Abstract
Muscle injuries can be classified as extrinsic or intrinsic injuries as well as contusions and lacerations, and clinical assessment is composed of the history and physical examination. Diagnostic imaging, particularly ultrasound (US) examination, is essential to a correct assessment of the severity of the injury and to exclude important complications as these two elements influence treatment decisions, prognosis and time to return to unrestricted physical activity. This paper presents the main clinical and US features of acute muscle injuries.
Keywords: Muscle injuries, Ultrasound
Riassunto
I traumi muscolari possono essere classificati in estrinseci, contusioni e lacerazioni, e intrinseci. Il riconoscimento avviene attraverso l’anamnesi e l’esame clinico. L’imaging, in particolare l’ecografia, é di fondamentale importanza per valutare correttamente la gravità del trauma e per escludere le principali complicanze, i due elementi che incideranno di più sul tipo di trattamento a cui sarà sottoposto il paziente, sulla prognosi e sulla tempistica del ritorno all’attività fisica. In questo articolo vengono presentate le principali caratteristiche cliniche ed ecografiche dei traumi muscolari acuti.
Introduction
According to the pathogenetic mechanism, muscle injuries are classified as extrinsic injuries such as contusions and penetrating wounds, where the site of the lesion corresponds to the site of impact, and intrinsic injuries caused by contraction and contemporary elongation of the muscles leading to muscle fiber destruction at the myotendinous junction.
Extrinsic injuries can involve all muscles, whereas intrinsic injuries mainly involve muscles consisting of type II muscle fibers which contract rapidly, are extended between two joints, perform eccentric contraction and have a fusiform muscle fiber arrangement.
Extrinsic injuries are classified clinically as mild, moderate or severe on the basis of functional impairment. Ultrasound (US) is performed to define location and extension of the lesion and to assess possible compression of the surrounding structures.
US is not the method of choice for classifying extrinsic muscle injuries, but in mild injuries US may show the muscle as hyperechoic without tearing of the muscle fibers, in moderate injuries US may show frayed muscle fibers involving less than 50 % in the axial plane, and in severe injuries US may show hematoma involving most of the muscles.
Intrinsic injuries are categorized into three grades based on the extension of the lesion: grade 1 involves a few muscle fibers within a bundle; in grade 2, the damaged fibers occupy up to 3/4 of the involved portion of the muscle; in grade 3, more than 3/4 is damaged and the lesion may involve the entire muscle belly (complete rupture). The role of US is to assess the longitudinal extent of the lesion, calculate the volume of the hematoma and detect possible compression of the adjacent structures.
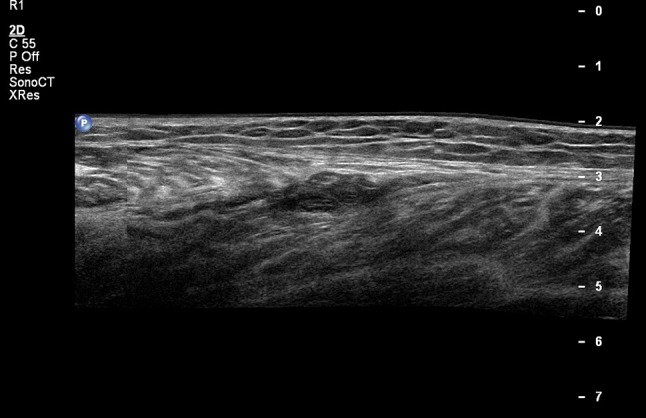
Us technique
US examination of a patient with suspected muscle injury should always be preceded by an accurate reporting of the patient’s medical history including the mechanism of injury, symptoms, possible pain and loss of strength, and a careful clinical evaluation which may reveal the presence of masses or morphological alterations of the of anatomical part under consideration. The patient should be placed in a comfortable position to facilitate transverse and longitudinal US scanning of the muscles in question, from the proximal attachment to the distal attachment including the myotendinous junction and entheses [1].
In some cases, a dynamic evaluation of the muscle groups in question may be useful [1, 2].
The entire muscle injury must be carefully studied, paying particular attention to the surrounding vascular and nervous elements. A careful study of the adjacent blood vessels is particularly important in view of the risk of venous thrombosis as a result of muscle injury [3].
Assessment of muscle injuries requires high frequency linear probes. Modern probes have a frequency ranging from 9 to 18 MHz and may be designed with broadband and multifrequency signal processing. According to the anatomical situation as well as the size and echogenicity of the muscle tissue, the operator will decide on the best compromise between resolution and signal penetration. The objective is to obtain a good resolution and image uniformity through entire field of view, from the near to the distant field [2, 4]. Accurate focus control is necessary to obtain the best possible resolution. The use of multiple focus points may be useful in the overall assessment of large areas to provide a uniform lateral resolution over the entire depth of field. In the detailed study of a specific area, it is useful to place at least one focus shortly below the specific area.
In the study of superficially located structures, compound imaging and harmonic imaging are used, as these techniques provide improved image quality and a better contrast due to the possibility to adjust the US beam [5].
Compound imaging rapidly acquires several overlapping scans from different view angles. Electronic beam steering provides sonographic information from different angles of insonation and also from interfaces which are not perpendicular to the beam. This technique therefore yields more information than conventional US even in case of increased anisotropy or in situations requiring a study of inclined surfaces and curves such as the myotendinous junction.
Tissue harmonic imaging uses higher frequencies generated on propagation of the US beam through the tissues yielding important information in the study of liquid/solid interfaces. As harmonic imaging reduces artifacts and improves contrast resolution, this technique is particularly useful in the evaluation of hematomas as it provides a marked distinction between liquids and solids.
In the study of deep lesions, it is useful to be able to control propagation velocity in the different tissues crossed by the US beams. When setting the machine, the operator must take into account that the beams will pass through different areas, some containing mainly adipose tissue and others containing mainly muscle tissue, particularly in superficial regions. These tissues have different densities and acoustic impedance and this may cause artifacts in the study of deep lesions.
The extended field of view technique is increasingly used in the evaluation of musculoskeletal disorders [5, 6]. In the study of large hematomas, assessment of the entire extension of the lesions is required, but the lesion is often larger than the probe, which generally measures 4–6 cm. In these cases, trapezoid US imaging is often used, as this technique provides an image which is enlarged through lateral beam steering. Panoramic imaging is even more effective; through longitudinal translation of the probe, the software can reconstruct an elongated and calibrated image, which is the result of registration and alignment of the scanning planes crossed by the beams. In that way the obtained images can present a large lateral field of view (up to 1 m) and this allows measurement and accurate assessment of large lesions thereby facilitating interpretation of the patient’s condition (Fig. 1). Panoramic imaging provides reconstruction of a composite image by simultaneous recording and acquisition in order to create a single image with a large field of view. This technique has the main advantage of making it easier for the clinician to interpret the US image [6, 7].
Fig. 1.
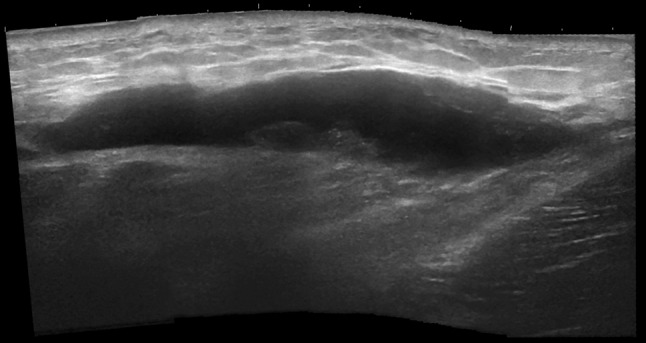
Subcutaneous hematoma, panoramic image. US shows a subcutaneous anechoic mass which does not involve the muscle
Power and color Doppler have proved useful in evaluating muscles, lesion vascularity and other blood vessels which may be affected by the muscle injury [5, 6]. In the study of vascularity in connection with muscle injury, it is crucial that the parameters are set correctly. Pulse repetition frequency (PRF) should be set to max 0.8 MHz, wall filter setting should be low and focus should be set on the area to be studied in order to increase sensitivity for the detection of slow blood flow [5].
However, if the dynamics of the traumatic event are not clear, if the size of the hematoma is disproportionate to the trauma, if the hematoma is evolving in an unusual way or in the presence of a mass located within the muscle tissue, it should be kept in mind that color Doppler US alone cannot exclude bleeding from an intramuscular tumor. In these cases US using contrast agent consisting of gas-containing microbubbles with a carbohydrate or protein shell should be performed as this technique can detect micro-and macrovessels of the studied area and show the pattern of possible perfusion abnormalities.
Us examination
Extrinsic injuries: contusions–lacerations
A muscle contusion is a non-penetrating injury to the soft tissue caused by a direct impact. These injuries occur most often in people who practice contact and/or collision sports, but they are also frequent in everyday life. Muscle contusions may produce tear of muscle fibers and damage blood vessels resulting in hemorrhage and myofiber necrosis [8]. The extent of the injury may produce a wide range of clinical conditions: from mild bruising to large intramuscular or intermuscular hematoma or hematoma located in the deep layers between the muscle tissue and the bone.
Physical examination may reveal localized pain, muscle stiffness, swelling and loss of muscle function resulting in moderate to severe loss of motion. The most frequently involved muscle groups are the quadriceps femoris and gastrocnemius, but contusion may also involve the muscles of the upper limbs, particularly in the so-called “weekend warriors” [2, 9].
A clinical grading of muscle contusions has been proposed in the literature. This grading is very useful for establishing prognosis and making appropriate decisions regarding when to return the patient to athletic activities. Contusions are graded as mild, moderate and severe [10]. In mild contusions, range of motion (ROM) is reduced by up to 1/3 as compared to ROM before the injury, and physical activity can generally be resumed after 6 days. In moderate contusions ROM is reduced by 1/3–2/3 of ROM before the injury, and physical activity can be resumed after an average of 56 days. In severe contusions ROM is reduced by more than 2/3 of ROM before the injury, and physical activity can generally be resumed after more than 60 days.
Diagnosis and grading of contusions are therefore based on the patient’s clinical history and residual muscle function. Diagnostic imaging, particularly US examination, is essential for detecting location and extent of the lesion as well as possible complications [3]. US appearance of muscle contusions depends on the size and on the time elapsed between the injury and the examination, the patient’s age and possible bleeding disorders.
In mild contusions, US may show focal isoechoic muscle swelling against the background of the undamaged muscle tissue. The lesion usually resolves quickly leaving no permanent damage.
More severe contusions with hematoma may appear differently depending on the time elapsed between the injury and the examination. Within the first 24 h, hematomas may appear both hypoechoic and hyperechoic. In the following days, hematomas will tend to appear hypoechoic or anechoic until they become inhomogeneous after coagulation (Figs. 2, 3); they will subsequently resolve, maybe leaving scar tissue [1, 2, 9].
Fig. 2.
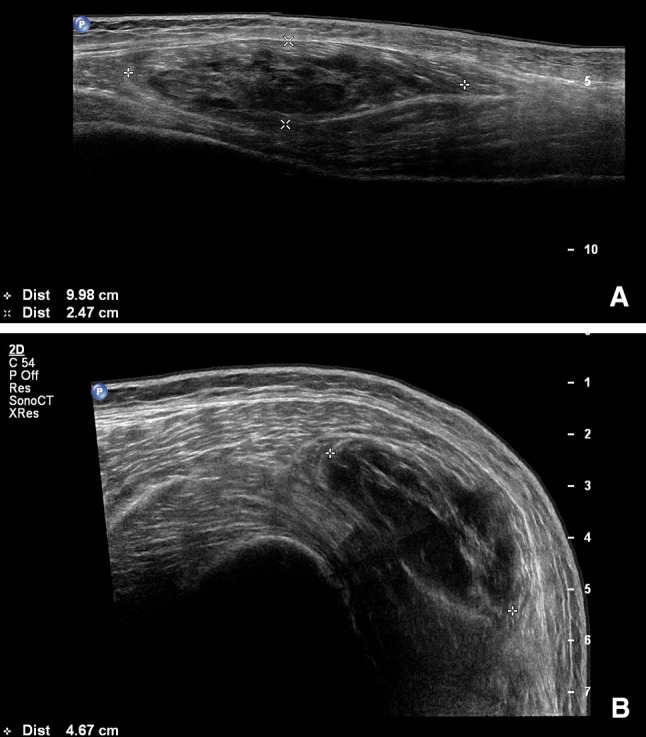
Intramuscular hematoma. US shows an intramuscular, inhomogeneous mass providing information about the size (a long axis and b short axis of the lesion)
Fig. 3.
Intra- and extramuscular hematoma. US shows location and size of the lesion (a, b) as well as the extramuscular portion of the hematoma
Muscle tears are caused by sharp edged and/or pointed instruments. Such injuries may be complete or incomplete and may involve several muscle compartments. They may also lead to the formation of hematomas. Diagnosis is mainly made on the basis of physical examination [1]. In the acute phase muscle tears are rarely assessed by US, but US imaging will show rupture of muscle fibers [1].
Intrinsic injuries
Intrinsic muscle injuries include a range of injuries affecting the myotendinous junction. They occur due to contraction and simultaneous elongation of the muscles leading to destruction of myofibers. They are the most frequent traumatic muscle injuries in athletes [10].
Intrinsic muscle injuries most often involve muscles containing type II fibers (fast-twitch fibers), i.e., biarticular muscles (spanning over two joints) producing eccentric contraction; these injuries are more frequent in muscles that have already been affected by intrinsic injury [11]. Most at risk are the rectus femoris, medial gastrocnemius, biceps brachii and the hamstrings. Histologically, these lesions present hemorrhage and muscle fiber necrosis followed by a phase of repair and remodeling of the tissue where stem cells and fibroblasts contribute to the formation of scar [12].
Clinical symptoms of intrinsic injuries are acute pain, muscle weakness and swelling typically during physical activity, e.g., runners during the sprinting stage. If the injury causes bleeding, patients may present with ecchymosis in the days following the trauma. The bleeding is not necessarily confined strictly to the injured muscle tissue as it may extend through the muscle fascia and the perimysium into the subcutaneous space and be located distally to the myotendinous junction. In contrast, contusions produce ecchymosis at the site of the injury [1, 2, 12].
The use of diagnostic imaging is essential in confirming clinical diagnosis, particularly in cases where the mechanism of injury is not clear, to exclude possible complications and to establish when the patient can return to unrestricted physical activity [13].
Different classification systems are published in the literature categorizing intrinsic muscle injuries; however, there is no universally accepted classification system. A widely used clinical grading system divides these injuries into three degrees according to functional impairment of the affected muscle. In grade 1, muscle function loss amounts to less than 5 %; in grade 2, muscle function loss ranges from 5 to 50 %; in grade 3, muscle function loss exceeds 50 % [10].
Recently, a new classification system for intrinsic muscle injuries has been proposed. Also this classification system divides the lesions into three types: type 1, the lesions are localized at the proximal myotendinous junction; type 2, the lesion is located within the muscle; type 3, the lesion is located at the distal myotendinous junction [14].
At US, intrinsic muscle injuries are divided into three grades on the basis of US appearance: mild, moderate and severe (Table 1) [15, 16]. This classification system has diagnostic and prognostic value. Grade 1 lesions generally heal in 1–2 weeks, whereas return to physical activity should be delayed for 5–8 weeks in grade 3 lesions in order to reduce the risk of recurrence, which is the main complication of intrinsic lesions [17].
Table 1.
US grading of intrinsic muscle injuries
| Grade | US findings |
|---|---|
| 0 | No US image suggesting muscle injury |
| 1 | Small areas of damaged muscle tissue (<5 %) |
| 2 | Partial lesion (>5 %) which does not involve the entire muscle |
| 3 | Complete rupture of the muscle at the myotendinous junction |
The role of US is of primary importance in the acute phase (from 2 to 48 h from the injury) when sensitivity of US is similar to that of magnetic resonance imaging (MRI) [17–19]. In grade 1 lesions, US appearance of the muscle may be normal or show small hyperechoic areas occupying less than 5 % of the muscle tissue. The presence of damaged muscle fibers used to be considered as an indication of a grade 1 injury, but this finding actually suggests a grade 2 injury [9, 14, 16]. Occasionally, US may reveal the presence of perifascial fluid [18]. Grade 2 injuries involve more than 5 % of the examined muscle compartment. US imaging often shows discontinuity of the perimysium at the myotendinous or myofascial junctions [1, 10, 15]. Grade 3 lesions present with complete rupture of the muscle associated with hematoma, which may be large (Figs. 4, 5) [2].
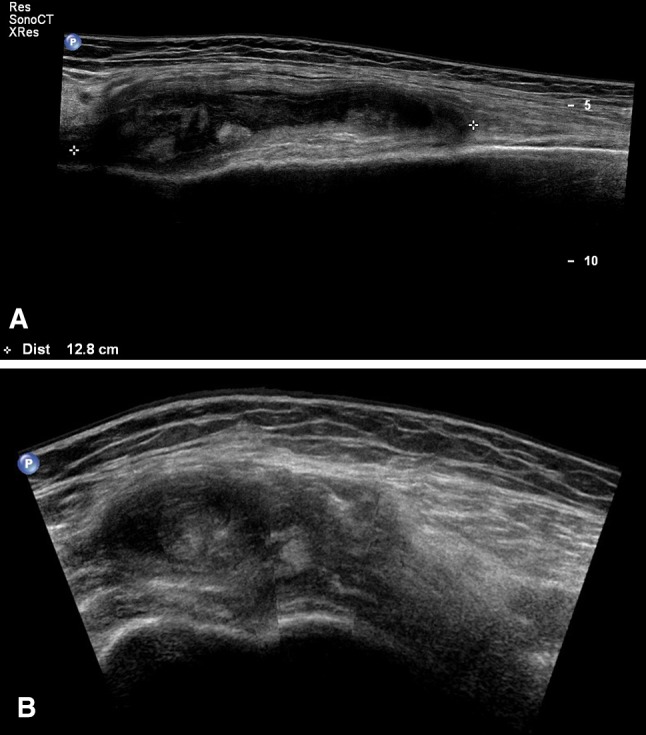
Fig. 4.
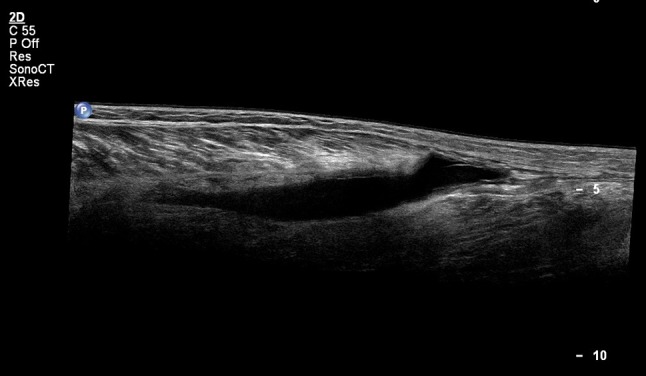
Medial gastrocnemius tendon rupture. The muscle is retracted and there is a large hematoma between the retracted muscle and the fascia
Fig. 5.
Medial gastrocnemius tendon rupture, coagulation phase. Appearance is similar to that of Fig. 4, except the pseudo-solid appearance of the hematoma
US is less sensitive than MRI in the detection of grade 1 lesions, but due to the high sensitivity of US in detecting areas with damaged muscle fibers, US has proved more reliable in the staging of grade 2 lesions, which are often classified as type 1 on the basis of MRI alone. Areas with damaged muscle fibers present an altered echogenicity and loss of striation in the muscle fibers and they are located near the myotendinous junction. They are found in less than 5 % of the muscle in grade 1 lesions and in more than 5 % of the muscle in grade 2 lesions and tend to be associated with hematoma [1, 2, 16].
Conclusion and discussion
Muscle injuries account for one-third of sports injuries. In a recent study, it was estimated that a senior football team with 25 players should expect about 15 muscle injuries in a single season, leading to an average of 225 days absence from the field. Data related to other sports activities are similar. These data show how important the impact of muscle injuries is on the costs. In view of this, it is essential that muscle injuries are detected and correctly graded, as type and severity of the injury influence management and time to return to sports activities [20, 21].
Imaging techniques are therefore essential for a correct classification of the injury, assessment of severity and to exclude complications. US imaging can be performed in the acute phase, 3–7 days and possibly 5–7 weeks after the trauma to assess the healing process of the muscle injury. MRI should be performed if there is a discrepancy between the outcome of clinical and US examination, if US imaging shows hematoma in the absence of trauma, and if the muscle injury has not healed at US follow-up after 5–7 weeks. Both US and MRI can furthermore show complications associated with muscle injury [3].
The role of other imaging modalities, such as radiography and computed tomography (CT) is limited and used only in special circumstances. Radiography is indicated in the evaluation of suspected myositis ossificans, and CT if the clinicians suspect the presence of expanding hematoma [3, 10].
Conflict of interest
The authors certify that there is no actual or potential conflict of interest in relation to this article.
References
- 1.Datir A, Connell DA. Muscle injury and complications. In: Robinson P, editor. Essential radiology for sports medicine. New York: Springer Science-Business Media, LLC.; 2010. pp. 199–215. [Google Scholar]
- 2.Woodhouse JB, McNally EG. Ultrasound of skeletal muscle injury: an update. Semin Ultrasound CT MRI. 2011;32:91–100. doi: 10.1053/j.sult.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Alessandrino F, Balconi G (2013) Complications of muscle injuries. J Ultrasound. doi:10.1007/s40477-013-0010-4 [DOI] [PMC free article] [PubMed]
- 4.Lee JC, Healy J. Sonography of lower limb muscle injury. AJR Am J Roentgenol. 2004;182(2):341–351. doi: 10.2214/ajr.182.2.1820341. [DOI] [PubMed] [Google Scholar]
- 5.Klauser AS, Peetrons P. Developments in musculoskeletal ultrasound and clinical applications. Skeletal Radiol. 2010;39(11):1067–1071. doi: 10.1007/s00256-009-0782-y. [DOI] [PubMed] [Google Scholar]
- 6.Barberie JE, Wong AD, Cooperberg PL, Carson BW. Extended field-of-view sonography in musculoskeletal disorders. AJR Am J Roentgenol. 1998;171(3):751–757. doi: 10.2214/ajr.171.3.9725310. [DOI] [PubMed] [Google Scholar]
- 7.Weng L, Tirumalai AP, Lowery CM, Nock LF, Gustafson DE, Von Behren PL, et al. US extended-field-of-view imaging technology. Radiology. 1997;203(3):877–880. doi: 10.1148/radiology.203.3.9169720. [DOI] [PubMed] [Google Scholar]
- 8.Järvinen TA, Järvinen TL, Kääriäinen M, Kalimo H, Järvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33:745–764. doi: 10.1177/0363546505274714. [DOI] [PubMed] [Google Scholar]
- 9.Jackson DW, Feagin JA. Quadriceps contusions in young athletes. Relation of severity of injury with treatment and prognosis. J Bone Joint Surg (Am) 1973;55:95–105. [PubMed] [Google Scholar]
- 10.Lee JC, Mitchell AW, Healy JC. Imaging of muscle injury in the elite athlete. Br J Radiol. 2012;85(1016):1173–1185. doi: 10.1259/bjr/84622172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shelly MJ, Hodnett PA, MacMahon PJ, Kavanagh EC, Eustace SJ. MR imaging of muscle injury. Magn Reson Imaging Clin N Am. 2009;17:757–773. doi: 10.1016/j.mric.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 12.Garrett WE., Jr Muscle strain injuries. Am J Sports Med. 1996;24:S2–S8. doi: 10.1177/036354659602400102. [DOI] [PubMed] [Google Scholar]
- 13.Orchard J, Best TM, Verrall GM. Return to play following muscle strains. Clin J Sport Med. 2005;15:436–441. doi: 10.1097/01.jsm.0000188206.54984.65. [DOI] [PubMed] [Google Scholar]
- 14.Chan O, Del Buono A, Best TM, Maffulli N. Acute muscle strain injuries: a proposed new classification system. Knee Surg Sports Traumatol Arthrosc. 2012;20(11):2356–2362. doi: 10.1007/s00167-012-2118-z. [DOI] [PubMed] [Google Scholar]
- 15.Peetrons P. Ultrasound of muscle. Eur Radiol. 2002;12:35–43. doi: 10.1007/s00330-001-1164-6. [DOI] [PubMed] [Google Scholar]
- 16.Peetrons P, Sintzoff S (1987) Les accidents du membre inferieur chez les sportifs: Integration des differents modes d’imagerie. J Francophone Radiol
- 17.Koh ESC, McNally EG. Ultrasound of skeletal muscle injury. Semin Musculoskelet Radiol. 2007;11(2):162–173. doi: 10.1055/s-2007-1001881. [DOI] [PubMed] [Google Scholar]
- 18.Bianchi S, Martinoli C, Abdelwahab IF, Derchi LE, Damiani S. Sonographic evaluation of tears of the gastrocnemius medial head (“tennis leg”) J Ultrasound Med. 1998;17:157–162. doi: 10.7863/jum.1998.17.3.157. [DOI] [PubMed] [Google Scholar]
- 19.Delgado GJ, Chung CB, Lektrakul N, Azocar P, Botte MJ, Coria D, et al. Tennis leg: clinical US study of 141 patients and anatomic investigation of four cadavers with MR imaging and US. Radiology. 2002;224(1):112–119. doi: 10.1148/radiol.2241011067. [DOI] [PubMed] [Google Scholar]
- 20.Mueller-Wohlfahrt HW, Haensel L, Mithoefer K, Ekstrand J, English B, McNally S, et al. Terminology and classification of muscle injuries in sport: the Munich consensus statement. Br J Sports Med. 2013;47:342–350. doi: 10.1136/bjsports-2012-091448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ekstrand J, Hagglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer) Am J Sports Med. 2011;39:1226–1232. doi: 10.1177/0363546510395879. [DOI] [PubMed] [Google Scholar]


