Abstract
Although research has shown positive associations among post-traumatic stress disorder (PTSD), depressive symptoms, and suicidal ideation, the nature of these relations is unclear, especially in African American women. This study examined the associations among these comorbid psychological difficulties in a sample of 136 low-income, African American women. Specifically, the goal of this investigation was to ascertain if overall depressive symptoms, as well as both the cognitive-affective and somatic components of depression, mediated the PTSD-suicidal ideation link. Results from bootstrapping analyses revealed that overall depressive symptoms and the cognitive-affective components of depression, but not the somatic components, mediated the PTSD-suicidal ideation link.
Keywords: African American, PTSD, Depression, Suicidal ideation and attempts
Post-traumatic stress disorder (PTSD) alone is a significant, functionally impairing illness with a high disruption in quality of life and morbidity as a common factor (Magruder et al., 2004; Stein, McQuaid, Pedrelli, Lenox, & McCahill,2000). It emerges after a traumatic experience. Research has revealed higher rates of exposure to trauma in African Americans than European Americans (Breslau et al., 1998) and has shown general high rates of traumatic experiences in African Americans who reside in urban, economically disadvantaged communities (Alim, Charney, & Mellman,2006; Breslau, Davis, Andreski, & Peterson, 1998; Davis, Ressler, Schwartz, Stephens, & Bradley, 2008; Schwartz, Bradley, Ressler, Sexton, & Sherry, 2004). Although exposure to a traumatic experience is required for the development of PTSD, trauma alone does not insure a PTSD diagnosis. PTSD affects about 9 % of the general population (Breslau et al., 1991), but rates among African Americans are more elevated and reports are as high as 33–43 % (Alim et al., 2006; Schwartz et al., 2004; Zoellner, Feeny, Fitzgibbons, & Foa, 1999). Furthermore, among lower socioeconomic African Americans, research has indicated a higher incidence of PTSD in women than among men (Alim et al., 2006; Bassuk, Buckner, Perloff, & Bassuk, 1998).
PTSD is a psychological risk factor for suicidal ideation, attempts, and completions (Bruce, 2010; Jakupcak et al.,2009; Oquendo et al., 2005). This finding has been found among African American women, as well, with regard to suicidal ideation and attempts (Kaslow et al., 2000, 2002; Leiner, Compton, Houry, & Kaslow, 2008). Given that African American women experience significant rates of trauma exposure, specifically assaultive trauma (Breslau et al., 1998), which has a high association with PTSD, they may be particularly prone to endorsing suicidal ideation.
Suicide completion rates among African Americans historically have been lower than those reported for European Americans (Poussaint & Alexander, 2000), despite some studies indicating the lack of such between group differences (Nisbet, 1996). There is a recent consensus that the gap is narrowing and more evidence points to the growing rate of suicides and/or more correctly identified deaths due to suicide in the African American community (Joe & Kaplan, 2001; Willis, Coombs, Drentea, & Cockerham, 2003). African American men kill themselves more often than do African American women (Gibbons, Hur, Bhamik, & Mann, 2005), however, African American women may kill themselves at a greater rate than is believed due to the misclassification of suicide as accidental deaths (Phillips & Ruth, 1993). Suicide attempts are risk factors for suicide completions (Borges, Angst, Nock, Ruscio, & Kessler, 2008) and women make three times as many suicide attempts as men (Moscicki, 2001). Furthermore, women experience higher rates of suicidal ideation than men (Cauffman, 2004), a finding that holds true for African American women (Joe & Kaplan, 2001) who also attempt suicide and experience suicidal ideation at a level comparable to women from other ethnic/racial backgrounds (Garlow et al., 2008; Nisbet, 1996).
In addition to being associated with suicidal behavior, PTSD often co-occurs with depression (Oquendo et al.,2005), exacerbating the symptoms and increasing the acuity of the disorders (Hankin, Spiro, Miller, & Kazis, 1999). In turn, depression has a strong positive association with suicidal ideation (Shahar, Bareket, Rudd, & Joiner, 2006). Suicidal individuals have higher rates of depression and depressive symptoms than their nonsuicidal counterparts (Garlow et al., 2008) and as depression increases suicide rates increase. Depression is shown at a 2:1 female-to-male ratio (Nolen-Hoeksema, 2001). Additionally, studies indicate that 10.4 % of African Americans experience major depression at some point in their life (Neighbors et al., 2007) and this rate is even higher among African American women with reported rates as high as 13.8 % (Cutrona et al., 2005). African American women from lower socioeconomic, disadvantaged communities are at an even greater risk for depression than their higher income counterparts and therefore potentially are at elevated risk for suicidal ideation (Cutrona et al., 2005).
Depressive symptoms can be categorized into cognitive-affective and somatic components (American Psychiatric Association, 2000), each potentially having a different presentation and treatment implications. The cognitive-affective components include feelings of sadness, emptiness, and worthlessness, inappropriate guilt, anhedonia, and recurrent thoughts of death. These typically are treated with psychotherapy, utilizing a range of different approaches such as cognitive-behavioral, nondirective supportive, behavioral activation, psychodynamic, problem-solving, interpersonal, and building social skills (Cuijpers et al., 2008). The focus of these therapeutic approaches is to decrease negative feelings, increase ability to change destructive thought patterns, and enhance the capacity to develop and utilize positive coping methods. The somatic components of depression include problems with sleep (insomnia, hypersomnia) and appetite (decreased or increased), psychomotor agitation or retardation, fatigue or loss of energy, and a diminished ability to concentrate or indecisiveness. These somatic symptoms typically are treated pharmacologically, with selective serotonin reuptake inhibitors and other second generation antidepressants. Somatic symptoms also can be addressed with psychosocial interventions, such as the behavioral activation associated with activity scheduling and exercise programs that utilize the bodies’ ability to create natural endorphins to increase energy and positive feelings (Cuijpers et al., 2007).
Understanding what components of depression influence the PTSD-suicidal ideation link in African American females is important given this populations’ vulnerability to these detrimental psychological disorders (Barbee, 1992; Breslau et al., 1991). Some research suggest that the cognitive-affective and somatic symptoms of depression can have a differing impact on propensity for suicidal ideation (Bohman, Jansson, Van Knorring, Päären, & Olsson,2010). However, more such information is needed, particularly if it is to inform interventions. For example, only one prior study has indicated evidence for a mediational relationship for depression in the PTSD-suicidal ideation link among African American women (Leiner et al., 2008).
Our investigation aimed to ascertain if depressive symptoms overall (Fig. 1) and the two components of depression (i.e., cognitive-affective and somatic; Fig. 2) mediated the PTSD-suicidal ideation link in inner-city, low-income, African American women. This is in part a replication of past research with African American women (Leiner et al., 2008), but is focused on a sample of inner-city, low-income, African American women who have attempted suicide. We also hypothesized that the specific cognitive-affective and somatic components of depression would serve a mediating role in this sample.
Fig. 1.
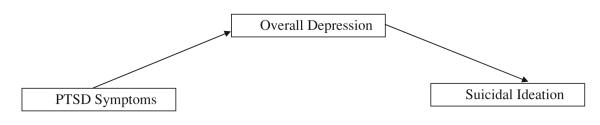
Model representing overall depression mediating the relationship between PTSD symptomatology and suicidal ideation
Fig. 2.
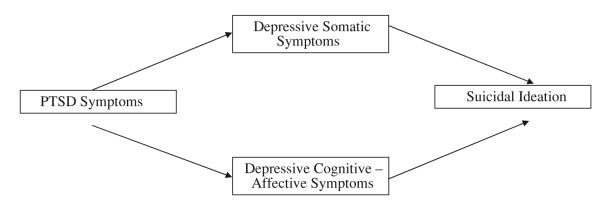
Multiple mediation model representing somatic symptoms of depression and cognitive-affective symptoms of depression mediating the relationship between PTSD symptomatology and suicidal ideation
Method
Participants
One hundred and thirty-six (N = 136) African American women, ages 18–64, were recruited from September 2002 to September 2006 at a large public hospital that serves a minority, inner-city, at-risk population. Individuals were included if they self-identified as African American and reported having made a suicide attempt in the prior 12 months. Of those women approached for study participation, 86 % agreed to do so, and thus the sample is representative of the population. Attempters were selected because they represent a group of individuals who have taken action on their ideation and they represent a more extreme form of suicidality on the suicide continuum (Silverman, Berman, Sanddal, O’Carroll, & Joiner, 2007). In addition, attempt status is a dichotomous variable that is concrete, whereas ideation is a continuous variable that is less concrete. Exclusion criteria included an inability to complete the interview due to delirium, cognitive impairment, or acute psychosis. Fifty-two percent (52 %) of the participants were homeless, 45 % were single and had never been married, 42 % had less than a twelfth grade education, only 29 % had a high school education, 15 % had some college or tech school, and only 5 % were college graduates (Table 1).
Table 1.
Demographic characteristics of the total sample
| Total sample (N = 136) N (%) |
|
|---|---|
| Relationship status | |
| Single/never married | 61 (44.9) |
| Partner, not living together | 12 (8.8) |
| Partner, living together | 16 (11.8) |
| Married | 7 (5.1) |
| Divorced | 21 (15.4) |
| Separated | 15 (11.0) |
| Widowed | 3 (2.2) |
| Missing | |
| Education | |
| <12th Grade | 57 (41.9) |
| High school graduate | 39 (28.7) |
| GED | 9 (6.6) |
| Some college/tech school | 20 (14.7) |
| Technical school graduate | 3 (2.2) |
| College graduate | 7 (5.1) |
| Graduate school | 1 (.1) |
| Missing | |
| Employed | |
| Yes | 16 (11.8) |
| No | 119 (87.5) |
| Missing | 1 (.7) |
| Homeless | |
| Yes | 71 (52.2) |
| No | 65 (47.8) |
| Age, M (SD) | 34.84 (11.16) |
Procedure
Referrals were done by hospital staff, who contacted the study pager 24/7/365 when an African American woman presented to the Level 1 trauma hospital used as the site for this study after a suicide attempt. Additionally, African American women who presented for nonpsychiatric medical care were screened and recruited if they met inclusion criteria. A psychotic screening questionnaire was administered to exclude any potential participants who were acutely psychotic. The Mini Mental State Exam (MMSE) (Folstein, Folstein, McHugh, & Fanjiang, 2001) and Rapid Estimate of Adult Literacy in Medicine (REALM) (Williams et al., 1995) were used to exclude potential participants that demonstrated cognitive limitations that might inhibit their ability to engage in the protocol. That is, women who scored <24 on the MMSE and whose reading was below a fourth grade reading level in accord with their scores on the REALM were excluded. Individuals who upon screening met the inclusion criterion were invited to complete a 2–3 h interview that encompassed a battery of measures including, but not limited to those examined in the current study. Some of the women had a low level of literacy, therefore the battery was provided by verbal administration to all participants to ensure consistency in administration and to not require women to disclose their difficulties with reading, which often is shameful to them. Participants were compensated $20 and referred for mental health services. The university Institutional Review Board and hospital Research Oversight Committee approved the study and ethics were followed for research by the American Psychological Association’s Ethical Principles of Psychologists and Code of Conduct.
Measures
Posttraumatic Diagnostic Scale (PDS)
Posttraumatic stress symptoms were examined with the PDS (Foa, 1995), a brief tool designed to assist clinicians in detecting and diagnosing PTSD. It measures PTSD symptoms related to a single identifiable traumatic event by assessing the DSM-IV criteria: severity, timeframe, experience of the event, and effects of symptoms on daily functioning. This 49 item measure has four sections: (1) trauma checklist, (2) description of respondent’s most upsetting traumatic event, (3) ratings of the 17 PTSD symptoms on a scale of 0 (“not all at one time”) to 3 (“5 or more times a week/always”), and (4) interference of the symptoms which ranges from 0 to 51 (0 = no rating, 1–10 = mild, 11–20 = moderate, 21–35 = moderate to severe, and >36 = severe) (Foa, Cashman, Jaycox, & Perry, 1997). The PDS has good construct validity, as well as high internal consistency reliability (α = .85 in the current sample) (Foa et al., 1997). Also, test–retest reliability was satisfactory for diagnosis of PTSD over a 2–3 week period (κ = .74) and test–retest using symptom severity scores yielded a significant correlation (.83). For the current study, the total number of PTSD symptoms was used as a continuous measure of PTSD symptoms.
Beck Depression Inventory-II (BDI-II)
Depressive symptoms were measured via the BDI-II (Beck, Steer, & Brown, 1996), the most widely used self-report scale for detecting depressive symptoms in adults (Arnua, Meagher, Norris, & Bramson, 2001; Beck et al.,1996). Each of the 21 items is rated on a 4-point scale, ranging from 0 to 3. Scores range from 0 to 63; 0–13 indicating minimal, 14–19 considered mild, 20–28 is moderate, and 29–63 considered severe symptoms. The measure has high internal consistency reliability (α = .92), and its construct validity and factorial validity has been established (Beck et al., 1996). There is evidence to support the validity of the measure and its factor structure in low-income samples of African Americans (Grother et al., 2005). In the current study, depression was assessed in terms of total depressive symptom scores, as well as the two factor scores that correspond with the two primary components of depression: cognitive-affective and somatic (Dozois, Dobson, & Ahnberg, 1998; Viljoen, Iverson, Griffiths, & Woodward, 2003; Whisman, Perez, & Ramel,2000). The cognitive-affective factor includes items related to sadness, past failure, anhedonia, guilt, feelings of punishment, low self-esteem, self-deprecation, suicidality, crying, agitation, loss of interest, indecisiveness, worthlessness, and irritability. The somatic factor is comprised of questions that tap loss of energy, changes in both sleep and appetite, difficulties with concentration, and tiredness or fatigue. These factors have been found to hold true with multiple samples and to have good concurrent validity. In the current sample, internal consistency reliability for the overall depressive symptom scale (α = .93) and cognitive-affective factor (α = .91) was excellent, and internal consistency reliability for the somatic factor was adequate (α = .79).
Beck Scale for Suicidal Ideation (BSS)
Suicidal ideation was assessed by the BSS (Beck & Steer, 1991), a 21-item self-report questionnaire that can identify the presence and severity of suicidal ideation. Items assess for the respondent’s plans for suicide, what may deter them from suicide, and their level of openness in revealing suicidal thoughts. The first two questions function as initial screening components, reducing the intrusiveness of the questionnaire for respondents who are not suicidal. Test–retest reliability has been reported at .54. Internal consistency has been found to be excellent (α = .90), including in the current sample (α = .91).
Results
Preliminary Analyses
Descriptive statistics on the variables of interest are presented in Table 2. Of the variables investigated, none of the distributions within the current sample deviated from normalcy. Although not surprising, given the demographic background of the sample, average levels of PTSD symptoms were higher than in the general population. Correlations among variables are outlined in Table 2. Results revealed significant and positive relations among PTSD symptoms, symptoms of depression (overall depressive symptoms, cognitive-affective symptoms, and somatic symptoms), and suicidal ideation.
Table 2.
Descriptive statistics and Pearson correlations among posttraumatic stress disorder (PTSD) symptoms, overall symptoms of depression, somatic symptoms of depression, cognitive-affective symptoms of depression, and suicidal ideation (N = 136)
| Variables | M (SD) | Min | Max | Correlations |
|||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||||
| 1. PTSDa | 11.78 (5.18) | 0 | 17 | – | – | – | – |
| 2. Depressionb | 32.10 (14.27) | 0 | 61 | .33** | – | – | – |
| 3. DEP-somaticc | 8.21 (3.59) | 0 | 15 | .31** | .86** | – | – |
| 4. DEP-cog-affectived | 22.64 (10.67) | 0 | 43 | .32** | .98** | .77** | – |
| 5. Suicidal ideatione | 12.06 (10.05) | 0 | 35 | .26** | .58** | .56** | .46** |
p<.05,
p<.01
Total number of PTSD symptoms from the Posttraumatic Diagnostic Scale (Foa, 1995)
Total score from Beck Depression Inventory-II (Beck et al., 1996)
Total score of somatic depression symptoms of depression from Beck Depression Inventory-II (Beck et al., 1996)
Total score of cognitive-affective symptoms of depression from Beck Depression Inventory-II (Beck et al., 1996)
Total suicidal ideation score from Beck Scale for Suicidal Ideation (Beck & Steer, 1991)
Planned Analyses
Recent research has supported bootstrapping techniques, over earlier models (Baron & Kenny, 1986; Holmbeck, 1997; Sobel, 1988), when examining indirect effects of meditational models (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; MacKinnon, Lockwood, & Williams, 2004; Preacher & Hayes, 2008). This methodology more accurately assesses the indirect effects of mediational models without assuming normality in the sampling distribution of indirect effects. Bootstrapping frees up power to assess multiple mediational models; it reduces the number of tests and controls for Type 1 error rates. In this study, indirect, direct, and total effects of PTSD symptoms, depressive symptoms (overall, cognitive-affective, and somatic) on suicidal ideation were calculated using appropriate SPSS macros (Preacher & Hayes, 2008). Indirect effects were considered significant if the bias corrected and accelerated bootstrapping confidence intervals (CIs, set at 95 % from 5,000 bootstrap samples) did not include zero.
First, overall depressive symptoms levels were tested as a mediator of the PTSD symptom-suicidal ideation link (Table 3). The overall model accounted for 34 % of the variance in suicidal ideation (R2 = .34, p < .01). As predicted, PTSD symptoms were associated positively with suicidal ideation (β = .25, p < .01), such that the greater the number of PTSD symptoms the higher the level of suicidal ideation. PTSD symptoms were associated significantly with overall depressive symptoms (β = .33, p < .01). Findings from the bootstrapping analysis revealed that overall depressive symptoms significantly mediated the relationship between PTSD symptoms and suicidal ideation (95 % bootstrap CI of .15 to .59, respectively).
Table 3.
Bootstrapping analyses investigating the relation among overall depressive symptoms, posttraumatic stress disorder (PTSD) symptoms and suicidal ideation, and the relation among somatic symptoms of depression, and cognitive-affective symptoms of depression on PTSD; N = 136
| Independent variable (DV) |
Mediator M | Effect of IV on M |
Effect of M on DV |
Total effects |
Direct effects |
Indirect effects |
BCa 95 % CI |
R 2 | |
|---|---|---|---|---|---|---|---|---|---|
| Coeff (SE) | Coeff (SE) | B (SE) | Coeff (SE) | Coeff (SE) | Lower | Upper | |||
| PTSD symptoms | Depression | .91 (.22)** | .39 (.05)** | .50 (.16)** | .14 (.15) | .36 (.10)** | .15 | .59 | .34** |
| Somatic | .22 (.06)** | .20 (.31) | .50 (.16)** | .16 (.15) | .04 (.07) | −.04 | .21 | .39** | |
| Cognitive | .66 (.17)** | .45 (.22)** | .30 (.10)** | .11 | .58 | ||||
BCa bias corrected and accelerated bootstrapping CIs; 5,000 bootstrap samples
p<.05,
p<.01
Results of the multiple mediational model tested through bootstrapping are presented in Table 3. The overall model accounted for 39 % of the variance in suicidal ideation (R2 = .39, p < .01), as well as both the cognitive-affective (β = .32, p < .01) and somatic (β = .31, p < .01) components of depression. When somatic and cognitive-affective symptoms of depression were assessed as multiple mediators of the PTSD-suicidal ideation relationship, only cognitive-affective symptoms significantly mediated the relationship (95 % bootstrap CI of .11 to .58, respectively). In other words, when controlling for the effects of the two types of depressive symptoms (i.e., cognitive-affective and somatic), only cognitive-affective symptoms could account for the link between PTSD symptoms and suicidal ideation.
Discussion
This study is the first of its kind to explore the relationship among PTSD symptoms, nature of depressive symptoms, and suicidal ideation in low-income, African American women who have attempted suicide. Consistent with previous findings, higher levels of PTSD symptoms were associated with overall levels of depressive symptoms and suicidal ideation (Campbell et al., 2007; Oquendo et al., 2003). As hypothesized, higher levels of PTSD symptoms also were associated with higher levels of both the cognitive-affective and somatic components of depression, which in turn also were correlated significantly with levels of suicidality. The mediating effect of depressive symptoms in the current sample was complex, such that overall depressive symptoms and the cognitive-affective components of depression, but not the somatic components of depression, accounted for the explained variance in the relationship between PTSD symptoms and suicidal ideation. Specifically, women with higher levels of PTSD symptoms tended to have higher levels of suicidal ideation and this was attributable at least in part to higher levels of overall depressive symptoms and more specifically, the cognitive-affective components of depression.
Thus, findings from the current study, which address not only overall depressive symptoms, but specific components of depression, offer new insights into these mediational processes. The results suggest that the cognitive-affective components of depression may play a unique mediational role in the association between PTSD symptoms and suicidal ideation. It is possible that African American women with PTSD are vulnerable to negative thoughts, which could lead to higher suicidal ideation. Additionally, this mediational role of cognitive-affective components of depression on the PTSD-suicidal ideation link may differ from what is the case for women of other races, socioeconomic statuses, and ethnicities due to higher rates of PTSD and a greater risk for depression and suicidal ideation among this low-income, inner-city population (Breslau et al., 1998; Cutrona et al., 2005). The mediating role of the cognitive-affective components of depression also may pertain to how many symptoms of PTSD are experienced in a cognitive-affective manner (i.e., re-experiencing, avoidance).
Despite the fact that the somatic components were associated positively with both PTSD symptoms and suicidal ideation, they did not have a mediational relationship, indicating that they may not mitigate the relationship or help explain how the relationship looks, a finding that was unexpected. We purport that the precedence of the cognitive-affective symptoms of depression in this mediational relationship may indicate that these processes are so profound that they may be causal of or overpower the somatic symptoms in this population. Furthermore, the fact that suicidal ideation involves cognition may offer a reasonable explanation for the stronger association for the cognitive-affective components of depression as a mediator rather than the somatic symptoms of depression. In addition, although the factor structure focused on in this study has been shown to be valid for African Americans (Grother et al., 2005), it is possible that another factor structure for the BDI-II may be more relevant to African Americans (Gary & Yarandi, 2004), and thus, the utility of these factors in this sample remains an empirical question. However, these findings remain somewhat surprising given that previous research has suggested that African Americans tend to endorse high levels of somatic symptoms when they are depressed and often show higher levels of somatic, but not cognitive-affective symptoms of depression when compared to their European American counterparts (Ayalon & Young, 2003; Brown, Schulberg, & Madonia, 1996; Das, Olfson, McCurtis, & Weissman, 2006).
Study findings must be considered in the context of a number of limitations. First, the sample was homogeneous with regard to gender, race/ethnicity, and social class, and thus the generalizability of the findings to other demographic groups is unknown. Second, this entire sample included individuals who had attempted suicide therefore findings are not generalizable to individuals who have not attempted suicide. Third, only self-report measures were used to assess PTSD and depressive symptoms. No diagnostic interviews were included, which would have allowed for testing of this model for disorders rather than symptoms associated with these psychiatric disorders. Fourth, our study did not delineate specific types of or severity of trauma, and these factors also might influence the associations that emerge. Fifth, the mediational relationship was assessed between PTSD symptoms and suicidal ideation, not the full continuum of suicidal behaviour such as attempted and completed suicide. Finally, the study was cross-sectional in nature and thus, the interpretation of study findings is limited to describing association among variables and not causation.
Despite these methodological weaknesses, our study underscores the crucial importance of assessing for, and treating overall depression, as well as the cognitive-affective components of depression, when African American women present for treatment with symptoms of PTSD and suicidal ideation. Given the risks associated with this clinical presentation, it is concerning that there are so many treatment barriers for low-income African Americans (Das et al., 2006; Davis et al., 2008) and outreach efforts need to be in place in communities to help reduce stigma and engage them in treatment (Pascoe & Smart Richman, 2009). When treatment is offered, mental health professionals should provide a multi-faceted treatment intervention that can decrease the acuity and presence of not only depressive symptoms in general, but the specific cognitive-affective components of depression, when an individual presents with both PTSD symptoms and depression. Such a clinical focus is likely to be particularly effective in decreasing suicidal ideation and the potential for suicide completions, as individuals that experience the comorbidity of these two illnesses are at a higher suicide risk (Bruce, 2010; Jakupcak et al., 2009). Cognitive-behavioral therapy and interpersonal therapy are designed in part to target the amelioration of the cognitive-affective presentation associated with PTSD, depression, and suicidal behaviour and thus are likely to be beneficial psychosocial interventions for this population (Bradley, Greene, Russ, Dutra, & Westen, 2005; Butler, Chapman, Forman, & Beck, 2006; Cuijpers et al., 2008; de Mello, de Jesus, Bacaltchuk, Verdeli, & Neugebauer, 2005). There is some suggestion that mindfulness-based cognitive therapy and mindfulness-based stress reduction may be particularly helpful in preventing relapse/recurrence of depression associated with difficulties in cognitive-affective processing (Ma & Teasdale, 2004; Ramel, Goldin, Carmona, & McQuaid,2004; Teasdale et al., 2000) and thus these intervention approaches should be seriously considered.
In the future, more attention should also be paid in the literature to ascertaining the optimal factor structure of the BDI-II for African Americans and assessing the mediational relationship with the full continuum of suicidal behaviour and specific types of trauma and across various demographic groups. Treatment outcome studies should be designed to test interventions that target PTSD and depressive symptoms in individuals at risk for suicidal behavior, with sessions devoted specifically to ameliorating the cognitive-affective components of depression. In addition, because African Americans are less likely than their European American counterparts to find antidepressant treatments beneficial (Cooper et al., 2003), they may be particularly receptive to psychological interventions that target primarily the cognitive-affective aspects of depression.
Acknowledgments
This research was supported by a grant from the Centers for Disease Control and Prevention National Center for Injury Prevention and Control: R49 CCR421767-01 entitled Group Interventions with Suicidal African American Women and a grant from the National Institute of Mental Health: 1R01MH078002-01A2 entitled Group Interventions for Abused, Suicidal Black Women, both awarded to the last author (Kaslow).
Footnotes
Conflicts of Interest None.
Contributor Information
Erika R. Carr, Department of Psychiatry and Behavioral Sciences, Grady Health System, School of Medicine, Emory University, 80 Jesse Hill Jr. Drive, NE, Atlanta, GA 30303, USA
Amanda M. Woods, Department of Psychiatry and Behavioral Sciences, Grady Health System, School of Medicine, Emory University, 80 Jesse Hill Jr. Drive, NE, Atlanta, GA 30303, USA
Arshya Vahabzadeh, Department of Psychiatry and Behavioral Sciences, Grady Health System, School of Medicine, Emory University, 80 Jesse Hill Jr. Drive, NE, Atlanta, GA 30303, USA.
Carla Sutton, Department of Psychiatry and Behavioral Sciences, Grady Health System, School of Medicine, Emory University, 80 Jesse Hill Jr. Drive, NE, Atlanta, GA 30303, USA.
Justine Wittenauer, Department of Psychiatry and Behavioral Sciences, Grady Health System, School of Medicine, Emory University, 80 Jesse Hill Jr. Drive, NE, Atlanta, GA 30303, USA.
Nadine J. Kaslow, Department of Psychiatry and Behavioral Sciences, Grady Health System, School of Medicine, Emory University, 80 Jesse Hill Jr. Drive, NE, Atlanta, GA 30303, USA
References
- Alim TN, Charney DS, Mellman TA. An overview of posttraumatic stress disorder in African Americans. Journal of Clinical Psychology. 2006;62:801–813. doi: 10.1002/jclp.20280. doi:10.1002/jclp.20280. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. fourth edition, text revision (DSMIV-TR) American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Arnua RC, Meagher MW, Norris MP, Bramson R. Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychology. 2001;20:112–119. doi: 10.1037//0278-6133.20.2.112. doi:10.1037//0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- Ayalon L, Young MA. A comparison of depressive symptoms in African Americans and Caucasian Americans. Journal of Cross-Cultural Psychology. 2003;34:111–124. doi:10.1177/0022022102239158. [Google Scholar]
- Barbee EL. African American women and depression: A review and critique of the literature. Archives of Psychiatric Nursing. 1992;6:257–265. doi: 10.1016/0883-9417(92)90036-i. doi:10.1016/0883-9417(92)90036-I. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. doi:10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bassuk EL, Buckner JC, Perloff JN, Bassuk SS. [Retrieved January 15, 2011];Prevalence of mental health and substance use disorders among homeless and low-income housed mothers. American Journal of Psychiatry. 1998 155:1561–1564. doi: 10.1176/ajp.155.11.1561. from http://ajp.psychiatryonline.org/ [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer R. Beck Scale for Suicidal Ideation: Manual. Harcourt Brace; San Antonio, TX: 1991. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory manual. 2nd ed Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Bohman H, Jansson U, Van Knorring A-L, Päären A, Olsson GI. Somatic symptoms as a marker for severity in adolescent depression. Acta Paediatrica. 2010;99:1724–1730. doi: 10.1111/j.1651-2227.2010.01906.x. doi:10.1111/j.1651-2227.2010.01906.x. [DOI] [PubMed] [Google Scholar]
- Borges G, Angst J, Nock MK, Ruscio AM, Kessler RC. Risk factors for the incidence and persistence of suicide-related outcomes: A 10-year follow-up study using the National Comorbidity Surveys. Journal of Affective Disorders. 2008;105:25–33. doi: 10.1016/j.jad.2007.01.036. doi:10.1016/j.jad.2007.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley RH, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. doi:10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. [Retrieved January 15, 2011];Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991 48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. from http://archpsyc.amaassn.org/ [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GD, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. doi:10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brown C, Schulberg HC, Madonia MJ. Clinical presentations of major depression by African Americans and whites in primary medical care practice. Journal of Affective Disorders. 1996;41:181–191. doi: 10.1016/s0165-0327(96)00085-7. doi:10.1016/S0165-0327(96)00085-7. [DOI] [PubMed] [Google Scholar]
- Bruce ML. Suicide risk and prevention in veteran populations. Annals of the New York Academy of Science. 2010;1208:98–103. doi: 10.1111/j.1749-6632.2010.05697.x. doi:10.1111/j.1749-6632.2010.05697.x. [DOI] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. doi:10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Campbell DG, Felker BL, Liu C-F, Yano EM, Kirchner JA, Chan D, et al. Prevalence of depression-PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine. 2007;22:711–718. doi: 10.1007/s11606-006-0101-4. doi:10.1007/s11606-006-0101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauffman E. A statewide screening of mental health symptoms among juvenile offenders in detention. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:430–439. doi: 10.1097/00004583-200404000-00009. doi:10.1097/00004583-200404000-00009. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, et al. The acceptability of treatment for depression among African-American, Hispanic, and White primary care patients. Medical Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. doi:10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Van Straten A, Andersson G, van Oppen P. Psychotherapy for depression in adults: A meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology. 2008;76:909–922. doi: 10.1037/a0013075. doi:10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Van Straten A, Warmerdan L. Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review. 2007;27:318–326. doi: 10.1016/j.cpr.2006.11.001. doi:10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Brown PA, Clark LA, Hessling RM, Gardner KA. Neighborhood context, personality, and stressful life events as predictors of depression among African American women. Journal of Abnormal Psychology. 2005;114:3–15. doi: 10.1037/0021-843X.114.1.3. doi:10.1037/0021-843X.114.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das AK, Olfson M, McCurtis HL, Weissman MM. [Retrieved February 5, 2011];Depression in African Americans: Breaking barriers to detection and treatment. Journal of Family Practice. 2006 55:30–39. from http://www.jfponline.com/ [PubMed] [Google Scholar]
- Davis RG, Ressler KJ, Schwartz AC, Stephens KJ, Bradley RG. Treatment barriers for low-income, urban African American with undiagnosed posttraumatic stress disorder. Journal of Traumatic Stress. 2008;21:218–222. doi: 10.1002/jts.20313. doi:10.1002/jts.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Mello MF, de Jesus M, Bacaltchuk J, Verdeli H, Neugebauer R. A systematic review of research findings on the efficacy of interpersonal therapy for depressive disorders. European Archives of Psychiatry and Clinical Neuroscience. 2005;255:75–82. doi: 10.1007/s00406-004-0542-x. doi:10.1007/s00406-004-0542-x. [DOI] [PubMed] [Google Scholar]
- Dozois DJA, Dobson KS, Ahnberg JL. A psychometric evaluation of the Beck Depression Inventory-II. Psychological Assessment. 1998;10:83–89. doi:10.1037/1040-3590.10.2.83. [Google Scholar]
- Foa EB. Posttraumatic Stress Diagnostic Scale: Manual. NCS Pearson Inc.; Minneapolis, MN: 1995. [Google Scholar]
- Foa EB, Cashman L, Jaycox LH, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. doi:10.1037/1040-3590.9.4.445. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR, Fanjiang G. Mini-mental State Examination. Psychological Assessment Resources; Odessa, FL: 2001. [Google Scholar]
- Garlow SJ, Rosenberg J, Moore JD, Haas AP, Koestner B, Hendin H, et al. Depression, desperation, and suicidal ideation in college students: Results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depression and Anxiety. 2008;25:482–488. doi: 10.1002/da.20321. doi:10.1002/da.20321. [DOI] [PubMed] [Google Scholar]
- Gary F, Yarandi HN. Depression among southern rural African American women: A factor analysis of the Beck Depression Inventory-II. Nursing Research. 2004;53:251–259. doi: 10.1097/00006199-200407000-00008. doi:10.1097/00006199-200407000-00008. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hur K, Bhamik DK, Mann JJ. The relationship between antidepressant use and rate of suicide. Archives of General Psychiatry. 2005;62:165–172. doi: 10.1001/archpsyc.62.2.165. doi:10.1001/archpsyc.62.2.165. [DOI] [PubMed] [Google Scholar]
- Grother KB, Dutton GR, Jones GN, Bodenlos J, Ancona M, Brantely PJ. Validation of the Beck Depression Inventory-II in a low-income African American sample of medical outpatients. Psychological Assessment. 2005;17:110–114. doi: 10.1037/1040-3590.17.1.110. doi:10.1037/1040-3590.17.1.110. [DOI] [PubMed] [Google Scholar]
- Hankin CS, Spiro AI, Miller DR, Kazis L. [Retrieved February 5, 2011];Mental disorders and mental health treatment among US Department of Veterans Affairs outpatients: The Veterans Health Study. American Journal of Psychiatry. 1999 156:1924–1930. doi: 10.1176/ajp.156.12.1924. from http://ajp.psychiatryonline.org/archive/ [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology. 1997;65:599–610. doi: 10.1037//0022-006x.65.4.599. doi:10.1037/0022-006X.65.4.599. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Cook J, Imel L, Fontana A, Rosenbeck R, McFall ME. Posttraumatic stress disorder as a risk factor for suicidal ideation in Iraq and Afghanistan war veterans. Journal of Traumatic Stress. 2009;22:303–306. doi: 10.1002/jts.20423. doi:10.1002/jts.20423. [DOI] [PubMed] [Google Scholar]
- Joe S, Kaplan MS. Suicide among African American men. Suicide and Life Threatening Behavior. 2001;31:106–121. doi: 10.1521/suli.31.1.5.106.24223. doi:10.1521/suli.31.1.5.106.24223. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Thompson M, Meadows L, Chance S, Puett R, Hollins L, et al. Risk factors for suicide attempts among African American women. Depression and Anxiety. 2000;12:13–20. doi: 10.1002/1520-6394(2000)12:1<13::AID-DA2>3.0.CO;2-Y. doi:10.1002/1520-6394(2000)12:1<13:AID-DA2>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Thompson MP, Okun A, Price A, Young S, Bender M, et al. Risk and protective factors for suicidal behavior in abused African American women. Journal of Consulting and Clinical Psychology. 2002;70:311–319. doi: 10.1037//0022-006x.70.2.311. doi:10.1037/0022-006X.70.2.311. [DOI] [PubMed] [Google Scholar]
- Leiner AS, Compton MT, Houry D, Kaslow NJ. Intimate partner violence, psychological distress, and suicidality: A path model using data from African American women seeking care at an urban emergency department. Journal of Family Violence. 2008;23:473–481. doi:10.1007/s10896-008-9174-7. [Google Scholar]
- Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology. 2004;72:31–40. doi: 10.1037/0022-006X.72.1.31. doi:10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JW, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. doi:10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. doi:10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magruder KM, Frueh BC, Knapp RG, Johnson MR, Vaughan JAI, Carson TC, et al. PTSD symptoms, demographic characteristics, and functional status among veterans treated in VA primary care clinics. Journal of Traumatic Stress. 2004;17:293–310. doi: 10.1023/B:JOTS.0000038477.47249.c8. doi:10.1023/B:JOTS.0000038477.47249.c8. [DOI] [PubMed] [Google Scholar]
- Moscicki EK. Epidemiology of completed and attempted suicide: Toward a framework for prevention. Clinical Neuroscience Research. 2001;1:310–323. doi:10.1016/S1566-2772(01)00032-9. [Google Scholar]
- Neighbors HW, Caldwell CH, Williams DR, Neese R, Taylor RJ, McKeever Bullard K, et al. Race, ethnicity, and the use of services for mental disorders: Results from the National Survey of American Life. Archives of General Psychiatry. 2007;64:485–494. doi: 10.1001/archpsyc.64.4.485. doi:10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]
- Nisbet PA. [Retrieved January 15, 2011];Protective factors for suicidal Black females. Suicide and Life-Threatening Behavior. 1996 26:325–341. from http://www.guilford.com/cgi-bin/cartscript.cgi?page=pr/jnsl.htm&dir=periodicals/per_psych&cart_id= [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in depression. Current Directions in Psychological Science. 2001;10:173–176. doi:10.1111/1467-8721.00142. [Google Scholar]
- Oquendo M, Brent DA, Birmaher B, Greenhill LL, Kolko D, Stanley B, et al. Posttraumatic stress disorder comorbid with major depression: Factors mediating the association with suicidal behavior. American Journal of Psychiatry. 2005;162:560–566. doi: 10.1176/appi.ajp.162.3.560. doi:10.1176/appi.ajp.162.3.560. [DOI] [PubMed] [Google Scholar]
- Oquendo M, Friend JM, Halberstam B, Brodsky BS, Burke AK, Grunebaum MF, et al. Association of comorbid posttraumatic stress disorder and major depression with greater risk for suicidal behavior. American Journal of Psychiatry. 2003;160:580–582. doi: 10.1176/appi.ajp.160.3.580. doi:10.1176/appi.ajp.160.3.580. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. doi:10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips DP, Ruth TE. [Retrieved January 15, 2011];Adequacy of official suicide statistics for scientific research and public policy. Suicide and Life-Threatening Behavior. 1993 23:307–319. from http://www.guilford.com/cgi-bin/cartscript.cgi?page=pr/jnsl.htm&dir=periodicals/per_psych&cart_id= [PubMed] [Google Scholar]
- Poussaint AF, Alexander A. Lay my burden down: Unraveling suicide and the mental health crisis among African Americans. Beacon Press; Boston: 2000. [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. doi:10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Ramel W, Goldin PR, Carmona PE, McQuaid JR. The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cognitive Therapy and Research. 2004;28:433–455. doi:10.1023/B:COTR.0000045557.15923.96. [Google Scholar]
- Schwartz A, Bradley R, Ressler KJ, Sexton M, Sherry A. [Retrieved January 15, 2011];Treating posttraumatic stress disorder in urban African American mental health patients. Journal of the American Psychoanalytic Association. 2004 52:464–465. from http://apa.sagepub.com/ [PubMed] [Google Scholar]
- Shahar G, Bareket L, Rudd MD, Joiner TE., Jr. In severely suicidal young adults, hopelessness, depressive symptoms, and suicidal ideation constitute a single syndrome. Psychological Medicine. 2006;36:913–922. doi: 10.1017/S0033291706007586. doi:10.1017/S0033291706007586. [DOI] [PubMed] [Google Scholar]
- Silverman MM, Berman AL, Sanddal ND, O’Carroll PW, Joiner TE. Rebuilding the tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide and Life-Threatening Behavior. 2007;37:248–263. doi: 10.1521/suli.2007.37.3.248. doi:10.1521/suli.2007.37.3.248. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Direct and indirect effect in linear structural equation models. In: Long JS, editor. Common problems/proper solutions: Avoiding error in quantitative research. Sage; Beverly Hills, CA: 1988. pp. 46–64. [Google Scholar]
- Stein MB, McQuaid JR, Pedrelli P, Lenox R, McCahill ME. Posttraumatic stress disorder in the primary care medical setting. General Hospital Psychiatry. 2000;22:261–269. doi: 10.1016/s0163-8343(00)00080-3. doi:10.1016/S0163-8343(00)00080-3. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. doi:10.1037//0022-006X.68.4.615. [DOI] [PubMed] [Google Scholar]
- Viljoen JL, Iverson GL, Griffiths S, Woodward TS. Factor structure of the Beck Depression Inventory-II in a medical outpatient sample. Journal of Clinical Psychology in Medical Settings. 2003;10:289–291. doi:10.1023/A:1026353404839. [Google Scholar]
- Whisman MA, Perez JE, Ramel W. Factor structure of the Beck Depression Inventory-Second edition (BDI-II) in a student sample. Journal of Clinical Psychology. 2000;56:545–551. doi: 10.1002/(sici)1097-4679(200004)56:4<545::aid-jclp7>3.0.co;2-u. doi:10.1002/(SICI)1097-4679. [DOI] [PubMed] [Google Scholar]
- Williams M, Parker R, Baker D, Parikh N, Pitkin K, Coates W, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–1682. doi:10.1001/jama.274.21.1677. [PubMed] [Google Scholar]
- Willis LA, Coombs DW, Drentea P, Cockerham WC. Uncovering the mystery: Factors of African American suicide. Suicide and Life-Threatening Behavior. 2003;33:412–429. doi: 10.1521/suli.33.4.412.25230. doi:10.1521/suli.33.4.412.25230. [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Feeny NC, Fitzgibbons LA, Foa EB. Response of African American and Caucasian women to cognitive behavioral therapy for PTSD. Behavior Therapy. 1999;30:581–595. doi:10.1016/S0005-7894(99)80026-4. [Google Scholar]


