Abstract
Background
Patients’ beliefs about treatment influence treatment engagement and adherence. The Necessity-Concerns Framework postulates that adherence is influenced by implicit judgements of personal need for the treatment (necessity beliefs) and concerns about the potential adverse consequences of taking it.
Objective
To assess the utility of the NCF in explaining nonadherence to prescribed medicines.
Data sources
We searched EMBASE, Medline, PsycInfo, CDSR/DARE/CCT and CINAHL from January 1999 to April 2013 and handsearched reference sections from relevant articles.
Study eligibility criteria
Studies using the Beliefs about Medicines Questionnaire (BMQ) to examine perceptions of personal necessity for medication and concerns about potential adverse effects, in relation to a measure of adherence to medication.
Participants
Patients with long-term conditions.
Study appraisal and synthesis methods
Systematic review and meta-analysis of methodological quality was assessed by two independent reviewers. We pooled odds ratios for adherence using random effects models.
Results
We identified 3777 studies, of which 94 (N = 25,072) fulfilled the inclusion criteria. Across studies, higher adherence was associated with stronger perceptions of necessity of treatment, OR = 1.742, 95% CI [1.569, 1.934], p<0.0001, and fewer Concerns about treatment, OR = 0.504, 95% CI: [0.450, 0.564], p<0.0001. These relationships remained significant when data were stratified by study size, the country in which the research was conducted and the type of adherence measure used.
Limitations
Few prospective longitudinal studies using objective adherence measures were identified.
Conclusions
The Necessity-Concerns Framework is a useful conceptual model for understanding patients’ perspectives on prescribed medicines. Taking account of patients’ necessity beliefs and concerns could enhance the quality of prescribing by helping clinicians to engage patients in treatment decisions and support optimal adherence to appropriate prescriptions.
Introduction
Prescribing medicines is fundamental to the medical management of most long-term conditions. However, approximately half of this medication is not taken as directed, representing a failure to translate potentially effective treatment into optimal outcomes for patients and society [1], [2]. Where prescriptions are appropriate, this level of nonadherence has potentially serious consequences, both for individual patients, in terms of lost opportunities for health gain with increased morbidity and mortality [3], and for the health care system, in terms of wasted resources, increased use of services and hospital admissions [4].
In the absence of a single definitive intervention to address nonadherence [5], the NICE Medicines Adherence Guidelines amalgamate insights from trials of interventions and explanatory studies of nonadherence [1]. They apply a perceptions and practicalities approach [4] recognising that nonadherence may be both unintentional and intentional. Unintentional nonadherence occurs when the patient wants to adhere but is unable to because they lack capacity or resources. For example, they may not have understood the instructions, cannot afford copayment costs, or find it difficult to schedule, administer or remember the treatment. Intentional nonadherence occurs when the patient decides not to follow the recommendations. It is best understood in terms of the perceptual factors (e.g. beliefs and preferences) influencing motivation to start and continue with treatment.
Prescribing consultations do not occur in a vacuum. Patients (and prescribers) bring pre-existing beliefs about the illness and treatment [6], [7] which influence the patient’s evaluation of the prescription, their adherence and even beneficial [8] or adverse outcomes [9]. Interventions to optimise adherence tend to be more effective if they are tailored to the needs of the individual taking account of the perceptions of the treatment as well as practical abilities and resources that enable or impede their adherence [10]. Although the perceptual and practical dimensions of adherence are influenced by the social, cultural, economic and healthcare system contexts, taking account of the patient’s beliefs about the prescribed medication is fundamental to shared-decision making and supporting adherence [1], [11].
Research conducted with patients with a variety of long-term conditions suggests that the key beliefs influencing patients’ common-sense evaluations of prescribed medicines can be grouped under two categories: perceptions of personal need for treatment (Necessity beliefs) and Concerns about a range of potential adverse consequences [7], [12], [13]. This ‘Necessity-Concerns Framework (NCF)’ potentially offers a convenient model for clinicians to elicit and address key beliefs underpinning patients’ attitudes and decisions about treatment.
Over the past decade, a number of studies have been conducted, using a validated questionnaire, the Beliefs about Medicines Questionnaire [14] to quantify Necessity beliefs and Concerns in order to explore the relationship between these beliefs and adherence. This research spans a range of long-term medical conditions, across different settings and within various cultural groups. Many of the individual studies have demonstrated the utility of the NCF in explaining nonadherence to medication (e.g. [15]–[18]). It is therefore timely that a meta-analysis is performed to consolidate the results from these studies and to examine the explanatory value of the NCF in predicting adherence to medication prescribed for long-term medical conditions. In line with the underlying theory, we hypothesized that adherence in long-term conditions would be associated with stronger perceptions of Necessity for treatment and fewer Concerns about adverse consequences.
Methods
This review was conducted in line with the MOOSE guidelines for meta-analysis of observational trials [19].
Literature Search
A computerised literature search was conducted by the investigators on April 22nd, 2013 using EMBASE, Medline, PsycInfo, CDSR/DARE/CCT and CINAHL. The search strategy included the following terms:
BMQ or belief$
and
treatment$ or medicine$ or medication$
and
adheren$ or complian$
The search was limited to studies published from the year 1999 onwards (the year in which the BMQ was published). Duplicates were removed.
Inclusion and Exclusion Criteria
Identified studies were included in the meta-analysis if they met the following criteria:
participants were suffering from a long-term condition
participants were taking medication
participants were adults
the article was published in a peer-reviewed journal
the Necessity and/or Concerns subscales of the BMQ were used
a measure of adherence was employed
There were no restrictions based on language, or on cultural or geographical factors.
Titles and abstracts were screened for relevance, and the full text of relevant articles was obtained. Data from each article was extracted as described below.
Selection of Results When Multiple Relationships between Beliefs and Adherence Were Reported
Fifteen studies reported multiple associations of beliefs related to different adherence measurements (details reported in Table 1). Where the choice was between adherence measures, the most objective measure was selected for the meta-analysis. Therefore, electronic monitoring of adherence [20] and prescription redemption data [16] were chosen over self-report. Where data was presented for both ‘on demand’ and prophylactic medications, data for the prophylactic medication data were chosen [21], [22], for consistency with medications prescribed for other long-term conditions. In studies where cross-sectional and longitudinal data were both available, longitudinal data was used within the analysis [21], [23]–[26]. Where one group provided cross-sectional data at multiple timepoints, the timepoint with the fewest missing data points was selected [27]. If the choice was between two self report measures of adherence, we used the more commonly used measure. Thus the Morisky Medication Adherence Scale (MMAS) was chosen over the Brief Medication Questionnaire [28] and the ACTG adherence measure was used over the Walsh VAS scale [29]. Where patients within a sample were taking multiple medications and individual associations were provided for each medication [30], [31], the mean association was used within the meta-analysis but individual effect sizes are reported in Table 1 to facilitate comparison. Where data on two samples are reported within the same study [32], [33] we included both associations within the analysis.
Table 1. Summary Data for Included Studies.
| Author and date | Country | Illness Group | N | % male | Mean age (SD) | Study Design | Adherence measure | BMQ (number of items) | OR | p |
| Aakre et al. | USA | Comorbid | 44 | 45% | 51.1 (9.3) | Cross- | 1) Brief Medication | Necessity (5) | 1.467 | 0.523 |
| (2012) [171] | Serious Mental | sectional | Questionnaire | Concerns (6) | 0.977 | 0.969 | ||||
| Illness and Type | (Antipsychotic | Necessity (5) | 4.151 | 0.024 | ||||||
| II Diabetes | medication) | Concerns (6) | 0.673 | 0.520 | ||||||
| 2) Brief Medication Questionnaire (Hypoglycaemic medication) | ||||||||||
| Aflakseir | IRN | Type II | 102 | 22% | 40.7 (11.4) | Cross- | MARS 10 item version | Necessity (5) | 1.670 | 0.172 |
| (2012) [172] | Diabetes | sectional | see Barnes et al., 2004 | Concerns (5) | 0.169 | <0.001 | ||||
| Aikens et al. | USA | Depression | 82 | 21% | 42.9 (10.63) | Cross- | 1) General adherence: 4- | Necessity (5) | 2.097 | 0.075 |
| (2005) [28] | sectional | item MMASa | Concerns (5) | 0.247 | 0.001 | |||||
| 2) Recent adherence: 3- | Necessity (5) | 3.129 | 0.008 | |||||||
| item Brief Medication Questionnaire | Concerns (5) | 0.333 | 0.009 | |||||||
| Aikens & Piette | USA | Diabetes | 803 | 38% | 55.3 (11.8) | Cross- | Single item | Necessity (5) | 1.430 | 0.069 |
| (2009) [173] | sectional | Concerns (6) | 0.357 | <0.001 | ||||||
| Aikens & | USA | Depression | 163 | 38% | 35 (10) | Prospective | Brief Medication | Necessity (5) | 2.582 | 0.002 |
| Klinkman (2012) [174] | Questionnaire AND STAR*D Medication Adherence Questionnaire | Concerns (5) | 0.683 | 0.195 | ||||||
| Allen LaPointe | USA | Acute Coronary | 972 | 6 | Medians for 6 | Prospective | Self-report of no | Necessity (5) | 1.262 | 0.137 |
| et al. (2011) [31] | Syndrome | groups | groups | discontinuation nor | Concerns (5) | 0.549 | <0.001 | |||
| in range | between 56- | missed doses in last | Necessity (5) | 1.315 | 0.059 | |||||
| 66–74% | 61 SD not | month for 1) ACEI/ARB; | Concerns (5) | 0.546 | <0.001 | |||||
| reported | 2) Beta-blocker and 3) | Necessity (5) | 1.033 | 0.826 | ||||||
| Lipid-lowering therapy | Concerns (5) | 0.488 | <0.001 | |||||||
| Barnes et al. | NZ | Diabetes | 82 | Not | European 59.6 | Cross- | MARS plus two items re | Necessity (5) | 4.054 | 0.001 |
| (2004) [175] | reported | (12.7); Tongan 59.2 (11.2) | sectional | natural remedies | Concerns (5) | 1.670 | 0.213 | |||
| Batchelder et al. | USA | Comorbid HIV | 62 | 45% | 52.8 (7.3) | Cross- | 5-item MARS 1) | Necessity | 1.300 | 0.306 |
| (2013) [30] | and Type II | sectional | Antiretroviral 2) Diabetes | Concerns | 0.200 | 0.001 | ||||
| Diabetes | medication | Necessity | 1.050 | 0.878 | ||||||
| Concerns Unspecified | 0.450 | 0.041 | ||||||||
| Beck et al. | SWZ | Schizophrenia | 150 | 65.3% | 44.9 (11.7) | Cross- | Medication adherence | Necessity (5) | 1.942 | 0.029 |
| (2011) [176] | or Schizoaffective Disorder | sectional | subscale of the Service Engagement Scale (Tait et al., 2002)- clinician rated. Brief Adherence Rating Scale (BARS; Byerly et al., 2008) BARS selected for use here | Concerns (5) | 0.775 | 0.396 | ||||
| Berglund et al. | SWE | Statin Users | 414 | 50.8% | 64.2 (9.5) | Cross- | 4-item MMAS | Necessity (5) | 2.266 | <0.001 |
| (2013) [177] | sectional | Concerns (5) | 1.338 | 0.105 | ||||||
| Bhattacharya et | UK | Colorectal or | 43 | 44.2% | 64.5 (7.4) | Cross- | 5-item MARS | Necessity (5) | 1.408 | 0.562 |
| al. (2012) [178] | Breast Cancer | sectional | Concerns (5) | 0.570 | 0.352 | |||||
| Brown et al. | USA | Depression | 192 | 29% | 45.2 (16.0) | Cross- | 4-item MMAS | Necessity (5) | 1.235 | 0.425 |
| (2005) [179] | sectional (Longitudinal study but only baseline results reported) | Concerns (5) | 0.362 | <0.001 | ||||||
| Brown et al. (2013) [160] | USA | HIV | 116 | 58% | 45.3 (8.6) | Cross-sectional | VAS scale 0–100% used to rate adherence to each medication over the last month dichotomized at 95% | Necessity (8) | 2.357 | 0.014 |
| Butler et al. | UK | Renal | 58 | 66% | 48.0 (13) | Cross- | Electronic monitorsb | Necessity (5) | 4.871 | 0.003 |
| (2004) [180] | Transplant | sectional | Concerns (7) | 0.517 | 0.184 | |||||
| Byer & Myers | UK | Asthma | 64 | 50% | 39.6 (13.83) | Cross- | 1) Number of preventer | Necessity (5) | 5.915 | 0.001 |
| (2000) [16] | sectional | inhaler prescriptions | Concerns (5) | – | – | |||||
| collecteda | Necessity (5) | 3.129 | 0.05 | |||||||
| 2) Number of reliever | Concerns (5) | – | – | |||||||
| inhaler prescriptions | Necessity (5) | 5.915 | 0.001 | |||||||
| collected | Concerns (5) | – | – | |||||||
| 3) Self-reported adherence | ||||||||||
| Byrne et al. | IRE | Coronary Heart | 1084 | 65% | 66.0 (9.1) | Cross- | 5-item MARS | Necessity (5) | 2.551 | <0.001 |
| (2005) [17] | Disease | sectional | Concerns (5) | 0.669 | <0.001 | |||||
| Chisholm-Burns | USA | Renal | 512 | 61.1% | 52.4 (10.7) | Cross- | Immunosuppressant | Necessity (5) | 2.065 | <0.001 |
| et al. | Transplant | sectional | Therapy Adherence Scale | Concerns (5) | ||||||
| (2012) [181] | (ITAS) <12 non-adherence | |||||||||
| Clatworthy et al. | UK | Bipolar | 223 | 36% | 48 (11.2) | Cross- | 5-item MARS | Necessity (5) | 2.114 | 0.006 |
| (2009) [18] | Disorders | sectional | Concerns (6) | 0.371 | 0.001 | |||||
| Clifford et al. | UK | Chronic illness | 146 | 52% | 64.3 (12.06) | Longitudinal | Telephone call (“When | Necessity (5) | 1.764 | 0.090 |
| (2008) [142] | was the last time you missed a dose of this medicine?”). Nonadherence defined as any dose missed in the previous 7 daysb | Concerns (5) | 0.457 | 0.020 | ||||||
| Cooper et al., | UK | HIV | 234 | 84% | 42 (8.9) | Longitudinal | At 48 weeks MASRI | Necessity (15) | 1.863 | 0.010 |
| (2011) [182] | (Walsh et al., 2002) scale- VAS % taken over last month dichotomized at 95% | Concerns (8) | 0.499 | 0.004 | ||||||
| de Boer-van der | NTL | HIV | 341 | 90% | 45 | Cross- | Self report % of | Necessity (8) | 1.600 | 0.018 |
| Kolk et al. (2008) [183] | sectional | prescribed medicines taken | Concerns (11) | 0.070 | 0.075 | |||||
| De Las Cuevas | ESP | Affective | 167 | 23.4% | 56.1 (12.3) | Cross- | 4-item MMAS | Necessity (5) | 1.111 | 0.710 |
| et al. (2013) [184] | Disorders | sectional | Concerns (5) | 2.521 | 0.002 | |||||
| De Smedt et al. | NTL | Heart Failure | 960 | 63.6% | 69.6 (11.9) | Cross- | SECope non-adherence | Necessity (5) | 1.257 | 0.616 |
| (2012) [185] | sectional | subscale (Johnson & Neilands, 2007) | Concerns (5) | 0.484 | 0.112 | |||||
| de Thurah et al. | DMK | Rheumatoid | 91 | 36% | Median 63 | Prospective | CQ-R 1) 9 months 2) | Necessity (5) | 9.600 | <0.001 |
| (2010) [21] | Arthritis | baseline | Concerns (5) | 0.420 | 0.132 | |||||
| Necessity (5) | 3.630 | 0.016 | ||||||||
| Concerns (5) | 0.793 | 0.652 | ||||||||
| Ediger et al | CAN | IBD | 326 | 40% | 41.0 (14.06) | Cross- | 5-item MARSb | Necessity (5) | 1.522 | 0.039 |
| (2007) [186] | sectional | Concerns (5) | 0.677 | 0.054 | ||||||
| Emilsson et al. | SWE | Asthma | 35 | 28.6% | 52.9 (14.7) | Cross- | Pill count | Necessity (5) | 4.438 | 0.032 |
| (2011) [187] | sectional | Concerns (5) | 0.555 | 0.365 | ||||||
| Fawzi et al. | EGT | Depression or | 108 | 33.3% | 61.3 (5.3) | Cross- | 10-item MARS | Necessity (5) | 3.712 | 0.001 |
| (2012) [188] | Adjustment Disorder with Depressed Mood | sectional | (Thompson et al., 2000) MARS chosen and GAM (global adherence measure- 1 item) | Concerns (5) | 0.269 | 0.001 | ||||
| Foo et al. | SGP | Glaucoma | 344 | 64.8% | 66.1 (10.2) | Cross- | 8-item MMAS dichot. at | Necessity (4) | 1.045 | 0.837 |
| (2012) [189] | sectional | 8 | Concerns (5) | 2.778 | <0.001 | |||||
| French et al. | UK | Type II | 453 | 57.4% | 65.9 (10) | Prospective | 5-item MARS 1) Baseline | Necessity (5) | 1.295 | 0.232 |
| (2013) [23] | Diabetes | 2) Prospective | Concerns (5) | 0.525 | 0.004 | |||||
| Necessity (5) | 1.800 | 0.013 | ||||||||
| Concerns (5) | 0.116 | <0.001 | ||||||||
| Gauchet et al. | FRA | HIV | 127 | 78% | 39.7 (9.2) | Cross- | 16-item self-report | Necessity (5) | 3.264 | 0.001 |
| (2007) [190] | sectional | measure (devised by authors) | Concerns (5) | 0.865 | 0.656 | |||||
| Gatti et al. | USA | Chronic illness | 275 | 27% | - | Cross- | 8-item MMAS dichot. at | Necessity (5) | 1.239 | 0.331 |
| (2009) [191] | sectional | 1 | Concerns (6) | 0.357 | <0.001 | |||||
| George & | CAN | Heart Failure | 350 | 69% | 61.0 (12.6) | Cross- | 1) Prescription dispensing | Necessity (5) | ||
| Shalansky | sectional | data (nonadherence | Concerns (5) | 1.529 | 0.069 | |||||
| (2007) [192] | defined as <90% mean refill adherence)b2) 4-item MMASc | 0.954 | 0.839 | |||||||
| Gonzalez et al. | USA | HIV | 325 | 60% | 40.9 (8.5) | Longitudinal | 1) ACTG | Necessity (8) | 1.494 | 0.048 |
| (2007) [20] | randomised | 2) MEMS cap – one drug | Concerns (11) | 0.459 | <0.001 | |||||
| trial | in each participant’s | Necessity (8) | 1.494 | 0.048 | ||||||
| regimen monitored, usually the protease inhibitor (% adherence)a | Concerns (11) | 0.720 | 0.106 | |||||||
| Griva et al. | UK | Kidney | 218 | 59.6% | 49.7 (12.3) | Cross- | 5-item MARS item plus | Necessity (5) | 7.278 | <0.001 |
| (2012) [193] | Transplant | sectional | serum immunosuppressant concentrations | Concerns (5) | ||||||
| Grunfeld et al | UK | Breast Cancer | 110 | 0% | 56.3 (7.0) | Cross- | 1) Asked “In the pastc | Necessity (5) | 2.916 | 0.007 |
| (2005) [194] | sectional | week have you taken your tamoxifen everyday?” (Yes/No)b 2) 5-item MARS | Concerns (5) | 0.868 | 0.708 | |||||
| Hedenrud et al. | SWE | Migraine | 174 | 16% | Not calculable | Cross- | 5-item MARSb | Necessity (5) | 0.747 | 0.309 |
| (2008) [195] | sectional | Concerns (5) | 0.588 | 0.064 | ||||||
| Horne et al. | UK | Cardiac and | 210 | 49% | 50.8 (16.2) | Cross- | 4-item RAM | Necessity (5) | 2.018 | 0.006 |
| (1999) [14] | General Medical (pooled data) | sectional | Concerns (5) | 0.347 | <0.001 | |||||
| Horne & | UK | Asthma, Renal | 324 | 54% | 54.1 (15.96) | Cross- | 4-item MARS | Necessity (5) | 2.180 | <0.001 |
| Weinman (1999) [7] | Cardiac, Oncology (pooled data) | sectional | Concerns (5) | 0.281 | <0.001 | |||||
| Horne et al. | UK | Renal | 47 | 49% | 49.0 (17.3) | Cross- | Single item: ‘How often | Necessity (5) | 1.115 | 0.842 |
| (2001) [196] | (Haemodialysis) | sectional | do you deliberately miss a dose of medication?’ | Concerns (5) | 0.215 | 0.010 | ||||
| Horne & | UK | Asthma | 100 | 39% | 49.3 (18.1) | Cross- | 9-item MARS | Necessity (6) | 3.405 | 0.002 |
| Weinman | sectional | Concerns (11) | 0.178 | <0.001 | ||||||
| (2002) [166] | ||||||||||
| Horne et al. | UK | HIV | 109 | 97% | 41.2 (9.0) | Cross- | Single item: ‘How much | Necessity (8) | 1.773 | 0.126 |
| (2004) [197] | sectional | of your HAART medication did you take within two hours of when you were supposed to?’b | Concerns (11) | 0.524 | 0.095 | |||||
| Horne et al. | UK | HIV | 117 | 96% | 37.8 (8.4) | Prospective | Single item: VAS from | Necessity (6) | 2.477 | 0.008 |
| (2007) [198] | follow-up | MASRIb | Concerns (7) | 0.298 | <0.001 | |||||
| Horne et al. | UK | IBD | 1871 | 37% | 50 (16.0) | Cross- | 4-item MARS | Necessity (8) | 1.790 | <0.001 |
| (2009) [167] | sectional | Concerns (9) | 0.600 | <0.001 | ||||||
| Horne et al. | UK | Hypertension | 230 | 88% | 67.6 | Prospective | 1) 6- item MARS– | Necessity (5) | 1.675 | 0.096 |
| (2010) [24] | baseline | Concerns (6) | 0.464 | 0.013 | ||||||
| 2) 6-item MARS | Necessity (5) | 1.007 | 0.987 | |||||||
| Prospective (Compared to tablet count for 48% of sample) | Concerns (6) | 0.195 | <0.001 | |||||||
| Hou et al. | UK | Bipolar | 35 | 28.6% | 45 (11) | Cross- | MMAS 4-item (dichot. at | Necessity (5) | 0.881 | 0.837 |
| (2010) [199] | Affective Disorder | sectional | 1) | Concerns (5) | 0.680 | 0.532 | ||||
| Hunot et al. | UK | Depression | 178 | 25% | 40.1 (12.6) | Longitudinal | 1) Single item: current | Necessity (5) | 3.346 | <0.001 |
| (2007) [200] | antidepressant use/non-use (“Are you currently taking antidepressants?”)b 2) MARSc 3) Prescription refill datac | Concerns (6) | 0.223 | <0.001 | ||||||
| Iihara et al | JPN | Hospital | 151 | 62.3% | – | Cross- | Measure based on MMAS | Necessity (5) | 1.998 | 0.020 |
| (2010) [201] | Inpatients | sectional | Concerns (5) | 0.593 | 0.079 | |||||
| Johnson et al. | USA | HIV | 295 | 100% | 45.2 (10.1) | Cross- | 1) ACTG 3 days (% | Necessity (5) | 0.960 | 0.365 |
| (2012) [29] | sectional | taken) dichot. at 100%a | Concerns (5) | 0.930 | 0.058 | |||||
| 2) Walsh VAS 0–100% | Necessity (5) | 1.020 | 0.572 | |||||||
| last 30 days dichot at 100% | Concerns (5) | 0.960 | 0.273 | |||||||
| Jonsdottir et al. | UK | Schizophrenia/ | 280 | 51% | 35.1 | Cross- | VAS (0%–100%) | Necessity (8) | 5.887 | <0.001 |
| (2009) [202] | Bipolar disorder | sectional | Concerns (9) | 0.493 | 0.057 | |||||
| Kemp et al. | UK | Epilepsy | 37 | 51% | 40.7 (SD not | Cross- | Low-dose of | Necessity (5) | 0.441 | 0.200 |
| (2007) [203] | reported) | sectional | phenobarbital indicative of nonadherence, and/or measurement of antiepileptic drug levels | Concerns (5) | 0.599 | 0.414 | ||||
| Khanderia et al. | USA | Coronary Artery | 132 | 83% | 65.8 (10.1) | Cross- | 4-item MMASb | Necessity (5) | 1.050 | 0.875 |
| (2008) [204] | Bypass Graft | sectional | Concerns (5) | 0.584 | 0.092 | |||||
| Kressin et al. | USA | Hypertension | 806 | 35% | 59 | Cross- | Hill-Bone Compliance to | Necessity (5) | 1.414 | 0.200 |
| (2010) [205] | sectional | High Blood Pressure Therapy Scale, 9 item adherence subscale | Concerns (5) | 0.525 | <0.001 | |||||
| Kronish et al | USA | Stroke or TIA | 600 | 60.6% | 63.4 (11.2) | Cross- | 8-item MMAS dichot. at | Necessity (5) | 1.120 | 0.557 |
| (2013) [206] | sectional | > = 6 | Concerns (4) (modified items) | 0.193 | <0.001 | |||||
| Kung et al. | NZ | Heart, Liver, | 326 | 64.4% | Heart | Cross- | Immunosuppressant | Necessity (5) | 1.605 | 0.021 |
| (2012) [207] | Lung Transplant | transplant: 54.4 (11.8) Lung transplant 49.3 (13.1) Liver transplant 55.1 (12.3) | sectional | Therapy Adherence Scale (ITAS) <12 non-adherence | Concerns (5) | 0.493 | 0.001 | |||
| Llewellyn | UK | Haemophilia | 65 | 100% | 36.4 (12.2) | Cross- | 1) Adherence to | Necessity (5) | 5.915 | 0.001 |
| et al. (2003) [22] | sectional | frequency of prophylactic | Concerns (5) | 0.599 | 0.270 | |||||
| infusion with clotting | Necessity (5) | 4.241 | 0.004 | |||||||
| factora 2) Adherence to recommended ‘on demand’ dose of clotting factor 3) Adherence to recommended dose of clotting factorc | Concerns (5) | 0.897 | 0.813 | |||||||
| Maguire et al. | UK | Hypertension | 327 | 46% | Not reported | Cross- | 4-item RAM | Necessity (5) | 0.665 | 0.242 |
| (2008) [208] | sectional | Concerns (5) | 0.422 | 0.014 | ||||||
| Mahler et al. | GMY | Mixed Chronic | 360 | 53.3% | 69.5 range 19– | Cross- | 5-item MARS D | Necessity (5) | 2.097 | <0.001 |
| (2012) [209] | Illness | 95 | sectional | Concerns (5) | 0.515 | 0.001 | ||||
| Maidment | UK | Depression | 67 | 49% | 74.2 (6.1) | Cross- | Global Adherence | Necessity (5) | 3.002 | 0.020 |
| et al. (2002) [15] | (older adults) | sectional | Measure (single rating by interviewer) | Concerns (5) | 0.247 | 0.004 | ||||
| Menckeberg et | NTL | Asthma | 238 | 33% | 36.2 (6.3) | Cross- | 5-item MARS | Necessity (9) | 3.878 | <0.001 |
| al. (2008) [210] | sectional | Concerns (12) | 0.496 | 0.004 | ||||||
| Moshkovska et | UK | Ulcerative | 169 | 51% | 49 (SD not | Cross- | 1) 12 item study specific | Necessity (5) | 1.976 | 0.002 |
| al. (2009) [211] | Colitis | reported) | sectional | self report questionnaire | Concerns (6) | 0.639 | 0.035 | |||
| Nakhutina et al. | USA | Epilepsy | 72 | 37.5% | 44 (14.2) | Cross- | 4-item MMAS | Necessity (5) | 1.388 | 0.455 |
| (2011) [212] | sectional | Concerns (5) | 0.694 | 0.406 | ||||||
| Neame & | UK | Rheumatoid | 344 | 33% | 49.5% aged | Cross- | Single item: ‘I often do | Necessity (5) | 0.885 | 0.737 |
| Hammond (2005) [213] | Arthritis | over 65 | sectional | not take my medicines as directed’b | Concerns (5) | 0.313 | 0.002 | |||
| Nicklas et al. | UK | Chronic Pain | 217 | – | – | Cross- | 6-item MARS | Necessity (5) | 2.018 | 0.005 |
| (2010) [214] | sectional | Concerns (5) | 0.645 | 0.079 | ||||||
| O’Carroll et al. | UK | Liver | 33 | 52% | 55.8 (13.37) | Cross- | 1) ‘Medication adherence’ | Necessity (5) | 1.734 | 0.411 |
| (2006) [215] | Transplant | sectional | factor of the Transplant Effects Questionnaire (TxEQ) 2) 5-item MARSc | Concerns (5) | 0.137 | 0.009 | ||||
| O’Carroll et al. | UK | Ischaemic | 180 | 54% | 69 (11.4) | Cross- | 5-item MARS with | Necessity (5) | 0.705 | 0.202 |
| (2011) [25] | Stroke | sectional | salicyclic acid/creatinine | Concerns (5) | 0.209 | <0.001 | ||||
| 1) Baseline | Necessity (5) | 0.778 | 0.359 | |||||||
| 2) Prospective | Concerns (5) | 0.328 | <0.001 | |||||||
| Ovchinikova et | AUS | Asthma | 134 | 31% | 53 (19) | Longitudinal | MARS 1) Baseline 2) | Necessity (5) | 1.429 | 0.262 |
| al. (2011) [26] | Prospective | Concerns (5) | 0.220 | <0.001 | ||||||
| Necessity (5) | 1.328 | 0.387 | ||||||||
| Concerns (5) | 0.278 | <0.001 | ||||||||
| Percival et | AUS | Heart Failure | 43 | 83.7% | 64.2 (17.1) | Cross- | 5-item MARS dichot. at | Necessity (5) | 3.068 | 0.165 |
| al.(2012) [216] | sectional | 23 | Concerns (5) | 0.508 | 0.399 | |||||
| Peters et al. | USA | Marfan | 174 | 42% | 39.8 (12.2) | Cross- | 3-item self-report measure | Necessity (5) | 1.299 | 0.417 |
| (2001) [217] | Syndrome | sectional | (adapted from MARS) | Concerns (5) | 0.424 | 0.010 | ||||
| Phatak & | USA | Hypertension, | 250 | 38% | <30 (11.2%) | Cross- | 9-item MMAS | Necessity (5) | 1.550 | 0.059 |
| Thomas | Arthritis, Back | 30–39 (14%) | sectional | Concerns (6) | 0.215 | <0.001 | ||||
| (2006) [218] | Problems, | 40–49 (37.2%) | ||||||||
| Asthma, | 50–59 (24.4%) | |||||||||
| Hypercholesterolemia | >60 (13.2%) | |||||||||
| Rajpura & | USA | Hypertension | 117 | 64.1% | 55–65 (23.9%) | Cross- | MMAS | Necessity (5) | 2.551 | 0.008 |
| Nayak (2013) | and aged 55 or over | >65 (52.1%) | sectional | Concerns (5) | 0.423 | 0.014 | ||||
| Rees et al. | AUS | Glaucoma | 131 | 61.1% | 67.7 (13.6) | Cross- | 4-item RAM | Necessity (5) | 1.966 | 0.035 |
| (2010) [219] | sectional | Concerns (8) | 0.651 | 0.180 | ||||||
| Rees et al. | USA, | Glaucoma | 475 | 55.4% | African | Cross- | 4-item RAM | Necessity (5) | 2.385 | <0.001 |
| (2013) [220] | SGP, AUS | Americans: 69.6 (12.4) White Americans: 68.65 (13.0) Australians: 69.2 (13.1) Singaporeans: 65.1 (11.8) | sectional | Concerns (8) | 0.414 | <0.001 | ||||
| Reynolds et al | USA | Osteoporosis | 193 | 0% | Cross- | Osteoporosis Specific 8- | Necessity (5) | 3.405 | <0.001 | |
| (2012) [221] | sectional | item MMAS | Concerns (6) | 0.424 | 0.005 | |||||
| Ross et al. | UK | Hypertension | 515 | 52% | 59.9 (12.16) | Cross- | 4-item MMASb | Necessity (5) | 3.060 | 0.001 |
| (2004) [159] | sectional | Concerns (5) | ||||||||
| Ruppar et al. | Hypertension | 33 | 21% | 70.6 (9.1) | Prospective | MEMS for 6 weeks post- | Necessity (5) | 0.501 | 0.306 | |
| (2012) [222] | BMQ | Concerns (5) | 0.254 | 0.053 | ||||||
| Russell & | NZ | Depression | 85 | 28% | 43.7 (11.5) | Cross- | 5-item MARS | Necessity (5) | 1.115 | 0.786 |
| Kazantzis (2008) [223] | sectional | Concerns (14) | 0.269 | 0.002 | ||||||
| Schoenthaler et | USA | Type II | 608 | 48% | 62.1 (9.2) | Cross- | MPR over last 2 years | Necessity (5) | 0.757 | 0.060 |
| al. (2012) [224] | Diabetes | sectional | Concerns (5) | 0.878 | 0.380 | |||||
| Schuz et al. | GMY | Older Adults | 309 | 59.3% | 73.3 (5.1) | Longitudinal | 2 items from RAM | Necessity (2) | 1,353 | 0.155 |
| (2011) [225] | with Comorbid Illnesses | Concerns (2) | 0.590 | 0.014 | ||||||
| Shiyanbola & | USA | Diabetes | 16 | 0% | 46.1 (10.2) | Cross- | 4-item MMAS | Necessity (5) | 0.917 | 0.931 |
| Nelson (2011) [226] | sectional | Concerns (5) | 1.539 | 0.671 | ||||||
| Sirey et al. | USA | Older Adults | 299 | 22.1% | Nonadherent | Cross- | 4-item MMAS | Necessity (5) | 1.182 | 0.435 |
| (2013) [227] | with Comorbid Illnesses | 75.6 (7.3); Adherent 76.7 (7.4) | sectional | Concerns (5) | 0.494 | 0.001 | ||||
| Sofianou et al. | USA | Asthma | 242 | 16.1% | 67.4 (6.8) | Cross- | 10-item MARS | Necessity (5) | 2.353 | <0.001 |
| (2012) [228] | sectional | Concerns (5) | 0.437 | 0.001 | ||||||
| Tibaldi et al., | Italy | Chronic illness | 427 | 45% | 59 (14) | Cross- | 5-item MARS | Necessity (5) | 1.314 | 0.123 |
| (2009) [229] | sectional | Concerns (6) | 0.488 | <0.001 | ||||||
| Sud et al., | USA | Acute Coronary | 208 | 60.6% | 64.9 (13.0) | Cross- | 4-item MMAS | Necessity (5) | 1.800 | 0.022 |
| (2005) [60] | Syndrome | sectional | Concerns (5) | 0.720 | 0.198 | |||||
| Trachtenberg et | USA, UK | Thalassemia | 371 | 47.4% | 24.0 (12.6) | Longitudinal | Self-reported number of | Necessity (5) | 0.694 | 0.256 |
| al. (2012) [32] | doses taken in the past | Concerns (5) | 0.964 | 0.910 | ||||||
| week and month 1) DFO | Necessity (5) | 1.115 | 0.633 | |||||||
| 2) Oral iron chelator; serum ferritin, liver biopsy, liver iron concentration. | Concerns (5) | 0.720 | 0.152 | |||||||
| Treharne et al. | UK | Rheumatoid | 85 | 25% | 58.9 (12.64) | Cross- | 1) 19-item CQR | Necessity (5) | 31.758 | <0.001 |
| (2004) [230] | Arthritis | sectional | 2) 2 items from the MARSc | Concerns (5) | 0.621 | 0.239 | ||||
| Unni & Farris | USA | Cholesterol | 420 | 54.4% | Cholesterol: | Cross- | Medication Adherence | Necessity (5) | 0.981 | 0.925 |
| (2011)a [33] | Loweing | 59.4; Asthma: | sectional | Reasons Scale (4 types of | Concerns (5) | 0.265 | <0.001 | |||
| Medication or | 48.7 | non-adherence for each | Necessity (5) | 1.714 | 0.004 | |||||
| Asthma Maintenance Medication Patients | medication combined into any or none) | Concerns (5) | 0.506 | <0.001 | ||||||
| Unni & Farris | USA | Older Adults | 1061 | 45.6% | Adherent: | Cross- | 4-item MMAS 1) time 1; | Necessity (5) | 1.010 | 0.931 |
| (2011)b [27] | 73.2 (9.2) | sectional | 2) time 2 | Concerns (5) | 0.462 | <0.001 | ||||
| Non-adherent: | (two time | Necessity (5) | 1.075 | 0.560 | ||||||
| 72.5 (5.5) | points) | Concerns (5) | 0.503 | <0.001 | ||||||
| Uusküla et al. | EST | HIV | 161 | 55% | ≤30 N = 45 | Cross- | Recall of proportion of | Necessity (6) | 1.516 | 0.442 |
| (2012) [231] | >30 N = 82 | sectional | total doses prescribed taken during past 3 days | Concerns (7) | 0.250 | 0.073 | ||||
| Van den Bemt | NTL | Rheumatoid | 228 | 33% | 56.2 (12.2) | Cross- | Self-report | Necessity (5) | 1.516 | 0.442 |
| et al. (2009) [232], [233] | Arthritis | sectional | Concerns (5) | 0.392 | <0.001 | |||||
| Voils et al. | USA | Hypertension | 201 | 86% | 64.1 (11.0) | Cross- | 8-item MMAS | Necessity (5) | 1.516 | 0.442 |
| (2012) [233] | sectional | Concerns (5) | 0.392 | <0.001 | ||||||
| Wileman et al. | UK | End-Stage | 76 | 60.5% | 63.1 (15.4) | Cross- | Medications adherence | Necessity (5) | 1.641 | 0.270 |
| (2011) [234] | Renal Disease | sectional | quesionnaire (MAQ) plus serum phosphate level > = 1.8 mmol/l | Concerns (5) | 0.750 | 0.521 | ||||
| Wong & | UK | Rheumatoid | 68 | 40% | 55.8 (13.0) | Longitudinal | Patient report of drug | Necessity (5) | 1.319 | 0.568 |
| Mulherin (2007) [235] | Arthritis | continuation at 1 year versus discontinuationb | Concerns (5) | 0.870 | 0.774 | |||||
| Yu et al. | SGP | Peritoneal | 20 | 60% | 64.4 (11.6) | Cross- | Specially designed 5 item | Necessity (5) | 1.828 | 0.499 |
| (2012) [236] | Dialysis | sectional | scale with 5 non-adherent behaviours, rated on 5 point Likert scale plus serum phosphate >1.78 mmol/l | Concerns (5) | 0.913 | 0.918 | ||||
| Zerah et al. | FRA | Patients taking | 182 | 21% | Median 47 | Cross- | 4-item MMAS | Necessity (5) | 2.008 | 0.042 |
| (2012) [237] | Glucocorticoids | [range 33–61] | sectional | Concerns (5) | 0.484 | 0.035 |
Note. NZ = New Zealand; IRE = Ireland; NTL = Netherlands; CAN = Canada; FRA = France; SWE = Sweden; IRN = Iran; SWZ = Switzerland; ESP = Spain; DMK = Denmark; EGT = Egypt; SGP = Singapore; JPN = Japan; EST = Estonia; GMY = Germany; AUS = Australia; IBD = inflammatory bowel disorder; TIA = Transient Ischemic Attack; MARS is the Medication Adherence Rating Scale from Thompson, Kulkarni, & Sergejew (2000); MEMS is Medication Event Monitoring System; CQ-R is the Compliance Questionnaire-Rheumatology from de Klerk, van der Heijde, Landewé, van der Tempel, & van der Linden (2003); MMAS is the Morisky Medication Adherence Scale from Morisky, Green, & Levine (1986); TxEQ is the Transplant Effects Questionnaire from Ziegelmann et al. (2002); ACTG is the Adherence to Combination Therapy Guide from Chesney et al., 2000; RAM is the Reported Adherence to Medication Scale from Horne et al., (1999), renamed MARS (Medication Adherence Report Scale); VAS = visual analogue scale.
Adherence result selected for use in meta-analysis;
Adherence measure dichotomised into adherent and nonadherent groups;
Relationship between adherence measure and BMQ scales not reported.
Data Extraction
The following information was extracted from papers onto coding forms: author names, date of publication, the country in which the research was conducted (dichotomized into UK or non-UK), sample size, illness group, sex (% male), mean age, study design (cross-sectional, longitudinal or prospective), the number of Necessity and Concerns items included (since items may be added specific to the medication prescribed), the adherence measure used, information (means and standard deviations, odds ratios and 95% confidence intervals or correlation coefficients) to calculate the effect size between adherence and Necessity beliefs and Concerns, and the p-value. Where the full required statistics were not reported, authors were contacted for further information.
Methodology/Quality Assessment
A simple methodology assessment tool was devised for this study. Methodology was assessed by two of three independent expert raters (SC, RP and VC) using the following parameters:
study location (UK or non-UK)
study design (cross-sectional or longitudinal/prospective)
measure of adherence (self-report or objective measure [electronic monitors, prescription redemption, blood test results]).
sample size (<82 = 0 or ≥82 = 1). This was based on the sample needed to detect a medium effect size for a correlation (r = 0.3) with an alpha level of 0.05 and 80% power.
Ratings were completed independently and then combined. There were no disagreements regarding ratings.
Statistical Analysis
The primary outcome measure was adherence to medication. For each study, the effect size was expressed as an odds ratio with 95% confidence intervals. Where studies reported the standard mean difference or correlation coefficient, the effect size was converted into an odds ratio, using the Comprehensive Meta-Analysis program. We used a random effects model to accommodate heterogeneity between studies which was anticipated due to differences with respect to sample characteristics, study design and the adherence measure used.
The presence of significant heterogeneity across studies was examined using the chi-squared statistic (Q). The magnitude of this heterogeneity across studies was estimated using the I 2 statistic [34], which assesses the percentage of variance among studies which is not due to chance.
Sensitivity analyses were conducted to ascertain whether the effect sizes seen were robust when individual studies, or studies grouped based on the methodological factors described above were excluded.
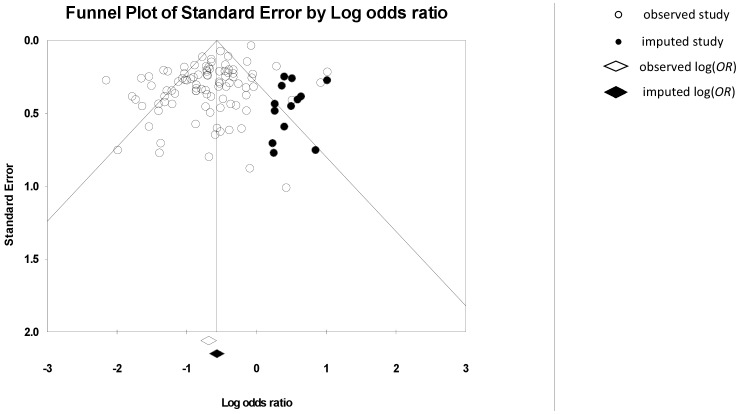
Orwin’s fail-safe N [35], [36] was calculated to estimate the number of unpublished studies necessary to reverse any conclusion that a significant effect exists (based on the conservative assumption that unpublished studies would have effect sizes of equal magnitude but opposite direction to the overall effect size in this meta-analysis). Egger’s t-test and funnel plots were also used to test for publication bias, in line with recent recommendations [37].
Results
Selection of Studies
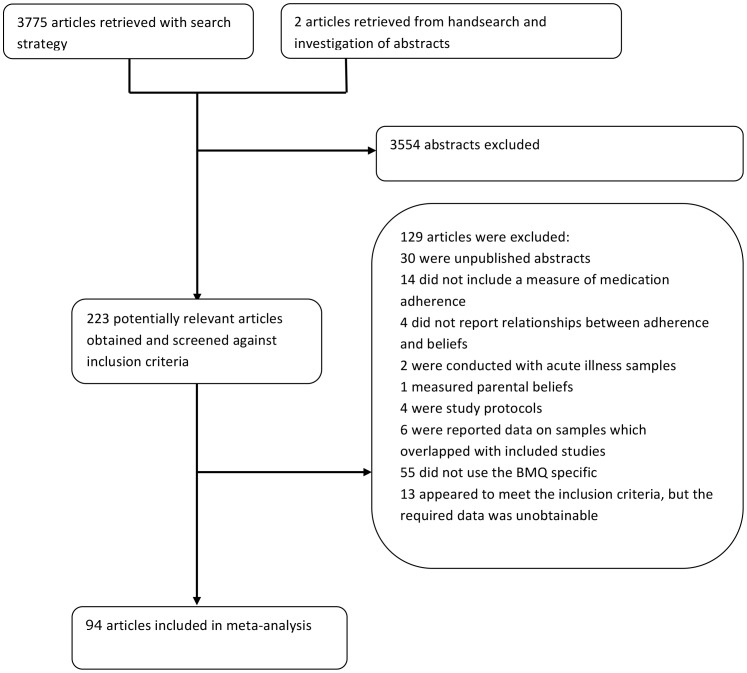
Ninety-four percent (3554) of the 3775 studies retrieved were rejected after checking the titles and abstracts against the selection criteria above (Figure 1). 223 relevant articles were identified. A search of the reference lists of these articles revealed one further relevant study [38].
Figure 1. Selection process for study inclusion.
Of the 223 studies identified, a further 129 were excluded (Figure 1). Thirty of these were unpublished studies and conference proceedings. These were investigated further and authors were contacted where necessary to clarify whether unpublished work had led to publications [39]–[45]. Sixteen studies [44], [46]–[59] [60] had since been published, fifteen of which already formed part of the included list and one additional eligible study was available online early [61]. Six papers reported data on samples which overlapped with included studies [62]–[67], and four were protocols for ongoing studies [68]–[71].
Thirteen studies were excluded because they did not include a measure of medication adherence [72]–[85]. Two of these included separate assessment modes for intentional and unintentional adherence but no overall adherence assessment [80], [85]. Fifty-five studies did not use the BMQ Specific scales [86]–[140]. Four studies were excluded because the relationship between treatment beliefs and adherence behaviour was not reported [24], [141]–[143]. Two articles were conducted in acute rather than long-term condition samples (influenza [144] and antibiotic use [145]) and one article was excluded because parental beliefs about medicine were measured [146]. Thirteen studies study met the inclusion criteria but the article did not contain the required statistical information. We contacted the authors but were unable to obtain the relevant data [38], [147]–[158]. Thus, once screened against the inclusion criteria, 94 articles were retained for inclusion in the meta-analysis. Table 1 provides a summary of each of the studies included in the meta-analysis.
Three of the included studies [16], [159], [160] reported associations between adherence and Necessity beliefs, but not Concerns. The authors of these articles were contacted, but the data for Concerns was unavailable. Two studies [32], [33] reported two largely non-overlapping samples for both Necessity beliefs and Concerns. Thus, data for 91 studies and 93 comparisons for Concerns, and data for 94 studies and 96 comparisons for Necessity beliefs, were included in the meta-analysis.
Sample Characteristics
The mean age of participants in the 94 included studies ranged from 24.0 to 74.2, with an overall mean age of 55.8 (it was not possible to calculate the mean age in 13 studies). The percentage of males ranged from 0–100% (breast cancer and haemophilia samples respectively), with an overall percentage of males of 49.7% male (excluding 3 studies where it was not possible to calculate the number of males). Sample sizes ranged from 16 to 1871.
The total sample, N = 25,072, encompassed patients with asthma, renal disease, organ transplantation, dialysis chronic pain, kidney transplantation, cancer, cardiovascular disorders, Marfan’s syndrome, depression, haemophilia, diabetes, HIV, rheumatoid arthritis, osteoporosis, thalassemia, inflammatory bowel disease, bipolar disorder, schizophrenia, epilepsy, migraine, back problems, glaucoma and mixed chronic illness.
Thirty-three studies (35.1%) used the MARS to measure adherence, 20 used the Morisky Medication Adherence Scale (21.2%), 3 used pharmacy refill (3.2%), 3 used electronic monitoring (3.2%) and two or fewer studies used the remaining measures.
Effect Sizes
Necessity beliefs
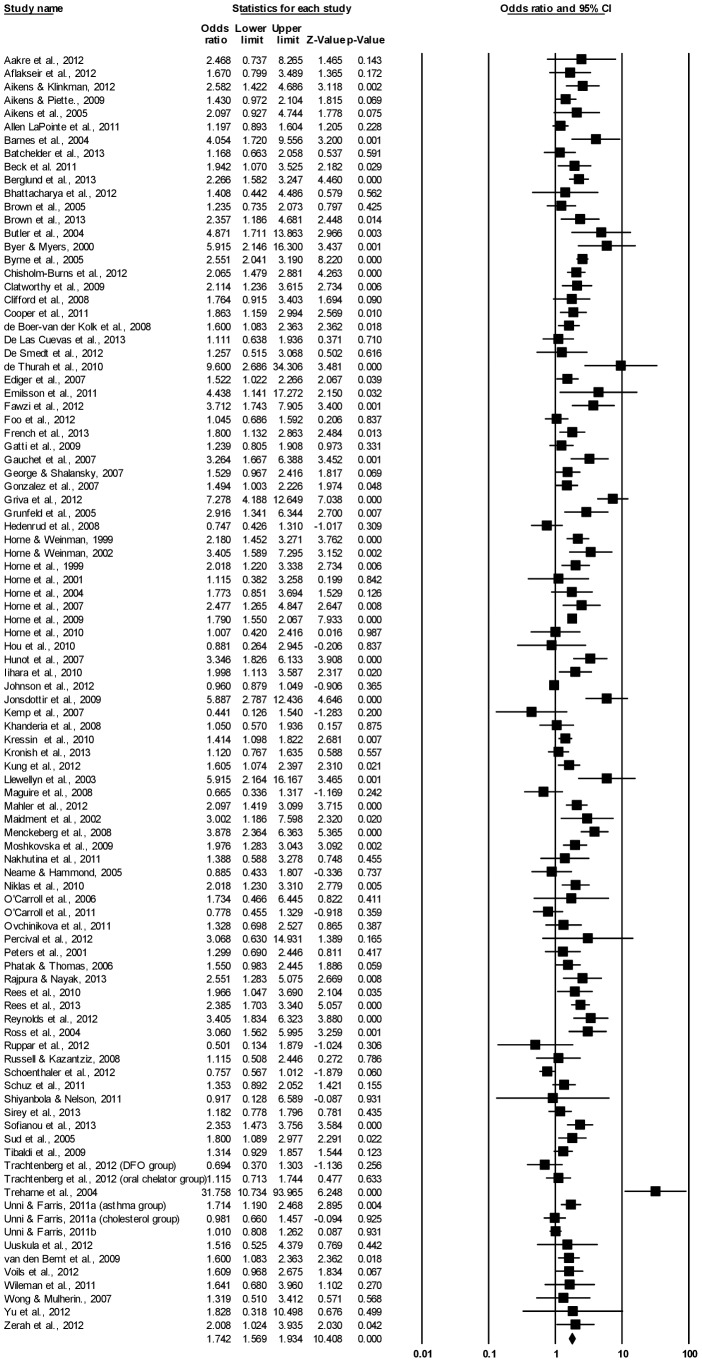
There was a significant relationship between Necessity beliefs and adherence, OR = 1.742, 95% CI [1.569, 1.934], p<0.0001. There was significant heterogeneity between the 96 comparisons from 94 studies, Q(95) = 422.662, p<0.001, which was substantial in magnitude, I 2 = 77.52%.
Figure 2 presents the individual effect-size estimates and shows that the relationship between Necessity beliefs and adherence was significant (p<0.05) for 49 (51.0%) of the included studies. Sensitivity analyses revealed that the overall result was not affected when any single finding was omitted.
Figure 2. Forest plot of effect sizes for BMQ Necessity and medication adherence.
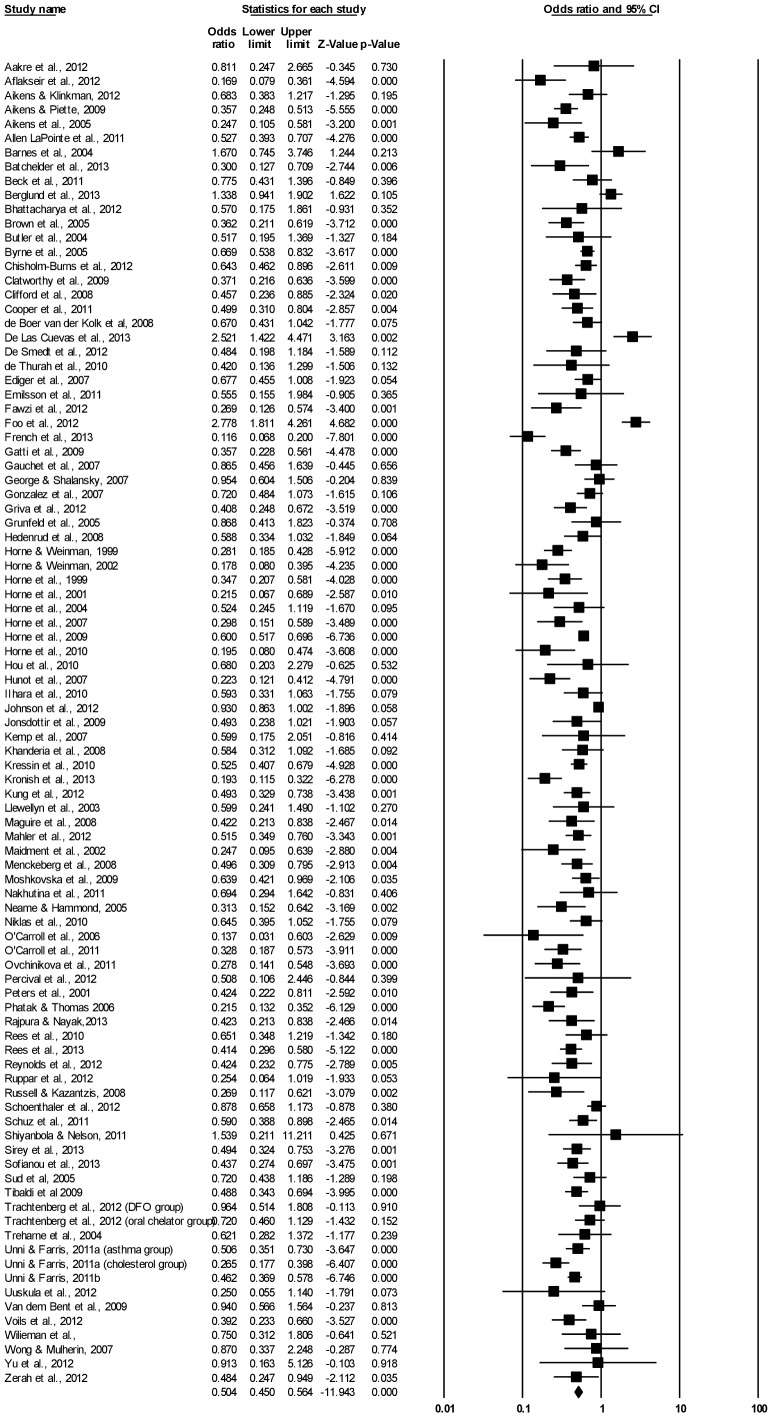
Concerns
There was a significant relationship between Concerns and adherence and fewer Concerns about adverse effects, OR = 0.502, 95% CI: [0.450, 0.560], p<0.0001. There was significant heterogeneity among the 93 comparisons from 91 studies, Q(92) = 481.84, p<0.001, suggesting that factors other than chance accounted for a moderate-substantial amount of variance, I 2 = 80.91%.
Figure 3 presents the individual effect-size estimates and shows that the relationship between concerns and adherence was significant (p<0.05) for 53 (57.0%) of the included studies. Sensitivity analyses revealed that the overall result did not change when any single finding was omitted.
Figure 3. Forest plot of effect sizes for BMQ Concerns and medication adherence.
Stratification by Long-Term Condition and Measurement
See Tables 2 and 3 for OR stratified by different long-term conditions and adherence measures. Two few studies reported data on the majority of conditions and measures to allow statistical tests for heterogeneity.
Table 2. Analyses Stratified By Long-Term Condition.
| k | OR | (95% CI) | p | |
| Necessity | ||||
| Asthma | 7 | 2.610 | 1.802–3.780 | <0.001 |
| Bipolar disorder | 2 | 1.624 | 0.739–3.567 | 0.227 |
| Blood disorders | 3 | 1.512 | 0.580–3.944 | 0.398 |
| Cancer | 2 | 2.313 | 1.190–4.496 | 0.013 |
| Depression | 8 | 1.989 | 1.382–2.862 | <0.001 |
| Diabetes | 6 | 1.502 | 0.930–2.425 | 0.096 |
| Dialysis/end stage renal disease | 3 | 1.454 | 0.771–2.742 | 0.247 |
| Epilepsy | 2 | 0.859 | 0.284–2.602 | 0.789 |
| Glaucoma | 3 | 1.697 | 0.976–2.949 | 0.061 |
| High cholesterol | 2 | 1.497 | 0.659–3.401 | 0.335 |
| HIV | 9 | 1.742 | 1.242–2.444 | 0.001 |
| Hypertension | 7 | 1.426 | 0.980–2.075 | 0.064 |
| IBD | 3 | 1.775 | 1.560–2.020 | <0.001 |
| Mixed sample | 11 | 1.504 | 1.249–1.810 | <0.001 |
| Organ transplant | 5 | 2.875 | 1.561–5.294 | 0.001 |
| Pain | 2 | 1.239 | 0.468–3.280 | 0.666 |
| Rheumatoid arthritis | 5 | 3.277 | 1.106–9.708 | 0.032 |
| Schizophrenia | 2 | 3.301 | 1.115–9.777 | 0.031 |
| Stroke/CHD/acute coronary syndrome | 9 | 1.402 | 1.022–1.924 | 0.036 |
| Concerns | ||||
| Asthma | 6 | 0.406 | 0.304–0.541 | <0.001 |
| Bipolar disorder | 2 | 0.410 | 0.250–0.672 | <0.001 |
| Blood disorders | 3 | 0.764 | 0.545–1.073 | 0.121 |
| Cancer | 2 | 0.771 | 0.411–1.445 | 0.417 |
| Depression | 8 | 0.408 | 0.215–0.772 | 0.006 |
| Diabetes | 6 | 0.450 | 0.202–1.003 | 0.051 |
| Dialysis/end stage renal disease | 3 | 0.509 | 0.211–1.232 | 0.134 |
| Epilepsy | 2 | 0.662 | 0.327–1.339 | 0.251 |
| Glaucoma | 3 | 0.909 | 0.258–3.204 | 0.882 |
| High cholesterol | 2 | 0.598 | 0.123–2.918 | 0.525 |
| HIV | 9 | 0.619 | 0.465–0.824 | 0.001 |
| Hypertension | 6 | 0.433 | 0.340–0.552 | <0.001 |
| IBD | 3 | 0.612 | 0.536–0.698 | <0.001 |
| Mixed sample | 11 | 0.423 | 0.339–0.501 | <0.001 |
| Organ transplant | 4 | 0.486 | 0.356–0.503 | <0.001 |
| Pain | 2 | 0.620 | 0.428–0.897 | 0.011 |
| Rheumatoid arthritis | 5 | 0.608 | 0.385–0.962 | 0.033 |
| Schizophrenia | 2 | 0.648 | 0.410–1.025 | 0.063 |
| Stroke/CHD/acute coronary syndrome | 9 | 0.518 | 0.382–0.704 | <0.001 |
Note. CHD = coronary heart disease.
Table 3. Analyses Stratified by Adherence Measure.
| k | OR | (95% CI) | p | |
| Necessity | ||||
| Brief Medication Questionnaire | 2 | 2.350 | 1.122–4.341 | 0.022 |
| CQ-R | 2 | 18.327 | 5.696–58.967 | <0.001 |
| Electronic monitoring | 3 | 1.625 | 0.599–4.412 | 0.340 |
| MARS | 33 | 1.838 | 1.581–2.137 | <0.001 |
| MASRI | 2 | 2.048 | 1.390–3.018 | <0.001 |
| MMAS | 20 | 1.558 | 1.305–1.862 | <0.001 |
| Pharmacy refill | 3 | 1.668 | 0.684–4.066 | 0.260 |
| Concerns | ||||
| Brief Medication Questionnaire | 2 | 0.415 | 0.131–1.321 | 0.137 |
| CQ-R | 2 | 0.546 | 0.286–1.044 | 0.067 |
| Electronic monitoring | 3 | 0.620 | 0.403–0.946 | 0.027 |
| MARS | 31 | 0.425 | 0.362–0.500 | <0.001 |
| MASRI | 2 | 0.410 | 0.251–0.669 | <0.001 |
| MMAS | 20 | 0.590 | 0.426–0.817 | 0.002 |
| Pharmacy refill | 3 | 0.785 | 0.630–0.979 | 0.031 |
Note. CQ-R = Compliance Questionnaire- Rheumatology from de Klerk, van der Heijde, Landewé, van der Tempel, & van der Linden (2003), MARS = Medication Adherence Report Scale Scale from Horne et al., (1999), MASRI = Medication Adherence Self-Report Index from Walsh et al., 2002, MMAS = Morisky Medication Adherence Scale from Morisky, Green, & Levine (1986).
Methodology/Quality Assessment
See Table 4 for sensitivity analyses.
Table 4. Analyses Stratified By Adherence Measure, Study Location, Design and Power.
| k | OR | (95% CI) | p | I2 | Heterogeneity test | |
| Necessity | ||||||
| UK study | 32 | 2.201 | 1.786–2.713 | <0.001 | 72.72%*** | Q(1) = 7.67, p<0.05 |
| Non-UK study | 64 | 1.573 | 1.405–1.761 | <0.001 | 74.79%*** | |
| Concerns | ||||||
| UK study | 31 | 0.403 | 0.335–0.485 | <0.001 | 62.75%*** | Q(1) = 7.61, p<0.05 |
| Non-UK study | 62 | 0.555 | 0.486–0.635 | <0.001 | 82.48%*** | |
| Necessity | ||||||
| Subjective adherence measure | 83 | 1.737 | 1.565–1.929 | <0.001 | 75.54%*** | Q(1) = 0.031, p = 0.86 |
| Objective adherence measure | 13 | 1.817 | 1.114–2.963 | 0.017 | 86.20%*** | |
| Concerns | ||||||
| Subjective adherence measure | 81 | 0.485 | 0.429–0.549 | <0.001 | 82.84%*** | Q(1) = 13.55, p<0.001 |
| Objective adherence measure | 12 | 0.726 | 0.609–0.866 | <0.001 | 8.93% | |
| Necessity | ||||||
| Prospective/longitudinal | 18 | 1.526 | 1.243–1.874 | <0.001 | 63.02*** | Q(1) = 1.82, p = 0.18 |
| Cross-sectional | 78 | 1.798 | 1.595–2.027 | <0.001 | 79.49%*** | |
| Concerns | ||||||
| Prospective/longitudinal | 18 | 0.449 | 0.356–0.567 | <0.001 | 70.88%*** | Q(1) = 1.14, p = 0.29 |
| Cross-sectional | 75 | 0.519 | 0.458–0.588 | <0.001 | 81.28%*** | |
| Necessity | ||||||
| Low power | 18 | 1.848 | 1.290–2.646 | 0.001 | 46.19%* | Q(1) = 0.12, p = 0.73 |
| High power | 78 | 1.730 | 1.550–1.930 | <0.001 | 80.16*** | |
| Concerns | ||||||
| Low power | 17 | 0.488 | 0.371–0.643 | <0.001 | 0.00% | Q(1) = 0.05, p = 0.82 |
| High power | 76 | 0.505 | 0.448–0.570 | <0.001 | 83.83%*** |
Note. *p<.05, ***p<.001 for Q statistic.
Study location
Most studies were conducted outside of the UK (n = 62; 66.0%). Stronger effects were apparent for both Necessity and Concerns for studies conducted in the UK relative to studies conducted outside of the UK, however the relationship between Necessity and Concerns was significant for both locations. Substantial and significant heterogeneity was present in all analyses.
Study design
The majority of studies (n = 77, 81.9%) were cross-sectional, with few studies using longitudinal or prospective designs (n = 17; 18.1%). Effect sizes were similar for longitudinal/prospective and cross-sectional designs for both Necessity and Concerns. Substanital and signficant heterogeneity was present in all analyses.
Measurement of adherence
Eighty-three studies (88.3%) employed measured adherence using self-report, while 11 (11.7%) used other methods. The association between adherence and Concerns was smaller, but still significant, when objective measures were used, and the heterogeneity around this estimate was small. The association between Necessity beliefs and adherence did not differ if objective or subjective adherence measures were used. Heterogeneity around the subjective measures estimates and the objective Necessity estimate was substantial.
Statistical power
Eighteen (19.1%) of the studies were classed as having small samples (less than 82). The size of the associations between Necessity and Concerns and adherence were similar for smaller and larger studies. Heterogeneity estimates indicated that variability around the larger samples estimates was substantial. However, the smaller sample estimates were less heterogeneous, with I2 values in the small range for Concerns and the moderate range for Necessity beliefs.
Assessment of Risk of Publication Bias
Necessity
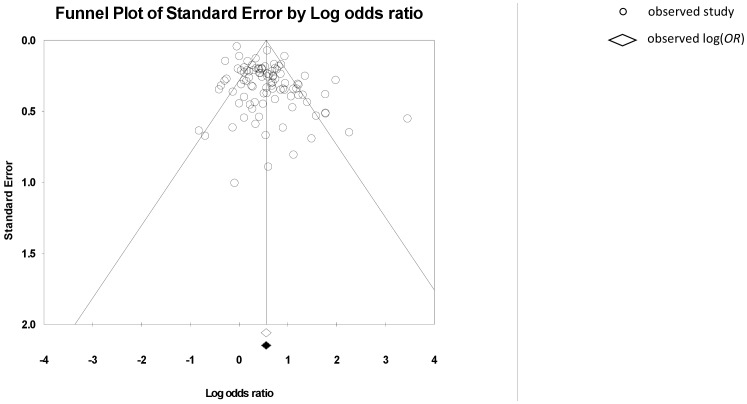
The fail-safe N (Nfs) was 96, indicating that there would need to be ≥96 unpublished findings of an equal magnitude but opposite direction, to reverse our conclusion that a significant effect exists. Inspection of the funnel plot suggested asymmetry (see Figure 4), however Duval and Tweedie’s trim and fill method did not suggest that studies should be added/removed. Egger’s t-test was significant, t(94) = 1.60, p<0.001, suggesting the presence of asymmetry.
Figure 4. Funnel plot for BMQ Necessity and medication adherence.
Concerns
The fail-safe N (Nfs) was 94, indicating that there would need to be ≥94 unpublished findings of an equal magnitude but opposite direction, to reverse our conclusion that a significant effect exists. Funnel plot inspection suggested the presence of asymmetry (see Figure 5), which was confirmed by a significant Egger’s t-test, t(91) = 1.80, p<0.001. Further, Duval and Tweedie’s trim and fill method suggested 13 studies should be added/removed to make the funnel plot symmetrical. The location of the imputed studies indicated that the asymmetry may arise from a lack of reporting of studies which find a negative relationship between concerns and adherence. However, the similarity between the adjusted OR 0.567 95% CI [0.507, 0.634], which includes the imputed trimmed and filled studies, and the observed OR 0.504 95% CI [0.450, 0.564], suggests that any bias does not have a large impact on the findings.
Figure 5. Funnel plot for BMQ Concerns and medication adherence.
Discussion
This meta-analytic review indicates that the Necessity-Concerns Framework (NCF) is a potentially useful model for understanding patients’ evaluations of prescribed medicines. The magnitude of the aggregate effect sizes indicates that, for each standard deviation increase in Necessity beliefs, the odds of adherence increases by a factor of 1.7. Conversely, for each standard deviation increase in Concerns, the odds of adherence decreases by a factor of 2.0.
Strengths and Limitations of the Study
The sensitivity and publication bias analyses conducted confirm our hypothesis that Necessity beliefs and Concerns are associated with adherence/nonadherence to medicines, across a wide range of conditions, medications, and study locations. No research synthesis can transcend the limitations of the primary studies. However, sensitivity analyses confirmed that this association is robust across methodological features; remaining when small, underpowered studies were removed, when only longitudinal/prospective designs were included, and when self-report and non self-report adherence assessments were included separately. The majority of the studies relied solely on self-reported adherence. Self-report measures have high face validity and high specificity for nonadherence, however they may be subject to self-presentation and recall bias [161]. Thus some people may be reporting higher adherence rates than they actually attain. This bias does not diminish our confidence in the finding that beliefs were related to adherence, as there is no evidence that such a bias would be associated with medication beliefs. Indeed some patients with high Concerns and low Necessity beliefs may be expected to incorrectly report high adherence in order to present themselves positively. This pattern would attenuate the relationship found between adherence and medication beliefs, making it less likely that we would find an association between beliefs and adherence. Moreover, given that this relationship remained when non-self report measures were used, we are confident that the observed relationships between beliefs and adherence are not an artifact arising from the limitations of self-report. Only published studies were included, creating a possible bias, since studies submitted for publication may be more likely to have positive results and larger effect sizes. Since for both Necessity beliefs and Concerns, the fail safe N indicated that the number of additional negative findings required to accept our null hypothesis was similar to the number of studies included in this meta-analysis, and there was little suggestion of publication bias through funnel plot analysis, our findings appear to reflect a true relationship between beliefs and adherence.
Stratifying by long-term condition and adherence measurement revealed a need for further studies using objective measures, and highlighted some conditions, for example epilepsy and functional pain syndromes where further research is needed. We do not know whether the Necessity-Concerns Framework will be of equal utility across medications administered by different routes e.g. depot injections, or if practical barriers to care may be of relatively greater importance in some groups using medications administered through different routes.
Eighteen studies assessed whether Concerns and Necessity beliefs could predict adherence using longitudinal/prospective designs. The relationship was not reduced in these studies, supporting the proposal that medication beliefs can influence later adherence as part of the self-regulation of illness [14]. We did not restrict our inclusion criteria to studies published in English. However, our search only identified one study published in any other language, despite the fact that the BMQ was translated into the native language for the study. Cultural values [162] can impact on the way in which individuals interact with the healthcare system. However, variations in treatment necessity and concerns and association between these beliefs and adherence were noted across different countries, languages and cultures. We found that studies outside the UK, where the BMQ and it’s disease-specific modifications have been predominantly developed, found reduced associations between necessity and concerns beliefs and adherence. Further work is needed to investigate potential cultural variations in medication beliefs.
Implications for Research and Practice
The development of more effective methods for addressing nonadherence is a priority for research and practice [1], [5]. Our findings suggest, that novel interventions to support informed choice and optimal adherence to appropriately prescribed medicines are likely to be more effective if they take account of patients’ beleifs about the treatment and how they judge their personal need for the prescription relative to concerns about ponteial adfverse consequences of taking it. Necessity beliefs and Concerns may trigger intentional nonadherence, for example, if patients decide not to take their medication due to concerns regarding potential or actual adverse consequences, and unintentional nonadherence, (e.g. if patients who believe a medicine is not important for their health forget to take it). Beliefs can have counter-balancing effects on adherence, such as when patients continue to take a medication they believe is essential for their health despite concerns regarding adverse effects 15. The challenge now is to develop effective interventions to address patients’ doubts about the necessity for treatment and concerns about adverse consequences in order to enhance adherence. The challenge goes beyond ‘getting patients to take more medicines’. Our findings show that many patients harbour significant, unresolved doubts and concerns about prescribed treatment suggesting a fault-line between patients’ and prescribers’ cultural perceptions of the treatment. Viewed from the perspective of biomedicine, nonadherence may seem irrational. However, from the patients’ perspective, nonadherence may be a ‘common-sense’ response to their implicit appraisal of the treatment. For some patients nonadherence might represent an informed choice. In this case the outcome of ‘adherence support’ would be to avoid prescribing an unwanted treatment, to the relief of patient and payer. However, for others, evaluations of treatment necessity and concerns may be based on misconceptions about the illness and treatment.
More detailed studies of patient representations illness and treatment show that, even when treatment evaluations are based on misconceptions they appear to draw on a ‘common-sense’ logic [12], [163], [164]. For example, the need for daily medication may seem less salient when symptoms are absent or cyclical [165]–[167]. Concerns about prescribed medication are not just related to side effects but are common, even when the medication is well tolerated. They are often related to beliefs about the negative effects of medication and include worries about long-term effects, dependence, cost of medication and dislike of having to rely on medicines [14], [167]. Concerns are related to more general beliefs about pharmaceuticals as a class of treatment which are often perceived as intrinsically harmful and over-prescribed by doctors [167], [168]. The package information leaflets, dispensed with many prescription medicines may exacerbate concerns as they list all possible side effects, leaving patients with outstanding questions and making it difficult to understand the likely risk and place them in context with potential benefits [169].
Nonadherence is often a hidden problem. Patients may be reluctant to express doubts or concerns about prescribed medication and to report nonadherence; sometimes because they fear that this will be perceived by the prescriber as a lack of faith in them. The first step to facilitating adherence is therefore to take a ‘no-blame approach’ and encourages an honest and open discussion to identify nonadherence and the reasons for nonadherence [1]. Adherence support should be tailored to the needs of the individual addressing perceptions (e.g. necessity beliefs and concerns) as well as practicalities (e.g. capacity and resources). This can be approached in a three stage process: 1) communicating a common-sense rationale for personal need that takes account of the patient’s perceptions of the illness and symptoms expectations and experiences 2) eliciting and addressing specific concerns and 3) making the treatment as convenient and as easy to use a possible. Interventions attempting to improve adherence by applying these approaches have had encouraging results [142], [170]. Nonadherence remains a fault-line in clinical practice. Consideration of patients’ perceptions of treatment necessity and concerns in prescribing and treatment review is essential to support informed choice and optimal adherence to appropriately prescribed treatment.
Supporting Information
PRISMA Checklist.
(DOC)
Acknowledgments
We would like to thank Christina Jackson for her help with the publication bias analysis, and the authors who sent additional data for their assistance.
Funding Statement
These authors have no support or funding to report.
References
- 1.National Institute for Health and Clinical Excellence (2009) Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence CG76. London: National Institute for Health and Clinical Excellence.
- 2.World Health Organisation (2003) Adherence to Long-term Therapies: Evidence for Action. Geneva: World Health Organisation.
- 3. Simpson SH, Eurich DT, Majumdar SR, Padwal RS, Tsuyuki RT, et al. (2006) A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 333: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horne R, Weinman J, Barber N, Elliott RA, Morgan M (2006) Concordance, Adherence and Compliance in Medicine Taking: A conceptual map and research priorities. London: National Institute for Health Research (NIHR) Service Delivery and Organisation (SDO) Programme. Available: http://www.sdo.lshtm.ac.uk/sdo762004.html. Accessed October 17th 2013.
- 5.Haynes RB, Yao X, Degani A, Kripalani S, Garg A, et al.. (2005) Interventions to enhance medication adherence. Cochrane Database Syst Rev: CD000011. [DOI] [PubMed]
- 6. Weinman J, Petrie KJ, Moss-Morris R, Horne R (1996) The illness perception questionnaire: A new method for assessing the cognitive representation of illness. Psychology & Health 11: 431–445. [Google Scholar]
- 7. Horne R, Weinman J (1999) Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness - processes and applications. Journal of Psychosomatic Research 47: 555–567. [DOI] [PubMed] [Google Scholar]
- 8. Benedetti F, Carlino E, Pollo A (2011) How placebos change the patient’s brain. Neuropsychopharmacology 36: 339–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Colloca L, Benedetti F (2007) Nocebo hyperalgesia: how anxiety is turned into pain. Current Opinion in Anesthesiology 20: 435–439. [DOI] [PubMed] [Google Scholar]
- 10.Horne R (2001) Compliance, adherence and concordance. In: Taylor K, Harding G, editors. Pharmacy Practice. London: Taylor and Francis. 165–184.
- 11. De Maeseneer J, Roberts RG, Demarzo M, Heath I, Sewankambo N, et al. (2012) Tackling NCDs: a different approach is needed. The Lancet 379: 1860–1861. [DOI] [PubMed] [Google Scholar]
- 12.Horne R (1997) Representations of medication and treatment: Advances in theory and measurement In: Petrie KJ, Weinman JA, editors. Perceptions of Health and Illness: Current Research and Applications. London: Harwood Academic Press. 155–188.
- 13.Horne R (2003) Treatment perceptions and self regulation. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. London: Routledge. 138–153.
- 14. Horne R, Weinman J, Hankins M (1999) The Beliefs about Medicines Questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychology and Health 14: 1–24. [Google Scholar]
- 15. Maidment R, Livingston G, Katona C (2002) Just keep taking the tablets: adherence to antidepressant treatment in older people in primary care. International Journal of Geriatric Psychiatry 17: 752–757. [DOI] [PubMed] [Google Scholar]
- 16. Byer B, Myers LB (2000) Psychological correlates of adherence to medication in asthma Psychology, Health and Medicine. 5: 389–393. [Google Scholar]
- 17. Byrne M, Walsh J, Murphy AW (2005) Secondary prevention of coronary heart disease: patient beliefs and health-related behaviour. Journal of Psychosomatic Research 58: 403–415. [DOI] [PubMed] [Google Scholar]
- 18. Clatworthy J, Bowskill R, Parham R, Rank T, Scott J, et al. (2009) Understanding medication non-adherence in bipolar disorders using a Necessity-Concerns Framework. Journal of Affective Disorders 116: 51–55. [DOI] [PubMed] [Google Scholar]
- 19. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, et al. (2000) Meta-analysis of Observational Studies in Epidemiology. JAMA: The Journal of the American Medical Association 283: 2008–2012. [DOI] [PubMed] [Google Scholar]
- 20. Gonzalez J, Penedo F, Llabre M, Duran R, Antoni M, et al. (2007) Physical symptoms, beliefs about medications, negative mood, and long-term HIV medication adherence. Annals of Behavioural Medicine 34: 46–55. [DOI] [PubMed] [Google Scholar]
- 21. de Thurah A, Norgaard M, Harder I, Stengaard-Pedersen K (2010) Compliance with methotrexate treatment in patients with rheumatoid arthritis: influence of patients’ beliefs about the medicine. A prospective cohort study. Rheumatol Int 30: 1441–1448. [DOI] [PubMed] [Google Scholar]
- 22. Llewellyn C, Miners A, Lee C, Harrington C, Weinman J (2003) The illness perceptions and treatment beliefs of individuals with severe haemophilia and their role in adherence to home treatment. Health Psychology 18: 185–2000. [Google Scholar]
- 23. French DP, Wade AN, Farmer AJ (2013) Predicting self-care behaviours of patients with type 2 diabetes: The importance of beliefs about behaviour, not just beliefs about illness. J Psychosom Res 74: 327–333. [DOI] [PubMed] [Google Scholar]
- 24. Horne R, Clatworthy J, Hankins M, ASCOT Investigators (2010) High adherence and concordance within a clinical trial of antihypertensives. Chronic Illness 6: 243–251. [DOI] [PubMed] [Google Scholar]
- 25. O’Carroll R, Whittaker J, Hamilton B, Johnston M, Sudlow C, et al. (2011) Predictors of adherence to secondary preventive medication in stroke patients. Ann Behav Med 41: 383–390. [DOI] [PubMed] [Google Scholar]
- 26. Ovchinikova L, Smith L, Bosnic-Anticevich S (2011) Inhaler technique maintenance: gaining an understanding from the patient’s perspective. J Asthma 48: 616–624. [DOI] [PubMed] [Google Scholar]
- 27. Unni EJ, Farris KB (2011) Unintentional non-adherence and belief in medicines in older adults. Patient Educ Couns 83: 265–268. [DOI] [PubMed] [Google Scholar]
- 28. Aikens JE, Nease DE Jr, Nau DP, Klinkman MS, Schwenk TL (2005) Adherence to maintenance-phase antidepressant medication as a function of patient beliefs about medication. Annals of Family Medicine 3: 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Johnson MO, Dilworth SE, Taylor JM, Darbes LA, Comfort ML, et al. (2012) Primary relationships, HIV treatment adherence, and virologic control. AIDS Behav 16: 1511–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Batchelder AW, Gonzalez JS, Berg KM (2013) Differential medication nonadherence and illness beliefs in co-morbid HIV and type 2 diabetes. J Behav Med. doi: 10.1007/s10865-012-9486-1. [DOI] [PubMed]
- 31. Allen LaPointe NM, Ou FS, Calvert SB, Melloni C, Stafford JA, et al. (2011) Association between patient beliefs and medication adherence following hospitalization for acute coronary syndrome. Am Heart J 161: 855–863. [DOI] [PubMed] [Google Scholar]
- 32. Trachtenberg FL, Mednick L, Kwiatkowski JL, Neufeld EJ, Haines D, et al. (2012) Beliefs about chelation among thalassemia patients. Health Qual Life Outcomes 10: 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Unni E, Farris KB (2011) Determinants of different types of medication non-adherence in cholesterol lowering and asthma maintenance medications: a theoretical approach. Patient Educ Couns 83: 382–390. [DOI] [PubMed] [Google Scholar]
- 34.Higgins J, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions: The Cochrane Collaboration. Available: http://handbook.cochrane.org/. Accessed 2013 Nov 10.
- 35. Orwin R (1983) A Fail-Safe N for effect size in meta-analysis. Journal of Educational Statistics 8: 157–159. [Google Scholar]
- 36. Rosenthal R (1979) The “file drawer problem” and tolerance for null results. Psychological Bulletin 85: 638–641. [Google Scholar]
- 37.Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, et al.. (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343. [DOI] [PubMed]
- 38. Magadza C, Radloff SE, Srinivas SC (2009) The effect of an educational intervention on patients’ knowledge about hypertension, beliefs about medicines, and adherence. Research in Social and Administrative Pharmacy 5: 363–375. [DOI] [PubMed] [Google Scholar]
- 39. Aburuz SM, McElnay JC, Millership JS, Andrews WJ, Smyth S (2002) Factors affecting self-care activities, postprandial plasma glucose, and HbA1c in patients with type 2 diabetes. International Journal Of Pharmacy Practice 10S: 96. [Google Scholar]
- 40.Engova D, Duggan C, MacCallum P, Bates I (2004) The role of medication adherence in warfarin anticoagulation control and its cognitive determinants. British Journal of Haematology Supplement 1S: 57.
- 41. Engova D, Duggan C, MacCallum P, Bates I (2002) Patients’ understanding and perceptions of treatment as determinants of adherence to warfarin treatment. International Journal Of Pharmacy Practice 10S: R69. [Google Scholar]
- 42. Kendrew P, Ward F, Buick D, Wright D, Horne R (2001) Satisfaction with information and its relationship with adherence in patients with chronic pain. International Journal Of Pharmacy Practice 9S: R5. [Google Scholar]
- 43. Skingle SJ (2004) A study to investigate factors that may be associated with patients’ decisions about starting disease modifying anti-rheumatic drugs. Rheumatology 43S: 153. [Google Scholar]
- 44. Stafkey DR, Erickson SR, Kline-Rogers EM, Smith DE, Cooper JV, et al. (2003) Relationship between patient beliefs about medication and self-reported medication adherence six months after discharge for acute coronary syndromes. Value in Health 6: 312. [Google Scholar]
- 45.Wade AN, Farmer AJ, French DP (2004) Association of beliefs about illness and medication with self-care activities in noninsulin treated Type 2 diabetes. Diabetic medicine Supplement 21S: 52.
- 46. Rajpura JR, Nayak R (2010) The role of illness burden and medication beliefs in medication compliance of elderly with hypertension. Value in Health 3): A168. [Google Scholar]
- 47. Batchelder A, Berg K, Carter A, Gonzalez J (2010) Differences in treatment adherence, illness perceptions, and beliefs about medications in co-morbid HIV and type 2 diabetes mellitus. Journal of the International Association of Physicians in AIDS Care 9 (4): 253. [Google Scholar]
- 48. Chisholm-Burns M, Pinsky B, Parker G, Johnson P, Buzinec P, et al. (2010) Patient reported factors influencing adherence to antirejection medications. American Journal of Transplantation 10: 204. [Google Scholar]
- 49. Daleboudt GM, Broadbent E, McQueen F, Kaptein AA (2010) Intentional and unintentional treatment non-adherence in patients with systemic lupus erythematosus. Lupus 19: 167–168. [DOI] [PubMed] [Google Scholar]
- 50. Gadkari A, McHorney C (2010) Prevalence and predictors of unintentional nonadherence among adults with chronic disease who self-identify as being adherent to prescription medications. Value in Health 3: A91. [Google Scholar]
- 51. McCann R, Jackson J, Stevenson M, Bickerstaff D, Cupples M, et al. (2010) Medication management in older people with visual impairment. International Journal of Pharmacy Practice 18: 95–96. [Google Scholar]
- 52. Moshkovska T, Mayberry J, Stone MA, Baker R, Bankart J, et al. (2010) The benefit of a tailored patient preference intervention in adherence to 5- ASA medication in ulcerative colitis: Results from a randomised controlled trial. Gastroenterology 1: S518. [DOI] [PubMed] [Google Scholar]
- 53. Weinberger MI, Mercado M, Sirey JA (2010) Medication beliefs and adherence among community-dwelling older adults. American Journal of Geriatric Psychiatry 1: S111. [Google Scholar]
- 54. Wilke T, Mueller S (2010) Why do patients not adhere to prescribed medication regimes? Results of two German surveys. Value in Health 13 (7): A380. [Google Scholar]
- 55.Wisnivesky JP, Roy A, Lurslurchachai L, Li X, Leventhal H, et al.. (2010) Complementary and alternative medication use and adherence to inhaled corticosteroid among inner-city asthmatics. American Journal of Respiratory and Critical Care Medicine Conference: American Thoracic Society International Conference, ATS 181.
- 56.Clerisme-Beaty EM, Wise RA, Bartlett SJ, Rand CS (2010) Outcome expectancy & medication adherence: “I think therefore I am”. American Journal of Respiratory and Critical Care Medicine Conference: American Thoracic Society International Conference, ATS 181.
- 57.Foster JM, Smith L, Bosnic-Anticevich SZ, Usherwood T, Sawyer SM, et al.. (2010) The beliefs and behaviours which predict objectively measured adherence to inhaled corticosteroids in asthma. American Journal of Respiratory and Critical Care Medicine Conference: American Thoracic Society International Conference, ATS 181.
- 58. Foster JM, Smith L, Bosnic-Anticevich SZ, Usherwood T, Sawyer SM, et al. (2010) Adherence with inhaled corticosteroids in asthma is predicted by beliefs, behaviours and side effects. Respirology 15: A29. [Google Scholar]
- 59. Harrold LR, Mazor KM, Peterson D, Firneno C, Yood RA (2010) Patient knowledge and beliefs concerning gout and its treatment. Arthritis and Rheumatism 62: 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sud A, Kline-Rogers EM, Eagle KA, Fang J, Armstrong DF, et al. (2005) Adherence to medications by patients after acute coronary syndromes. Annals of Pharmacotherapy 39: 1792–1797. [DOI] [PubMed] [Google Scholar]
- 61.Rajpura JR, Nayak R (2013) Role of Illness Perceptions and Medication Beliefs on Medication Compliance of Elderly Hypertensive Cohorts. J Pharm Pract. doi: 10.1177/0897190013493806. [DOI] [PubMed]
- 62.Edmondson D, Horowitz CR, Goldfinger JZ, Fei K, Kronish IM (2013) Concerns about medications mediate the association of posttraumatic stress disorder with adherence to medication in stroke survivors. Br J Health Psychol. In press. [DOI] [PMC free article] [PubMed]
- 63. Manze M, Rose AJ, Orner MB, Berlowitz DR, Kressin NR (2010) Understanding racial disparities in treatment intensification for hypertension management. J Gen Intern Med 25: 819–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Schuz B, Wurm S, Ziegelmann JP, Warner LM, Tesch-Romer C, et al. (2011) Changes in functional health, changes in medication beliefs, and medication adherence. Health Psychol 30: 31–39. [DOI] [PubMed] [Google Scholar]
- 65.Shiyanbola OOFKB, Shiyanbola OOOSse (2010) Variation in patients’ and pharmacists’ attribution of symptoms and the relationship to patients’ concern beliefs in medications. Research in Social & Administrative Pharmacy Vol6(4), Dec 2010, 334–344. [DOI] [PubMed]
- 66. Horne R, Faasse K, Cooper V, Diefenbach MA, Leventhal H, et al. (2013) The perceived sensitivity to medicines (PSM) scale: an evaluation of validity and reliability. Br J Health Psychol 18: 18–30. [DOI] [PubMed] [Google Scholar]
- 67. McHorney CA, Zhang NJ, Stump T, Zhao X (2012) Structural equation modeling of the proximal-distal continuum of adherence drivers. Patient Prefer Adherence 6: 789–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lopez-Torres J, Parraga I, Del Campo JM, Villena A (2013) Follow up of patients who start treatment with antidepressants: treatment satisfaction, treatment compliance, efficacy and safety. BMC Psychiatry 13: 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. O’Carroll R, Dennis M, Johnston M, Sudlow C (2010) Improving adherence to medication in stroke survivors (IAMSS): a randomised controlled trial: study protocol. BMC Neurol 10: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Timmers L, Boons CC, Mangnus D, Moes JE, Swart EL, et al. (2011) The use of erlotinib in daily practice: a study on adherence and patients’ experiences. BMC Cancer 11: 284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Timmers L, Swart EL, Boons CC, Mangnus D, van de Ven PM, et al. (2012) The use of capecitabine in daily practice: a study on adherence and patients’ experiences. Patient Prefer Adherence 6: 741–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Gill A, de C. Williams AC (2001) Preliminary study of chronic pain patients’ concerns about cannabinoids as analgesics. Clinical Journal of Pain 17: 245–248. [DOI] [PubMed] [Google Scholar]
- 73. Hobro N, Weinman J, Hankins M (2004) Using the self-regulatory model to cluster chronic pain patients: the first step towards identifying relevant treatments? Pain 108: 276–283. [DOI] [PubMed] [Google Scholar]
- 74. Horne R, Frost S, Hankins M, Wright S (2001) ‘In the eye of the beholder’: Pharmacy students have more positive perceptions of medicines than students of other disciplines. International Journal Of Pharmacy Practice 9: 85–89. [Google Scholar]
- 75. Horne R, Graupner L, Frost S, Weinman J, Wright SM, et al. (2004) Medicine in a multi-cultural society: The effect of cultural background on beliefs about medications. Social Science & Medicine 59: 1307–1313. [DOI] [PubMed] [Google Scholar]
- 76. Jorgensen TM, Andersson KA, Mardby A-CM (2006) Beliefs about medicines among Swedish pharmacy employees. Pharmacy World & Science 28: 233–238. [DOI] [PubMed] [Google Scholar]
- 77. Ramstrom H, Afandi S, Elofsson K, Petersson S (2006) Differences in beliefs between patients and pharmaceutical specialists regarding medications. Patient Education & Counselling 62: 244–249. [DOI] [PubMed] [Google Scholar]
- 78. Gellaitry G, Cooper V, Davis C, Fisher M, Date HL, et al. (2006) Patients’ perception of information about HAART: impact on treatment decisions. AIDS Care 17: 367–376. [DOI] [PubMed] [Google Scholar]
- 79. Kumar K, Gordon C, Toescu V, Buckley CD, Horne R, et al. (2008) Beliefs about medicines in patients with rheumatoid arthritis and systemic lupus erythematosus: a comparison between patients of South Asian and White British origin. Rheumatology 47: 690–697. [DOI] [PubMed] [Google Scholar]
- 80. Wray J, Waters S, Radley-Smith R, Sensky T (2006) Adherence in adolescents and young adults following heart or heart-lung transplantation. Pediatric Transplantation 10: 694–700. [DOI] [PubMed] [Google Scholar]
- 81. Aikens JE, Nease DE, Klinkman MS (2008) Explaining Patients’ Beliefs About the Necessity and Harmfulness of Antidepressants. The Annals of Family Medicine 6: 23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Argentero P, Torchio E, Tibaldi G, Horne R, Clatworthy J, et al. (2010) The beliefs about drug treatment. The Italian version of the BMQ (the Beliefs about Medicines Questionnaire): its validity and applicability. [Italian] Le convizioni sui trattamenti farmacologici. Validita e utilita della versione Italiana del BMQ (the Beliefs about Medicines Questionnaire). Epidemiologia e psichiatria sociale 19: 86–92. [PubMed] [Google Scholar]
- 83. Allen LaPointe NM, Ou FS, Calvert SB, Melloni C, Stafford JA, et al. (2010) Changes in beliefs about medications during long-term care for ischemic heart disease. Am Heart J 159: 561–569. [DOI] [PubMed] [Google Scholar]
- 84. Tempier R, Hepp SL, Duncan C, Rohr B, Hachey K, et al. (2010) Patient-centered care in affective, non-affective, and schizoaffective groups: Patients’ opinions and attitudes. Community Mental Health Journal 46: 452–460. [DOI] [PubMed] [Google Scholar]
- 85. Gadkari AS, McHorney CA (2012) Unintentional non-adherence to chronic prescription medications: how unintentional is it really? BMC Health Serv Res 12: 98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Burra TA, Chen E, McIntyre RS, Grace SL, Blackmore ER, et al. (2007) Predictors of Self-Reported Antidepressant Adherence. Behavioral Medicine 32: 127–134. [DOI] [PubMed] [Google Scholar]
- 87. Le TT, Bilderback A, Bender B, Wamboldt FS, Turner CF, et al. (2008) Do asthma medication beliefs mediate the relationship between minority status and adherence to therapy? J Asthma 45: 33–37. [DOI] [PubMed] [Google Scholar]
- 88. Mann D, Allegrante J, Natarajan S, Halm E, Charlson M (2007) Predictors of Adherence to Statins for Primary Prevention. Cardiovascular Drugs and Therapy 21: 311–316. [DOI] [PubMed] [Google Scholar]
- 89. McHorney CA, Schousboe JT, Cline RR, Weiss TW (2007) The impact of osteoporosis medication beliefs and side-effect experiences on non-adherence to oral bisphosphonates*. Current Medical Research and Opinion 23: 3137–3152. [DOI] [PubMed] [Google Scholar]
- 90. Perkins DO, Johnson JL, Hamer RM, Zipursky RB, Keefe RS, et al. (2006) Predictors of antipsychotic medication adherence in patients recovering from a first psychotic episode. Schizophrenia Research 83: 53–63. [DOI] [PubMed] [Google Scholar]
- 91. Schönnesson LN, Williams ML, Ross MW, Diamond PM, Keel B (2007) Three types of adherence to HIV antiretroviral therapy and their association with AIDS diagnosis, medication side-effects, beliefs about antiretroviral therapy, and beliefs about HIV disease. International Journal of STD & AIDS 18: 369–373. [DOI] [PubMed] [Google Scholar]
- 92. Talbot JT, Viall A, Direny A, de Rochars MB, Addiss D, et al. (2008) Predictors of Compliance in Mass Drug Administration for the Treatment and Prevention of Lymphatic Filariasis in Leogane, Haiti. The American Journal of Tropical Medicine and Hygiene 78: 283–288. [PubMed] [Google Scholar]
- 93. van der Wal MHL, Jaarsma T, Moser DK, Veeger NJGM, van Gilst WH, et al. (2006) Compliance in heart failure patients: the importance of knowledge and beliefs. European Heart Journal 27: 434–440. [DOI] [PubMed] [Google Scholar]
- 94. Wang X, Wu Z (2007) Factors associated with adherence to antiretroviral therapy among HIV/AIDS patients in rural China. AIDS 21: S149–S155. [DOI] [PubMed] [Google Scholar]
- 95. Wetzels G, Nelemans P, van Wijk B, Broers N, Schouten J, et al. (2006) Determinants of poor adherence in hypertensive patients: Development and validation of the “Maastricht Utrecht Adherence in Hypertension (MUAH)-questionnaire”. Patient Education and Counseling 64: 151–158. [DOI] [PubMed] [Google Scholar]
- 96. Adepu R, Ari SM (2010) Influence of structured patient education on therapeutic outcomes in diabetes and hypertensive patients. Asian Journal of Pharmaceutical and Clinical Research 3: 174–178. [Google Scholar]
- 97.Gabriel AVC, Gabriel Aguc, Violato Cvuc (2010) Knowledge of and attitudes towards depression and adherence to treatment: The Antidepressant Adherence Scale (AAS). Journal of Affective Disorders Vol126(3), Nov 2010, 388–394. [DOI] [PubMed]
- 98. Garay-Sevilla ME, Porras JS, Malacara JM (2011) Coping strategies and adherence to treatment in patients with type 2 diabetes mellitus. Rev Invest Clin 63: 155–161. [PubMed] [Google Scholar]
- 99. Garcia Vega OA, Buendia Rodriguez JA (2010) Beliefs about antihypertensive medications in primary care patients: Validation of beliefs about medicines questionnaire (BMQ) in Colombia. Value in Health 3: A177. [Google Scholar]
- 100. McCann RM, Jackson AJ, Stevenson M, Dempster M, McElnay JC, et al. (2012) Help needed in medication self-management for people with visual impairment: case-control study. Br J Gen Pract 62: e530–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. McHorney CA, Gadkari AS (2010) Individual patients hold different beliefs to prescription medications to which they persist vs nonpersist and persist vs nonfulfill. Patient Prefer Adherence 4: 187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Quintero MA, Quintero Mamjec (2010) Dimensions of treatment adherence among Colombian women living with HIV/AIDS: A social perspective. Revista Latinoamericana de Psicologia 42(2).
- 103.Anuradha S, Joshi A, Negi M, Nischal N, Rajeshwari K, et al.. (2012) Factors Influencing Adherence to ART: New Insights from a Center Providing Free ART under the National Program in Delhi, India. J Int Assoc Physicians AIDS Care (Chic). [DOI] [PubMed]
- 104. Armour CL, Lemay K, Saini B, Reddel HK, Bosnic-Anticevich SZ, et al. (2011) Using the community pharmacy to identify patients at risk of poor asthma control and factors which contribute to this poor control. J Asthma 48: 914–922. [DOI] [PubMed] [Google Scholar]
- 105. de Guzman AB, Guevara KIJ, Guiang FJB, Gutierrez ALI, Habaluyas AS, et al. (2013) Developing a Model of Medication Adherence among Filipino Elderly. Educational Gerontology 39: 298–313. [Google Scholar]
- 106. Benner JS, Nichol MB, Rovner ES, Jumadilova Z, Alvir J, et al. (2010) Patient-reported reasons for discontinuing overactive bladder medication. BJU Int 105: 1276–1282. [DOI] [PubMed] [Google Scholar]
- 107. Bermingham M, Hayden J, Dawkins I, Miwa S, Gibson D, et al. (2011) Prospective analysis of LDL-C goal achievement and self-reported medication adherence among statin users in primary care. Clin Ther 33: 1180–1189. [DOI] [PubMed] [Google Scholar]
- 108. Brandt S, Dickinson B (2013) Time and risk preferences and the use of asthma controller medication. Pediatrics 131: e1204–1210. [DOI] [PubMed] [Google Scholar]
- 109. Brask-Lindemann D, Cadarette SM, Eskildsen P, Abrahamsen B (2011) Osteoporosis pharmacotherapy following bone densitometry: importance of patient beliefs and understanding of DXA results. Osteoporos Int 22: 1493–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Broadbent E, Donkin L, Stroh JC (2011) Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care 34: 338–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Brubaker L, Fanning K, Goldberg EL, Benner JS, Trocio JN, et al. (2010) Predictors of discontinuing overactive bladder medications. BJU Int 105: 1283–1290. [DOI] [PubMed] [Google Scholar]
- 112. Cottrell WN, Denaro CP, Emmerton L (2013) Exploring beliefs about heart failure treatment in adherent and nonadherent patients: use of the repertory grid technique. Patient Prefer Adherence 7: 141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Crowley MJ, Grubber JM, Olsen MK, Bosworth HB (2013) Factors associated with non-adherence to three hypertension self-management behaviors: preliminary data for a new instrument. J Gen Intern Med 28: 99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Davis DP, Jandrisevits MD, Iles S, Weber TR, Gallo LC (2012) Demographic, socioeconomic, and psychological factors related to medication non-adherence among emergency department patients. J Emerg Med 43: 773–785. [DOI] [PubMed] [Google Scholar]
- 115. Ferreira C, Gay M, Regnier-Aeberhard F, Bricaire F (2010) Representation of illness and of treatment side effects as determinants of adherence to treatment of HIV patients. Annales Medico-Psychologiques 168: 25–33. [Google Scholar]
- 116. Foster JM, Smith L, Bosnic-Anticevich SZ, Usherwood T, Sawyer SM, et al. (2012) Identifying patient-specific beliefs and behaviours for conversations about adherence in asthma. Intern Med J 42: e136–144. [DOI] [PubMed] [Google Scholar]
- 117. Garvie PA, Flynn PM, Belzer M, Britto P, Hu C, et al. (2011) Psychological factors, beliefs about medication, and adherence of youth with human immunodeficiency virus in a multisite directly observed therapy pilot study. J Adolesc Health 48: 637–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Gerber BS, Cano AI, Caceres ML, Smith DE, Wilken LA, et al. (2010) A pharmacist and health promoter team to improve medication adherence among Latinos with diabetes. Ann Pharmacother 44: 70–79. [DOI] [PubMed] [Google Scholar]
- 119. Jarab AS, Alqudah SG, Khdour M, Shamssain M, Mukattash TL (2012) Impact of pharmaceutical care on health outcomes in patients with COPD. Int J Clin Pharm 34: 53–62. [DOI] [PubMed] [Google Scholar]
- 120. Joseph HA, Flores SA, Parsons JT, Purcell DW (2010) Beliefs about transmission risk and vulnerability, treatment adherence, and sexual risk behavior among a sample of HIV-positive men who have sex with men. AIDS Care 22: 29–39. [DOI] [PubMed] [Google Scholar]
- 121. Kalichman SC, Eaton L, Cherry C (2010) ‘There is no proof that HIV causes AIDS’: AIDS denialism beliefs among people living with HIV/AIDS. Journal of Behavioral Medicine 33: 432–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Kalichman SC, Amaral CM, White D, Swetsze C, Kalichman MO, et al. (2012) Alcohol and adherence to antiretroviral medications: interactive toxicity beliefs among people living with HIV. J Assoc Nurses AIDS Care 23: 511–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Kalichman SC, Grebler T, Amaral CM, McNerey M, White D, et al. (2013) Intentional non-adherence to medications among HIV positive alcohol drinkers: prospective study of interactive toxicity beliefs. J Gen Intern Med 28: 399–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Markotic F, Cerni Obrdalj E, Zalihic A, Pehar R, Hadziosmanovic Z, et al. (2013) Adherence to pharmacological treatment of chronic nonmalignant pain in individuals aged 65 and older. Pain Med 14: 247–256. [DOI] [PubMed] [Google Scholar]
- 125. Natarajan N, Putnam W, Van Aarsen K, Beverley Lawson K, Burge F (2013) Adherence to antihypertensive medications among family practice patients with diabetes mellitus and hypertension. Can Fam Physician 59: e93–e100. [PMC free article] [PubMed] [Google Scholar]
- 126. Ng CH, Smith DJ, King J, Ong S, Schweitzer I (2012) Medication attitudes and beliefs in patients with psychotic and affective disorders on maintenance treatment. Hum Psychopharmacol 27: 57–62. [DOI] [PubMed] [Google Scholar]
- 127. Nordmann JP, Baudouin C, Renard JP, Denis P, Regnault A, et al. (2010) Identification of noncompliant glaucoma patients using Bayesian networks and the Eye-Drop Satisfaction Questionnaire. Clin Ophthalmol 4: 1489–1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Petrie KJ, Perry K, Broadbent E, Weinman J (2012) A text message programme designed to modify patients’ illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psychol 17: 74–84. [DOI] [PubMed] [Google Scholar]
- 129.Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger PM (2012) Factors associated with injection omission/non-adherence in the Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabetes Obes Metab 9999. [DOI] [PubMed]
- 130. Piette JD, Heisler M, Harand A, Juip M (2010) Beliefs about prescription medications among patients with diabetes: variation across racial groups and influences on cost-related medication underuse. J Health Care Poor Underserved 21: 349–361. [DOI] [PubMed] [Google Scholar]
- 131. Piette JD, Beard A, Rosland AM, McHorney CA (2011) Beliefs that influence cost-related medication non-adherence among the “haves” and “have nots” with chronic diseases. Patient Prefer Adherence 5: 389–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Powers BJ, Danus S, Grubber JM, Olsen MK, Oddone EZ, et al. (2011) The effectiveness of personalized coronary heart disease and stroke risk communication. Am Heart J 161: 673–680. [DOI] [PubMed] [Google Scholar]
- 133. Saks EK, Wiebe DJ, Cory LA, Sammel MD, Arya LA (2012) Beliefs about medications as a predictor of treatment adherence in women with urinary incontinence. J Womens Health (Larchmt) 21: 440–446. [DOI] [PubMed] [Google Scholar]
- 134. Shams MEE, Barakat EAME (2010) Measuring the rate of therapeutic adherence among outpatients with T2DM in Egypt. Saudi Pharmaceutical Journal 18: 225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. van Geffen EC, Heerdink ER, Hugtenburg JG, Siero FW, Egberts AC, et al. (2010) Patients’ perceptions and illness severity at start of antidepressant treatment in general practice. Int J Pharm Pract 18: 217–225. [DOI] [PubMed] [Google Scholar]
- 136. Wilke T, Muller S, Morisky DE (2011) Toward identifying the causes and combinations of causes increasing the risks of nonadherence to medical regimens: combined results of two German self-report surveys. Value Health 14: 1092–1100. [DOI] [PubMed] [Google Scholar]
- 137. Zarani F, Besharat MA, Sadeghian S, Sarami G (2010) The effectiveness of the information-motivation-behavioral skills model in promoting adherence in CABG patients. Journal of Health Psychology 15: 828–837. [DOI] [PubMed] [Google Scholar]
- 138. Zeber JE, Miller AL, Copeland LA, McCarthy JF, Zivin K, et al. (2011) Medication adherence, ethnicity, and the influence of multiple psychosocial and financial barriers. Adm Policy Ment Health 38: 86–95. [DOI] [PubMed] [Google Scholar]
- 139. Mardby A-C, Akerlind I, Jorgensen T (2007) Beliefs about medicines and self-reported adherence among pharmacy clients. Patient Education & Counseling 69: 158–164. [DOI] [PubMed] [Google Scholar]
- 140. Webb DG, Horne R, Pinching AJ (2001) Treatment-related empowerment: preliminary evaluation of a new measure in patients with advanced HIV disease. International Journal of STD & AIDS 12: 103–107. [DOI] [PubMed] [Google Scholar]
- 141. Higgins N, Livingstone G, Katona C (2004) Concordance therapy: an intervention to help older people take antidepressants. Journal of Affective Disorders 81: 287–291. [DOI] [PubMed] [Google Scholar]
- 142. Clifford S, Barber N, Elliott R, Hartley E, Horne R (2006) Patient-centred advice is effective in improving adherence to medicines. Pharmacy World & Science 28: 165–170. [DOI] [PubMed] [Google Scholar]
- 143. Theunissen NC, de Ridder DT, Bensing JM, Rutten GE (2003) Manipulation of patient-provider interaction: discussing illness representations or action plans concerning adherence. Patient Education and Counselling 51: 247–258. [DOI] [PubMed] [Google Scholar]
- 144. Bekker HL, Gough D, Williams M (2003) Attendance choices about the Influenza Immunization Programme: evidence for targeting patients’ beliefs. Psychology, Health and Medicine 8: 279–288. [Google Scholar]
- 145. Lam F, Stevenson FA, Britten N, Stell IM (2001) Adherence to antibiotics prescribed in an accident and emergency department: the influnce of consultation factors. European Journal of Emergency Medicine 8: 181–188. [DOI] [PubMed] [Google Scholar]
- 146. Conn KM, Halterman JS, Fisher SG, Yoos HL, Chin NP, et al. (2005) Parental beliefs about medications and medication adherence among urban children with asthma. Ambulatory Pediatrics 5: 306–310. [DOI] [PubMed] [Google Scholar]
- 147. Bane C, Hughes CM, McElnay JC (2006) The impact of depressive symptoms and psychosocial factors on medication adherence in cardiovascular disease. Patient Education & Counseling 60: 187–193. [DOI] [PubMed] [Google Scholar]
- 148. Beck EM, Vögelin R, Wirtz M, Cavelti M, Kvrgic S, et al. (2012) Do patients with schizophrenia distinguish between attitudes toward antipsychotic medication and pharmacotherapy in general?: validation of the beliefs about medication questionnaire. Journal of Nervous & Mental Disease 200: 33–43. [DOI] [PubMed] [Google Scholar]
- 149. Bender BG, Apter A, Bogen DK, Dickinson P, Fisher L, et al. (2010) Test of an interactive voice response intervention to improve adherence to controller medications in adults with asthma. J Am Board Fam Med 23: 159–165. [DOI] [PubMed] [Google Scholar]
- 150. Daleboudt GM, Broadbent E, McQueen F, Kaptein AA (2011) Intentional and unintentional treatment nonadherence in patients with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 63: 342–350. [DOI] [PubMed] [Google Scholar]
- 151. Gray TA, Fenerty C, Harper R, Spencer AF, Campbell M, et al. (2012) Individualised patient care as an adjunct to standard care for promoting adherence to ocular hypotensive therapy: an exploratory randomised controlled trial. Eye (Lond) 26: 407–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Lennerling A, Forsberg A (2012) Self-reported non-adherence and beliefs about medication in a Swedish kidney transplant population. Open Nurs J 6: 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Mann DM, Ponieman D, Montori VM, Arciniega J, McGinn T (2010) The Statin Choice decision aid in primary care: a randomized trial. Patient Educ Couns 80: 138–140. [DOI] [PubMed] [Google Scholar]
- 154. Montgomery AT, Kalvemark Sporrong S, Manap N, Tully MP, Lindblad AK (2010) Receiving a pharmaceutical care service compared to receiving standard pharmacy service in Sweden-How do patients differ with regard to perceptions of medicine use and the pharmacy encounter? Research in Social and Administrative Pharmacy 6: 185–195. [DOI] [PubMed] [Google Scholar]
- 155. Moshkovska T, Stone MA, Smith RM, Bankart J, Baker R, et al. (2011) Impact of a tailored patient preference intervention in adherence to 5-aminosalicylic acid medication in ulcerative colitis: results from an exploratory randomized controlled trial. Inflamm Bowel Dis 17: 1874–1881. [DOI] [PubMed] [Google Scholar]
- 156. Roy A, Lurslurchachai L, Halm EA, Li XM, Leventhal H, et al. (2010) Use of herbal remedies and adherence to inhaled corticosteroids among inner-city asthmatic patients. Ann Allergy Asthma Immunol 104: 132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Shiyanbola OO, Farris KB, Chrischilles E (2012) Concern beliefs in medications: Changes over time and medication use factors related to a change in beliefs. Res Social Adm Pharm 9(4): 446–457. [DOI] [PubMed] [Google Scholar]
- 158. van den Bemt BJ, den Broeder AA, van den Hoogen FH, Benraad B, Hekster YA, et al. (2011) Making the rheumatologist aware of patients’ non-adherence does not improve medication adherence in patients with rheumatoid arthritis. Scand J Rheumatol 40: 192–196. [DOI] [PubMed] [Google Scholar]
- 159. Ross S, Walker A, MacLeod MJ (2004) Patient compliance in hypertension: role of illness perceptions and treatment beliefs. Journal of Human Hypertension 18: 607–613. [DOI] [PubMed] [Google Scholar]
- 160. Brown JL, Littlewood RA, Vanable PA (2013) Social-cognitive correlates of antiretroviral therapy adherence among HIV-infected individuals receiving infectious disease care in a medium-sized northeastern US city. AIDS Care 25(9): 1149–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Garfield S, Clifford S, Eliasson L, Barber N, Willson A (2011) Suitability of measures of self-reported medication adherence for routine clinical use: A systematic review. BMC Medical Research Methodology 11: 149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hofstede G (2001) Culture’s Consequences, Comparing Values, Behaviors, Institutions, and Organizations Across Nations. Thousand Oaks CA: Sage Publications.
- 163.Leventhal H, Brissette I, Leventhal E (2003 ) The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. New York: Routledge. p.42.
- 164.Kleinman A (1986) Illness meanings and illness behaviour. In: McHugh S, Vallis TM, editors. Illness behavior: A multidisciplinary model. New York: Plenum Press. 149–160.
- 165. Halm EA, Mora P, Leventhal H (2006) No Symptoms, No Asthma*The Acute Episodic Disease Belief Is Associated With Poor Self-Management Among Inner-City Adults With Persistent Asthma. CHEST Journal 129: 573–580. [DOI] [PubMed] [Google Scholar]
- 166. Horne R, Weinman J (2002) Self regulation and self management in asthma: Exploring the role of illness perceptions and treatment beliefs in explaining non-adherence to preventer medication. Psychology and Health 17: 17–32. [Google Scholar]
- 167. Horne R, Parham R, Driscoll R, Robinson A (2009) Patients’ attitudes to medicines and adherence to maintenance treatment in inflammatory bowel disease. Inflammatory Bowel Diseases 15: 837–844. [DOI] [PubMed] [Google Scholar]
- 168. Calnan M, Montaner D, Horne R (2005) How acceptable are innovative health-care technologies? A survey of public beliefs and attitudes in England and Wales. Social Science & Medicine 60: 1937–1948. [DOI] [PubMed] [Google Scholar]
- 169. Bowskill R, Clatworthy J, Parham R, Rank T, Horne R (2007) Patients’ perceptions of information received about medication prescribed for bipolar disorder: Implications for informed choice. Journal of Affective Disorders 100: 253–257. [DOI] [PubMed] [Google Scholar]
- 170. Elliott R, Barber N, Clifford S, Horne R, Hartley E (2008) The cost effectiveness of a telephone-based pharmacy advisory service to improve adherence to newly prescribed medicines. Pharmacy World & Science 30: 17–23. [DOI] [PubMed] [Google Scholar]
- 171. Aakre JM, Medoff DR, Dixon LB, Kreyenbuhl JA (2012) Beliefs about antipsychotic versus hypoglycemic medications among individuals with serious mental illness and type 2 diabetes. Patient Prefer Adherence 6: 389–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Aflakseir A (2012) Role of illness and medication perceptions on adherence to medication in a group of Iranian patients with type 2 diabetes. J Diabetes 4: 243–247. [DOI] [PubMed] [Google Scholar]
- 173. Aikens JE, Piette JD (2009) Diabetic Patients’ Medication Underuse, Illness Outcomes, and Beliefs About Antihyperglycemic and Antihypertensive Treatments. Diabetes Care 32: 19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Aikens JE, Klinkman MS (2012) Changes in patients’ beliefs about their antidepressant during the acute phase of depression treatment. Gen Hosp Psychiatry 34: 221–226. [DOI] [PubMed] [Google Scholar]
- 175. Barnes L, Moss-Morris R, Kaufusi M (2004) Illness beliefs and adherence in diabetes mellitus: a comparison between Tongan and European patients. New Zealand Medical Journal 117: 743. [PubMed] [Google Scholar]
- 176. Beck EM, Cavelti M, Kvrgic S, Kleim B, Vauth R (2011) Are we addressing the ‘right stuff’ to enhance adherence in schizophrenia? Understanding the role of insight and attitudes towards medication. Schizophr Res 132: 42–49. [DOI] [PubMed] [Google Scholar]
- 177. Berglund E, Lytsy P, Westerling R (2013) Adherence to and beliefs in lipid-lowering medical treatments: a structural equation modeling approach including the necessity-concern framework. Patient Educ Couns 91: 105–112. [DOI] [PubMed] [Google Scholar]
- 178. Bhattacharya D, Easthall C, Willoughby KA, Small M, Watson S (2012) Capecitabine non-adherence: exploration of magnitude, nature and contributing factors. J Oncol Pharm Pract 18: 333–342. [DOI] [PubMed] [Google Scholar]
- 179. Brown C, Battista DR, Bruehlman R, Sereika SS, Thase ME, et al. (2005) Beliefs about antidepressant medications in primary care patients: relationship to self-reported adherence. Medical Care 43: 1203–1207. [DOI] [PubMed] [Google Scholar]
- 180. Butler JA, Peveler RC, Roderick P, Smith PWF, Horne R, et al. (2004) Modifiable risk factors for non-adherence to immunosuppressants in renal transplant recipients: A cross sectional study. Nephrology Dialysis Transplantation 19: 3144–3149. [DOI] [PubMed] [Google Scholar]
- 181. Chisholm-Burns M, Pinsky B, Parker G, Johnson P, Arcona S, et al. (2012) Factors related to immunosuppressant medication adherence in renal transplant recipients. Clin Transplant 26: 706–713. [DOI] [PubMed] [Google Scholar]
- 182. Cooper V, Moyle GJ, Fisher M, Reilly G, Ewan J, et al. (2011) Beliefs about antiretroviral therapy, treatment adherence and quality of life in a 48-week randomised study of continuation of zidovudine/lamivudine or switch to tenofovir DF/emtricitabine, each with efavirenz. AIDS Care 23: 705–713. [DOI] [PubMed] [Google Scholar]
- 183. de Boer-van der Kolk IM, Sprangers MAG, Ende Mvd, Schreij G, Wolf Fd, et al. (2008) Lower Perceived Necessity of HAART Predicts Lower Treatment Adherence and Worse Virological Response in the ATHENA Cohort. JAIDS Journal of Acquired Immune Deficiency Syndromes 49: 460–462. [DOI] [PubMed] [Google Scholar]
- 184. De Las Cuevas C, Penate W, Sanz EJ (2013) Psychiatric outpatients’ self-reported adherence versus psychiatrists’ impressions on adherence in affective disorders. Hum Psychopharmacol 28: 142–150. [DOI] [PubMed] [Google Scholar]
- 185. De Smedt RH, Jaarsma T, Ranchor AV, van der Meer K, Groenier KH, et al. (2012) Coping with adverse drug events in patients with heart failure: Exploring the role of medication beliefs and perceptions. Psychol Health 27: 570–587. [DOI] [PubMed] [Google Scholar]
- 186. Ediger JP, Walker JR, Graff L, Lix L, Clara I, et al. (2007) Predictors of medication adherence in inflammatory bowel disease. American Journal of Gastroenterology 102: 1417–1426. [DOI] [PubMed] [Google Scholar]
- 187. Emilsson M, Berndtsson I, Lotvall J, Millqvist E, Lundgren J, et al. (2011) The influence of personality traits and beliefs about medicines on adherence to asthma treatment. Prim Care Respir J 20: 141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Fawzi W, Abdel Mohsen MY, Hashem AH, Moussa S, Coker E, et al. (2012) Beliefs about medications predict adherence to antidepressants in older adults. Int Psychogeriatr 24: 159–169. [DOI] [PubMed] [Google Scholar]
- 189. Foo RC, Lamoureux EL, Wong RC, Ho SW, Chiang PP, et al. (2012) Acceptance, attitudes, and beliefs of Singaporean Chinese toward an ocular implant for glaucoma drug delivery. Invest Ophthalmol Vis Sci 53: 8240–8245. [DOI] [PubMed] [Google Scholar]
- 190. Gauchet A, Tarquinio C, Fischer G (2007) Psychosocial predictors of medication adherence among persons living with HIV. International Journal of Behavioral Medicine 14: 141–150. [DOI] [PubMed] [Google Scholar]
- 191. Gatti ME, Jacobson KL, Gazmararian JA, Schmotzer B, Kripalani S (2009) Relationships between beliefs about medications and adherence. American Journal of Health-System Pharmacy 66: 657–664. [DOI] [PubMed] [Google Scholar]
- 192. George J, Shalansky SJ (2007) Predictors of refill non-adherence in patients with heart failure. British Journal of Clinical Pharmacology 63: 488–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Griva K, Davenport A, Harrison M, Newman SP (2012) Non-adherence to immunosuppressive medications in kidney transplantation: intent vs. forgetfulness and clinical markers of medication intake. Ann Behav Med 44: 85–93. [DOI] [PubMed] [Google Scholar]
- 194. Grunfeld EA, Hunter MS, Sikka P, Mittal S (2005) Adherence beliefs among breast cancer patients taking tamoxifen. Patient Education & Counseling 59: 97–102. [DOI] [PubMed] [Google Scholar]
- 195. Hedenrud T, Jonsson P, Linde M (2008) Beliefs about medicines and adherence among Swedish migraineurs. Annals of Pharmacotherapy 42: 39–45. [DOI] [PubMed] [Google Scholar]
- 196. Horne R, Sumner S, Jubraj B, Weinman J, Frost S (2001) Haemodialysis patients’ beliefs about treatment: Implications for adherence to medication and fluid-diet restrictions. International Journal of Pharmacy Practice 9: 169–175. [Google Scholar]
- 197. Horne R, Buick D, Fisher M, Leake H, Cooper V, et al. (2004) Doubts about necessity and concerns about adverse effects: Identifying the types of beliefs that are associated with non-adherence to HAART. International Journal of STD and AIDS 15: 38–44. [DOI] [PubMed] [Google Scholar]
- 198. Horne R, Cooper V, Gellaitry G, Date HL, Fisher M (2007) Patients’ Perceptions of Highly Active Antiretroviral Therapy in Relation to Treatment Uptake and Adherence: The Utility of the Necessity-Concerns Framework. JAIDS 45: 334–341. [DOI] [PubMed] [Google Scholar]
- 199. Hou R, Cleak V, Peveler R (2010) Do treatment and illness beliefs influence adherence to medication in patients with bipolar affective disorder? A preliminary cross-sectional study. Eur Psychiatry 25: 216–219. [DOI] [PubMed] [Google Scholar]
- 200. Hunot VM, Horne R, Leese MN, Churchill RC (2007) A Cohort Study of Adherence to Antidepressants in Primary Care: The Influence of Antidepressant Concerns and Treatment Preferences. The Primary Care Companion to The Journal of Clinical Psychiatry 9: 91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Iihara N, Suzuki K, Kurosaki Y, Morita S, Hori K (2010) Factorial invariance of a questionnaire assessing medication beliefs in Japanese non-adherent groups. Pharm World Sci 32: 432–439. [DOI] [PubMed] [Google Scholar]
- 202. Jónsdóttir H, Friis S, Horne R, Pettersen KI, Reikvam Å, et al. (2009) Beliefs about medications: measurement and relationship to adherence in patients with severe mental disorders. Acta Psychiatrica Scandinavica 119: 78–84. [DOI] [PubMed] [Google Scholar]
- 203. Kemp S, Feely M, Hay A, Wild H, Cooper C (2007) Psychological factors and use of antiepileptic drugs: pilot work using an objective measure of adherence. Psychology, Health & Medicine 12: 107–113. [DOI] [PubMed] [Google Scholar]
- 204. Khanderia U, Townsend KA, Erickson SR, Vlasnik J, Prager RL, et al. (2008) Medication adherence following coronary artery bypass graft surgery: assessment of beliefs and attitudes. Annals of Pharmacotherapy 42: 192–199. [DOI] [PubMed] [Google Scholar]
- 205. Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D (2010) Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes 3: 173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Kronish I, Diefenbach M, Edmondson D, Phillips LA, Fei K, et al. (2013) Key Barriers to Medication Adherence in Survivors of Strokes and Transient Ischemic Attacks. Journal of General Internal Medicine 28: 675–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Kung M, Koschwanez HE, Painter L, Honeyman V, Broadbent E (2012) Immunosuppressant nonadherence in heart, liver, and lung transplant patients: associations with medication beliefs and illness perceptions. Transplantation 93: 958–963. [DOI] [PubMed] [Google Scholar]
- 208. Maguire LK, Hughes CM, McElnay JC (2008) Exploring the impact of depressive symptoms and medication beliefs on medication adherence in hypertension–A primary care study. Patient Education and Counseling 73: 371–376. [DOI] [PubMed] [Google Scholar]
- 209. Mahler C, Hermann K, Horne R, Jank S, Haefeli WE, et al. (2012) Patients’ beliefs about medicines in a primary care setting in Germany. J Eval Clin Pract 18: 409–413. [DOI] [PubMed] [Google Scholar]
- 210. Menckeberg TT, Bouvy ML, Bracke M, Kaptein AA, Leufkens HG, et al. (2008) Beliefs about medicines predict refill adherence to inhaled corticosteroids. Journal of Psychosomatic Research 64: 47–54. [DOI] [PubMed] [Google Scholar]
- 211. Moshkovska T, Stone M, Baker R, Smith R, Clatworthy J, et al. (2009) An investigation of medication adherence to 5-aminosalicylic acid therapy in patients with ulcerative colitis. Gut 58: A43–A44. [DOI] [PubMed] [Google Scholar]
- 212. Nakhutina L, Gonzalez JS, Margolis SA, Spada A, Grant A (2011) Adherence to antiepileptic drugs and beliefs about medication among predominantly ethnic minority patients with epilepsy. Epilepsy Behav 22: 584–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Neame R, Hammond A (2005) Beliefs about medications: a questionnaire survey of people with rheumatoid arthritis.[see comment]. Rheumatology 44: 762–767. [DOI] [PubMed] [Google Scholar]
- 214. Nicklas LB, Dunbar M, Wild M (2010) Adherence to pharmacological treatment of non-malignant chronic pain: the role of illness perceptions and medication beliefs. Psychol Health 25: 601–615. [DOI] [PubMed] [Google Scholar]
- 215. O’Carroll RE, McGregor LM, Swanson V, Masterton G, Hayes PC (2006) Adherence to medication after liver transplantation in Scotland: a pilot study. Liver Transplantation 12: 1862–1868. [DOI] [PubMed] [Google Scholar]
- 216. Percival M, Cottrell WN, Jayasinghe R (2012) Exploring the beliefs of heart failure patients towards their heart failure medicines and self care activities. Int J Clin Pharm 34: 618–625. [DOI] [PubMed] [Google Scholar]
- 217. Peters KF, Horne R, Kong F, Francomano CA, Biesecker BB (2001) Living with Marfan syndrome II. Medication adherence and physical activity modification. Clinical Genetics 60: 283–292. [DOI] [PubMed] [Google Scholar]
- 218. Phatak HM, Thomas J 3rd (2006) Relationships between beliefs about medications and nonadherence to prescribed chronic medications. Annals of Pharmacotherapy 40: 1737–1742. [DOI] [PubMed] [Google Scholar]
- 219. Rees G, Leong O, Crowston JG, Lamoureux EL (2010) Intentional and unintentional nonadherence to ocular hypotensive treatment in patients with glaucoma. Ophthalmology 117: 903–908. [DOI] [PubMed] [Google Scholar]
- 220.Rees G, Chong XL, Cheung CY, Aung T, Friedman DS, et al.. (2013) Beliefs and Adherence to Glaucoma Treatment: A Comparison of Patients From Diverse Cultures. J Glaucoma. doi: 10.1097/IJG.0b013e3182741f1c. [DOI] [PubMed]
- 221. Reynolds K, Viswanathan HN, O’Malley CD, Muntner P, Harrison TN, et al. (2012) Psychometric properties of the Osteoporosis-specific Morisky Medication Adherence Scale in postmenopausal women with osteoporosis newly treated with bisphosphonates. Ann Pharmacother 46: 659–670. [DOI] [PubMed] [Google Scholar]
- 222. Ruppar TM, Dobbels F, De Geest S (2012) Medication beliefs and antihypertensive adherence among older adults: a pilot study. Geriatr Nurs 33: 89–95. [DOI] [PubMed] [Google Scholar]
- 223. Russell J, Kazantzis N (2008) Medication beliefs and adherence to antidepressants in primary care. The New Zealand medical journal 121: 14–20. [PubMed] [Google Scholar]
- 224. Schoenthaler AM, Schwartz BS, Wood C, Stewart WF (2012) Patient and physician factors associated with adherence to diabetes medications. Diabetes Educ 38: 397–408. [DOI] [PubMed] [Google Scholar]
- 225. Schuz B, Marx C, Wurm S, Warner LM, Ziegelmann JP, et al. (2011) Medication beliefs predict medication adherence in older adults with multiple illnesses. J Psychosom Res 70: 179–187. [DOI] [PubMed] [Google Scholar]
- 226. Shiyanbola OO, Nelson J (2011) Illness perceptions, beliefs in medicine and medication non-adherence among South Dakota minority women with diabetes: a pilot study. S D Med 64: 365–368. [PubMed] [Google Scholar]
- 227. Sirey JA, Greenfield A, Weinberger MI, Bruce ML (2013) Medication beliefs and self-reported adherence among community-dwelling older adults. Clin Ther 35: 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Sofianou A, Martynenko M, Wolf MS, Wisnivesky JP, Krauskopf K, et al. (2013) Asthma beliefs are associated with medication adherence in older asthmatics. J Gen Intern Med 28: 67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Tibaldi G, Clatworthy J, Torchio E, Argentero P, Munizza C, et al. (2009) The utility of the Necessity–Concerns Framework in explaining treatment non-adherence in four chronic illness groups in Italy. Chronic Illness 5: 129–133. [DOI] [PubMed] [Google Scholar]
- 230. Treharne GJ, Lyons AC, Kitas GD (2004) Medication adherence in rheumatoid arthritis: effects of psychosocial factors Psychology, Health and Medicine. 13: 337–349. [Google Scholar]
- 231. Uusküla A, Laisaar K-T, Raag M, Šmidt J, Semjonova S, et al. (2012) Antiretroviral therapy (ART) adherence and correlates to nonadherence among people on ART in Estonia. AIDS Care 24: 1470–1479. [DOI] [PubMed] [Google Scholar]
- 232. van den Bemt BJF, van den Hoogen FHJ, Benraad B, Hekster YA, van Riel PLCM, et al. (2009) Adherence Rates and Associations with Nonadherence in Patients with Rheumatoid Arthritis Using Disease Modifying Antirheumatic Drugs. The Journal of Rheumatology 36: 2164–2170. [DOI] [PubMed] [Google Scholar]
- 233. Voils CI, Maciejewski ML, Hoyle RH, Reeve BB, Gallagher P, et al. (2012) Initial validation of a self-report measure of the extent of and reasons for medication nonadherence. Med Care 50: 1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Wileman V, Chilcot J, Norton S, Hughes L, Wellsted D, et al. (2011) Choosing not to take phosphate binders: the role of dialysis patients’ medication beliefs. Nephron Clin Pract 119: c205–213. [DOI] [PubMed] [Google Scholar]
- 235. Wong M, Mulherin D (2007) The influence of medication beliefs and other psychosocial factors on early discontinuation of disease-modifying anti-rheumatic drugs. Musculoskeletal Care 5: 148–159. [DOI] [PubMed] [Google Scholar]
- 236. Yu ZL, Yeoh LY, Seow YY, Luo XC, Griva K (2012) Evaluation of adherence and depression among patients on peritoneal dialysis. Singapore Med J 53: 474–480. [PubMed] [Google Scholar]
- 237. Zerah L, Arena C, Morin AS, Blanchon T, Cabane J, et al. (2012) [Patients’ beliefs about long-term glucocorticoid therapy and their association to treatment adherence]. Rev Med Interne 33: 300–304. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist.
(DOC)