INTRODUCTION
Cholesterol granulomas (CGs) of the petrous apex (PA) are expansile cystic lesions containing cholesterol crystals surrounded by foreign body giant cells, fibrous tissue reaction and chronic inflammation. The literature describes two mechanisms of origin for CGs of the petrous apex. The older theory asserts that temporal bone mucosal swelling combined with resorption of gas that is present results in negative pressure and hemorrhage into the temporal bone air cells (1).The subsequent degradation of hemosiderin and cholesterol results in an inflammatory granulomatous reaction. An alternative theory, described by Jackler and colleagues, asserts that exuberant pneumatization of the temporal bone exposes marrow-filled spaces of the PA (1). The resulting coaptation of the marrow and mucosa results in proclivity towards hemorrhage. Hemorrhage is triggered and clot develops, resulting in obstruction of the PA outflow tract. Resulting degradation of hemosiderin and cholesterol results in an inflammatory granulomatous reaction. Recently, this latter theory has gained greater acceptance.
The clinical presentation of PA cholesterol granuloma can vary depending on the extension (2). A previous review at our institution of 34 patients with petrous apex cholesterol granuloma management revealed that the most common presenting symptom was hearing loss (64.7%) followed by vestibular symptoms (56%), tinnitus (50%), headache (32.3%), facial twitching (23.5%), facial paresthesia (20.6%), otorrhea (11.8%), diplopia (5.9%), and facial weakness (2.9%) (3). Sanna and colleagues have noted that hearing loss and vertigo are present in approximately 50%, followed by tinnitus (36.6%), headache (32.5%), trigeminal neuralgia (25%), diplopia (16.6%), and facial weakness (17.5%) (4). Accurate radiologic diagnosis of petrous apex (PA) cholesterol granuloma is essential to subsequent treatment.
Generally, patients with symptoms are managed surgically while non-surgical management is advocated for asymptomatic patients. Surgical management of cholesterol granuloma is performed primarily by drainage procedures via the translabyrinthine, infralabyrinthine, middle fossa, transphenoidal, or more commonly, the infracochlear approach. The main goal of these drainage procedures is to establish an outflow drainage pathway that is maintained so that CG expansion does not result in recurrence of patient symptoms. While outcomes such as lesion size, resolution of patient symptoms, occurrence of complications, and presence of aeration have been reported previously (2,3,4), maintenance of drainage pathway has not been widely reported. Given that the most common cause of recurrence is obstruction of the drainage site by fibrous tissue (3), this is a critical outcome that is ultimately a more direct measure for success.
The aims of the current study include: 1) To assess the maintenance of drainage pathway patency in patients who undergo surgical management of PA cholesterol granulomas; 2) To review the histopathologic and radiologic changes associated with surgical drainage of petrous apex (PA) cholesterol granulomas; and 3) To provide histopathologic evidence regarding the exposed marrow theory of petrous apex cholesterol granulomas.
MATERIALS AND METHODS
The institutional review board (IRB) of St. Vincent Medical Center approved this study (IRB # 11-014).
Patients
All patients with PA cholesterol granuloma seen from August 1983 to December 2010 who had surgical treatment and for whom charts were accessible were reviewed. Patients without follow-up care at our institution were excluded from the study. 17 patients were identified for whom charts were available (11 males, 6 females). The mean age at surgery was 38 years (range 14 to 62 years). The distribution of surgical procedures was 14 transcanal infracochlear drainage procedures, 2 infralabyrinthine drainage procedures, and 1 middle fossa craniotomy drainage procedure. The mean length of follow-up care for these patients, as measured from surgery to last imaging date, was 90.7 months (SD= 97 mos), ranging from 5 to 297 mos.
Procedures
Clinical Review
The presenting clinical features, audiometric data, and imaging findings were recorded on a Case Report Form developed for this study. Preoperative and postoperative pure-tone averages were calculated using thresholds obtained at 500 Hz, 1000 Hz, 2000 Hz, and 3000 Hz for bone conduction. The primary outcome was demonstrated maintenance of a PA outflow drainage pathway following the surgical drainage procedure. This was assessed by radiologic imaging or histopathology, when available. In the absence of these indicators, recurrence of symptoms was used as a proxy for failure of drainage pathway maintenance. The surgical approach used and the associated operative complications were noted. When available, postoperative imaging studies were assessed for the maintenance of drainage pathway patency. Aeration of the petrous apex cholesterol granuloma cyst, presence of new bone growth along the outflow drainage pathway, recurrence of presenting symptoms, placement of a stent in the drainage pathway, and need for revision surgery were also recorded.
Temporal Bone Histopathology
Temporal bone specimens of patients with cholesterol granuloma from the House Research Institute temporal bone collection were analyzed in an effort to identify evidence regarding the exposed marrow theory of petrous apex cholesterol granuloma formation. Temporal bones were fixed, decalcified, embedded in celloidin, and sectioned at 20µm. Every 10th section was stained with hematoxylin and eosin and mounted on a glass slide; the other 9 sections were stored for special evaluations. 10 temporal bone specimens from patients with incidentally discovered, non-intervened petrous apex cholesterol granulomas were analyzed for evidence regarding the exposed marrow theory of PA cholesterol granuloma formation. One temporal bone specimen was obtained from a patient who underwent surgical drainage of a petrous apex cholesterol granuloma. Sectioning of this temporal bone was performed in the plane of the drainage stent (angiocatheter) to allow for an analysis of histopathologic changes associated with surgical drainage and stent placement.
Statistical Analysis
Both descriptive and inferential statistics were performed. The primary outcome, ‘maintenance of drainage’, was compared between those with and without stent placement, using chi-square (or Fisher’s Exact test for small n’s). Other factors influencing outcome were evaluated using chi-square for categorical variables and t-test or the nonparametric Mann-Whitney U test, as appropriate, for interval level (continuous) data. Criterion for statistical significance was set at p≤0.05, two-tailed.
RESULTS
Clinical Review
The presenting symptoms for the group as a whole are presented in Table 1 and most commonly included hearing loss (52.9%) and dizziness (47.1%). Thirteen (76.4%) patients had more than one symptom at time of presentation. Patients who reported tinnitus as a presenting symptom tended to be more likely to undergo revision surgery (5 of 7 patients; 71%) than those who did not report tinnitus (2 of 10 patients; 20%) (Fisher exact test, p = .058). Patients who reported facial paresthesias as a presenting symptom were more likely to undergo revision surgery than those patients who did not experience facial paresthesias (Fisher exact test, p = .015). Specifically, all 4 patients (100%) who experienced facial paresthesias underwent revision surgery, while only 3 (23%) who did not experience facial paresthesias underwent revision. No other presenting symptoms resulted in a greater likelihood of revision surgery. While patients who underwent revision tended to have a greater number of presenting symptoms compared to those who did not undergo revision (medians=3 and 2 presenting symptoms, respectively), this difference did not achieve statistical significance.
Table 1.
| Symptom | No. | % |
|---|---|---|
| Hearing loss | 9 | 52.9 |
| Vertigo/dysequilibrium | 8 | 47.1 |
| Tinnitus | 7 | 41.2 |
| Headache | 6 | 35.3 |
| Facial weakness | 1 | 5.9 |
| Facial twitching | 0 | 0 |
| Facial paresthesia | 4 | 23.5 |
| Otorrhea | 2 | 11.8 |
| Diplopia | 1 | 5.9 |
Of those patients with both pre- and posttreatment audiograms (n = 12), the change between pretreatment and last available audiogram was not statistically significant, with a mean pre-surgery pure tone average (PTA) of 34 dB and a mean PTA at last audiologic follow-up of 48 dB (p = .076). Patients with longer followup (4, 8, 24, and 24 years, respectively) were noted to have larger declines in their hearing and this may simply be representative of progression of age-related hearing loss, rather than attributable to the cholesterol granuloma.
Surgical characteristics are summarized in Table 2. The majority of patients (n = 13 patients) underwent infracochlear (IC) drainage procedures, with the remainder undergoing drainage procedures by infralabyrinthine (IL) approach (n = 3 patients) and middle fossa craniotomy (MFC) approach (n = 1 patient). Stents were placed in 11 of 17 patients, with stent placement in 8 of 13 IC patients and 3 of 3 IL patients. Mean cholesterol granuloma cyst maximal diameter was approximately 29.9 millimeters, ranging from 20 to 50 millimeters (SD 8.8 mm). There was no statistically significant difference in cholesterol granuloma maximal diameter between patients who underwent stent placement and those who did not. While reaccumulation of cholesterol granuloma within the cyst cavity occurred in some patients over time, the mean maximal diameter of the cyst remained relatively stable (mean 28.6 mm, range 16 to 50 mm, SD 9.4 mm).
Table 2.
| Characteristic | |
|---|---|
| Age at surgery, mean (min-max), yr | 38 (14–62) |
| Side (right:left) | 8:9 |
| Sex (male:female) | 11:6 |
| Surgical approach | Patients (n = 17) |
| Infracochlear | 13 |
| Fnfralabyrinthine | 3 |
| Middle cranial fossa | 1 |
| Stent placement | Patients (n = 17) |
| No stent | 6 |
| Stent | 11 |
| Size at surgery, mean (min-max), mm | 29.9 (18–50) |
| No stent | 30.5 (25–40) |
| Stent | 29.9 (18–50) |
| Last follow-up sizea, mean (min-max), mm | 28.6 (16–50) |
| No stent | 28.3 (18–35) |
| Stent | 28.8 (16–50) |
Size change from surgery to latest follow-up was not statistically significant.
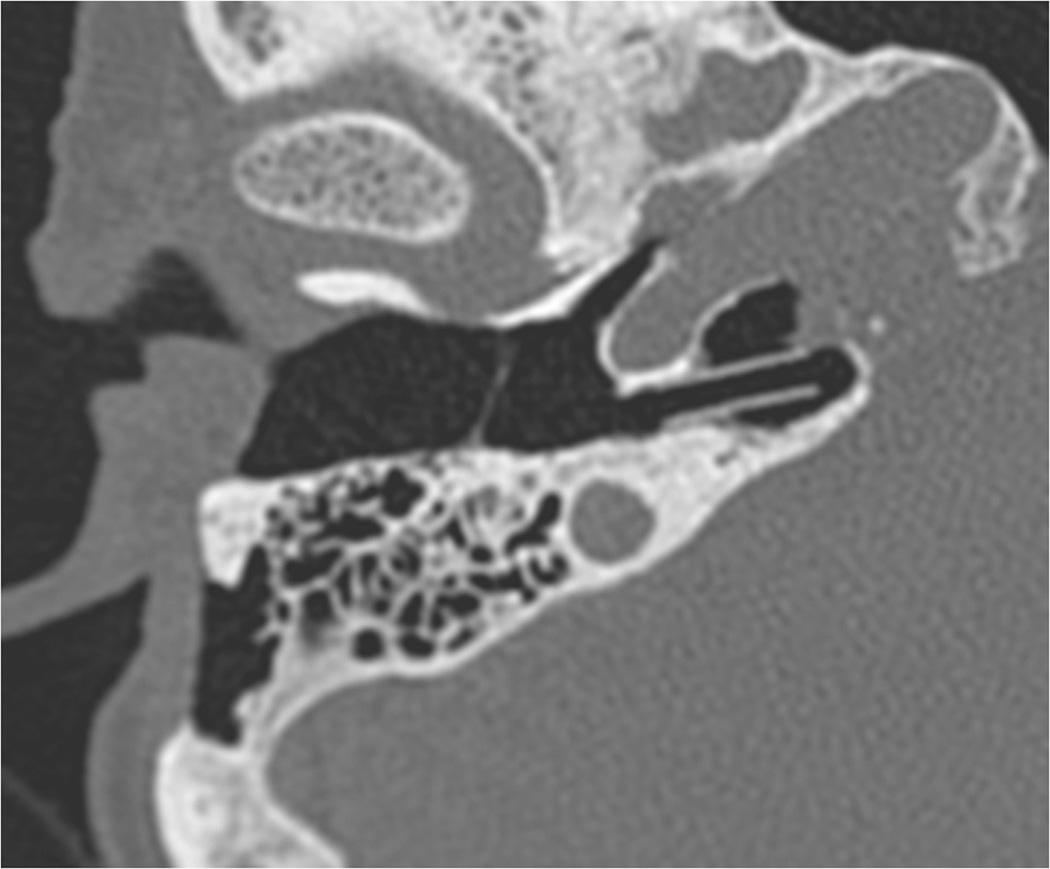
Table 3 presents radiologic findings regarding maintenance of the drainage pathway. In two cases, radiological follow-up information was not available. Of the 15 patients for whom radiology was reviewed, 11 patients(73.3%) exhibited drainage pathway maintenance (Fig. 1). Only one of the patients (20%) who did not have a stent placed at the time of surgery, maintained drainage pathway patency. In contrast, all 10 of those in whom a stent was placed maintained patency (Fisher’s Exact p = .004). Cyst aeration was exhibited by only 4 patients (24%) and, given the small percentage of patients who exhibited this radiologic characteristic, little conclusion can be drawn regarding the effect of stent placement. In the absence of cyst aeration, drainage pathway maintenance was judged on the basis of either aeration within the stent or the combination of stent visualization, low signal intensity of the cyst on T1-weighted MRI, and lack of expansion of the cyst on subsequent radiologic imaging. Evidence of new bone formation around the stent or drainage pathway was found in 6 (35%) patients.
Table 3.
| Patients | Drainage pathway maintained |
|
|---|---|---|
| N | % | |
| All (n = 15)a | 11 | 73.3 |
| No stent (n = 5) | 1 | 20.0 |
| Stent (n = 10) | 10 | 100.0 |
Stent versus no stent, Fisher's exact p = 0.004.
Radiologic follow-up information not available in 2 cases.
Fig. 1.
Axial CT image demonstrating maintenance of the petrous apex (PA) outflow tract with stent in place.
Table 4 provides individual patient data, including surgical approach, stent placement, and need for revision surgery. Recurrence of presenting symptoms and number of surgical revisions are also noted. Recurrence of presenting symptoms occurred in 7 patients (41%). Five patients (83%) without stent placement but only 2 patients (18%) with stent placement exhibited presenting symptom recurrence, and all patients with recurrence required revision surgery. The difference in the rate of revision surgery between those with and without a stent was significant (p = .035).
Table 4.
| Patient | Approach | Stent placed |
Recurrence of presenting symptoms |
Need for revision surgery |
No. of surgical revisions |
|---|---|---|---|---|---|
| 1 | MFC | No | No | No | 0 |
| 2 | IC | No | Yes | Yes | 2 |
| 3 | IC | No | Yes | Yes | 1 |
| 4 | IC | No | Yes | Yes | 1 |
| 5 | IC | No | Yes | Yes | 1 |
| 6 | IC | No | Yes | Yes | 1 |
| 7 | IL | Yes | No | No | 0 |
| 8 | IL | Yes | Yes | Yes | 2 |
| 9 | IL | Yes | No | No | 0 |
| 10 | IC | Yes | Yes | Yes | 3 |
| 11 | IC | Yes | No | No | 0 |
| 12 | IC | Yes | No | No | 0 |
| 13 | IC | Yes | No | No | 0 |
| 14 | IC | Yes | No | No | 0 |
| 15 | IC | Yes | No | No | 0 |
| 16 | IC | Yes | No | No | 0 |
| 17 | IC | Yes | No | No | 0 |
TC indicates infracochlear approach; IL, infralabyrinthine approach; MFC, middle fossa approach.
Of patients without stent placement at initial surgery, patient #2 underwent subsequent revision surgeries without stent placement, while the other patients had a stent placed at time of revision. Of those who had stent placement at initial surgery, patients #8 and #10 also had stent placement at their subsequent surgeries but developed fibrous tissue obstruction of the stent resulting in recurrence of presenting symptoms, necessitating additional surgical revision. Evidence of new bone formation around the stent or drainage pathway was seen more commonly in patients who underwent stent placement. However, this feature could not be assessed in the majority of patients who did not undergo stent placement.
Histopathology of a Surgically Managed PA Cholesterol Granuloma
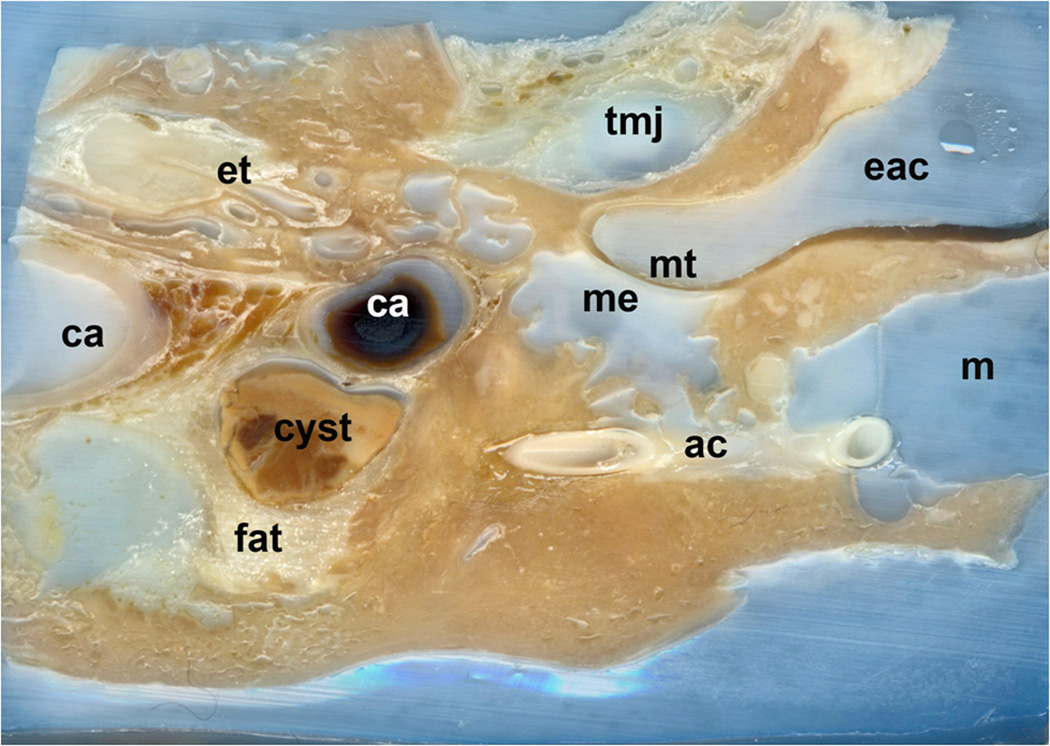
The temporal bone specimen of a patient with surgically managed PA cholesterol granuloma was obtained, and sectioning was performed in the plane of the drainage catheter. This specimen provided an opportunity for examination of the histopathologic changes associated with surgical drainage of PA cholesterol granulomas. Figure 2 shows the partially sectioned temporal bone, demonstrating the cholesterol granuloma drained into the mastoid by an angiocatheter.
Fig. 2.
Partially sectioned embedded temporal bone from patient with a cholesterol granuloma (cyst and fat) drained into the mastoid by an angiocath (ac). Temporal mandibular joint (tmj), Eustachian tube (et), external auditory canal (eac), tympanic membrane (mt), middle ear (me) carotid artery, one segment containing clotted blood (ca). (Hematoxylin and Eosin [H&E] X 5)
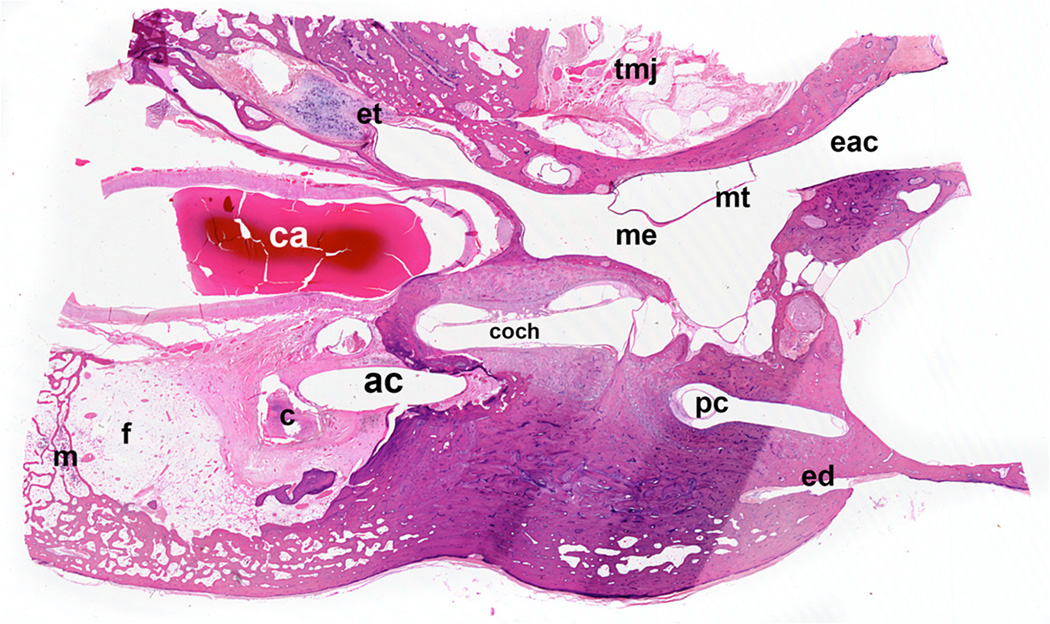
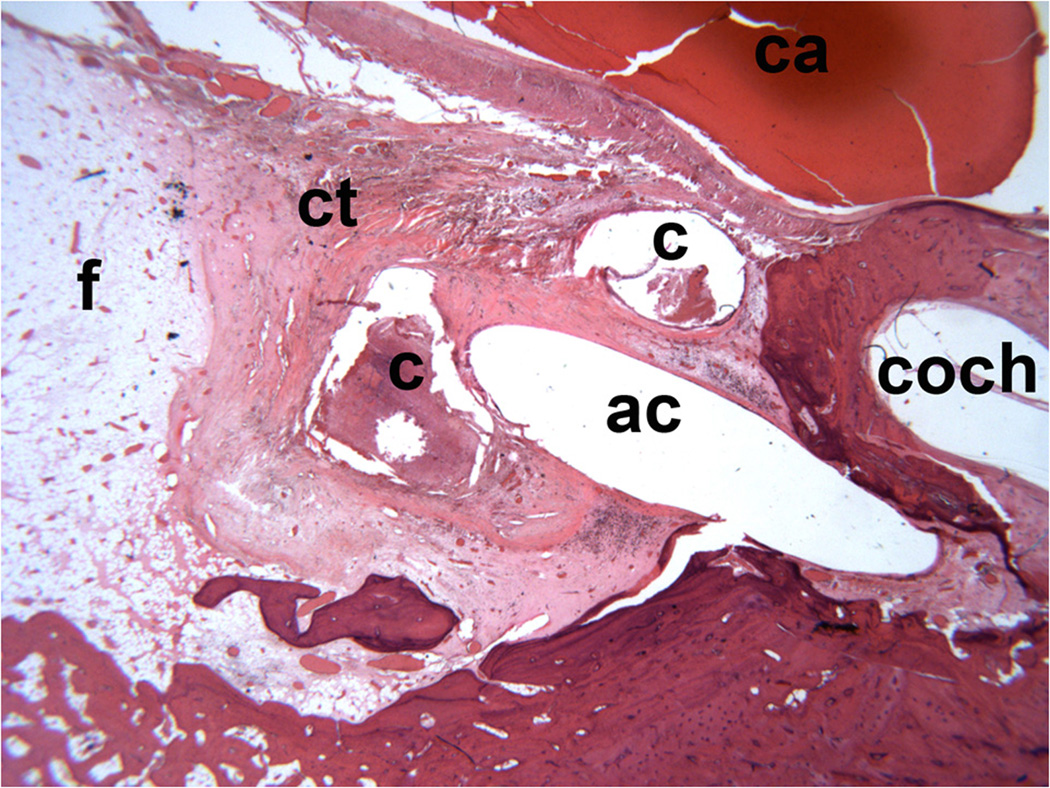
An adjacent hematoxylin and eosin stained section demonstrates fatty replacement of the cholesterol granuloma cyst with hematopoietic bone marrow adjacent to the cholesterol granuloma cyst (Figure 3). This figure demonstrates the angiocatheter entering the PA cholesterol granuloma cyst. Figure 4 shows a magnified view of the angiocatheter draining the PA cholesterol granuloma cyst. Connective tissue is noted to surround the PA cholesterol granuloma cyst with fatty replacement of the cyst. On closer examination, new bone formation is noted around the site of the angiocatheter (Figure 5).
Fig. 3.
Section made close to the level of Fig. 1. remnants of cyst (c), angiocath path (ac), fat replacing cyst (f), hematopoietic bone marrow (m), temporal mandibular joint (tmj), eustachian tube (et), external auditory canal (eac), tympanic membrane, displaced (mt), middle ear (me) cochlea (coch), posterior semicircular canal (pc), endolymphatic duct (ed). (Hematoxylin and Eosin [H&E] X 5).
Fig. 4.
Cyst (c) and angiocath (ac). Carotic artery (ca), connective tissue surrounding cyst (ct), Newly formed fat (f), cochlear (coch). (H&E X 10)
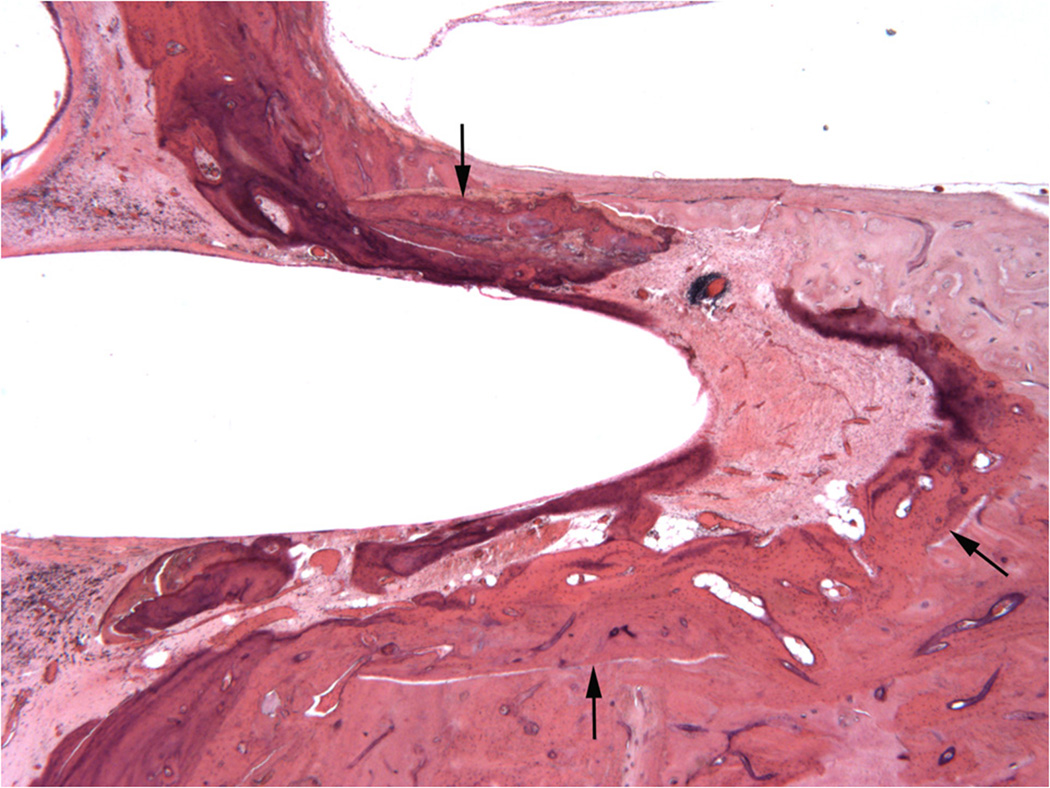
Fig. 5.
New bone (arrows) surrounding angiocath. (H&E X 20)
Histopathologic Evidence Regarding the Exposed Marrow Theory of PA Cholesterol Granuloma Formation
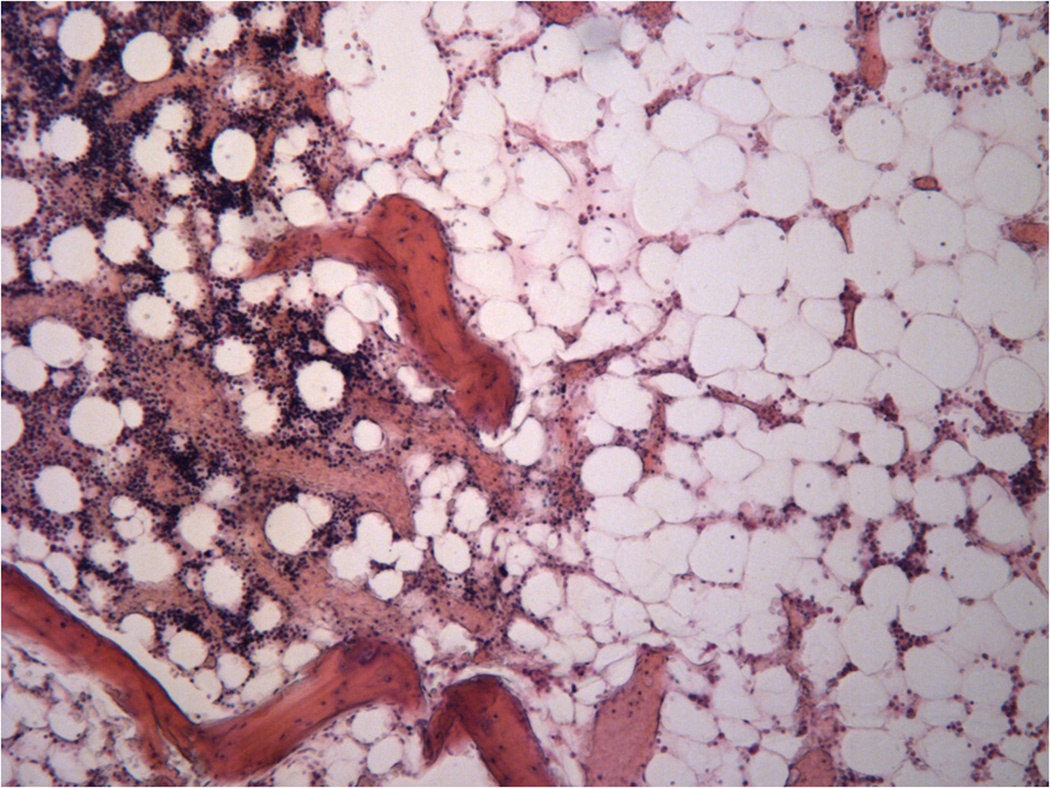
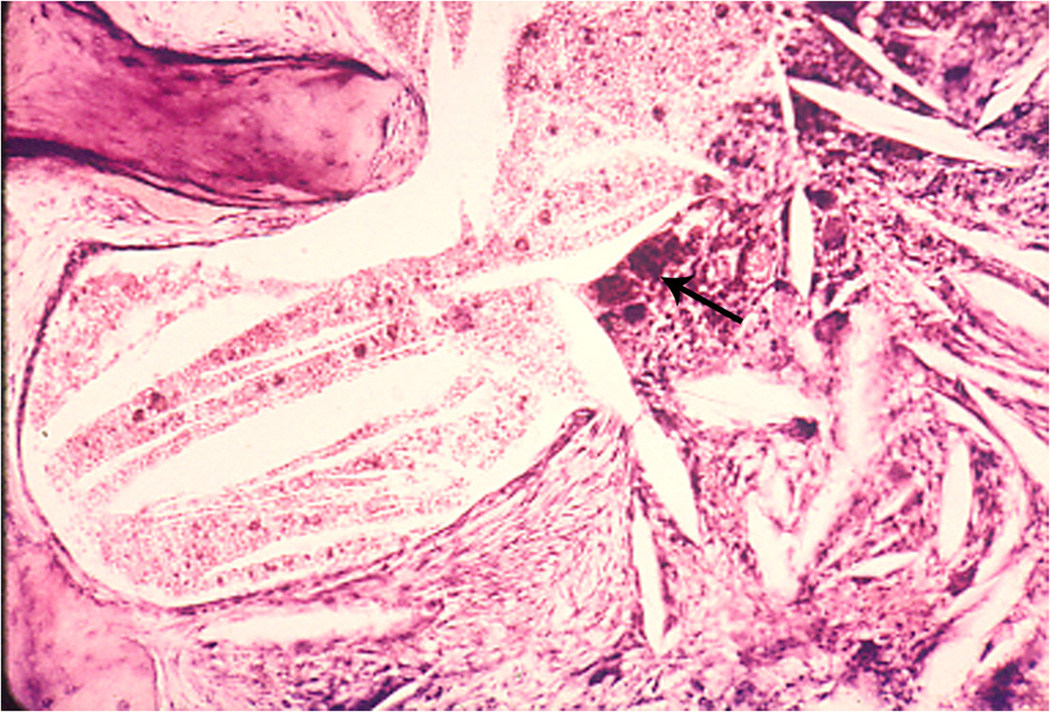
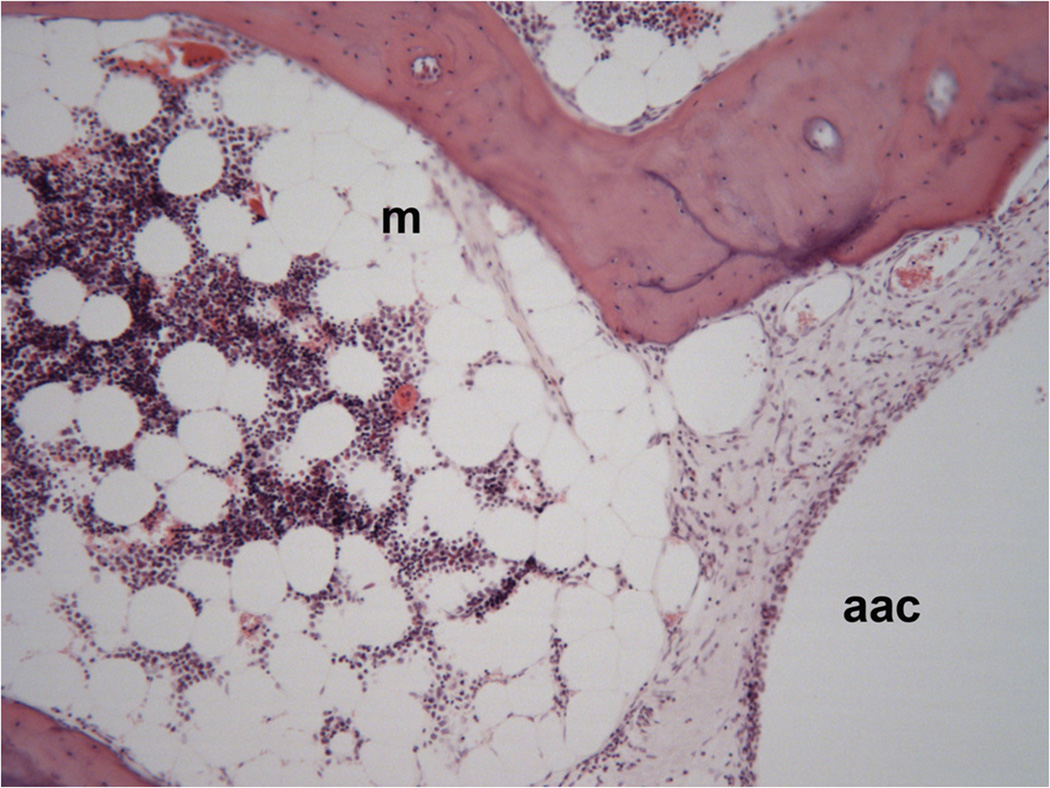
According to both theories of petrous apex cholesterol granuloma formation, degradation of hemosiderin and cholesterol results in an inflammatory granulomatous reaction. Thus, the formation of a cholesterol granuloma requires a source of blood and cholesterol. Petrous apex marrow satisfies both of these requirements as a ready source for hemosiderin, cholesterol, and lipids. Our analysis of temporal bone sections from 10 patients with cholesterol granulomas yielded evidence supportive of the exposed marrow theory. Figure 6 demonstrates the presence of hematopoietic marrow adjacent to fat in a remnant of the cholesterol granuloma cyst. Figure 7 demonstrates that cholesterol granuloma formation does occur in former air cells and contains both degradation products of hemosiderin and cholesterol. Foreign body giant cells are also noted in the surrounding proliferating granulation tissue. Evidence supporting the coaptation of marrow and mucosa is demonstrated in Figure 8. Specifically, this figure demonstrates hematopoietic marrow adjacent to an apical air cell, abutting the air cell mucosa. Embryologic evidence exists for this coaptation of marrow and mucosa as seen in Figure 9, which demonstrates a marrow mucosal connection in an infant.
Fig. 6.
Hematopoietic marrow adjacent of fat in remnant of cyst. (H&E X 100)
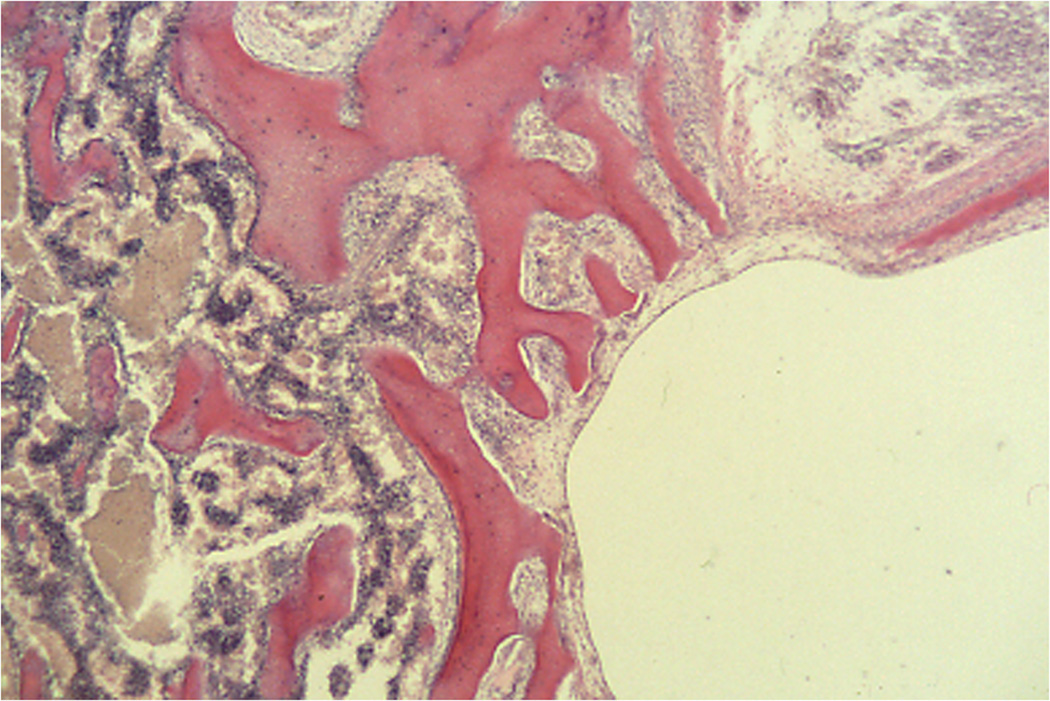
Fig. 7.
Cholesterol granuloma in former air cell. Clefts left from dissolved cholesterol crystals are present in the remaining fluid as well as the surrounding proliferating granulation tissue containing foreign body giant cells (arrow). (H&E X 100)
Fig. 8.
Hematopoietic marrow (m) adjacent of an apical air cell (aac) in an unrelated case (H&E X 100)
Fig. 9.
Marrow mucosa connections in infant. (H&E X 100)
DISCUSSION
Based on radiological evaluation, the majority of patients in this study maintained a drainage pathway after surgical management of petrous apex cholesterol granuloma. Recurrence of symptoms and need for revision surgery were more common in those patients in whom a stent was not placed.
Given the success of surgical management, accurate radiological diagnosis of this entity is essential. While radiologic diagnosis has been discussed extensively in the literature, some ‘pearls’ about radiologic diagnosis are worth repeating prior to proceeding with the discussion (5,6). Specifically, a petrous apex cholesterol granuloma must be distinguished from petrous apex simple effusion, fatty marrow, or mucocele. While imaging characteristics of PA effusions and cholesterol granulomas on MRI are similar (iso- to hypointense on T1-weighted imaging, hyperintense on T2-weighted imaging, and non-enhancement with gadolinium), effusions typically demonstrate intact septations in the petrous apex on CT and are non-expansile. Fatty marrow may show similar characteristics on MRI, but CT will show a non-destructive, non-expansile lesion. Furthermore, the use of fat-saturation imaging on MRI will distinguish fatty marrow from a cholesterol granuloma, as fatty marrow on fat-saturation imaging will be hypointense on T1- and T2-weighted imaging. Mucoceles typically demonstrate bony expansion on CT and on MRI, are hypointense on T1-weighted imaging, hyperintense on T2-weighted imaging, and demonstrate enhancement with gadolinium.
Clinical Review of Surgically Managed PA Cholesterol Granulomas
The primary goal of surgical drainage of PA cholesterol granulomas is to provide and maintain an outflow pathway to allow for continued drainage of the cholesterol granuloma. Radiologic characteristics of cholesterol granuloma that have been used as proxies or indicators for successful long-term drainage have included stable size in terms of maximal diameter, the presence of cyst aeration, and placement of a draining stent (3). In general, cyst size remained relatively stable in the majority of patients. However, patients did experience recurrence of presenting symptoms with reaccumulation within their cysts without enlargement. Thus, stability in terms of size may not be the most ideal proxy by which to define success of surgical management of PA cholesterol granulomas. Cyst aeration was present in a small percentage of our patients and, while its presence does suggest successful drainage, the absence of cyst aeration does not necessarily indicate inadequate drainage. This is in agreement with a previous study that showed that PA cholesterol granuloma cyst aeration had no correlation to symptom resolution or cyst enlargement (7). Radiologic evidence of new bone formation around the drainage pathway did not surface as a reliable indicator of unsuccessful surgical drainage in our study patients as this feature was identified more commonly in patients who had stents placed at the time of surgery yet were less likely to undergo revision surgery.
Review of the study patients revealed that placement of a stent was more likely to result in the maintenance of drainage pathway patency. However, stent placement did not necessarily guarantee that the drainage pathway would remain patent as noted in two patients (#s 8 and 10). The revision surgery rate was 41% overall (7 of 17 patients). However, 18% of patients with stents placed at the time of surgery underwent revision versus 83% of patients who did not have a stent placed. The rate of revision surgery with stent placement is more consistent with the rates published in the literature (2,3,4,8). The universal surgical finding at revision surgery was the presence of fibrous tissue obstruction of the drainage pathway. We believe that assessment of drainage pathway patency is a more direct measure of surgical success in the long-term management of petrous apex cholesterol granulomas. Our institutional bias is towards either an infracochlear or infralabyrinthine approach to drainage of these lesions.
Histopathology of Surgically Managed PA Cholesterol Granulomas
The analysis of a temporal bone specimen from a patient with surgically managed PA cholesterol granuloma suggests that long-term preservation of drainage pathway patency is possible with the placement of a stent, in this case for approximately 24 years after surgical drainage. However, the presence of new bone formation suggests that these drainage pathways may obstruct over time due to a combination of bony regrowth as well as fibrous tissue obstruction and cholesterol granuloma reaccumulation. The placement of a stent at the time of surgical drainage procedure may help prevent eventual obstruction of this drainage pathway.
Recurrence of presenting symptoms and subsequent revision surgery, while suggesting drainage pathway obstruction, do not necessarily indicate new bone formation around the drainage pathway. But, the question does arise whether the presence of the stent as a foreign body may stimulate bony growth. Clinically, determination of whether stent placement causes or prevents bony formation in the drainage pathway is difficult to assess as radiologic evidence of new bone formation around the drainage pathway could not be determined in 4 of the 6 patients without stent placement. In the current study, this made it appear that bony growth was more common in those with stents. While new bone formation may be evident in other parts of the cyst, the relatively small caliber of the drainage pathway makes determination of radiologic evidence of new bone formation along the drainage pathway relatively difficult. However, on histopathology, the presence of bony growth in areas not adjacent to the stent, in fact in the areas adjacent to the cavity of the cyst, argues that bony growth occurs for some reason other than proximity to the stent. It has been suggested that ischemia may lead to new bone formation (9,10). We hypothesize that drainage prevents the continual pressure on the cavity exerted by the cholesterol granuloma. As a result, the fibrosis within the cyst cavity may promote an ischemic environment leading to new bone formation.
The presence of hematopoietic bone marrow adjacent to the cyst suggests that the exposed marrow theory of PA cholesterol granuloma may have some relevancy. The examination of this temporal bone specimen indicates that surgical drainage with stent placement in the drainage pathway can be quite successful and enduring.
Histopathologic Evidence for the Exposed Marrow Theory of PA Cholesterol Granuloma Formation
The exposed marrow theory as put forth by Jackler and Cho suggests that exuberant pneumatization of the temporal bone exposes marrow-filled spaces of the petrous apex to the mucosa-lined air-filled spaces of the petrous apex (1). The histopathologic images presented demonstrate that these marrow-filled spaces exist adjacent to known cholesterol granuloma cysts (Figure 6) and that they can exist adjacent to mucosa-lined air-filled spaces of the petrous apex (Figure 8).
The theory subsequently suggests that this coaptation of the marrow and mucosa results in a proclivity towards hemorrhage and that ensuing hemorrhage results in PA outflow tract obstruction. Marrow in the petrous apex serves as a source for both hemosiderin and lipids. Cholesterol crystals that result from both breakdown of these lipids within the marrow instigate an inflammatory reaction that is believed to be necessary for formation of these cysts (1,11). Some have suggested that the variability in aggressiveness of the cholesterol granuloma is related to the richness of the adjacent blood supply (12). The end result of this process is demonstrated in Figure 7, where clefts left from dissolved cholesterol crystals are present in the remaining fluid as well as surrounding granulomatous reaction with foreign body giant cells present. Conceivably, if this process is widespread enough in the petrous apex, as we know occurs clinically, obstruction of the PA outflow tract would occur. Finally, there is an embryologic basis for these marrow-mucosa coaptations with marrow-mucosal connections known to exist in infant temporal bones as seen in Figure 9. While previously suggested by radiologic evidence, we have not previously seen reports providing histopathologic evidence supporting the exposed marrow theory of PA cholesterol granuloma formation.
CONCLUSIONS
The majority of patients who undergo surgical drainage of PA cholesterol granulomas remain symptom-free after surgical drainage. Loss of patency of the PA drainage pathway may be an important predictor for symptomatic recurrence of petrous apex cholesterol granulomas. Placement of a stent to maintain the drainage pathway may decrease the likelihood of symptomatic recurrence. Histopathology of surgically managed petrous apex cholesterol granulomas demonstrates new bone formation around the drainage pathway, which along with drainage pathway obstruction by fibrous tissue and granulomatous reaction, may contribute to failure of the long-term durability of surgical drainage. Finally, to our knowledge, this is the first presentation of histopathologic evidence supporting the exposed marrow theory of PA cholesterol granuloma formation.
ACKNOWLEDGMENTS
We thank Karen I. Berliner, PhD for assistance with statistical analyses and manuscript editing, and Ayub Samidon for assistance with the computerized patient database.
REFERENCES
- 1.Jackler RK, Cho M. A new theory to explain the genesis of petrous apex cholesterol granulomas. Otol Neurotol. 2003;24:96–106. doi: 10.1097/00129492-200301000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Mosnier I, Cyna-Gorse F, Grayeli AB, Fraysse B, Martin C, Robier A, Gardini B, Chelikh L, Sterkers O. Management of cholesterol granulomas of the petrous apex based on clinical and radiologic evaluation. Otol Neurotol. 2002;23:522–528. doi: 10.1097/00129492-200207000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Brackmann DE, Toh EH. Surgical management of petrous apex cholesterol granulomas. Otol Neurotol. 2002;23:529–533. doi: 10.1097/00129492-200207000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Sanna M, Dispenza F, Mathur N, De Stefano A, De Donato G. Otoneurological management of petrous apex cholesterol granulomas. Am J Otolaryngol. 2009;30:407–414. doi: 10.1016/j.amjoto.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Isaacson B, Kutz JW, Roland PS. Lesions of the Petrous Apex: Diagnosis and Management. Otolaryngol Clin N Am. 2007;40:479–519. doi: 10.1016/j.otc.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Connor SEJ, Leung R, Natas S. Imaging of the petrous apex: a pictorial review. Br J Radiol. 2008;81:427–435. doi: 10.1259/bjr/54160649. [DOI] [PubMed] [Google Scholar]
- 7.Castillo MP, Samy RN, Isaacson B, Roland PS. Petrous apex cholesterol granuloma aeration: Does it matter? Otolaryngol Head Neck Surg. 2008;138:518–522. doi: 10.1016/j.otohns.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Fong BP, Brackmann DE, Telischi FF. The long-term follow-up of drainage procedures for petrous apex cholesterol granulomas. Arch Otolaryngol Head Neck Surg. 1995;121:426–30. doi: 10.1001/archotol.1995.01890040050008. [DOI] [PubMed] [Google Scholar]
- 9.Kimura R, Perlman HB. Arterial obstruction of the labyrinthine. Part I. Cochlear changes. Ann Otol Rhinol Laryngol. 1958;67:5–40. doi: 10.1177/000348945806700101. [DOI] [PubMed] [Google Scholar]
- 10.Keithley EM, Chen M-C, Linthicum F. Clinical diagnoses associated with histologic findings of fibrotic tissue and new bone in the inner ear. Laryngoscope. 1998;108:87–91. doi: 10.1097/00005537-199801000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Friedmann I, Graham MD. The ultrastructure of cholesterol granuloma of the middle ear. J Laryngol Otol. 1979;93:433–442. doi: 10.1017/s0022215100087272. [DOI] [PubMed] [Google Scholar]
- 12.Pfister MHF, Jackler RK, Kunda L. Aggressiveness in cholesterol granuloma of the temporal bone may be determined by the vigor of its blood source. Otol Neurotol. 2007;28:232–235. doi: 10.1097/MAO.0b013e31802bea4b. [DOI] [PubMed] [Google Scholar]