Abstract
Purpose
The receptor for advanced glycation end products (RAGE) contributes to multiple pathologies, including diabetes, arthritis, neurodegenerative diseases, and cancer. Despite the obvious need, no RAGE inhibitors are in common clinical use. Therefore, we developed a novel small RAGE antagonist peptide (RAP) which blocks activation by multiple ligands.
Experimental Design
RAGE and its ligands were visualized by immunohistochemical analysis of human pancreatic tissues, and siRNA was used to analyze their functions. Interactions between RAGE and S100P, S100A4, and HMGB-1 were measured by ELISA. Three S100P-derived small antagonistic peptides were designed, synthesized, and tested for inhibition of RAGE binding. The effects of the peptide blockers on NFκB-luciferase reporter activity was used to assess effects on RAGE mediated signaling. The most effective peptide was tested on glioma and pancreatic ductal adenocarcinoma (PDAC) models.
Results
Immunohistochemical analysis confirmed the expression of RAGE and its ligands S100P, S100A4, and HMGB-1 in human PDAC. siRNA silencing of RAGE or its ligands reduced the growth and migration of PDAC cells in vitro. The most effective RAGE antagonistic peptide (RAP) inhibited the interaction of S100P, S100A4, and HMGB-1 with RAGE at micromolar concentrations. RAP also reduced the ability of the ligands to stimulate RAGE activation of NFκB in cancer cells in vitro and in vivo. Importantly, systemic in vivo administration of RAP reduced the growth and metastasis of pancreatic tumors and also inhibited glioma tumor growth.
Conclusion
RAP shows promise as a tool for the investigation of RAGE function and as an in vivo treatment for RAGE-related disorders.
Keywords: Pancreatic cancer, RAGE, RAP, S100P, Bioluminescence
Introduction
The receptor for advanced glycation end products (RAGE) is a multi-ligand receptor of the immunoglobulin superfamily that is expressed in all tissues (1–3). First described as a receptor for advanced glycation end-products (AGEs), which are products of the non-enzymatic glycation and oxidation of proteins, RAGE also responds to several molecules released during periods of acute and chronic stress (1–3). Non-AGE ligands of RAGE include members of the S100 family, high mobility group box 1 peptide (HMGB-1, also called amphoterin), and amyloid-β peptide (1–4). Binding of these ligands to RAGE activates key cell signaling pathways, including MAP kinase and nuclear factor NFκB pathways (1, 5). Consistent with its interactions with this group of disease-related ligands, RAGE has been confirmed to contribute to the pathogenesis of cancer, diabetes mellitus, Alzheimer’s disease, arthritis, and other acute and chronic inflammatory disorders (1–4).
Translational Relevance.
RAGE is a key molecule in several important pathologies, including diabetes, Alzheimer’s disease, sepsis, arthritis, and cancer. Blocking RAGE-ligand interaction is clinically beneficial, but there are currently no drugs available for this purpose. We have developed a small peptide antagonist, RAGE antagonistic peptide (RAP), that prevents RAGE from binding with several of its most important ligands, including HMGB-1, S100P, and S100A4. The current study also evaluated whether RAP could achieve relevant levels of inhibition in vivo. We showed that systemic administration to orthotopic tumors resulted in the inhibition of tumor growth and metastasis. Therefore, this peptide should be useful for the study of RAGE in various diseases. RAP may itself be a useful treatment for several diseases involving RAGE, although more study is needed to verify this.
In preclinical models, RAGE has been inhibited using several approaches, including expression of a dominant-negative truncated receptor (6), treatment with a RAGE-blocking antibody (7), treatment with a 33 amino acid antagonistic peptide derived from HMGB-1 (8), treatment with cromolyn (9), gene silencing with anti-sense oligonucleotides, and treatment with a truncated form of RAGE called sRAGE (10). sRAGE, a synthetic version of a naturally occurring secreted form of the receptor that sequesters RAGE ligands, has been most studied in this regard. Administration of sRAGE was shown to suppress the growth of tumor cells in animal studies (6), improve outcomes in diabetes (11, 12), and block the transport of amyloid-β across the blood-brain barrier (13). These preclinical studies support the hypothesis that blocking RAGE activation will be useful as a treatment in a variety of pathologies. However, none of these current strategies has become available clinically.
As an approach to developing a RAGE inhibitor that would be useful in vivo, we tested small peptide antagonists. In this study, we show that a ~1kD peptide RAP binds RAGE and blocks its activation by a variety of ligands in vitro and in vivo. RAP blocked S100P, S100A4, and HMGB-1-mediated activation of RAGE in vitro and in vivo and inhibited tumor growth and metastasis. These data support the proposition that RAP can be used to further investigate the involvement of RAGE in disease and is a potential novel therapeutic peptide for the treatment of various cancers and other RAGE-mediated pathologies.
Material and Methods
Cell Lines
All cell lines were obtained from the American Type Culture Collection (Manassas, VA). Cell line identities were verified using DNA fingerprinting (Powerplex16 system, Promega, WI). Cells were routinely cultured in recommended media. All cells were maintained at 37°C in a humidified atmosphere of 5% CO2.
SiRNA Transfection
Cells in 6-well plates were grown to 70–80% confluence and transfected with double-stranded siRNA (Qiagen Inc, CA) for RAGE (SI00022393) S100P (SI03246677), S100A4 (SI00709667) and HMGB-1 (SI02627828) or with a control siRNA (SI03650318) in serum-free medium without antibiotic supplements using HiPerFect Transfection Reagent (Qiagen Inc. CA). Cells were incubated under these conditions for 72 hrs and silencing was then confirmed by western blotting.
Western blotting
Protein lysate from control and target SiRNA trasnfected cells were prepared, and protein concentrations were measured by Bio-Rad reagent. Protein (50 µg) was loaded onto 10% (RAGE) and 15% (S100P, S100A4 and HMGB-1) SDS-PAGE gels, and Western blot was conducted using primary antibody against S100P (0.1µg/ml, R&D Systmes, MN), S100A4 (1:100 dilution, DakoCytomation, CA), HMGB-1 (1:1000 dilution, Abcam, CA) and RAGE (1:200 dilution, Millipore, MA) The same blot was probed GAPDH (0.5µg/ml, R&D Systems, MN) and E-Cadherin (1:100 dilutions, BD Biosciences, NJ) which served as loading control for the experiment. Precision plus protein standards (Bio-Rad, CA) served as molecular weight markers. Western blot imaging and processing were done with Odyssey machine (LiCor BioScience, NE).
Peptide Antagonists
Previously the specific amino acid sequence between 150–183 of COOH-terminal motif in HMGB-1 was reported to be similar to the sequence of some members of the S100 family and responsible for RAGE binding (8). This 33 a.a. peptide competitively blocked the binding of HMGB-1 with RAGE and had anti-cancer effects in an experimental metastasis study. In the current study, we compared the HMGB-1 blocking peptide sequence with the sequence of S100P and observed a similarity in amino acid sequence and pattern between the first 40 a.a. of S100P and the 33 a.a RAGE binding peptide derived from HMGB-1. Based on this similarity, we designed and synthesized 3 peptides from the sequence of S100P (elkvlmekelkelpgflqsgkdkd, and gkdkdavdkllkd) with 95% purity (CPC Scientific, CA). These peptides were designed with the amino terminus blocked by amidation and the carboxyl terminus by acetylation to improve peptide stability.
Mice
Four-week-old male athymic nude mice were acquired from (NCI). All animals were maintained in a sterile environment according to the institutional animal welfare guidelines. Cages, bedding, food, and water were all autoclaved. All animals were maintained on a daily 12-hr light/12-hr dark cycle. Each group consisted of five animals.
Immunohistochemical staining
Unstained 4 µm sections of clinical specimens were deparaffinized with xylene and rehydrated with ethanol. Immunohistochemistry used RTU Vectastain Elite ABC Universal kit (Vector Laboratories, Burlingame, CA) according to the manufacturer's instructions. Primary antibodies against S100P, RAGE (R&D Systems, MN), S100A4 and HMGB-1 (Abcam, MA) was diluted 1:250 in 2% bovine serum albumin/0.2% Triton in PBS. Finally, slides were developed with 3,3-diaminobenzidine substrate counterstained with hematoxylin, dehydrated with ethanol, fixed with xylene, and mounted.
Cell Growth and Migration Studies
Pancreatic cancer cells (MPanc96, MOH, HPAF II, and BxPC-3) were plated on 100-mm dishes and transiently transfected with siRNAs against RAGE, S100P, S100A, HMGB-1, and siControl at a final concentration of 10 nmol/L (Qiagen, CA) with HiPerFect transfection reagent (Qiagen, CA), and silencing was confirmed by quantitative reverse transcriptase polymerase chain reaction (qRT-PCR). Cell growth was analyzed using MTS reagent (Promega, WI) according to the manufacturer's directions. Pancreatic cancer cells (10,000 cells/well) transiently transfected with siControl or target siRNAs were plated on 96-well plates and grown in medium containing 10% serum. Different pancreatic cancer cells were plated (10,000 cells/well), and RAP and control peptide (10 µM) were added daily for 3 days. Cell numbers were estimated after 72 h by adding MTS to the wells 1 h before taking the photometric reading. For studies of cell migration, siRNA-transfected cell suspensions in serum-free culture medium (1×104 cells/100 µL top solution) were pipetted into the inserts of Transwell cell migration plates, and the inserts were transferred into the wells. For peptide treatment studies, cells were seeded on the insert and RAP or control peptide were added. For control assays, the bottom well was filled with 10% serum-containing medium and serum-free medium. The plates were incubated in a humidified CO2 incubator at 37°C for 8 h. The top solution was then removed, the cells on the top membrane surface were gently scraped with a cotton swab, and the cells on the bottom surface were counted after staining with hemotoxylin.
S100P, S100A4, and HMGB-1 Binding Study
Recombinant S100P (14), S100A4 and HMGB-1 proteins (R&D Systems, MN), S100P monoclonal antibody (R&D Systems, MN), S100A4 and HMGB-1 antibody (Abcam, MA), and an ELISA kit (KPL, MD) were used in to develop an ELISA-based assay to determine the binding of S100P with its receptor RAGE. Briefly, sRAGE (6) (5 µg/mL) was coated onto an ELISA plate by using an antigen coating solution for 1 h at room temperature; non-specific binding sites were blocked by incubating the plate in 1% BSA solution. Different concentrations of ligands with and without RAP were incubated in sRAGE-coated wells for 1 h, and unbound molecules were removed by washing with wash solution. Bound S100P, S100A4, and HMGB-1 were detected with horseradish peroxidase-labeled anti-S100P, S100A4, and HMGB-1 secondary antibodies and 3,3',5,5'-tetramethylbenzidene substrate. Color development was blocked with 1 M phosphoric acid and read at 450 nm.
Luciferase Assay for NFκB Activity
In vitro, BxPC-3 cells stably expressing a Lenti-NFκB-luc reporter construct (9) were treated with S100P alone or in combination with RAP for 5 h. D-luciferin (150 µg/mL) was added to the cells, and luciferase activity was measured using an IVIS bioluminescence system (Caliper Life Sciences, MA).To measure NFκB promoter activity in vivo, BxPC-3 cells (200,000/50 µL) stably expressing an NFκB-luc reporter were injected orthotopically into the pancreas of 4-week-old male nude mice. After 2 weeks, mice were injected intraperitoneally with D-luciferin (150 mg/kg), and basal NFκB activity was determined using the IVIS system. Subsequently, mice were injected with RAP (100 µg/day) intratumorally or intraperitoneally, and NFκB luciferase activity was reanalyzed after 5 h.
Tumor Growth and Invasion Study in Nude Mice
Subcutaneous glioma model
The anti-tumorigenic capability of RAP was assessed in mice by using a luciferase gene stably expressing rat C6-glioma cells. Luciferase-labeled C6-glioma cells (1x104/100 µL) were injected subcutaneously, and control and RAP peptide (100 µg/day/i.p.) were injected for another 3 weeks. At the end of the experiment, tumor growth was analyzed by bioluminescence imaging.
Pancreatic orthotopic model
The anti-tumorigenic capability of RAP was assessed in the mice by using a luciferase gene stably expressing highly aggressive MPanc96 cells. Luciferase-labeled Mpanc96 cells (2x105/50 µL) were injected into the pancreas. Bioluminescent imaging was utilized to estimate tumor volume after 1 week, and the animals were divided into two groups of five animals per group such that the mean tumor size was equal among the groups. For the next 4 weeks, group I animals were treated intraperitoneally with control peptide (100 µg/day) and group II animals were treated with RAP (100 µg/day). At the end of the experiment, the animals were sacrificed, tumor weight was measured and tumor volume and invasion of the liver were assessed by bioluminescence imaging.
Statistical Analysis
Data are presented as mean ± standard error of the mean. All in vitro experiments were repeated at least three times (n=3). For in vivo studies we used five animals per group (n=5). Statistically significant differences were determined by using the unpaired t test. When more than two groups were analyzed, ANOVA was used to analyze the data and the Newman-Keuls multiple comparison test was utilized to check the post-test significance. Statistical significance was defined as p < 0.05. Results were compared using GraphPad Prism 4 software.
Results
Pancreatic Cancer Cells Express and are Stimulated by RAGE and its Ligands S100P, S100A4, and HMGB-1
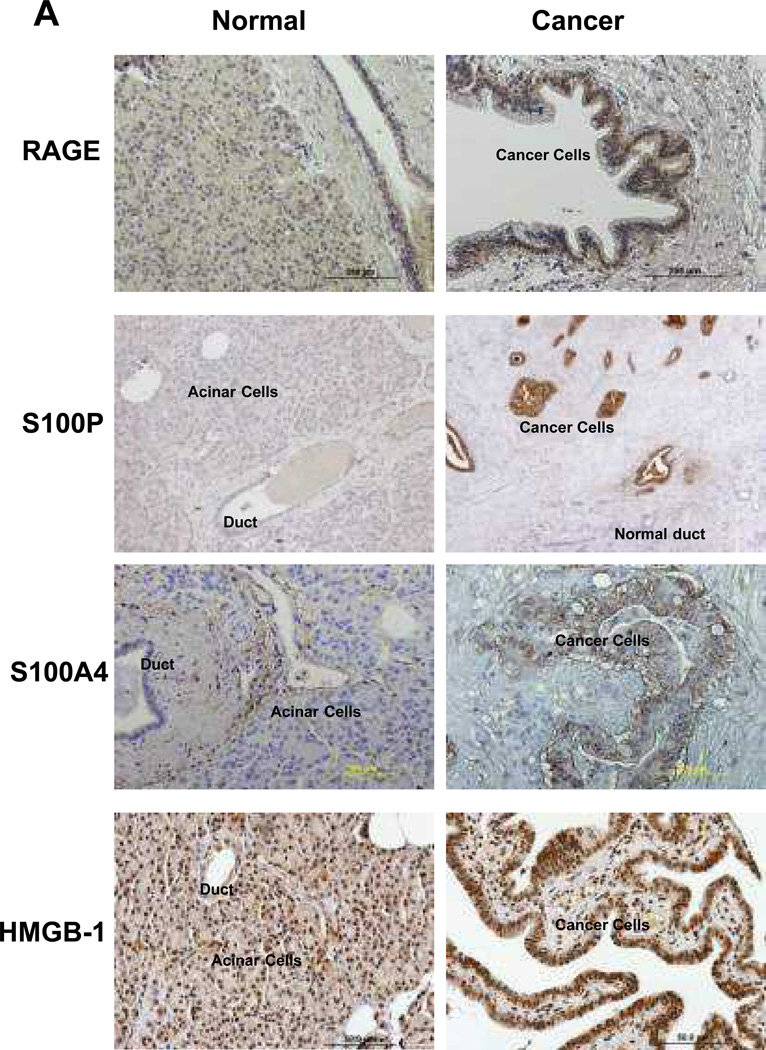
We and others have previously reported that mRNAs for RAGE, S100P, S100A4, and HMGB-1 are specifically expressed in pancreatic ductal adenocarcinoma (PDAC) tissue (1, 5). In the current study, RAGE, S100P, S100A4, and HMGB-1 protein expression in human tissues was evaluated by immunohistochemical analysis. S100P was very specifically present in cancer cells but not in normal cells; 92% (92/100) of pancreatic cancer patient tissue samples possessed S100P (Fig. 1A). S100A4 was also specifically expressed in cancer when compared with normal ducts, but immune and stromal cells in cancer tissue also expressed S100A4. RAGE and HMGB-1 were expressed in both normal and cancer cells. SiRNAs were used to reduce the protein levels for RAGE and its ligands in PDAC cells (Fig.1B). Silencing of the constitutively released RAGE ligands, S100P and S100A4, significantly reduced the growth of PDAC cell lines (Fig. 1C). In contrast, silencing of HMGB-1, which is not constitutively released by these cells, had no effect on their growth in vitro.
Fig. 1. Pancreatic cancer cells expressed and were stimulated by RAGE and its ligands S100P, S100A4, and HMGB-1.
(A) Immunohistochemical analysis of RAGE, S100P, S100A4, and HMGB-1 in normal and PDAC tissues showed the specific expression of S100P and S100A4 in cancer cells but not in normal cells. RAGE and HMGB-1 were expressed in both normal and cancer cells, but their expression was more prominent in cancer cells. (B). Silencing efficiency of SiRNAs for RAGE, S100P, S100A4 and HMGB-1 were confirmed by western blotting. (Full-length gels are shown in supplementary figure (S1). (C) Silencing of S100P or S100A4 but not HMGB-1 reduced the growth of Mpanc96, MOH, and HPAF II pancreatic cancer cells. Results shown are means +/− SEM for 3 independent experiments. *=p<0.05
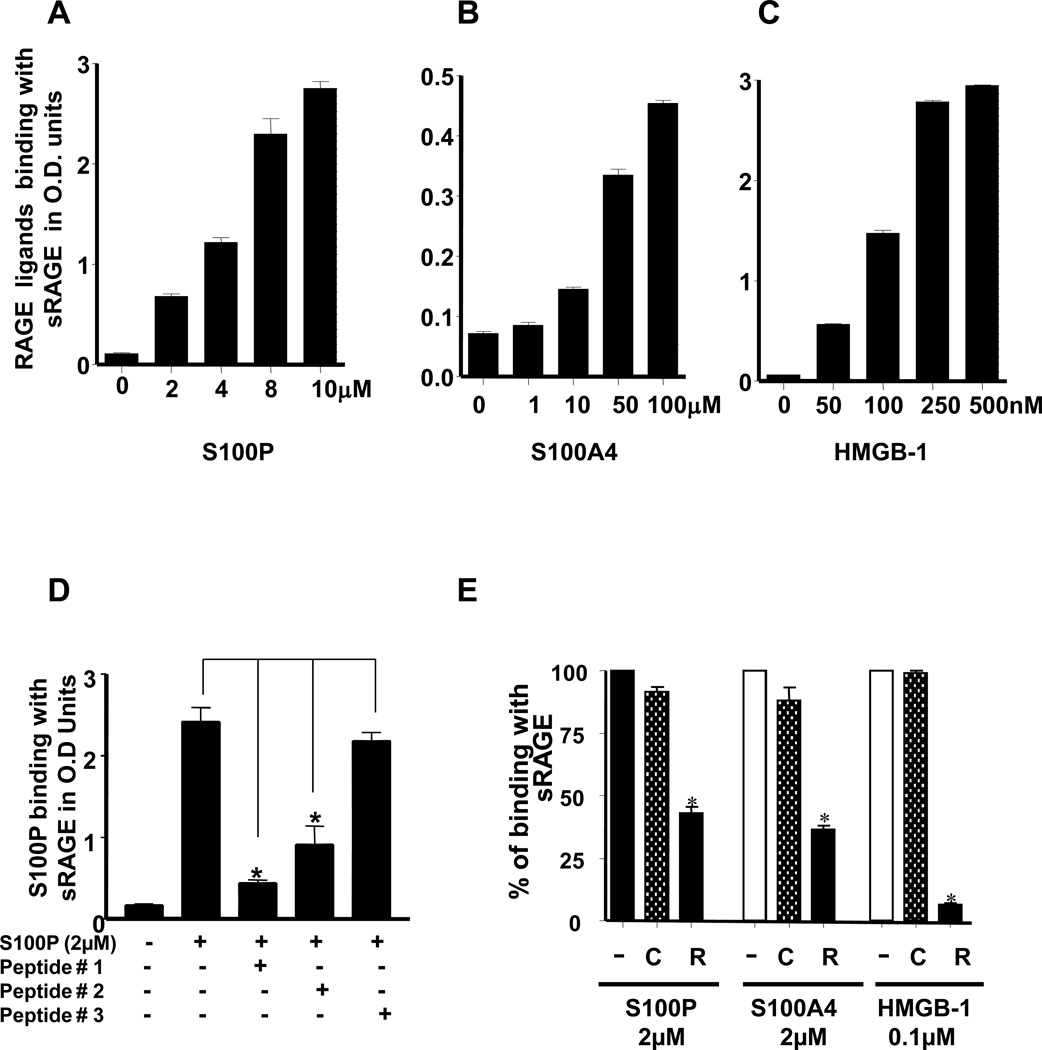
Small Peptides Based on the Structure of S100P Block the Binding of Multiple Ligands to RAGE
A cell-free ELISA was developed to screen peptides for the ability to block ligand binding with RAGE. Recombinant sRAGE, a secretory form of the extracellular portion of RAGE, was coated onto ELISA plates, and the binding of specific RAGE ligands was quantified using an anti-IgG-HPR antibody. In this assay, S100P, S100A4, and HMGB-1 bound with RAGE in a concentration-dependent manner with HMGB-1 showing the highest affinity of binding (Fig. 2A-C).
Fig. 2. RAGE binding of S100P, S100A4, and HMGB-1 was inhibited by an S100P-derived RAGE antagonistic peptide (RAP).
(A-C) In ELISA-based assays, S100P, S100A4 , and HMGB-1 each bound with RAGE in a concentration-dependent manner. (D) The effects of S100P-based small antagonistic peptides (10µM) on the binding of S100P with RAGE were examined. Peptide #1 Elkvlmekel (renamed RAP) inhibited the binding of S100P nearly to control levels and was superior to peptides #2 and #3. (E). RAP (10µM) inhibited the binding of S100P, S100A4, and HMGB-1 with RAGE. Results shown are means +/− SEM for 3 independent experiments. *=p<0.05.
We then analyzed the effects of three small peptides (elkvlmekel, kelpgflqsgkdkd, and gkdkdavdkllkd), designed on the basis of the structure of S100P, to inhibit the binding of RAGE ligands with sRAGE. Elkvlmekel and kelpgflqsgkdkd, but not gkdkdavdkllkd, reduced S100P binding (Fig. 2D). Elkvlmekel was the most efficacious at blocking S100P and was therefore selected as the lead molecule and is henceforth referred to as RAP (RAGE antagonistic peptide). Gkdkdavdkllkd, which did not inhibit RAGE binding, was used as a control peptide for further studies. The effects of RAP on the binding of RAGE with S100P, S100A4 and HMGB-1 was then assessed (Fig. 2E). RAP inhibited the binding of each these RAGE ligands, suggesting that RAP competes for a site on RAGE that is required for receptor binding by each of these ligands.
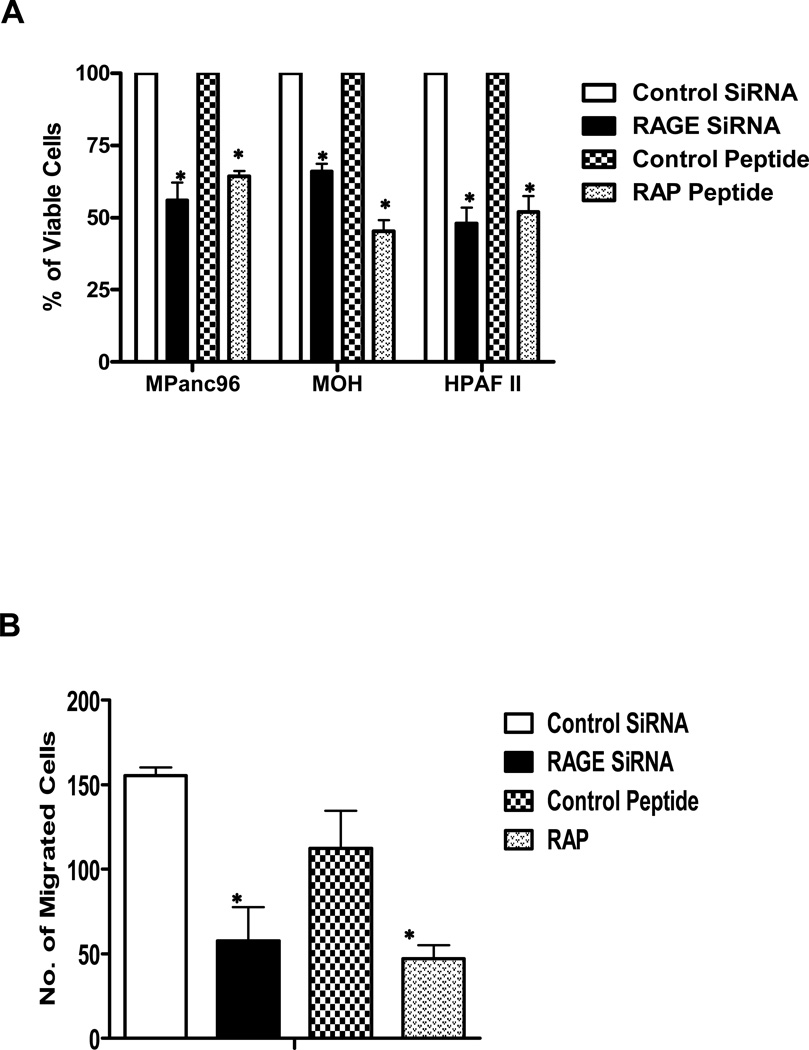
Next we examined the ability of RAP to inhibit RAGE activated cell functions and signaling. We compared the effects of RAP treatments to those of siRNA-mediated RAGE silencing on the growth of in three different cancer cell lines (MPanc96, MOH, and HPAF II) in vitro. Each of these cell lines expresses both RAGE and RAGE ligands (data not shown). RAP treatment and siRNA-mediated silencing of RAGE both reduced the growth of each of the cancer cell lines (Fig. 3A). We also observed an inhibition of migration after RAP treatment (Fig. 3B). Ligand binding with RAGE activates a number of intracellular pathways, including NFκB (14). NFkB signaling is of particular interest in PDAC where it is constitutively high in PDAC cells (9). Therefore, in the current study, we examined the effects of RAP on RAGE mediated NFκB activity. Cells expressing NFκB-luc were treated with S100P, with or without RAP, and NFκB activity was analyzed after 5 h. RAP greatly reduced the ability of S100P to stimulate RAGE-mediated NFκB activation (Fig. 3C).
Fig. 3. RAP blocked RAGE induced cell growth, migration and NFκB activity in vitro.
(A) Treatment of Mpanc96, MOH, or HPAF II PDAC cells with RAGE siRNA or with RAP each significantly reduced cell proliferation to a similar extent. (B) Inhibition of RAGE activity by either siRNA or RAP treatments inhibited the migration of PDAC cells. Mpanc96 cells are shown as representative. (C) RAP treatment blocked the ability of S100P to induce NFκB activity in PDAC cells. BxPC-3 cells stably labeled with an NFκB luciferase reporter are shown as representative. Results shown are means +/− SEM for 3 independent experiments. *=p<0.05.
RAP Inhibits RAGE-Mediated Basal NFκB Activity in PDAC Cells In Vivo
To examine the utility of RAP as a RAGE antagonist in vivo, we utilized cancer cells expressing the NFκB-luc reporter implanted into immune-deficient mice. Intratumoral delivery of both siRNA (Fig 4A) against RAGE or RAP (100 µg) (Fig 4B) to subcutaneously implanted pancreatic cancer cells bearing NFkB-luc caused a dramatic reduction in NFκB activity. To determine the effectiveness of RAP delivered systemically, we next administered RAP (100 µg) intraperitoneally to mice bearing orthotopic PDAC tumors formed with NFκB-luc reporter cancer cells (Fig 4C). We observed that RAP systemic administration caused a substantial reduction (p<0.05) in the NFκB signal 5 h after injection.
Fig. 4. RAP treatment reduced RAGE mediated NFκB activity in vivo.
Constitutive NFκB activity in PDAC xenografts was inhibited by reducing RAGE activity with either (A) liposomal-coupled siRNA against RAGE, or with RAP treatments (100 µg/day) intratumoral (B) or intraperitoneal (C). NFκB activity was monitored by imaging the level of luciferase expressed downstream from an NFκB promoter stably transfected into BxPC-3 cells. *=p<0.05
RAP Treatment Reduces PDAC Tumor Growth and Metastasis In Vivo
RAP showed significant in vivo activity on RAGE signaling. Therefore, we next wished to examine its ability to inhibit in vivo tumor growth. It has previously been shown that inhibition of RAGE using sRAGE reduced C6-glioma tumors. So, initially to confirm the efficacy of RAP, we next analyzed its effects on rat C6-glioma cells bearing luciferase injected subcutaneously into nude mice. Mice with glioma tumors were treated systemically with RAP or a control peptide (each 100 µg/day intraperitoneally for 3 weeks). RAP treatment significantly reduced glioma tumor growth, as assessed by bioluminescence imaging, compared to the control peptide (Fig. 5A).
Fig. 5. RAP treatment reduced tumor growth and metastasis.
(A) Intraperitoneal delivery of RAP (100 µg/day) reduced C6-glioma tumor growth. (B) PDAC Mpanc96 tumor growth and metastasis to the liver (C) were also significantly inhibited by RAP treatments. (D) RAP treated animals did not showed any toxicity as evidenced by un-altered body weight. *=p<0.05
To examine the effects of RAP in a more difficult tumor model, pancreatic cancer Mpanc96 cells bearing luciferease were implanted orthotopically into the pancreas and tumors were established. The effects of RAP treatments on tumor burden and metastasis were analyzed by weekly bioluminescent imaging. Control peptide–treated animals showed extensive tumor growth and metastasis to the liver. In contrast, RAP-treated animals had significantly smaller primary tumors (Fig. 5B) and a lower incidence of metastatic spread (Fig. 5C). RAP treated animals did not showed any toxicity as evidenced by un-altered body weight when compared with control peptide treated animals (5D).
Discussion
In the current study, we provide evidence that a small peptide developed from the structure of S100P can block the binding of several key RAGE ligands that are each involved in inflammation and cancer. This peptide was functional in vivo and provided therapeutic benefit against glioma and pancreatic cancer in preclinical models. This represents the first RAGE competitive antagonist shown to be effective in vivo. The data shown suggest that this peptide may be useful as a treatment for cancer. Based on its ability to block several diverse RAGE ligands, it is also likely that it will be useful in other diseases in which RAGE is involved.
A peptide consisting of residues 150–183 of HMGB-1 (the end of the B-box and its linker to the acidic tail) was previously shown to successfully compete with HMGB-1 binding to RAGE in vitro (8). Pretreatment of cancer cells with this peptide in vitro successfully blocked their subsequent migration and their metastasis in an experimental in vivo model (8). This HMGB-1-derived peptide also blocked the binding and activation of RAGE by S100P (15). The sequence of the HMGB-1 RAGE antagonist is similar to the first 40 amino acids (the first EF-hand helix-loop-helix sequence) of several S100 proteins (8). The peptides examined in the current study were designed on the basis of the structural and pattern similarity of S100P within this same region. The RAP amino acid sequence occurs between amino acids 32–41 of S100P. RAP blocked the binding of not only S100P but also HMGB-1 and S100A4 to RAGE. Other ligands were not evaluated, but it is likely that this peptide will block a wide variety of RAGE ligands as the S100s and HMGB-1 appear to share a common binding domain. These data support the further development of antagonistic peptides to block RAGE activation.
RAGE has previously been shown to transduce the extracellular effects of many different ligands (1–5). RAGE is expressed ubiquitously in many tissues and cell types; in our IHC data we observed RAGE expressed in both cancer cells and in normal tissue. Despite its wide-spread distribution, RAGE-deficient mice developed normally (1). Physiologically, RAGE plays a crucial role in embryonic neuronal outgrowth. However, in the adult, RAGE appears to act in pathological responses as a receptor for a very broad range of ligands that fall into the category of damage-associated molecular pattern molecules (DAMPs). Expression of RAGE ligands is elevated in a variety of inflammatory conditions and in most cancers and the levels of these ligands determine the activity of RAGE (1–5). RAGE has three immunoglobulin-like regions: one “V-type” domain and two “C-type” domains, a short transmembrane domain, and a 43-amino acid cytoplasmic tail (1; 16). The V-type domain has been found to confer ligand binding (1–3, 16). However, the specific basis of RAGE binding has yet to be determined. Comparisons of amino acid sequences in different RAGE ligands do not indicate a high conservation of structure. Narrowing the list of ligands to the numerous members of the S100 family of proteins indicates that these molecules also do not share a high level of sequence homology outside of the Ca2+-binding EF-hand domains. Nevertheless, these molecules, as well as other non-S100 molecules, act as ligands for RAGE. In the current study, experimental peptides elkvlmekel and kelpgflqsgkdkd possess little sequence homology, but both were inhibitory to RAGE binding. Taken together, these observations suggest that RAGE binding is not determined by a specific sequence of amino acids but rather a general pattern. For this reason, RAGE is considered a pattern recognition receptor (17–20).
The use of peptides as therapeutics is often limited by their short half life in vivo and the potential for generation of an immune response. To reduce the degradation of RAP by exoproteases, we blocked the amino and carboxyl termini. The half-life of RAP was not measured in the current study. However, strong inhibition of both NFkB activity and tumor growth were observed when RAP was administered intraperitoneally. This indicates that RAP has a sufficient half-life in vivo to provide therapeutic benefit. Future improvements in the molecule, especially with regard to its stability, are likely to increase this in vivo effectiveness.
Activation of RAGE by S100P stimulates several cellular signaling pathways, including MAP kinase and NFκB (5, 14). These two pathways are constitutively active in many cancer cell lines (21) and influence tumor growth and chemotherapeutic drug resistance (22, 23). This and previous studies indicate that inhibiting S100P-RAGE interactions significantly reduces basal levels of NFκB activity in PDAC and support the existence of an autocrine loop involving RAGE ligands and RAGE in PDAC (9). This characteristic provides the explanation for the ability of RAP to inhbibit basal NFκB activity in cancer cells in vivo.
High mobility group box 1 (HMGB-1) is another well-known ligand for RAGE. HMGB-1 is the prototypic damage-associated molecular pattern (DAMP) molecule and has been implicated in several inflammatory disorders and cancer (1, 4, 24). HMGB-1 is a DNA-binding nuclear protein expressed in the nucleus of most normal cells, but it is secreted after a variety of stresses including cancer, inflammation, necrosis, and chemo- or radio-therapy. Once released, HMGB-1 binds with RAGE and activates signaling (1–5). HMGB-1 release from damaged cells used acts as a “necrotic marker” used by the immune system to recognize tissue damage, initiate reparative responses, and promote maturation of lymphocytes. Extracellular HMGB-1 also acts as a potent pro-inflammatory cytokine, contributing to the pathogenesis of a wide variety of inflammatory disorders (1). HMGB-1 expression and secretion is elevated in melanoma, colon cancer, prostate cancer, pancreatic cancer, and breast cancer (24). HMGB-1 expression in cancer is associated with increased angiogenesis, migration, invasion, and metastasis. Previous in vivo studies showed that blockade of HMGB-1 and RAGE interaction using treatments with sRAGE suppresses tumor growth and metastasis in a murine model of lung cancer (8). HMGB-1 was also found to drive the aggressive growth of glioma tumors (6). In the current study, RAP was able to block HMGB-1 binding to RAGE in vitro and to inhibit glioma growth in vivo. These data support RAP as a useful HMGB-1 inhibitor. Apart from binding with RAGE, HMGB-1 can also act through Toll like receptors (TLR-2 and -4) especially in immune cells including macrophages and act as late mediator of inflammatory responses (25). We did not find higher expression of TLRs in PDAC cells compared to normal pancreas (data not shown). Nevertheless, future studies blocking both RAGE and TLRs may be useful to understand further the roles of HMGB-1 in PDAC.
S100A4 is a member of the S100 family of proteins, which has roles in inflammation and cancer. Originally cloned from highly metastatic murine mammary carcinoma cells, S100A4 has well-established importance in the process of cancer metastasis (26). S100A4 has also been reported to influence pancreatic cancer resistance to therapy (27). In the current study, RAP blocked S100A4 binding to RAGE. The activities promoted by S100A4 that are mediated by RAGE remain uncertain. However, RAP should be a useful tool for the determination of these functions.
In summary, our study identifies RAP as a peptide antagonist that binds with RAGE and blocks its activation by several clinically relevant RAGE ligands. This peptide should be useful for studies of the roles of RAGE in a variety of diseases. This peptide will also be a starting point for the further development of a therapeutic for the many diseases involving RAGE.
Supplementary Material
Acknowledgments
Grant information:
This work was supported in part by the Lockton Endowment and by Public Health Service Grant DK56338 to CD Logsdon, which funds the Texas Medical Center Digestive Diseases Center. This research is supported in part by the National Institutes of Health through MD Anderson's Cancer Center Support Grant CA016672.
References
- 1.Logsdon CD, Fuentes MK, Huang EH, Arumugam T. RAGE and RAGE ligands in cancer. Curr Mol Med. 2007;7(8):777–789. doi: 10.2174/156652407783220697. [DOI] [PubMed] [Google Scholar]
- 2.Ramasamy R, Vannucci SJ, Yan SS, Herold K, Yan SF, Schmidt AM. Advanced glycation end products and RAGE: a common thread in aging, diabetes, neurodegeneration, and inflammation. Glycobiology. 2005;15:16R–28R. doi: 10.1093/glycob/cwi053. [DOI] [PubMed] [Google Scholar]
- 3.Bierhaus A, Humpert PM, Morcos M, Wendt T, Chavakis T, Arnold B, et al. Understanding RAGE, the receptor for advanced glycation end products. J Mol Med. 2005;83:876–886. doi: 10.1007/s00109-005-0688-7. [DOI] [PubMed] [Google Scholar]
- 4.Bierhaus A, Stern DM, Nawroth PP. RAGE in inflammation: a new therapeutic target? Curr Opin Investig Drugs. 2006;7:985–991. [PubMed] [Google Scholar]
- 5.Arumugam T, Logsdon CD. S100P: a novel therapeutic target for cancer. Amino Acids. 2011;41(4):893–899. doi: 10.1007/s00726-010-0496-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taguchi A, Blood DC, del Toro G, Canet A, Lee DC, Qu W, et al. Blockade of RAGE-amphoterin signalling suppresses tumour growth and metastases. Nature. 2000;405:354–360. doi: 10.1038/35012626. [DOI] [PubMed] [Google Scholar]
- 7.Abe R, Shimizu T, Sugawara H, Watanabe H, Nakamura H. Regulation of human melanoma growth and metastasis by AGE-AGE receptor interactions. J Invest Dermatol. 2004;122:461–467. doi: 10.1046/j.0022-202X.2004.22218.x. [DOI] [PubMed] [Google Scholar]
- 8.Huttunen HJ, Fages C, Kuja-Panula J, Ridley AJ, Rauvala H. Receptor for advanced glycation end products-binding COOH-terminal motif of amphoterin inhibits invasive migration and metastasis. Can Res. 2002;62:4805–4811. [PubMed] [Google Scholar]
- 9.Arumugam T, Ramachandran V, Logsdon CD. Effect of cromolyn on S100P interactions with RAGE and pancreatic cancer growth and invasion in mouse models. J Natl Cancer Inst. 2006;98:1806–1818. doi: 10.1093/jnci/djj498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuniyasu H, Oue N, Wakikawa A, Shigeishi H, Matsutani N, Kuraoka K, et al. Expression of receptors for advanced glycation end-products (RAGE) is closely associated with the invasive and metastatic activity of gastric cancer. J Pathol. 2002;196:163–170. doi: 10.1002/path.1031. [DOI] [PubMed] [Google Scholar]
- 11.Wear-Maggitti K, Lee J, Conejero A, Schmidt AM, Grant R, Breitbart A. Use of topical sRAGE in diabetic wounds increases neovascularization and granulation tissue formation. Ann Plast Surg. 2004;52:519–521. doi: 10.1097/01.sap.0000122857.49274.8c. [DOI] [PubMed] [Google Scholar]
- 12.Bucciarelli LG, Wendt T, Qu W, Lu Y, Lalla E, Rong LL, et al. RAGE blockade stabilizes established atherosclerosis in diabetic apolipoprotein E-null mice. Circulation. 2002;106:2827–2835. doi: 10.1161/01.cir.0000039325.03698.36. [DOI] [PubMed] [Google Scholar]
- 13.Deane R, DuYan S, Submamaryan RK, LaRue B, Jovanovic S, Hogg E, et al. RAGE mediates amyloid-beta peptide transport across the blood-brain barrier and accumulation in brain. Nat Med. 2003;9:907–913. doi: 10.1038/nm890. [DOI] [PubMed] [Google Scholar]
- 14.Arumugam T, Simeone DM, Schmidt AM, Logsdon CD. S100P stimulates cell proliferation and survival via receptor for activated glycation end products (RAGE) J Biol Chem. 2004;279:5059–5065. doi: 10.1074/jbc.M310124200. [DOI] [PubMed] [Google Scholar]
- 15.Arumugam T, Simeone DM, Van Golen K, Logsdon CD. S100P promotes pancreatic cancer growth, survival, and invasion. Clin Cancer Res. 2005;11:5356–5364. doi: 10.1158/1078-0432.CCR-05-0092. [DOI] [PubMed] [Google Scholar]
- 16.Heizmann CW, Ackermann GE, Galichet A. Pathologies involving the S100 proteins and RAGE. Subcell Biochem. 2007;45:93–138. doi: 10.1007/978-1-4020-6191-2_5. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt AM, Yan SD, Yan SF, Stern DM. The multiligand receptor RAGE as a progression factor amplifying immune and inflammatory responses. J Clin Invest. 2001;108:949–955. doi: 10.1172/JCI14002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chavakis T, Bierhaus A, Schneider D, Linn T, Nagashima K, Morser J, et al. The pattern recognition receptor (RAGE) is a counter receptor for leukocyte integrins: a novel pathway for inflammatory cell recruitment. J Exp Med. 2003;198:1507–1515. doi: 10.1084/jem.20030800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liliensiek B, Weigand MA, Bierhaus A, Nicklas W, Kasper M, Hofer S, et al. Receptor for advanced glycation end products (RAGE) regulates sepsis, but not the adaptive immune response. J Clin Invest. 2004;113:1641–1650. doi: 10.1172/JCI18704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gordon S. Pattern recognition receptors: doubling up for the innate immune response. Cell. 2002;111:927–930. doi: 10.1016/s0092-8674(02)01201-1. [DOI] [PubMed] [Google Scholar]
- 21.Wang W, Abbruzzese JL, Evans DB, Larry L, Cleary KR, Chiao PJ. The nuclear factor-kappa B RelA transcription factor is constitutively activated in human pancreatic adenocarcinoma cells. Clin Cancer Res. 1999;5:119–127. [PubMed] [Google Scholar]
- 22.Karin M, Cao Y, Greten FR, Li ZW. NF-kappaB in cancer: from innocent bystander to major culprit. Nat Rev Cancer. 2002;4:301–310. doi: 10.1038/nrc780. [DOI] [PubMed] [Google Scholar]
- 23.Arlt A, Vorndamm J, Breitenbroich M, Fölsch UR, Kalthoff H, Schmidt WE, et al. Inhibition of NF-kappaB sensitizes human pancreatic carcinoma cells to apoptosis induced by etoposide (VP16) or doxorubicin. Oncogene. 2001;20(7):859–868. doi: 10.1038/sj.onc.1204168. [DOI] [PubMed] [Google Scholar]
- 24.Sims GP, Rowe DC, Rietdijk ST, Herbst R, Coyle AJ. HMGB-1 and RAGE in inflammation and cancer. Annu Rev Immunol. 2010;28:367–388. doi: 10.1146/annurev.immunol.021908.132603. [DOI] [PubMed] [Google Scholar]
- 25.Park JS, Gamboni-Robertson F, He Q, Svetkauskaite D, Kim JY, Strassheim D, et al. High mobility group box 1 protein interacts with multiple Toll-like receptors. Am J Physiol Cell Physiol. 2006 Mar;290(3):C917–C924. doi: 10.1152/ajpcell.00401.2005. [DOI] [PubMed] [Google Scholar]
- 26.Boye K, Maelandsmo GM. S100A4 and metastasis: a small actor playing many roles. Am J Pathol. 2010;176(2):528–535. doi: 10.2353/ajpath.2010.090526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahon PC, Baril P, Bhakta V, Chelala C, Caulee K, Harada T, et al. S100A4 contributes to the suppression of BNIP3 expression, chemoresistance, and inhibition of apoptosis in pancreatic cancer. Cancer Res. 2007;67(14):6786–6795. doi: 10.1158/0008-5472.CAN-07-0440. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.