay of $200 for an additional screened patient at 6 months, but were markedly different at willingness to pay thresholds of $100 (0.97 and 0.64 for older vs. younger patients, respectively) and $40 (0.75 and 0.35 for older vs. younger patients, respectively). We found a similar pattern of results at 9 months.
The cost per additional positive FOBT screen was $1,156 at 9 months. The probability of cost-effectiveness was 0.47 at a willingness to pay of $1,000 and increased to 0.70 at a willingness to pay of $7,000.
Discussion
We found that, depending on one’s willingness to pay for an additional screen, automated telephone calls can be cost-effective. For example, at a willingness to pay of $100 per additional screen, the probability of cost-effectiveness is 0.84 and increases to near-certainty (0.99) at a willingness to pay of $200 per additional screen. But at lower willingness to pay levels (i.e. $40 per additional screen) there is considerable uncertainty in the cost-effectiveness (probability of being cost effective = 0.49).
A recent systematic review2 noted that, compared to no screening, all types of colorectal cancer screening are cost-effective at common thresholds (e.g. $50,000 per year of life gained) and some are even estimated to be cost-saving. Our study focused on the cost and cost-effectiveness of using automated telephone calling to promote FOBT screening relative to usual care. We found that automated calls were low-cost and compare favorably with other reported CRC screening programs at about $40 per additional patient screened, with any test. For example, a recent report5 reviewed several studies that analyzed the cost-effectiveness of comparable interventions to increase CRC screening. Those authors noted that the cost per additional patient screened ranged from more than $6,000 to $94 for a range of interventions including physician communication training and patient education, physician feedback, and patient mailings. Our intervention differed from previous interventions in several important ways that may have had a direct effect on the differential program costs. First, we did not send stool cards unless the patient requested the kit. By requiring a patient request prior to mailing a kit (and thus prior to incurring associated costs) a relatively costly component of the intervention was avoided by presumably targeting those patients most likely to complete testing. Additionally, by requiring a patient ‘commitment’ (i.e. positive response to the call) the intervention potentially further enhanced patient follow-through. Our results suggest that future reviews on this topic might usefully compare the costs and cost-effectiveness of patient-directed versus provider-directed interventions, and consider whether automated systems are more cost-effective, perhaps in a stepped approach.
Overall we found that the cost of an additional test was about $40 at both 6 and 9 months, but the intervention’s cost effectiveness differed markedly by age. We found that among patients aged 70 years and greater, automated calls were associated with higher screening rates and lower costs (about $0.69 lower per patient at 6 months and about $10 lower per patient at 9 months). Because we counted all screening costs during the follow-up interval, this suggests that older patients who received the automated calls were more likely to choose FOBT over non-fecal tests. While the overall frequency was small, we did find that among patients 70 years and older, fewer patients in the intervention arm received non-fecal tests compared to usual care. The intervention was associated with an apparent substitution effect (i.e. FOBT for non-fecal tests). It is known that non-fecal tests have better test performance characteristics (e.g. greater sensitivity and specificity) than does FOBT14 and thus FOBT might be used preferentially for lower risk patients. Therefore one question that arises with the potential substitution effect of FOBT for non-fecal tests is whether the automated telephone intervention is enhancing screening, but among lower risk patients only. To further explore the possibility, we examined whether the rate of positive tests differed between the intervention and usual care groups. Automated results were only available for FOBT. Among patients aged 70 years and older, we found that 5.39% of the treatment group’s FOBTs and 7.26% of the usual care group’s FOBT were positive at 9 months, (p>0.5) while 5.43% and 5.50% (intervention and usual care, respectively) FOBT’s were positive for younger patients (p>0.9). So while we did find that older patients in the intervention group who screened with FOBT were potentially at a lower CRC risk, the large p-value suggests that finding was due to chance, although we may have been underpowered for this exploratory subgroup analysis. An important caveat is that the trial was not designed to assess this issue, but it does suggest a possible future direction for study. Such a study might use survey or qualitative methods. We also note that our findings take on a short-term perspective, namely <1 year. This distinction is relevant because a longer-term perspective would take account of the longer recommended time interval of the colonoscopy for screening (e.g. up to 10 years) compared with fecal screening (e.g. annually).
Our finding that the automated phone intervention is more effective in older patients has been noted in other studies,8 and is also consonant with cost-effectiveness findings from previous CRC screening analyses.5 The increased rate of screening of among older patients highlights that the intervention’s promotion of FOBT screening makes CRC screening more readily accessible to a segment of the population that may find it difficult to arrange for non-fecal tests, or may have comorbidities that contraindicate non-fecal screening.
Our intervention was carried out in a health system with an electronic medical record (EMR) that was an integral part of the program’s patient identification scheme. Specifically, the HMOs automated systems were used to target patients who were age appropriate and due for CRC screening by examining databases of health care encounters for tests and procedures that patients had previously received. While the intervention and patient identification would likely work most efficiently in a similar system, the existence of an EMR is not critical, but access to electronically stored data may be critical. For example, a claims-based health care insurer would be able to search for candidate patients using claims consistent with receipt of screening, and couple that their enrollment files to achieve a similar result. The scalability of the intervention is also important. As the number of patients called increases, the marginal cost per patient decreases, leading to even greater efficiency gains. Likewise, fewer patients would lead to higher marginal costs and decreased efficiency.
Our study’s strengths include being conducted as part of a randomized trial and being embedded in an integrated health care system, allowing us detailed electronic capture of the health care resources involved in the intervention. On the other hand, the sample size and follow-up time restricted the ability to observe long-term outcomes such as cancer cases and deaths. However, a trial that could answer questions with those final outcomes would be expensive and very lengthy. Also, while our study did employ tactics aimed at increasing CRC screening with a US Preventive Services Task Force recommended screening modality, namely FOBT, our findings do not speak to interventions that promote other screening methods, or use other types of interventions (e.g. physician directed interventions). Additionally, our analysis was limited to the cost per additional screen and we did not consider possible changes in quality of life or costs associated with cancer detection and treatment. Our approach assumes that, because CRC screening is cost-effective at common thresholds, finding the most cost-effective testing strategy will lead to an economically attractive screening strategy; this assumption may not hold for all populations and situations. Depending on one’s willingness to pay for an additional patient screened, automated telephone calls which prompt interested patients to request an FOBT kit and then remind those who requested a kit to return the kit can be a cost effective method to promote CRC screening. Furthermore, compared with reports of other methods, the cost per patient screened are lower with automated calls. In particular, we found automated calling is associated with lower costs and improved screening rates in older patients, mainly through a decrease in the use of comparatively more expensive non-fecal tests. Our work adds to the growing literature showing the clinical utility and economic benefits of combining health information technology and medical record information to promote healthy behaviors.
Acknowledgment
We thank Mary Rix and Lucy Fulton for their work on this project, as well as the many staff at KPNW who helped with data collection.
Reference List
- (1).Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Cronin K, Chen HS, Feuer EJ, Stinchcomb DG, Edwards BK, editors. World Wide Web. National Cancer Institute; Bethesda, MD: 2010. SEER Cancer Statistics Review, 1975-2007. http://seer.cancer.gov/csr/1975_2007/ based on November 2009 SEER data submission, posted to the SEER web site. [Google Scholar]
- (2).Lansdorp-Vogelaar I, Knudsen AB, Brenner H. Cost-effectiveness of colorectal cancer screening - An overview. Best Practice & Research Clinical Gastroenterology. 2010;24:439–449. doi: 10.1016/j.bpg.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).Sun Hee Rim, Joseph Djenaba A, Steele Brooke, Thompson Trevor D, Seeff Laura C. Colorectal Cancer Screening --- United States, 2002, 2004, 2006, and 2008. MMWR Morb Mortal Wkly Rep. 2011;60:42–46. [PubMed] [Google Scholar]
- (4).Lairson DR, DiCarlo M, Myers RE, et al. Cost-effectiveness of targeted and tailored interventions on colorectal cancer screening use. Cancer. 2008;112:779–788. doi: 10.1002/cncr.23232. [DOI] [PubMed] [Google Scholar]
- (5).Sequist TD, Franz C, Ayanian JZ. Cost-effectiveness of patient mailings to promote colorectal cancer screening. Med Care. 2010;48:553–557. doi: 10.1097/MLR.0b013e3181dbd8eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (6).Wolf MS, Fitzner KA, Powell EF, et al. Costs and Cost Effectiveness of a Health Care Provider-ûDirected Intervention to Promote Colorectal Cancer Screening Among Veterans. J Clin Oncol. 2005;23:8877–8883. doi: 10.1200/JCO.2005.02.6278. [DOI] [PubMed] [Google Scholar]
- (7).Khankari K, Eder M, Osborn CY, et al. Improving colorectal cancer screening among the medically underserved: a pilot study within a federally qualified health center. J Gen Intern Med. 2007;22:1410–1414. doi: 10.1007/s11606-007-0295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Feldstein AC, Smith DH, Perrin N, et al. Improved therapeutic monitoring with several interventions: a randomized trial. Arch Intern Med. 2006;166:1848–1854. doi: 10.1001/archinte.166.17.1848. [DOI] [PubMed] [Google Scholar]
- (9).Mosen DM, Feldstein AC, Perrin N, et al. Automated Telephone Calls Improved Completion of Fecal Occult Blood Testing. Med Care. 2010 doi: 10.1097/MLR.0b013e3181dbdce7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Vollmer WM, Kirshner M, Peters D, et al. Use and impact of an automated telephone outreach system for asthma in a managed care setting. Am J Manag Care. 2006;12:725–733. [PubMed] [Google Scholar]
- (11).Forster AJ, van WC. Using an interactive voice response system to improve patient safety following hospital discharge. J Eval Clin Pract. 2007;13:346–351. doi: 10.1111/j.1365-2753.2006.00702.x. [DOI] [PubMed] [Google Scholar]
- (12).Meenan R, Stevens V, Hornbrook M, et al. Cost-effectiveness of a hospital-based smoking cessation intervention. Med Care. 1998;36:670–678. doi: 10.1097/00005650-199805000-00007. [DOI] [PubMed] [Google Scholar]
- (13).Bureau-of-Labor-and-Statistics Handbook of Methods: Chapter 17: The Consumer Price Index. 2012. 2-28-2012.
- (14).Whitlock EP, Lin JS, Liles E, Beil TL, Fu R. Screening for colorectal cancer: a targeted, updated systematic review for the U. S. Preventive Services Task Force. Ann Intern Med. 2008;149:638–658. doi: 10.7326/0003-4819-149-9-200811040-00245. [DOI] [PubMed] [Google Scholar]
- (15). [accessed November, 2010];OCCUPATIONAL EMPLOYMENT AND WAGES. 2009 May; http://www.bls.gov/news.release/pdf/ocwage.pdf. 2009.
- (16).Smith DH, Feldstein AC, Perrin NA, et al. Improving laboratory monitoring of medications: an economic analysis alongside a clinical trial. Am J Manag Care. 2009;15:281–289. [PubMed] [Google Scholar]
- (17).Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Economics. 2002;11:415–430. doi: 10.1002/hec.678. [DOI] [PubMed] [Google Scholar]
- (18).Hoch JS, Rockx MA, Krahn AD. Using the net benefit regression framework to construct cost-effectiveness acceptability curves: an example using data from a trial of external loop recorders versus Holter monitoring for ambulatory monitoring of “community acquired” syncope. BMC Health Serv Res. 2006;6:68. doi: 10.1186/1472-6963-6-68. 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Hoch JS. Improving efficiency and value in palliative care with net benefit regression: an introduction to a simple method for cost-effectiveness analysis with person-level data. J Pain Symptom Manage. 2009;38:54–61. doi: 10.1016/j.jpainsymman.2009.04.010. [DOI] [PubMed] [Google Scholar]