Abstract
Purpose: Atrial fibrillation (AF) is one of the most common types of sustained dysrhythmia and there are some disagreements about its treatment. The goals of AF treatment include the control of ventricular rate, the establishment of sinus rhythm and the prevention of thromboembolic events. In this study, the effect of verapamil was compared to digoxin on heart rate control in patients with AF. Methods: This descriptive study was conducted in an emergency department (ED) in Iran. Sixty patients with a new onset AF and rapid ventricular response receiving digoxin or verapamil were included and observed. Results: Two thirty-patient groups receiving verapamil or digoxin were evaluated. The heart rate was significantly decreased in both groups (p = 0.002); however, the cardioversion was not noticed in both of them. The best rate control in verapamil and digoxin groups was observed after 5.9 mg (46.7%) and 0.6 mg (36.7%), respectively. Conclusion: Administration of verapamil in comparison with digoxin has no difference to control the heart rate in AF patients. It should be taken into consideration that prospective randomized studies should be conducted to identify the efficacy and select the best of these two drugs to treat AF patients.
Keywords: Digoxin, Verapamil, Treatment, Atrial fibrillation
Introduction
Atrial fibrillation (AF) is one of the most common types of sustained dysrhythmia; however, there are some disagreements about AF treatment. The prevalence of AF in adult population is 4% and rises with age, from 0.5% in 25 to 35-year old patients to 5% in 69-year old ones.1-4 patients with rapid ventricular response AF frequently require hospitalization. Long-term high ventricular rate can lead to tachycardia-mediated cardiomyopathy.2,5 The goals of AF treatment include the control of ventricular rate, the establishment of sinus rhythm, the prevention of thromboembolic events and the elimination of predisposing factors.5-7 Rates of complications and death among patients treated with rate control and rhythm control protocols demonstrated no difference.6 The optimal level of heart rate in AF is unknown.5-8 Approximately 60-70% of patients with AF have rapid ventricular response and the symptoms and complaints of patients usually depend on the ventricular rate. In emergency department (ED), the first target is usually the control of ventricular rate.6,7,9 The clinical guidelines of the American Heart Association (AHA) and European Society of Cardiology have classified atrial fibrillation into 4 types:7,10 first detected episode, paroxysmal (terminates spontaneously), persistent (electrical or pharmacologic termination is necessary), and permanent AF (resistant to electrical or pharmacologic conversion or accepted by physicians).7,11,12 According to the AHA protocol in heart failure patients with atrial fibrillation, IV beta blockers and nondihydropyridine calcium channel blockers like diltiazem are the drugs of choice for acute rate control in patients with rapid response AF. Digoxin and amidarone could be used for rate control in congestive heart failure patients, but the potential risk of cardioversion to sinus rhythm should be considered with amiodarone.13-15 In this study, digoxin and verapamil were administered by attending physicians and we observed and compared the heart rate control of AF patients who came to the emergency department.
Materials and Methods
This study was approved by ethics committee of Tehran University of Medical Sciences. The study involved 60 patients presented with rapid response AF who came to the emergency department of Imam Khomeini hospital.
A rapid ventricular rate was defined as one with more than 100 ventricular beats per minute (bpm). Patients with systolic blood pressure less than 90 mm Hg, acute symptoms or signs of congestive heart failure or acute coronary syndrome, ventricular rates more than 200 bpm, coexisting unstable medical conditions (e.g. fever, sepsis, acute renal failure, acute hepatic failure, thyrotoxicosis, or ARDS), pre-excitation syndrome and histories of allergy to verapamil or digoxin and those without the consent form and taking any anti-dysrhythmic medications within 1 week before presentation were excluded from the study. Atrial fibrillation within the preceding 72 hours was considered as a new onset AF.
The study was a descriptive one in which the patients were observed in two treatment groups. The selection of treatment protocol was done by attending physicians (cardiologists) according to patients clinical conditions. One group (30 patients) was treated with intravenous (IV) verapamil with doses of 2.5 to 15 mg and the other group (30 patients) received 0.5 to 1 mg IV digoxin.
According to the orders of attending physicians, in the first group, an initial dose of 0.5 mg IV digoxin was given followed by two doses of 0.25 mg IV digoxin at 8 hours intervals. The second and third doses of digoxin were withheld if the ventricular rate was less than 110 bpm at the scheduled dose time. Furthermore, the second group received an initial dose of 2.5 mg verapamil followed by repeated 2.5 mg doses (max. 15 mg) to fulfill heart rate control. All patients were continuously monitored for heart rate and cardiac rhythm in the emergency department for 12 hours. A successful rate control was defined as a ventricular rate of less than 110 bpm persisting for 1 hour or converting to sinus rhythm. The patients were evaluated before, 1, 2, 4 and 12 hours after the treatment.
The loss of rate control after receiving 1 mg of digoxin or 15 mg of verapamil was defined as an episode of increase in ventricular rate more than 110 bpm persisting for more than 30 min or as a rebound to atrial fibrillation in cases where the AF had been converted to sinus rhythm. The parameters examined included the number of patients with successful rate control and episodes of loss of rate control. The serum digoxin levels were not measured routinely, but the study was designed to do it in patients who displayed the symptoms or signs of digoxin toxicity.16
Statistical Analysis
The variables were expressed as frequency for qualitative variables and mean ± SD for quantitative variables and were analyzed by repeated measure ANOVA. The categorical variables were shown in percentages and were analyzed by chi-square test. A p-value of 0.05 was considered significant. All the statistical analyses were performed using SPSS version 17.
Results
Sixty patients with AF and rapid ventricular rates, (30 patients treated with verapamil and 30 patients treated with digoxin) were studied. The different chief complaints for each group are demonstrated in Table 1.
Table 1. Comparison of chief complaints between two groups.
|
Chief complaints |
Group |
Total |
|
| Verapamil | Digoxin | ||
| Dyspnea | 6(10.0) | 8(13.3) | 14(23.3) |
| Abdominal pain and chest pain | 0(.0) | 1(1.7) | 1(1.7) |
| Palpitation | 11(18.3) | 5(8.3) | 16(26.7) |
| Hemiparesis | 2(3.3) | 2(3.3) | 4(6.7) |
| Fatigue | 4(6.7) | 2(3.3) | 6(10.0) |
| Abdominal pain only | 3(5.0) | 2(3.3) | 5(8.3) |
| Symptoms of Deep Vein Thrombosis | 0(.0) | 1(1.7) | 1(1.7) |
| Vertigo | 0(.0) | 2(3.4) | 2(3.4) |
| Chest pain only | 3(5.0) | 7(11.7) | 10(16.7) |
| Hematuria | 1(1.7) | 0(.0) | 1(1.7) |
| Total | 30(50.0) | 30(50.0) | 60(100.0) |
The mean age was 60.83±15.65 years in verapamil group and 66.63±12.47 years in digoxin group which did not have a significant difference (P value: 0.1). The ventricular rates between two groups before drug administration, 1 hour, 2 hours and 4 hours after treatment and successful rate control were not significantly different (Figure 1).
Figure 1.
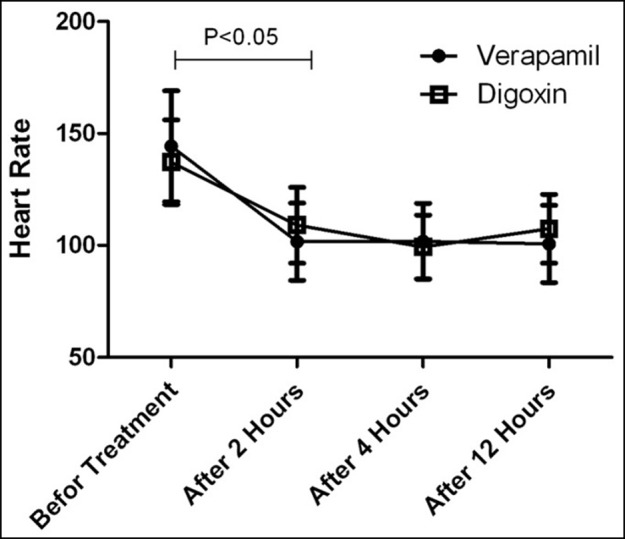
Comparison of successful rate control between two groups throughout study
Mean heart rate in both groups showed that this parameter has been significantly reduced until the 4th hour of evaluation (p = 0.002). No significant difference in heart rate control was noticed between groups and both drugs were almost equally effective (response to therapy was achieved in 20 patients in verapamil group and 23 patients in digoxin group). None of the two drugs converted the patients` rhythm to sinus. The best response in verapamil group was seen after average dose of 5.92 mg (46.7%) and in patients treated with digoxin was observed after average dose of 0.61 mg (36.7%) (Table 2).
Table 2. Comparison of frequency of successful rate control between two groups according to different doses in each group.
| Group | Different doses |
Frequency of successful rate control |
Successful rate control |
Mean dose |
| Verapamil | 2.5mg | 2 | (20)66.6% | 5.92±3.11 |
| 5 mg | 6 | |||
| 7.5 mg | 6 | |||
| 10 mg | 3 | |||
| 15 mg | 3 | |||
| Total | 20 | |||
| Digoxin | 0.25 mg | 4 | (23)76.6% | 0.61±0.26 |
| 0.5 mg | 8 | |||
| 0.75 mg | 8 | |||
| 1 mg | 3 | |||
| Total | 23 |
Discussion
AF treatment goals include the control of ventricular rate, establishing sinus rhythm and preventing thromboembolic events.5-7Approximately 60 - 70% of patients with AF have rapid ventricular response. The control of ventricular rate is usually the first target of treatment in emergency department. King et al17 recommended IV calcium channel blocker or beta blocker drugs for acute control of rapid ventricluar response AF. In our study, the reduction of heart rate after administration of digoxin and verapamil was studied. Intravenous administration of verapamil can easily reduce ventricular rate in AF patients. Verapamil causes prolongation of the conduction time through the atrioventricular (AV) node. The best effect of verapamil on AV nodal conduction time and reducing rate happens during the attack of tachycardia and its effect decreases in normal heart rate.10
Digoxin has been one of the most common medications in control of ventricular rate in AF patients since more than 200 years ago.7 Digoxin is a positive inotropic agent and used especially in patients with systolic heart failure.9
In our study, patients with AF had similar chief complaints in both groups treated with digoxin and verapamil (p = 0.4).
Mean heart rate in both groups of patients also showed that it has been significantly reduced during the 4 hours after the treatment (p = 0.002).
In one study, the effects of intravenous verapamil on acute control of ventricular rate in 24 patients with atrial fibrillation or atrial flutter were evaluated. In 71% of patients (17 cases), after administration of the first bolus dose of verapamil (0.075 mg/kg) within 60 seconds, the ventricular rate decreased to below 100 bpm. All patients who received verapamil (83%) had decreased heart rates below 100.10
Schreck et al compared digoxin with diltiazem in controlling AF and showed that diltiazem achieved a rapid reduction in ventricular rate compared to digoxin, the results becoming statistically significant (p=0.0006) by 5 minutes, which maintained though the study period.18 Heart rate reduction with digoxin did not reach statistical significance until the end of study and there was no benefit in addition of digoxin to verapamil.18Waxman et al showed that verapamil reduced heart rate significantly(p<0.01) compared to placebo group in patients with AF.19 In another study Phillips et al showed that there were no significant differences in mean ventricular response between verapamil and diltiazem.20
Jordanes et al and Falk et al in two studies showed that digoxin can reduce heart rate significantly after 30 minutes and after 2 hours in order in patients with acute AF, but the persistent slowing of heart rate was only seen in 30% of nonconverted patients.21,22
Hemels ME et al showed that verapamil has no beneficial effect in the treatment of patients with AF compared to digoxin and it needs future studies.23The evidence indicates that IV digoxin can control ventricular rhythm within 1 hour of administration. Digoxin controls heart rate at rest but fails to control heart rate at activity or excretion.24 Many studies showed that verapamil decrease heart rate significantly at rest and exertion.25-28
In our study, the best response to treatment with digoxin was seen after 0.6 mg (36.7%) and for patients who were treated with verapamil most desirable response to therapy was observed at 5.9 mg of verapamil (46.7%).
In our evaluation of heart rate control regarding the definition (less than 110 bpm) over the time of the beginning up to 4 h after treatment showed that the rate of improvement in both groups were similar.
Mean heart rate of the patients measured by a 24-h holter monitoring for two weeks after entering the study was 82±12 bpm in digoxin group and 84±13 bpm in the verapamil group. The side effects of digoxin were toxicity, heart block and bradycardia and of verapamil were hypotension, heart block and heart failure.23,29 None of these side effects was seen in our study. Our study also showed that mean heart rate was 99.33 ±14.25 bpm in the digoxin group and 101.83 ±16.94 bpm in the verapamil group (4 hours). However, there was no significant difference between two groups in heart rate control in the 2nd and 4th hour of observation. Heart rate control is achieved after 2 hours in both groups which was significant (Figure 1).
Limitations of study: With respects to the fact that in our study patients’ evaluation is conducted only until twenty four hours after treatment and patient selection was not randomized, other studies with randomization and continuous evaluation until discharging these patients are recommended for the future.
Conclusion
Verapamil has no advantage over digoxin in heart rate control in patients with acute onset AF.
Acknowledgments
We thank all participants and the physicians of Imam Khomeini hospital that helped us in this study.
Conflict of interest
There is no conflict of interest between authors in this study.
References
- 1.Wolf PA, Abbot RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the framingham study. Stroke. 1991;22:983–8. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, Wolf PA. Epidemiology of atrial fibrillation. In: Falk RH, Podrid PJ, editors. Atrial Fibrillation: Mechanisms and management. New York: Raven Press; 1992.
- 3.Boriani G, Biffi M, Branzi A, Magnani B. Pharmacological treatment of atrial fibrillation: a review on prevention of recurrences and control of ventricular response. Arch Gerontol Geriatr. 1998;27:127–39. doi: 10.1016/s0167-4943(98)00106-x. [DOI] [PubMed] [Google Scholar]
- 4.Safaie N, Maghamipour N, Jodati AR, Mahmoodpoor A, Dashtaki L, Hakimzadeh M. New procedure for treatment of atrial fibrilation in patients with valvular heart disease. Acta Med Iran. 2010;48:337–41. [PubMed] [Google Scholar]
- 5.Mackstaller LL, Alpert JS. Atrial fibrillation: a review of mechanism, etiology and therapy. Clin Cardiol. 1997;20:640–50. doi: 10.1002/clc.4960200711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tavel ME, Sopher SM, Camm AJ. Atrial fibrillation: problem in management. Chest. 1996;110:1089–91. doi: 10.1378/chest.110.4.1089. [DOI] [PubMed] [Google Scholar]
- 7.Prystowski EN, Benson DW, Fuster V, Hart RG, Kay N, Myerburg RJ. et al. Management of patients with atrial ibrilation. Circulation. 1996;93:1262–77. doi: 10.1161/01.cir.93.6.1262. [DOI] [PubMed] [Google Scholar]
- 8.Khan IJ, Nair CK, Singh N, Gowda RM, Nair RC. Acute ventricular rate control in atrial fibrillation and atrial flutter. Int J Cardiol. 2004;97:7–13. doi: 10.1016/j.ijcard.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Jordaens L, Trouerbach J, Calle P, Tavernier R, Deycke E, Vertongen P. et al. Conversion of atrial fibrillation to sinus rhythm and rate control by digoxin in comparison to placebo. Eur Heart J. 1997;18:643–8. doi: 10.1093/oxfordjournals.eurheartj.a015310. [DOI] [PubMed] [Google Scholar]
- 10.Roberts SA, Diaz C, Nolan PE, Salerno DM, Stapczynsky JS, Zbrosek AS. et al. Effectiveness and costs of digoxin treatment for atrial fibrillation and flutter. Am J Cardiol. 1993;72:567–73. doi: 10.1016/0002-9149(93)90353-e. [DOI] [PubMed] [Google Scholar]
- 11.Hartel G, Hartikainen M. Comparison of verapamil and practolol in paroxysmal supraventricular tachycardia. Eur J Cardiol. 1976;4:87–90. [PubMed] [Google Scholar]
- 12.Shamroth L, Krikjer DM, Garret C. Immediate effect of intravenous verapamil in cardiac arrhythmias. BR Med J. 1972;1:660–2. doi: 10.1136/bmj.1.5801.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gonzalez R, Scheinman MM. Treatment of supraventricular arrhythmias with intravenous and oral verapamil. Chest. 1981;80:465–70. doi: 10.1378/chest.80.4.465. [DOI] [PubMed] [Google Scholar]
- 14.Fort S, Lewis MJ, Luscombe DK, John DN. Preliminary investigation of the efficacy of sublingual verapamil in the management of acute atrial fibrillation and flutter. Br J Clin Pharmacol. 1994;37:460–3. doi: 10.1111/j.1365-2125.1994.tb05715.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Numar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW. et al. Adult advanced cardiovascular life support: 2010 american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:s729–56. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 16.Wattanasuwan N, Khan IA, Mehta NJ, Arora P, Vasavada BC, Sacchi TJ. Acute ventricular rate control in atrial fibrillation : iv combination of diltiazem and digoxin vs iv diltiazem alone. Chest. 2001;119:502–6. doi: 10.1378/chest.119.2.502. [DOI] [PubMed] [Google Scholar]
- 17.King DE, Dickerson LM, Sack JL. Acute management of atrial fibrilation. Am Fam Physician. 2002;66:249–56. [PubMed] [Google Scholar]
- 18.Schreck DM, Rivera AR, Tricarico VJ. Emergency management of atrial fibrillation and flutter: intravenous diltiazem versus intravenous digoxin. Ann Emerg Med. 1997;29:135–40. doi: 10.1016/s0196-0644(97)70319-6. [DOI] [PubMed] [Google Scholar]
- 19.Waxman HL, Myerburg RJ, Appel R. Verapamil for the control of ventricular rhythm in paroxysmal supraventricular tachycardia and atrial fibrillation or flutter: a double blind randomized cross over study. Ann Intern Med. 1981;9:1–6. doi: 10.7326/0003-4819-94-1-1. [DOI] [PubMed] [Google Scholar]
- 20.Philips BG, Gandhi AJ, Sanoski CA. Comparison of intravenous verapamil and diltiazem for the acute treatment of atrial fibrillation and flutter. Pharmacotherapy. 1997;17:1238–45. [PubMed] [Google Scholar]
- 21.Jordanes J, Trouerbach J, Calle P. Conversion of atrial fibrillation to sinus rhythm and rate control by digoxin in comparison to placebo. Eur Heart J. 1997;18:643–8. doi: 10.1093/oxfordjournals.eurheartj.a015310. [DOI] [PubMed] [Google Scholar]
- 22.Falk RH, Knowlton AA, Bernard SA. Digoxin for converting recent onset atrial fibrillation to sinus rhythm: a randomized double blinded trial. Ann Intern Med. 1987;106:503–6. doi: 10.7326/0003-4819-106-4-503. [DOI] [PubMed] [Google Scholar]
- 23.Hemels ME, Noord TV, Crijns HJ, Van Veldhuisen DJ, Veeger NJ, Bosker HA. et al. Verapamil Versus Digoxin and Acute Versus Routine Serial Cardioversion for the Improvement of Rhythm Control for Persistent Atrial Fibrillation. J Am Coll Cardiol. 2006;48:1001–9. doi: 10.1016/j.jacc.2006.05.043. [DOI] [PubMed] [Google Scholar]
- 24.Tamariz LJ, Bass EB. Pharmacological rate control of atrial fibrillation. Cardiol Clin. 2004;22:35–45. doi: 10.1016/s0733-8651(03)00111-5. [DOI] [PubMed] [Google Scholar]
- 25.Panidis IP, Morganroth J, Baessler C. Effectiveness and safety of oral verapamil to control exercise induced tachycardia in patients with atrial fibrillation receiving digitalis. Am J Cardiol. 1983;52:1197–201. doi: 10.1016/0002-9149(83)90573-8. [DOI] [PubMed] [Google Scholar]
- 26.Lewis RV, Mcmurray J, Mcdevitt DG. Effects of atenolol, verapamil, and xamoterol on heart rate and exercise tolerance in digitalised patients with chronic atrial fibrillation. J Cardiovasc Pharmacol. 1989;13:1–6. doi: 10.1097/00005344-198901000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Lundstrom T, Ryden L. Ventricular rate control and exercise performance in chronic atrial fibrillation: effects of diltiazem and verapamil. J Am Coll Cardiol. 1990;16:86–90. doi: 10.1016/0735-1097(90)90461-w. [DOI] [PubMed] [Google Scholar]
- 28.Lundstrom T, Moor E, Ryden R. Differential effects of xamoterol and verapamil on ventricular rate regulation in patients with chronic atrial fibrillation. AM Heart J. 1992;124:917–23. doi: 10.1016/0002-8703(92)90973-y. [DOI] [PubMed] [Google Scholar]
- 29.Van noord T, Van gelder IC, Tieleman RG, Bosker HA, Tuinenburg AE, Volkers C. et al. Verdict: the verapamil versus digoxin cardioversion trial: a randomized study on the role of calcium lowering for maintenance of sinus rhythm after cardioversion of persistent atrial fibrillation. J Cardiovasc Electrophysiol. 2001;12:766–9. doi: 10.1046/j.1540-8167.2001.00766.x. [DOI] [PubMed] [Google Scholar]


