Abstract
This study explored intervention outcomes and mechanisms that could help explain why low-income, African American women with a history of intimate partner abuse and suicide attempt improve in response to a culturally-informed intervention, the Grady Nia Project. Specifically, the investigation examined whether or not the intervention had effects on the women and whether or not spiritual well-being and coping mediated the effects of the intervention on suicidal ideation and depressive symptoms. In this randomized controlled clinical trial, data from 89 women who completed both pre- and post-intervention assessments were analyzed. During the post-intervention follow-up, women in the active intervention group reported lower levels of suicidal ideation and depressive symptoms and higher levels of existential well-being and adaptive coping skills than those women randomized to the treatment as usual group. However, only existential well-being was found to mediate treatment effects on suicidal ideation and depressive symptoms. Religious well-being, as well as adaptive and maladaptive coping, did not serve a mediational function. These findings highlight the importance of designing and implementing culturally-sensitive and evidence-based strategies that enhance existential well-being in this population.
Keywords: African American women, Suicidal ideation, Depressive symptoms, Spiritual well-being, Coping skills, Mediation
Intimate Partner Violence, Race, and Socioeconomic Factors
African American women have a higher risk of dying from intimate partner violence (IPV) than women from other racial or ethnic backgrounds (Azziz-Baumgartner, McKeown, Melvin, Dang, & Reed, 2011). Some studies suggest that compared to women from other racial or ethnic backgrounds, African American women are at greater risk for nonfatal IPV perpetrated by their current or former husbands or partners controlling for other demographic factors (Capaldi, Knoble, Shortt, & Kim, 2012), whereas other research indicates that these between group differences disappear when social class is controlled (Rennison & Planty, 2003). African American women’s reactions to IPV may be impacted by their experiences of racism and oppression within their social contexts (Campbell et al., 2008). Such discrimination might dissuade them from seeking help and might lead them to feel they have limited options for resisting the violence. In addition, exposure to lethal and nonfatal violence perpetrated by a partner more often occurs for economically and socially disadvantaged women (Capaldi et al., 2012; Fox, Benson, DeMaris, & Van Wyk, 2002) and those living in urban environment characterized by poverty, unemployment, and alcohol outlet density (Cunradi, Mair, Ponicki, & Remer, 2011). Women from low-income backgrounds, including those in urban communities, who experience ongoing IPV have poor physical and mental health and consequently have difficulty finding and maintaining gainful employment (Yoshihama, Hammock, & Horrocks, 2006), all of which are risk factors for suicidal behavior and depression (Joe & Neidermeier, 2008; Kubrin & Wadsworth, 2009).
IPV, Suicidality, and Depressive Symptoms in Low-Income, African American Women
Worldwide, IPV is one of the most consistently reported risk factors for suicide attempts (Devries et al., 2011; Rees et al., 2011). Twenty percent of female IPV survivors threaten or attempt suicide during their lifetime (Cavanaugh, Messing, Del-Colle, O’Sullivan, & Campbell, 2011). Low-income, African American women with suicide attempt histories report physical and nonphysical IPV three times more than their nonsuicidal counterparts (Kaslow et al., 2000). The greater number of types of IPV these women report, the more suicidal ideation they endorse (Houry, Kemball, Rhodes, & Kaslow, 2006). As their number of risk factors increases for low-income, African American women with a history of IPV, their likelihood of attempting suicide increases exponentially (Thompson, Kaslow, & Kingree, 2002).
IPV is also a risk factor for depressive symptoms and disorders (Nathanson, Shorey, Tirone, & Rhatigan, 2012), including in African American women from low-income backgrounds (Bent-Goodley, 2004; Houry et al., 2006). Poor African American women experiencing IPV who attempt suicide are more depressed than those who currently experience IPV but have never attempted suicide (Houry, Kaslow, & Thompson, 2005). Experiencing IPV leads to an increase in depressive symptoms, which is associated with higher levels of suicidal ideation among low-income, African American women (Leiner, Compton, Houry, & Kaslow, 2008). African American women are more susceptible than women from other ethnic/racial background to depression (McKnight-Eily et al., 2009) and untreated depression is a risk factor for suicidal behavior in this population, as well as in other ethnic/racial groups (Spates, 2011).
Treatment for Low-Income, African American Women with IPV and Suicidal Behavior
Although a growing literature examines treatment outcome studies for women with a history of IPV, only recently has an intervention been designed to target African American women who acknowledge a recent history of both IPV exposure and suicide attempt (Davis et al., 2009). The Grady Nia Project (Nia) is a culturally competent empowerment based group intervention based upon the Theory of Triadic Influence (TTI) (Flay & Petraitis, 1994). A randomized clinical trial examining Nia versus treatment as usual (TAU, which is the control condition) revealed that women receiving Nia demonstrated more rapid reductions in depressive symptoms initially and these between-group differences persisted at follow-up and exhibited less significant suicidal ideation in response to both physical and nonphysical IPV (Kaslow et al., 2010). However, when considering the impact of treatment for low-income, African American women with a history of IPV in terms of reducing suicidal ideation and depressive symptoms, it is useful to ascertain factors that might mediate treatment outcome. A cultural lens can inform our understanding of factors that influence responses to traumatic events, such as IPV, and to treatment. One culturally relevant protective factor for African American women that may serve a mediating role is spirituality (Ellison & Hummer, 2010), a multifaceted concept that includes spiritual well-being, religious involvement, and religious coping (Arnette, Mascaro, Santana, Davis, & Kaslow, 2007; Levin, Taylor, & Chatters, 1995). Religious involvement refers to the content of religious practice. Religious coping, one kind of coping, focuses on religiosity as a skill to deal with stressful life situations. Spiritual well-being, the construct that we examined in the current study, refers to both the individual’s relationship to God (the religious aspect of the construct) and ability to derive meaning from life (the existential aspect of the construct) (Ellison, 1983). Efforts have been directed at understanding the complex relationship between spirituality and psychological variables, such as coping and well-being (Chapman & Steger, 2010; Gullatte, Brawley, Kinney, Powe, & Mooney, 2010). Spirituality is salient as a protective factor in the lives of female survivors of IPV (Short et al., 2000), including African American women from impoverished environments (Paranjape & Kaslow, 2010). Low-income, African American women with a recent history of IPV who report high levels of spiritual well-being show reduced risk for attempting suicide (Arnette et al., 2007; Kaslow et al., 2002) and those who evidence higher levels of spirituality have lower levels of depressive symptoms (Watlington & Murphy, 2006).
Coping is another variable that may mediate treatment outcome for this population. Coping behaviors affect one’s ability to psychologically adjust and endure stressful situations (Folkman, 2010). There is a growing body of literature related to the coping strategies of a women with a history of IPV (Waldrop & Resick, 2004). Coping mediates the IPV-suicidal ideation link in African American women with limited socioeconomic resources (Kaslow et al., 1998). Low-income, African American women who have attempted suicide and who have a recent history of IPV endorse lower levels of adaptive coping than their nonsuicide attempter counterparts (Kaslow et al., 2002; Reviere et al., 2007). Among African American women who experienced IPV, coping mediates the IPV-depression link (Mitchell et al., 2006).
Hypotheses
To better understand mechanisms that account for the impact of Nia on the psychological outcomes of low-income, African American women with a history of a suicide attempt and IPV, this study aimed to ascertain the psychological outcomes of Nia and to determine if spiritual well-being and/or coping mediated the link between intervention condition (Nia, TAU) and both suicidal ideation and depressive symptoms. It was hypothesized that (1) women randomly assigned to Nia would endorse lower levels of suicidal ideation and depressive symptoms at post-intervention than those in the TAU condition; (2) women randomly assigned to Nia would endorse higher levels of spiritual well-being and adaptive coping and lower levels of maladaptive coping than those in the TAU condition; and (3) spiritual well-being (religious, existential) and both adaptive and maladaptive coping would mediate the treatment condition (Nia, TAU)—psychological outcome (suicidal ideation, depressive symptom) links.
Method
Participants
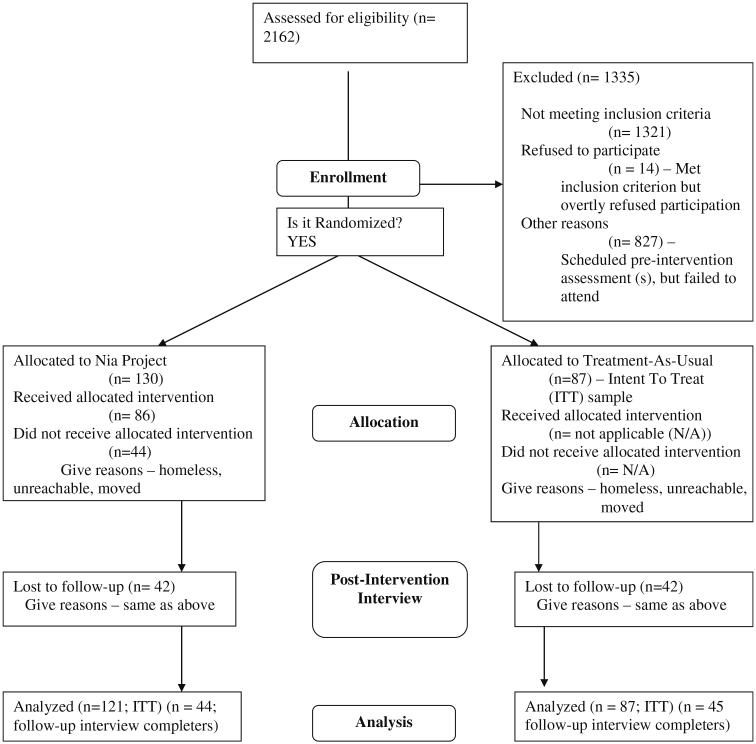
The women were from a large, Southern, urban, university-affiliated comprehensive health care system that provides health and mental health care to an indigent and minority population of patients. They were recruited from medical and psychiatric emergency rooms and outpatient clinics, both following referrals from hospital personnel and in response to completing random screening protocols. A total of 2,162 potential participants were screened for eligibility, 217 were enrolled, and 130 and 87 respectively were randomly assigned to Nia and TAU. There was an ~2:1 randomization used, with two women assigned to Nia and then one to TAU. Among the participants in Nia, 86 completed the 10-session intervention, but 42 did not complete the post-intervention assessment. Eventually, 89 of all the participants (41 %; 45 in Nia and 44 in TAU) completed the post-intervention assessment. A detailed participant flow chart is shown in Fig. 1. Data analyses were based on the 89 women who completed all measures associated with this research at both pre- and post-intervention assessments. Over 95 % of the participants had yearly income below the 2005 national poverty line (U.S. Census Bureau, 2005). All of the women self-identified as African American and during a screening process endorsed a history of both IPV and a suicide attempt. To meet criterion for IPV, the women needed to answer in the affirmative to one of five physical, sexual, and emotional IPV related questions on the Universal Violence Prevention Screening protocol, which has good construct validity, sensitivity, and specificity in this sample (Dutton, Mitchell, & Haywood, 1996; Heron, Thompson, Jackson, & Kaslow, 2003). To meet criterion for a suicide attempt, they needed to answer in the affirmative to questions related to self-harm within the prior year and endorse a significant level of suicidal intent on the 20-item Suicide Intent Scale (Beck, Schuyler, & Herman, 1974). There were few study exclusion criterion and thus individuals were only excluded from participation if they were less than 18 or older than 64, demonstrated cognitive limitations on the Mini-Mental State Exam (Folstein, Folstein, McHugh, & Fanjiang, 2001) resulting in the inability to complete the interview process, and/or endorsed a significant number of active psychotic symptoms on the 10-item Nia Psychotic Screen. The University’s Institutional Review Board and the hospital’s Research Oversight Committee approved this study prior to its inception.
Fig. 1.
The participant-flowchart
Procedure
Assessments
Participants provided data at four collection intervals; pre-intervention, post-intervention, 6- and 12-month follow-ups. The pre-intervention assessment collected baseline information about participants. Given sample size considerations, for this study, only interview data gathered at the pre- and post-intervention interviews was analyzed. At all data collection interviews, interviewers were blind to the participant’s condition. The women were compensated $20 and $30 for pre-intervention and post-intervention interviews, respectively.
Measures
With regard to collecting background data, the Demographics Questionnaire has been used by this research team in previous studies and it provides basic demographic information (e.g., relationship status, children, homelessness status, employment status, and monthly income, etc.). In addition, The Index of Spouse Abuse (ISA) was used to evaluate two forms of IPV: physical abuse and nonphysical abuse (Hudson & McIntosh, 1981). The ISA is a 30-item measurement with 5-point Likert scale from 1 (never) to 5 (very frequently) regarding the severity of abuse. A higher total weighed score on either the physical abuse or non-physical abuse indicates a higher degree of abuse. The two subscales of ISA have good internal reliability and construct validity (Campbell, Campbell, King, Parker, & Ryan, 1994; Hudson & McIntosh, 1981). In the current study, the clinical cutoffs of 10 and 25 were used for determination of physical and nonphysical abuse respectively (Hudson & McIntosh, 1981).
There were two primary outcome measures, one for suicidal ideation and the other for depressive symptoms. The 21-item Beck Scale for Suicide Ideation (BSS) (Beck, Brown, & Steer, 1997; Beck & Steer, 1991) assesses active and passive suicidal ideation, behaviors, as well as attitudes toward suicide. Items 1–5 (Part I) of the BSS serve a screening function, by which a zero rating on both Items 4 and 5 indicates no active suicidal ideation or avoidance of death in life threatening situations (in the passive suicidal desire) or these items prompts participants to skip the remaining 16 items. Items 4 and 5 are as follows: Item 4: (0) I have no desire to kill myself, (1) I have a weak desire to kill myself, (2) I have a moderate (medium) to strong desire to kill myself; Item 5: (0) I would try to save my life if I found myself in a life-threatening situation, (1) I would take a chance on life or death if I found myself in a life-threatening situation, (2) I would not take the steps necessary to avoid death if I found myself in a life-threatening situation. The total BSS scores were not included for the analyses because Part II of the scale was only completed by a subgroup of participants (62.5 %), and this might impair the study assumption of randomization. Psychometric analyses from other studies reveal that the BSS has high internal reliability with Cronbach’s alpha coefficients ranging from .87 to .97. The Cronbach’s alpha for this measure in the sample was .89 for Part I and .85 for the whole scale. There is support for use of this measure with African Americans from other samples (Carr et al., 2013; Leiner et al., 2008). The Beck Depression Inventory, 2nd Version (BDI-II) (Beck, Steer, & Brown, 1996) is a 21 item self-report scale designed to measure the severity of depressive symptoms. Items responses are on a 4-point scale ranging from 0 to 3, with increased scores representing increased severity. Two typical items are as follows: Sadness: (0) I do not feel sad, (1) I feel sad much of the time, (2) I am sad all of the time, (3) I am so sad or unhappy that I can’t stand it; and Pessimism: (0) I am not discouraged about my future, (1) I feel more discouraged about my future than I used to be, (2) I do not expect things to work out for me, (3) I feel my future is hopeless and will only get worse. Total scores range from 0 to 63, representing mild (0–13), moderate (14–19), and severe (29–63) depressive symptoms. The measure has adequate full-scale reliability (α = .94) in other samples of low-income, African American suicide attempters (Joe, Woolley, Brown, Ghahramanlou-Holloway, & Beck, 2008) and good internal consistency in the current sample (α = .90).
Two constructs, namely spiritual well-being and coping skills, were examined as outcome variables and mediators, using the Spiritual Well-Being Scale (SWBS) and the Brief COPE Scale (B-COPE), respectively. The SWBS (Ellison, 1983; Paloutzian & Ellison, 1991) measures religious and existential well-being. This 20-item scale asks people to identify to what extent they are in agreement with each statement using a 6-point Likert scale ranging from 1 (strongly agree) to 6 (strongly disagree). Only the two subscale scores, not the total score, were used for the analyses. The subscales measure two distinct constructs (Genia, 2001). A sample item that belongs to the religious well-being subscale is “I believe that God loves me and cares about me.” A sample item that belongs to the existential well-being subscale is “I believe there is some real purpose for my life.” Although concerns have been raised with regard to ceiling effects, particularly with religious populations although not with psychiatric populations, the overall scale and its two subscales have been found to be reliable (internal consistency) and valid (convergent, construct, discriminative) and to have good clinical utility, including with African Americans (Arnette et al., 2007; West, Davis, Thompson, & Kaslow, 2011). For this sample, Cronbach’s alpha was .86 for religious well-being and .84 for existential well-being. Typically, the two subscales are used in the literature, because they assess different constructs, and rarely is the total scale used. The 28-item B-COPE (Carver, 1997) assesses adaptive and maladaptive coping skills and has been used effectively with African Americans (Culver, Arena, Antoni, & Carver, 2002; Culver, Arena, Wimberly, Antoni, & Carver, 2004; Schuettler & Boals, 2011). It uses a 4 point Likert scale ranging from 1 (I haven’t been doing this at all) to 4 (I’ve been doing this a lot) and total scores range from 28 to 112. It is comprised of adaptive (Active Coping, Planning, Using Instrumental Support, Using Emotional Support, Positive Reframing, Humor, Acceptance, Religion) and maladaptive (Venting, Behavioral Disengagement, Self-Distraction, Self-Blame, Denial, and Substance Use) coping strategies (Meyer, 2001). A sample item from the adaptive coping subscale is “I’ve been getting help and advice from other people.” A sample item from the maladaptive coping subscale is “I’ve been giving up trying to deal with it.” In other samples, these two subscales have demonstrated adequate internal consistency reliability and construct validity (Meyer, 2001). In the current sample, the Cronbach’s alpha values for the adaptive and maladaptive subscales were respectively .81 and .65, indicating acceptable internal reliability for the adaptive subscale. The internal reliability for the 12 items on the maladaptive scale indicates that the items are heterogeneous and may represent diverse constructs.
Random Assignment
The women were randomized to one of two conditions following the pre-intervention assessment, Nia or TAU. Assignments were made by the Project Coordinator who utilized a random number sequence. No reports of adverse events were reported for women in either condition.
Intervention Conditions
Participants assigned to both Nia and TAU received referrals for standard psychiatric and medical services offered by the hospital, which includes weekly suicide and IPV support groups. They also had access to the comprehensive Resource Room associated with the program, as well as to the on-call person, available 24/7.
In addition, the women randomized to Nia participated in a 10-meeting, culturally-informed, empowerment-focused psychoeducational group intervention (Davis et al., 2009; Kaslow et al., 2010). Nia, the Kwanza term for purpose, incorporates Afrocentric theory to create an empowering experience for women. Meeting content is informed by the TTI model, which attends to risk and protective factors in three domains: intrapersonal, social/ situational, and environmental/contextual. As such the meetings are designed to reduce risk factors in each of these domains and enhance associated protective factors. Each 90-min Nia meeting consists of a weekly check-in that is includes monitoring of IPV and suicidality, discussion of a specific topic associated with the TTI model, and activities associated with the topic. Meetings are guided by a detailed intervention manual that is flexibly applied. To minimize the tension between flexibility and fidelity during the implementation of the manual (Aarons et al., 2012), the adaptation for the participants adheres strictly to the underling TTI model. Specifically, although participants might provide different responses to questions regarding risk and protective factors in the three domains, and the discussion might be shaped by the content of the risk and protective factors, the process maintained high fidelity to the guiding principle of the TTI model. Additional effort was made to improve the fidelity, including ensuring participants’ attendance in all the 10 meetings, abiding by the detailed instructions in the manual, and receiving feedback from group helpers who observed the implementation of the intervention (Carroll et al., 2007). Because the Nia intervention is a hybrid efficacy and effectiveness design, the research participants might bring to the group unexpected situations (e.g., intense thoughts of self-harm) that might cause the group content to deviate from the intervention manual. If a Nia woman did not fully participate in a meeting due to understandable reasons, she would have the opportunity to be re-trained in the group. Two co-therapists, one of whom self-identifies as African American, co-facilitate the program. The first three meetings set the stage for the TTI focused work, as they cover an introduction and commitment to safety (Meeting 1) and education about and safety planning related to IPV and suicide (Meetings 2 and 3). Meetings 4 and 5 target reducing intrapersonal risk factors and enhancing intra-personal protective factors, respectively. Spiritual well-being and coping are two such protective factors. Meetings 6 and 7 do the same for the social/situational domain, whereas Meetings 8 and 9 are devoted to the environmental/cultural domain. The final meeting is a termination and wrap-up session. Nia is designed to expand the extant body of evidenced-based treatments for suicidal behaviors and IPV by serving as the first culturally informed group intervention for African American women with concomitant suicidal behavior and IPV.
The women randomized to Nia began their intervention with rolling admission. Specifically, each participant started her first meeting by joining an on-going group. Depending on the schedule of the group, she could start anywhere from Meeting 1 to Meeting 10. In the beginning of each meeting, there would be a 30-min introduction and check-in when the new participant would be introduced to the group. Her intervention would be completed if she participated in all 10 meetings regardless of which meeting she began with. Given the nature of the rolling admission, the time span between pre-intervention administration of the tools and intervention onset was normally about 1 week; therefore it was unlikely that the time span significantly impacted the intervention outcomes.
Results
Statistical Analyses
In accord with standard procedure for assessing mediation (Holmbeck, 2002), multiple linear regressions were used to assess the following questions: whether or not the intervention impacted the outcome variables (i.e., suicidal ideation, depressive symptoms, religious and spiritual well-being, and adaptive and maladaptive coping skills). In addition, bootstrap estimates based on 10,000 resamples were generated for each multiple mediator models using the SPSS Macro (Hayes, 2013). The use of bootstrapping was recommended for testing of indirect effects because it does not assume normality in sampling distribution (Preacher & Hayes, 2008).
Descriptive Statistics
Chi square and independent t-tests for categorical and continuous variables respectively were conducted to compare the completer and non-completer samples. Analyses of the sample characteristics of completers and non-completers did not reveal differences in demographic information, critical relationship variables, or in pre-intervention variables, including individual income, homelessness, employment, whether or not have children, relationship status, length of current romantic relationship, whether or not the current relationship is abusive, number of abusive relationships in the past, the severity of most recent physical and emotional abuse, suicidal ideation, depressive symptoms, spiritual well-being subscale scores, and coping subscale scores. A closer examination of the subgroup of noncompleters showed no differences between the Nia and the TAU non-completers with regard to demographic factors and pre-intervention outcome variables.
This study only analyzed data from the 89 participants who completed the post-intervention assessment. The high attrition rate, despite tremendous outreach efforts on the part of the project staff in accord with recommendations for evidence-based solutions for reducing attrition (Snell-Johns, Mendez, & Smith, 2004), is not uncommon in low-income communities (Self, Oates, Pinnock-Hamilton, & Leach, 2005). In addition, there often are many barriers to service utilization within the African American community that often result in high rates of attrition (Thompson, Bazile, & Akbar, 2004). The demographic information of the participants appears in Table 1. Descriptive statistics of variables of interest for the Nia and TAU groups are shown in Table 2. For all the participants at pre-intervention assessment, the rate of physical abuse was 88.6 % and the rate of nonphysical abuse was 88.8 %. The Nia and TAU did not differ in major demographic factors or additional treatment utilization (Kaslow et al., 2010). In addition, independent t-tests showed no pre-intervention differences between these two groups regarding depressive symptoms, religious well-being, adaptive coping, or maladaptive coping. However, the TAU group reported higher levels of suicidal ideation [t (86) = 2.56, p = .01] and lower levels of existential well-being [t (87) = −2.02, p = .05]. Since preintervention scores on all variables served as covariates for all subsequent analyses, we controlled for these between group differences.
Table 1.
Demographic characteristics of the participants
| Demographic characteristics | Descriptive statistics |
|---|---|
| Relationship status (%) | |
| Single or never married | 25.8 |
| With partner, not living together | 14.6 |
| With partner, living together, not married | 20.2 |
| Married | 6.7 |
| Separated | 11.2 |
| Divorced | 15.7 |
| Widowed | 5.6 |
| Have children (%) | 86.5 |
| Homeless (%) | 47.2 |
| Unemployed (%) | 86.4 |
| Individual monthly income | |
| $0–$249 | 61.8 |
| $250–$499 | 16.9 |
| $500–$999 | 19.1 |
| >$999 | 2.2 |
Table 2.
Descriptive statistics of BDI-II, BSS, Part I, Brief COPE Subscales, and SWBS subscales
| Preintervention |
Postintervention |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nia |
TAU |
Nia |
TAU |
|||||||||
| n | M | SD | n | M | SD | N | M | SD | N | M | SD | |
| BSS Part I | 45 | 2.86 | 2.59 | 44 | 4.45 | 3.22 | 45 | 1.04 | 1.85 | 44 | 2.27 | 2.45 |
| BDI-II | 45 | 34.9 | 12.9 | 45 | 36.8 | 12.1 | 45 | 22.8 | 13.2 | 44 | 29.5 | 13.1 |
| SWBS | ||||||||||||
| Religious WB | 45 | 47.3 | 9.14 | 44 | 45.1 | 10.5 | 45 | 49.7 | 7.67 | 44 | 49.4 | 7.77 |
| Existential WB | 45 | 38.9 | 11.1 | 44 | 34.3 | 10.7 | 45 | 41.7 | 8.34 | 44 | 37.5 | 9.07 |
| Brief COPE | ||||||||||||
| Adaptive CP | 45 | 45.4 | 9.62 | 44 | 41.7 | 11.0 | 45 | 49.7 | 9.47 | 44 | 44.3 | 8.45 |
| Maladaptive CP | 45 | 29.7 | 5.98 | 44 | 32.1 | 6.12 | 45 | 27.5 | 7.61 | 44 | 29.5 | 7.74 |
BDI-II beck depression inventory-II, BSS–Part I beck scale for suicidal ideation—part I, SWBS spiritual well-being scale, WB well-being, Adaptive CP adaptive coping, Maladaptive CP maladaptive coping
Impact of Intervention on Suicidal Ideation and Depressive Symptoms
The first hypothesis pertained to the impact of intervention condition on the primary outcome variables, suicidal ideation and depressive symptoms. Results from two separate multiple regression analyses revealed that at post-intervention, the women randomly assigned to Nia were less suicidal than their counterparts in the TAU condition, even when controlling for preintervention levels of suicidal ideation: Part I of the BSS, t(85) = −1.94, p = .03, Cohen’s d = −.57. Similarly, even after controlling for pre-intervention levels of depressive symptoms, women in Nia were less depressed than women in the TAU condition at the post-intervention assessment: BDI-II, t(86) = −2.29, p = .01, Cohen’s d = −.51. Thus, the findings were consistent with the first hypothesis.
Impact of Intervention on Spiritual Well-Being and Coping Skills
The second hypothesis related to the impact of intervention condition on the spiritual well-being and coping. Results from a series of multiple regression analyses revealed that compared to the women randomly assigned to TAU, those in Nia endorsed higher scores on the post-intervention (1) existential well-being subscale of the SWBS, t (86) = 1.622, p = .05, Cohen’s d = .48, controlling for pre-intervention differences; and (2) the adaptive coping sub-scale of the B-COPE, t (86) = 2.406, p = .009, Cohen’s d = .60. However, no difference between the groups was found on religious well-being (SWBS), t (86) = −.32, p = .38, Cohen’s d = .04, or maladaptive coping (B-COPE), t (86) = −.77, p = .23, Cohen’s d = −.26. Thus, there was only partial support for the prediction that women randomly assigned to Nia would report more positive spiritual well-being and coping than the women in TAU following the intervention period.
Mediational Analyses
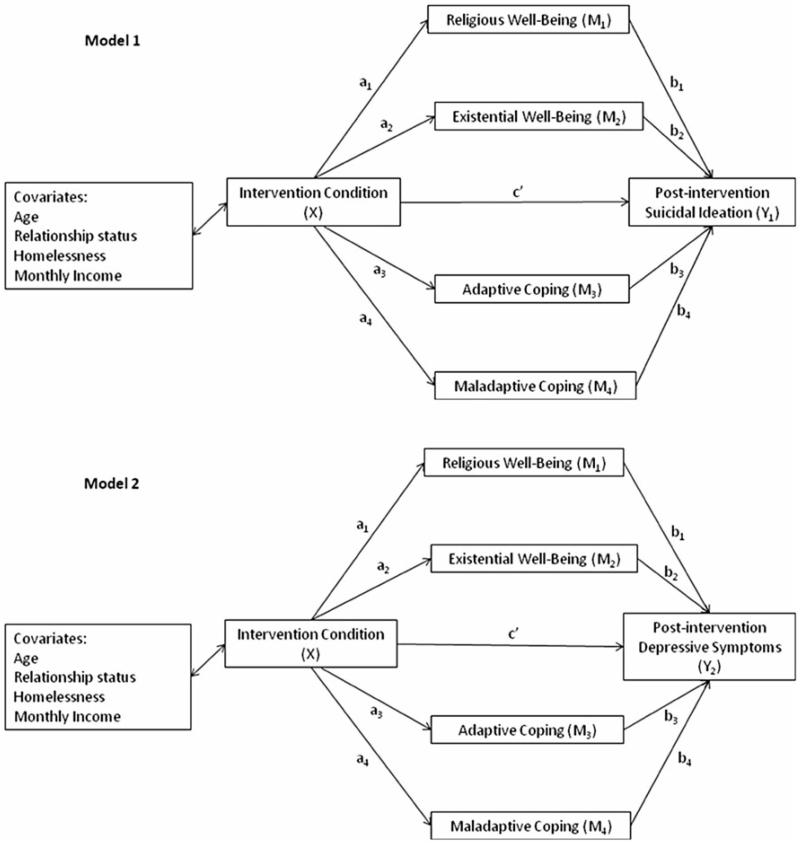
The third hypothesis related to the mediational role of spiritual well-being and coping in the intervention condition-psychological symptom outcome link. Bootstrap estimates were used to test two multiple mediator models. In Model 1 intervention condition was the independent variable; religious well-being, existential well-being, adaptive coping, and maladaptive coping were the parallel mediators; and suicidal ideation served as the outcome variable. In Model 2, intervention condition was the independent variable; religious well-being, existential well-being, adaptive coping, and maladaptive coping were parallel mediators; and depressive symptoms served as the outcome variable. These two models also are shown graphically in Fig. 2. Post-intervention variables were used for the analyses. Results based on 10,000 bootstrap samples showed significant indirect effects via existential well-being, 95 % confidence interval for both suicidal ideation (−1.15, −.026) and for depressive symptoms (−6.90, −.025). However, there were nonsignificant indirect effects for religious well-being, adaptive coping, and maladaptive coping. Detailed results of these two multiple mediator models are shown in Tables 3 and 4. Thus, bootstrap estimates support the significance of the indirect pathway through existential well-being, but not any other proposed mediators.
Fig. 2.
Path diagram showing results of two multiple mediator models controlling for covariates
Table 3.
Regression results for the multiple mediator model with intervention condition as independent variable, religious well-being, existential well-being, adaptive coping, and maladaptive coping as parallel mediators, post-intervention suicidal ideation as outcome, and age, relationship status, homelessness, and monthly income as covariates
| Regression results | Coefficient | t | P |
|---|---|---|---|
| 1. BSS Part I regressed on IC (c) | −1.17 | −2.49 | .01 |
| 2. RWB regressed on IC (a1) | .050 | −.030 | .96 |
| 3. EWB regressed on IC (a2) | 3.61 | 1.91 | .06 |
| 4. AC regressed on IC (a3) | 4.92 | 2.66 | .01 |
| 5. MAC regressed on IC (a4) | −2.20 | −1.30 | .20 |
| 6. BSS Part I regressed on RWB controlling for EWB, AC, MAC, and IC (b1) | .043 | 1.41 | .16 |
| 7. BSS Part I regressed on EWB controlling for RWB, AC, MAC, and IC (b2) | −.123 | −4.49 | <.001 |
| 8. BSS Part I regressed on AC controlling for RWB, EWB, MAC, and IC (b3) | −.039 | −1.34 | .19 |
| 9. BSS Part I regressed on MAC controlling for RWB, EWB, AC, and IC (b4) | .066 | 2.04 | .045 |
| 7. BSS Part I regressed on IC controlling for RWB, EWB, AC, and MAC (c’) | −.386 | −.872 | .39 |
| Indirect effects | Value | SE | |
|---|---|---|---|
| Total indirect effects (a1b1 + a2b2 + a3b3 + a4b4) | −.783 | .360 | |
| a1b1 | −.002 | .095 | |
| a2b2 | −.443 | .265 | |
| a3b3 | −.193 | .173 | |
| a4b4 | −.145 | .137 |
| 95 % confidence interval based on 10,000 bootstrap samples | Lower limit | Upper limit | |
|---|---|---|---|
| Total indirect effects (a1b1 + a2b2 + a3b3) | −1.58 | −.164 | |
| a1b1 | −.232 | .177 | |
| a2b2 | −1.15 | −.026 | |
| a3b3 | −.650 | .065 | |
| a4b4 | −.535 | .029 |
BSS Part I beck scale for suicidal ideation—part I, IC intervention condition, RWB religious well-being from spiritual well-being scale, EXB existential well-being from spiritual well-being scale, AC adaptive coping from brief COPE, MAC maladaptive coping from brief COPE
Table 4.
Regression results for the multiple mediator model with intervention condition as independent variable, religious well-being, existential well-being, adaptive coping, and maladaptive coping as parallel mediators, post-intervention depressive symptoms as outcome, and age, relationship status, homelessness, and monthly income as covariates
| Regression results | Coefficient | t | P |
|---|---|---|---|
| 1. BDI-II regressed on IC (c) | −7.14 | −2.49 | <.001 |
| 2. RWB regressed on IC (a1) | −.050 | −.030 | .98 |
| 3. EWB regressed on IC (a2) | 3.61 | 1.91 | .06 |
| 4. AC regressed on IC (a3) | 4.92 | 2.66 | .01 |
| 5. MAC regressed on IC (a4) | −2.20 | −1.30 | .20 |
| 6. BDI-II regressed on RWB controlling for EWB, AC, MAC, and IC (b1) | .012 | .074 | .94 |
| 7. BDI-II regressed on EWB controlling for RWB, AC, MAC, and IC (b2) | −.851 | −5.76 | <.001 |
| 8. BDI-II regressed on AC controlling for RWB, EWB, MAC, and IC (b3) | −.102 | −.643 | .52 |
| 9. BDI-II regressed on MAC controlling for RWB, EWB, AC, and IC (b4) | .436 | 2.49 | .02 |
| 7. BDI-II regressed on IC controlling for RWB, EWB, AC, and MAC (c’) | −2.61 | −1.09 | .28 |
| Indirect effects | Value | SE | |
|---|---|---|---|
| Total indirect effects (a1b1 + a2b2 + a3b3 + a4b4) | −4.53 | 2.23 | |
| a1b1 | −.001 | .277 | |
| a2b2 | −3.07 | 1.75 | |
| a3b3 | −.501 | .858 | |
| a4b4 | −.958 | .843 |
| 95 % confidence interval based on 10,000 bootstrap samples | Lower limit | Upper limit |
|
|---|---|---|---|
| Total indirect effects (a1b1 + a2b2 + a3b3 + a4b4) | −8.97 | −.148 | |
| a1b1 | −.590 | .600 | |
| a2b2 | −6.90 | −.025 | |
| a3b3 | −2.77 | .848 | |
| a4b4 | −3.26 | .200 |
BDI-II beck depression inventory-II, IC intervention condition, RWB religious well-being from spiritual well-being scale, EXB existential well-being from spiritual well-being scale, AC adaptive coping from brief COPE, MAC maladaptive coping from brief COPE
Discussion
Intervention Effects
The current study explored the relations among primary psychological outcomes, religious and existential well-being, and adaptive and maladaptive coping, in an effort to understand the intervention outcomes and mechanisms involved in intervention gains a culturally-sensitive intervention with African American women with a history of IPV and suicide attempt. The results of this study revealed that for low-income African American women with a recent history of both IPV and a suicide attempt, participation in an empowerment-based group intervention protocol was associated with more positive outcomes than involvement in standard care with regard to the reduction of both suicidal ideation and depressive symptoms, supporting the efficacy of a culturally-sensitive intervention in alleviating adverse psychological symptoms in this population.
These findings are consistent with our recent results using hierarchical linear regression models with an intent-to-treat sample (Kaslow et al., 2010), which indicated that low-income, African American women with a history of IPV and suicide attempt from the Nia group reported fewer depressive symptoms than the TAU group post-intervention controlling for pre-intervention levels. Interestingly, however, although the previous investigation did not find group difference in self-reported levels of suicidal ideation by using the total scores of the BSS (Kaslow et al., 2010), the current analyses using a sub-scale of the BSS showed significant group differences on this measure. The BSS has two subscales: (1) BSS Part I—a 5-item subscale that serves as a screening tool and participants skip the next section if they endorse 0 on both the fourth and fifth items; and (2) BSS Part II—16-item subscale that inquiries about attitudes, behaviors, and plans to commit suicide. Respondents who only answered BSS Part I could have artificially skewed the results toward the lower end, due to their missing responses on the BSS Part II.
Results showed that as predicted, women in the Nia condition reported higher levels of existential well-being and adaptive coping than women receiving standard care, but contrary to predictions, no group differences emerged in levels of religious well-being or maladaptive coping. The results on existential well-being underscore the positive effects that the Nia intervention had on one key intrapersonal protective factor, which is to help participants enhance meaning in their lives by a gaining better sense of purpose (Davis et al., 2009), which is key to quality of life among African American women (Dalmida, Holstad, Dilorio, & Laderman, 2011). Therefore, it is not surprising that women who received the intervention evidenced higher levels of existential well-being, than the TAU group post-intervention. In addition, participants in the Nia group reported more improvement in adaptive coping skills than participants in the TAU group post-intervention, further supporting its impact on another intrapersonal protective factor. These adaptive changes associated with participation in Nia included being proactive in seeking social and emotional support, facing and changing their current situations, learning to interpret events more positively and with a better sense of humor, and engaging in religious coping. In relation to the key elements of the Nia intervention based on the TTI, progress in adaptive coping implies that the psychoeducational session targeting intrapersonal protective factor was generally effective and had the intended impact on a group of minority women with a history of IPV and suicide attempt.
In comparison, no post-intervention difference was found between the two groups regarding levels of religious well-being or maladaptive coping. These findings suggest Nia may not change participants’ internal sense of religious affiliation or reduce their maladaptive coping behavior above and beyond women in the TAU group. Although religious coping is emphasized in the intervention, religious well-being is different from religious coping as the former refers to one’s internal sense of a relationship with God, whereas the latter pertains to behavioral means, such as praying and meditation. The fact that Nia does not aim to directly impact an individual’s religious beliefs does not exclude the possibility that Nia women improved more on their religious coping skills. Likewise, Nia, which is strength-oriented and empowerment-based, emphasizes enhancing adaptive coping behavior rather than reducing maladaptive behavior. Therefore, it might not have direct effect on changes of maladaptive coping behavior. In addition, the low internal consistency of the maladaptive coping skill measure, which indicates a host of heterogeneous constructs, might have contributed to the nonsignificant results.
Existential Well-Being as a Mediator
The third hypothesis was partly supported as existential well-being was found to mediate the treatment effect on suicidal ideation and depressive symptoms, whereas religious well-being and adaptive and maladaptive coping did not serve such a mediational role. The role of existential well-being and religious well-being as mediators have been explored in a few cross-sectional studies (Edmondson, Park, Blank, Fenster, & Mills, 2008; Utsey et al., 2007). Studies generally support a stronger relationship between existential well-being and psychological outcomes than religious well-being and these outcomes, including quality of life, psychological adjustment, hopelessness, and despair (Edmondson et al., 2008; Simonelli, Fowler, Maxwell, & Andersen, 2008). Existential well-being has also been found to play a mediational role between various predicting factors and outcomes, including suicidal ideation and depressive symptoms (Simonelli et al., 2008). For example, one study linked levels of existential well-being at one time point to levels of depressive symptoms and hopefulness 2 months later, supporting the role that existential well-being played in predicting psychological outcomes in longitudinal research (Mascaro & Rosen, 2005). Overall, the current study is the first investigation that evaluated the relations among existential/religious well-being, adaptive/maladaptive coping, and primary psychological outcomes in an intervention research design and ascertained the role of existential well-being in mediating the effect of an intervention on the outcomes.
Study Limitations and Future Implications
Despite the presentation of promising results, several limitations should be considered associated with the current study. Firstly, although the Nia intervention staff made an effort to keep sustained participation, the chaotic nature of many participants’ life experiences seriously impaired their adherence to the study. The high attrition rate might seriously challenge the generalizability of the results to the whole group. Second although the group differences in the majority of the outcome variables at post-intervention still held true after controlling for pre-intervention scores, the intervention effect could be explained, at least in part, by pre-existing differences between the Nia and TAU groups. Specifically, although there were no between group differences found on most of the variables of interest for this research, the Nia group endorsed higher levels of suicidal ideation and lower levels of existential well-being than the TAU group pre-intervention, and the pre-existing differences might have influenced the findings. Third, differences between the Nia and the TAU groups in symptoms, existential well-being, and coping skills might be alternatively explained by the additional attention that the intervention group received or due to the intervention group’s appreciation of additional services provided. Therefore, it is important for future investigators of the Nia intervention to add a placebo group to the TAU condition. Further, another weakness is that the study did not differentiate the specific culturally and ethnic background among African American women (e.g., indigenous vs. foreign born), therefore it is impossible to examine whether cultural backgrounds might be a moderating factor in treatment efficacy.
Despite the weaknesses of the current study, it is one of the few empirical investigations that have explored a culturally-informed intervention on an at-risk and underserved population of suicidal and depressed minority women. The findings highlight Nia as an evidence-based treatment that successfully applies the TTI (Flay & Petraitis, 1994). The current study has shown intervention effects with a variety of psychological outcomes. Importantly, existential well-being has been implied to alleviate suicidal ideation and/or depressive symptoms in our population of interest. The results of the current study offer some insights with regard to potentially fruitful intervention studies in the future. While investigations have shown that spiritual well-being is a significant factor in resilience, it may be the existential well-being component of the construct that may have the most impact on coping and thus intervention outcome. Findings highlight the need for future longitudinal studies on existential well-being and its associated psychological outcomes. Interventions that engender a sense of meaning and peace can protect against despair and ultimately suicidal behavior (Taliaferro, Rienzo, Pigg, Miller, & Dodd, 2009). In addition to continued study of the role that existential well-being plays in negative psychological outcomes, there is a need to explore the mechanisms by which existential well-being has been enhanced, to address how the improvement of existential well-being can buffer the negative impacts of adverse life experiences, and to examine if existential well-being mediates the treatment effects on positive outcomes (e.g., self-compassion and social support). It will be useful to further understand certain aspects of existential well-being that can be boosted by a culturally-sensitive intervention approach, such as goal- and future-orientations, self-purpose, and a sense of belongingness.
It is noteworthy that there is conceptual overlap between existentialism and mindfulness, both of which acknowledge common human experiences, such as impermanence, change, uncertainty, and suffering (Claessens, 2009). Therefore, other promising approaches likely to enhance the existential well-being are acceptance- and mindfulness-based in nature, such as acceptance and commitment therapy, which highlights acceptance of ever-changeable internal experiences and action toward valued directions (Hayes, Strosahl, & Wilson, 1999). When adopting acceptance- and mindfulness-based treatments for underserved populations, it is important to take a culturally— sensitive approach to enhance resilience in face of adversity, by validating intense internal experiences surrounding critical life stressors (Sobezak & West, 2013).
The theoretical framework of TTI also sheds light on the role that an interdisciplinary team of providers can play to optimize the protective factors and minimize risk factors in the environmental/contextual domain of care receivers in medical settings. The advantage of a medical setting in providing services is that health professionals can work together to offer comprehensive care, including but not limited to general and specialized medical services, spiritual counseling, individual and group therapy, crisis intervention, and community outreach programs.
Acknowledgments
This research was supported by grants from the Centers for Disease Control and Prevention National Center for Injury Prevention and Control (R49 CCR421767-01, Group interventions with suicidal African American women) and the National Institute of Mental Health (1R01MH078002-01A2, Group interviews for abused, suicidal Black women) awarded to the last author (Kaslow).
Footnotes
Conflict of interest Huaiyu Zhang, Tomina J. Schwenke, Miesha N. Rhodes, and Nadine J. Kaslow, Emory University; Kiranmayi Neelarambam, Georgia State University; Delishia M. Pittman, Lewis & Clark College. None of the authors have any conflicts of interest to report.
References
- Aarons GA, Green AE, Palinkas LA, Self-Brown S, Whitaker DJ, Lutzker JR, et al. Dynamic adaptation process to implement an evidence-based child maltreatment intervention. Implementation Science. 2012;7:32–40. doi: 10.1186/1748-5908-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnette NC, Mascaro N, Santana MC, Davis S, Kaslow NJ. Enhancing spiritual well-being among suicidal African American female survivors of intimate partner violence (IPV) Journal of Clinical Psychology. 2007;63:909–924. doi: 10.1002/jclp.20403. [DOI] [PubMed] [Google Scholar]
- Azziz-Baumgartner E, McKeown L, Melvin P, Dang Q, Reed J. Rates of femicide in women of different races, ethnicities, and places of birth: Massachusetts, 1993–2007. Journal of Interpersonal Violence. 2011;26:1077–1090. doi: 10.1177/0886260510365856. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown GK, Steer RA. Psychometric characteristics of the scale for suicide ideation with psychiatric outpatients. Behavior Research and Therapy. 1997;35:1039–1046. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- Beck AT, Schuyler D, Herman I. The development of suicide intent scales. In: Beck AT, Resnick HL, Littieri DJ, editors. Prediction of suicide. Charles Press; Bowie, MD: 1974. pp. 45–56. [Google Scholar]
- Beck AT, Steer R. Beck scale for suicide ideation manual. Harcourt Brace; San Antonio: 1991. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck depression inventory manual. 2nd Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Bent-Goodley TB. Perceptions of domestic violence: A dialogue with African American women. Health and Social Work. 2004;29:307–316. doi: 10.1093/hsw/29.4.307. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Campbell DW, Gary F, Nedd D, Price-Lea P, Sharps PW, et al. African American women’s responses to intimate partner violence: An examination of cultural context. Journal of Aggression, Maltreatment & Trauma. 2008;16:277–295. [Google Scholar]
- Campbell DW, Campbell J, King C, Parker B, Ryan J. The reliability and factor structure of the index of spouse abuse with African–American women. Violence and Victims. 1994;9(3):259–274. [PubMed] [Google Scholar]
- Capaldi DM, Knoble NB, Shortt JW, Kim HK. A systematic review of risk factors for intimate partner violence. Partner Abuse. 2012;3:1–194. doi: 10.1891/1946-6560.3.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr ER, Woods AM, Vahabzadeh A, Sutton C, Witteneaur J, Kaslow NJ. PTSD, depressive symptoms, and suicidal ideation in African American women: A mediated model. Journal of Clinical Psychology in Medical Settings. 2013;20:37–45. doi: 10.1007/s10880-012-9316-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll C, Patterson MD, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implementation Science. 2007;2:40–48. doi: 10.1186/1748-5908-2-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cavanaugh CE, Messing JT, Del-Colle M, O’Sullivan C, Campbell JC. Prevalence and correlates of suicidal behavior among adult female victims of intimate partner violence. Suicide and Life-Threatening Behavior. 2011;41:372–383. doi: 10.1111/j.1943-278X.2011.00035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman LK, Steger MF. Race and religion: Differential prediction of anxiety symptoms by religious coping in African American and European American young adults. Depression and Anxiety. 2010;27:316–322. doi: 10.1002/da.20510. [DOI] [PubMed] [Google Scholar]
- Claessens M. Mindfulness and existential therapy. Existential Analysis. 2009;20:109–119. [Google Scholar]
- Culver JL, Arena PL, Antoni MH, Carver CS. Coping and distress among women under treatment for early stage breast cancer: Comparing African Americans, Hispanics, and Non-Hispanic Whites. Psycho-Oncology. 2002;11:495–504. doi: 10.1002/pon.615. [DOI] [PubMed] [Google Scholar]
- Culver JL, Arena PL, Wimberly SR, Antoni MH, Carver CS. Coping among African-American, Hispanic, and non-Hispanic White women recently treated for early stage breast cancer. Psychology and Health. 2004;19:157–166. [Google Scholar]
- Cunradi CB, Mair C, Ponicki W, Remer L. Alcohol outlets, neighborhood characteristics, and intimate partner violence: Ecological analysis of a California city. Journal of Urban Health. 2011;88:191–200. doi: 10.1007/s11524-011-9549-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalmida SG, Holstad M, Dilorio C, Laderman G. Spiritual well-being and health-related quality of life among African-American women with HIV/AIDS. Applied Research in Quality of Life. 2011;6:139–157. doi: 10.1007/s11482-010-9122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis SP, Arnette NC, Bethea KI, Graves KN, Rhodes MN, Harp SE, et al. The Grady Nia Project: A culturally competent intervention for low-income, abused and suicidal African American women. Professional Psychology: Research and Practice. 2009;40:141–147. [Google Scholar]
- Devries K, Watts C, Yoshihama M, Kiss L, Schraiber LB, Deyessa N, et al. Violence against women is strongly associated with suicide attempts: Evidence from the WHO multi-country study on women’s health and domestic violence against women. Social Science and Medicine. 2011;73:79–86. doi: 10.1016/j.socscimed.2011.05.006. [DOI] [PubMed] [Google Scholar]
- Dutton MA, Mitchell B, Haywood Y. The emergency department as a violence prevention center. Journal of the American Medical Women’s Association. 1996;51:92–96. [PubMed] [Google Scholar]
- Edmondson D, Park CL, Blank TO, Fenster JR, Mills MA. Deconstructing spiritual well-being: Existential well-being and HRQOL in cancer survivors. Psycho-Oncology. 2008;17:161–169. doi: 10.1002/pon.1197. [DOI] [PubMed] [Google Scholar]
- Ellison CW. Spiritual well-being: Conceptualization and measurement. Journal of Psychology and Theology. 1983;11:330–340. [Google Scholar]
- Ellison CG, Hummer R, editors. Religion, family, and health: Population-based research in the United States. Rutgers University Press; New Brunswick, NJ: 2010. [Google Scholar]
- Flay BR, Petraitis J. The theory of triadic influence: A new theory of health behavior with implications for preventive interventions. Advances in Medical Sociology. 1994;4:19–44. [Google Scholar]
- Folkman S. Stress, coping, and hope. Psycho-Oncology. 2010;19:901–908. doi: 10.1002/pon.1836. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR, Fanjiang G. Mini-mental state examination. Psychological Assessment Resources; Odessa, FL: 2001. [Google Scholar]
- Fox GL, Benson ML, DeMaris AA, Van Wyk J. Economic distress and intimate violence: Testing family stress and resource theories. Journal of Marriage and Family. 2002;64:793–807. [Google Scholar]
- Genia V. Evaluation of the spiritual well-being scale in a sample of college students. The International Journal for the Psychology of Religion. 2001;11:25–33. [Google Scholar]
- Gullatte M, Brawley O, Kinney A, Powe B, Mooney K. Religiosity, spirituality, and cancer fatalism beliefs in delay in breast cancer diagnosis in African American women. Journal of Religion and Health. 2010;49:62–72. doi: 10.1007/s10943-008-9232-8. [DOI] [PubMed] [Google Scholar]
- Hayes AF. An introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford; New York: 2013. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. Guilford; New York: 1999. [Google Scholar]
- Heron SL, Thompson MP, Jackson EB, Kaslow NJ. Do responses to an intimate partner violence screen predict scores on a comprehensive measure of intimate partner violence in low-income Black women? Annals of Emergency Medicine. 2003;42:483–491. doi: 10.1067/s0196-0644(03)00718-2. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Houry D, Kaslow NJ, Thompson MP. Depressive symptoms in women experiencing intimate partner violence. Journal of Interpersonal Violence. 2005;20:1467–1477. doi: 10.1177/0886260505278529. [DOI] [PubMed] [Google Scholar]
- Houry D, Kemball R, Rhodes KV, Kaslow NJ. Intimate partner violence and mental health symptoms in African American female ED patients. American Journal of Emergency Medicine. 2006;24:444–450. doi: 10.1016/j.ajem.2005.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson WW, McIntosh SR. The assessment of spouse abuse: Two quantifiable dimensions. Journal of Marriage and the Family. 1981;43:873–888. [Google Scholar]
- Joe S, Neidermeier DM. Social work research on African Americans and suicidal behavior: A systematic 25-year review. Health and Social Work. 2008;33:249–257. doi: 10.1093/hsw/33.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joe S, Woolley ME, Brown GK, Ghahramanlou-Holloway M, Beck AT. Psychometric properties of the Beck depression inventory-II in low-income African American suicide attempters. Journal of Personality Assessment. 2008;90:521–523. doi: 10.1080/00223890802248919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaslow NJ, Leiner AS, Reviere SL, Jackson E, Bethea K, Bhaju J, et al. Suicidal, abused African American women’s response to a culturally-informed intervention. Journal of Consulting and Clinical Psychology. 2010;78:449–458. doi: 10.1037/a0019692. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Thompson M, Meadows L, Chance S, Puett R, Hollins L, et al. Risk factors for suicide attempts among African American women. Depression and Anxiety. 2000;12:13–20. doi: 10.1002/1520-6394(2000)12:1<13::AID-DA2>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Thompson M, Meadows L, Jacobs D, Chance S, Gibb B, et al. Factors that mediate and moderate the link between partner abuse and suicidal behavior in African American women. Journal of Consulting and Clinical Psychology. 1998;66:533–540. doi: 10.1037//0022-006x.66.3.533. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Thompson MP, Okun A, Price A, Young S, Bender M, et al. Risk and protective factors for suicidal behavior in abused African American women. Journal of Consulting and Clinical Psychology. 2002;70:311–319. doi: 10.1037//0022-006x.70.2.311. [DOI] [PubMed] [Google Scholar]
- Kubrin CE, Wadsworth T. Explaining suicide among Blacks and Whites: How socioeconomic factors and gun availability affect race-specific rates. Social Science Quarterly. 2009;90:1203–1227. [Google Scholar]
- Leiner AS, Compton MT, Houry D, Kaslow NJ. Intimate partner violence, psychological distress, and suicidality: A path model using data from African American women seeking care at an urban emergency department. Journal of Family Violence. 2008;23:473–481. [Google Scholar]
- Levin JS, Taylor RJ, Chatters LM. A multidimensional measure of religious involvement for African Americans. The Sociological Quarterly. 1995;36:157–173. [Google Scholar]
- Mascaro N, Rosen DH. Existential meaning’s role in the enhancement of hope and prevention of depressive symptoms. Journal of Personality. 2005;73:985–1014. doi: 10.1111/j.1467-6494.2005.00336.x. [DOI] [PubMed] [Google Scholar]
- McKnight-Eily LR, Presley-Cantrell L, Elam-Evans LD, Chapman DP, Kaslow NJ, Perry GS. Prevalence and correlates of current depressive symptomatology and lifetime diagnosis of depression in Black women. Women’s Health Issues. 2009;19:243–252. doi: 10.1016/j.whi.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Meyer B. Coping with severe mental illness: Relations of the Brief COPE with symptoms, functioning, and well-being. Journal of Psychopathology and Behavioral Assessment. 2001;23:265–277. doi: 10.1023/A:1010929402770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell MD, Hargrove GL, Collins MH, Thompson MP, Reddick TL, Kaslow NJ. Coping variables that mediate the relation between intimate partner violence and mental health outcomes among low-income, African American women. Journal of Clinical Psychology. 2006;62:1503–1520. doi: 10.1002/jclp.20305. [DOI] [PubMed] [Google Scholar]
- Nathanson AM, Shorey RC, Tirone V, Rhatigan DL. The prevalence of mental health disorders in a community sample of female victims of intimate partner violence. Partner Abuse. 2012;3:59–75. doi: 10.1891/1946-6560.3.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paloutzian RE, Ellison CW. Manual for the spiritual well-being scale. Life Advance; Navack, NY: 1991. [Google Scholar]
- Paranjape A, Kaslow NJ. Family violence exposure and health outcomes among older African American women: Do spirituality and social support play protective roles? Journal of Women’s Health. 2010;19:1899–1904. doi: 10.1089/jwh.2009.1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rees S, Silove D, Chey T, Ivancic L, Steel Z, Creamer M, et al. Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. JAMA. 2011;306:513–521. doi: 10.1001/jama.2011.1098. [DOI] [PubMed] [Google Scholar]
- Rennison CM, Planty M. Nonlethal intimate partner violence: Examining race, gender, and income patterns. Violence and Victims. 2003;18:433–443. doi: 10.1891/vivi.2003.18.4.433. [DOI] [PubMed] [Google Scholar]
- Reviere SL, Farber E, Twomey H, Okun A, Jackson E, Zanville H, et al. Intimate partner violence and suicidality in low-income African American women: A multimethod assessment of coping factors. Violence Against Women. 2007;13:1113–1129. doi: 10.1177/1077801207307798. [DOI] [PubMed] [Google Scholar]
- Schuettler D, Boals A. The path to posttraumatic growth versus posttraumatic stress disorder: Contributions of event centrality and coping. Journal of Loss and Trauma: International Perspectives on Stress & Coping. 2011;16:180–194. [Google Scholar]
- Self R, Oates P, Pinnock-Hamilton T, Leach C. The relationship between social deprivation and unilateral termination (attrition) from psychotherapy at various stages of the health care pathway. Psychology and Psychotherapy: Theory, Research, and Practice. 2005;78:11–95. doi: 10.1348/147608305X39491. [DOI] [PubMed] [Google Scholar]
- Short LM, McMahon PM, Chervin DD, Shelley GA, Lezin N, Sloop KS, et al. Survivor’s identification of protective factors and early warning signs for intimate partner violence. Violence Against Women. 2000;6:272–285. [Google Scholar]
- Simonelli L, Fowler J, Maxwell G, Andersen B. Physical sequelae and depressive symptoms in gynecologic cancer survivors: Meaning in life as a mediator. Annals of Behavioral Medicine. 2008;35:275–284. doi: 10.1007/s12160-008-9029-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snell-Johns J, Mendez J, Smith B. Evidence-based solutions for overcoming access barriers, decreasing attrition, and promoting change with underserved families. Journal of Family Psychology. 2004;18:19–35. doi: 10.1037/0893-3200.18.1.19. [DOI] [PubMed] [Google Scholar]
- Sobezak LR, West LM. Clinical considerations in using mindfulness- and acceptance-based approaches with diverse populations: Addressing challenges in service delivery in diverse community settings. Cognitive and Behavioral Practice. 2013;20:13–22. [Google Scholar]
- Spates K. African-American women and suicide: A review and critique of the literature. Sociology Compass. 2011;5:336–350. [Google Scholar]
- Taliaferro LA, Rienzo BA, Pigg RM, Jr, Miller MB, Dodd VJ. Spiritual well-being and suicidal ideation among college students. Journal of American College Health. 2009;58:83–90. doi: 10.3200/JACH.58.1.83-90. [DOI] [PubMed] [Google Scholar]
- Thompson VLS, Bazile A, Akbar M. African Americans’ perceptions of psychotherapy and psychotherapists. Professional Psychology: Research and Practice. 2004;35:19–26. [Google Scholar]
- Thompson MP, Kaslow NJ, Kingree JB. Risk factors for suicide attempts among African American women experiencing recent intimate partner violence. Violence and Victims. 2002;17:283–295. doi: 10.1891/vivi.17.3.283.33658. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2005). Poverty thresholds 2005.
- Utsey SO, Bolden MA, Williams O, III., Lee A, Lanier Y, Newsome C. Spiritual well-being as a mediator of the relation between culture-specific coping and quality of life in a community sample of African Americans. Journal of Cross-Cultural Psychology. 2007;38:123–136. [Google Scholar]
- Waldrop AE, Resick PA. Coping among adult female victims of domestic violence. Journal of Family Violence. 2004;19:291–302. [Google Scholar]
- Watlington CG, Murphy CM. The roles of religion and spirituality among African American survivors of domestic violence. Journal of Clinical Psychology. 2006;62:837–856. doi: 10.1002/jclp.20268. [DOI] [PubMed] [Google Scholar]
- West LM, Davis TA, Thompson MP, Kaslow NJ. “Let me count the ways:” Fostering reasons for living among low-income, suicidal, African American women. Suicide and Life-Threatening Behavior. 2011;41:491–500. doi: 10.1111/j.1943-278X.2011.00045.x. [DOI] [PubMed] [Google Scholar]
- Yoshihama M, Hammock AC, Horrocks J. Intimate partner violence, welfare receipt, and health status of low-income African American women: A lifecourse analysis. American Journal of Community Psychology. 2006;37:95–109. doi: 10.1007/s10464-005-9009-0. [DOI] [PubMed] [Google Scholar]