Abstract
Introduction
Fiberoptic bronchoscopy is the standard method for verifying the correct position of a double-lumen endotracheal tube (DLET) prior to one-lung ventilation. However, it must be performed by a specially trained anesthesiologist and is often resource consuming. The aim of this study was to compare this approach with thoracic ultrasound done by a nurse anesthetist in terms of sensitivity, specificity, and cost-effectiveness.
Methods
We conducted a prospective cross-over case–control study involving 51 adult patients consecutively undergoing thoracic surgery with one-lung ventilation. After orotracheal intubation with a DLET, correct exclusion of the lung being operated on exclusion was assessed first by a certified anesthesiologist using standard fiberoptic bronchoscopy and then by a trained nurse anesthetist using thoracic ultrasound. The nurse was blinded as to the findings of the anesthesiologist’s examination.
Results
The two approaches proved to be equally sensitive and specific, but the ultrasound examination was more rapid. This factor, together with the fact that ultrasound was performed by a nurse instead of a physician, and the costs of materials and sterilization, had a significant economic impact amounting to a net saving of €37.20 ± 5.40 per case.
Conclusions
Although fiberoptic bronchoscopy is still the gold standard for checking the position of a DLET, thoracic ultrasound is a specific, sensitive, cost-effective alternative, which can be used to rapidly verify the proper function of the tube based on the demonstration of correct lung exclusion.
Keywords: Thoracic ultrasound, Anesthesia, Thoracic surgery
Riassunto
Introduzione
La fibrobroncoscopia è attualmente la tecnica di scelta per la verifica di un corretto posizionamento del tubo endotracheale a doppio lume, prima dell’esclusione polmonare necessaria alla ventilazione monopolmonare. Tale tecnica richiede tuttavia un medico anestesista specialista adeguatamente formato ed è dunque spesso costosa. Scopo dello studio è di compararla all’ecografia toracica effettuata da infermieri anestesisti, in termini di sensibilità, specificità e costo-efficacia.
Metodi
Abbiamo dunque realizzato uno studio caso-controllo, cross-over, in effettuata da un infermiere anestesista specificamente formato.una coorte continua di pazienti adulti sottoposti a chirurgia toracica in ventilazione monopolmonare. Dopo intubazione oro-tracheale con tubo doppio lume, ciascun paziente è stato sottoposto dapprima a controllo fibrobroncoscopico effettuato da un medico anestesista e successivamente ad ecografia toracica effettuata da un infermiere anestesista specificamente formato per determinare una corretta esclusione del polmone operato. L’infermiere non era a conoscenza dei risultati del controllo fibrocroncoscopico.
Risultati
Le due tecniche sono risultate comparabili in termini di sensibilità e specificità. L’ecografia toracica è risultata una tecnica significativamente più rapida da eseguire rispetto alla fibrobroncoscopia. Il tempo di esecuzione, unitamente al fatto che l’ecografia è stata eseguita da un infermiere, al costo del materiale nonché della sua sterilizzazione, hanno determinato un impatto economico significativo, con un risparmio netto di €37.20 ± 5.40 per caso trattato con ecografia toracica.
Conclusioni
Sebbene la fibrobroncoscopia rimanga il gold standard per il controllo e l’ottimizzazione del posizionamento del tubo endotracheale a doppio lume, l’ecografia toracica è una metodica sensibile, specifica e costo-efficace per valutarne rapidamente il corretto funzionamento, attraverso la verifica di una corretta esclusione polmonare.
Background
Double-lumen endotracheal tubes (DLETs) are commonly employed in thoracic surgery and other interventions requiring surgical access to the chest cavity, such as esophageal surgery and orthopedic surgery on the thoracic spine. DLETs are also used in intensive care settings to isolate a diseased lung or provide differential ventilation of the two lungs [1–3]. Of the various models that have been developed, the Carlens, the White, and the Robertshaw tubes are the ones most widely used. Regardless of the model, DLETs are generally inserted under direct laryngoscopy (like any other endotracheal tube), with the longer bronchial lumen curved anteriorly. Once this lumen has passed through the glottis, the tube is blindly rotated 70–90°, so that the bronchial lumen will enter main-stem bronchus that is to be intubated. Left-sided DLETs are more commonly employed than their right-sided counterparts. The latter tubes are mainly used for delivery of anesthesia during specific surgical procedures, such as substantial left-sided lung resections or left pneumonectomies, because their use is associated with a high risk of right upper lobe bronchus exclusion, which can lead to intraoperative atelectasis and hypoxia [2, 3].
Correct placement of DLETs is vital: incomplete lung exclusion resulting from a malpositioned tube is a direct or indirect cause of significant morbidity and mortality in patients undergoing thoracic surgery, and it accounts for up to 30 % of the perioperative deaths occurring in specific subpopulations, such as esophageal surgery patients. For this reason, the method of choice for verifying correct DLET placement involves auscultation confirmed by fiberoptic bronchoscopy [1–3].
The costs of this approach are high, however, in terms of both personnel and equipment. The bronchoscopy procedure is generally performed by a fully trained anesthesiologist, and the costs of the scope itself and its sterilization after each procedure are by no means negligible. Moreover, sterilization is a relatively lengthy process, so multiple bronchoscopes are mandatory in anesthesiology departments with high thoracic surgery case loads. Repeated sterilization can also significantly shorten the life of the bronchoscope life, inevitably producing some degree of damage to the optic fibers [2, 3].
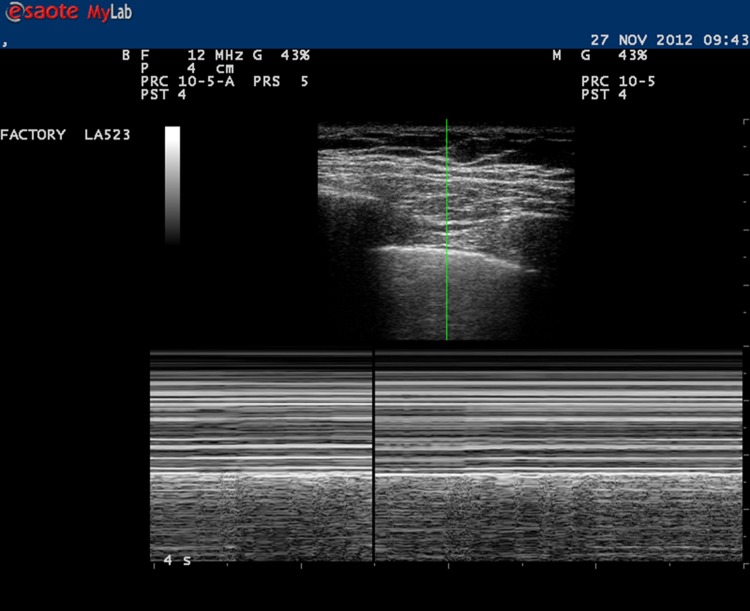
Thoracic ultrasound is playing increasingly important roles in the fields of emergency and intensive care medicine. It allows prompt detection of life-threatening conditions, such as hemothorax or pneumothorax, and it has proved to be extremely helpful in accelerating the differential diagnosis of acute respiratory distress in critically ill patients [4–6]. It has been shown to have very high sensitivity and specificity in the detection of pneumothorax and outperforms plain chest radiography in emergency settings [4–15]. Ultrasonographic diagnosis of pneumothorax is based on the absence of two specific findings. The first is the so-called sliding sign, which reflects the movement of the hyperechoic visceral pleura as it glides over the parietal pleura in a normally aerated and ventilated lung. The second is the seashore sign, which represents M-mode depiction of pleural movements in a single section of the thorax [15] (Fig. 1).
Fig. 1.
Thoracic ultrasound: sliding sign and seashore sign in M-mode
Recent years have also witnessed an increase in the use of specially trained ultrasound nurses, particularly in emergency settings. Protocols that include image acquisition by such nurses, such as the extended Focused Assessment with Sonography in Trauma (FAST) protocol, have been successfully implemented in many centers and multiple settings, including the emergency room and extra-hospital sites. These protocols provide for the use of thoracic ultrasound for the exclusion of pneumothorax and hemothorax. In this context, standardized ultrasound images acquired by nurses according to specific protocols can be just as effective and less expensive than ultrasound performed by physicians [16, 17].
The present study was conducted to compare the time requirements, specificity, sensitivity, and cost-effectiveness of preoperative fiberoptic bronchoscopy by a staff anesthesiologist and thoracic ultrasound performed by a trained nurse anesthetist for confirming correct placement of left-sided DLET in patients undergoing thoracic surgery.
Materials and methods
The protocol received local ethics committee approval, and oral consent was obtained from all enrolled patients. The prospective cross-over case–control study was conducted on a consecutive cohort of adult patients undergoing thoracic surgery under single lung ventilation. The sole exclusion criteria were patient refusal and airway features that prevented use of a DLET.
Anesthesia was induced, a left-sided Robertshaw DLET was inserted, and positive pressure ventilation was delivered through a Bain circuit. At this point, the anesthesiologist checked the position of the DLET with a fiberoptic bronchoscope (Karl Storz & Co, Germany) inserted via the tracheal lumen of the tube. The tube was considered to be correctly positioned when the upper margin of the bronchial cuff was visualized protruding from the left main-stem bronchus. When the bronchoscopic examination had been completed, a specially trained nurse anesthetist, who was unaware of the anesthesiologist’s findings, performed thoracic ultrasound with an 8-MHz linear probe (LogicQ, GE, Michigan, IN, USA). The presence/absence of the sliding sign was assessed with B-mode imaging in right and left lower quadrants of the thorax, at the level of the costophrenic angles. The tube was considered to be correctly positioned when bronchial lumen occlusion was followed by selective loss of the sliding sign on the left.
Each examiner recorded the results of his/her evaluation on separate pieces of paper. The results were expressed as follows: correct position, incorrect position, or inconclusive exam. The two evaluations were then compared, and if the results were discordant (including cases in which one of the methods produced inconclusive results), the two examinations were repeated until consensus was obtained.
The duration of the bronchoscopic examination was calculated from the time the scope was introduced into the tracheal lumen of the DLET. The starting point of the ultrasound examination was placement of the transducer on the patient’s chest. For both procedures, the end point was when the examiner had recorded his/her judgment.
A sample size of 51 patients per group was chosen to demonstrate the non-inferiority of nurse-performed ultrasound vs. physician-performed bronchoscopy with a significance level of 5 % and a power of 90 %. Data were collected anonymously in an electronic database.
The economic assessment of the two procedures was based on a cost-minimization analysis. In both cases, the point of view adopted for the economic analysis was that of the hospital administration. A top–down technique was used to estimate staff-related costs, and micro-costing was used to calculate costs related to the use of drugs and devices in the two groups. Indirect fixed costs (material and resources required for operation and anesthesia) and costs related to in-hospital management and postoperative care were assumed to identical in the two groups (i.e., unrelated to the procedure used to verify correct DLET placement). The economic analysis did consider costs directly related to the execution of the two techniques (i.e., those for staff, materials, and equipment sterilization). All costs were expressed in Euros.
Unpaired t tests were used to determine the significance of parametric data, and the Mann–Whitney U test was used for non-parametric data. A p value <0.05 was considered statistically significant (95 % confidence interval). Results are reported as means (m) ± standard deviation (SD) for normally distributed variables or medians (M) and interquartile ranges (IQR) for those with non-normal distributions. Statistical analyses were performed with the SPSS (IBM, Armonk, NY, USA) and Numbers’09 (version 2.1) (Apple Inc., Cupertino, CA, USA) software packages.
Results
A total of 51 patients were enrolled over a period of 5 months. All were adults (mean age 62.6 ± 1.95 years, 29 males, 22 females) with American Society of Anesthesiologists (ASA) grades ranging from I to III. No patient was excluded from the study.
The two techniques proved to be equally sensitive and specific in verifying the correct position of the left DLET positioning. Results were discordant in only one case. In this patient, fiberoptic bronchoscopy confirmed the correct position of the DLET position while thoracic ultrasound findings were inconclusive owing to the absence of an suitable acoustic window, which precluded clear-cut demonstration of the sliding sign. The difference between the two groups was not, however, statistically significant (p = 0.308). The sensitivities of the two methods were identical (p = 1.000).
The ultrasound assessment was associated with a significantly shorter mean procedure time than fiberoptic bronchoscopy (2.08 ± 0.5 vs. 7.70 ± 4.2 min, p < 0.05). This difference, together with the fact that the ultrasound examination was performed by a nurse anesthetist instead of an anesthesiologist, had a significant economic impact consisting of a net saving of €5.20 ± 0.40 per patient treated (p < 0.05). The difference between the two approaches was even more obvious when we considered costs linked to standard cleaning and sterilization procedures: the savings associated with the ultrasound examination increased by €23.30 ± 5.30 (p < 0.05). Finally, when we also included the costs of materials and equipment amortization, an additional savings of €8.70 ± 2.40 emerged in favor of ultrasound (p < 0.05). Ultrasound was thus significantly associated with a net reduction in overall costs, including those related to staff, material, and equipment. In this case series, the total reduction per case (€37.20 ± 5.40) translated into an overall reduction in hospital costs of €7,810.72 ± 52.70.
Discussion
To our knowledge, this is the first study that has evaluated the use of thoracic ultrasound for verification of correct lung exclusion before initiating one-lung ventilation for thoracic surgery. Ultrasound has been well established in many settings, especially in the rapid diagnosis of emergencies and trauma. Its steep learning curve has favored its widespread use by physicians working in a variety of specialist fields, as well as by other healthcare professionals, such as nurses and paramedics. This trend is also the result of technological advances, which have reduced the costs of ultrasound machines while improving their performance, thereby expanding the range of potential applications.
In light of our findings, thoracic ultrasound assessment of DLET placement prior to initiating one-lung ventilation after DLET intubation can be as specific and sensitive as fiberoptic bronchoscopy, but it is more cost-effective, particularly when performed by a specially trained nurse instead of an anesthesiologist. In our opinion, it is unlikely that thoracic ultrasound will ever completely replace fiberoptic bronchoscopy for this purpose: the direct visualization of DLET position offered by bronchoscopy still has certain advantages. For example, it can facilitate proper positioning of the bronchial lumen cuff relative to the carina or, if a right DLET is being used, it can guide placement of the opening in the right bronchial lumen at the entry of the right upper lobe bronchus.
However, thoracic ultrasound might be considered the method of choice for verifying correct lung exclusion after placement of a left DLET. Fiberoptic bronchoscopy could be used solely as a rescue technique when additional information is needed to resolve doubts or when complications occur.
Conclusions
Although fiberoptic bronchoscopy is still the gold standard for checking the position of a DLET, thoracic ultrasound is a specific, sensitive, cost-effective alternative, which can be used to rapidly verify the proper function of the tube based on the demonstration of correct lung exclusion.
Conflict of interest
The authors, Andrea Saporito, Antonio Lo Piccolo, Daniele Franceschini, Renato Tomasetti, and Luciano Anselmi declare that they have no conflicts of interest relative to this article.
Informed consent
All of the procedures performed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 [5]. All patients provided written informed consent to enrollment in the study and to the inclusion in this article of information that could potentially lead to their identification.
References
- 1.Ahmed S, Janjua S, Ishaq M, Tariq M, Raza H. Double lumen intubation; reliability of the auscultatory method? Professional Med J. 2009;16:105–108. [Google Scholar]
- 2.Karzai W, Schwarzkopf K. Hypoxemia during one lung ventilation: prediction, prevention, and treatment. Anesthesiology. 2009;110:1402–1411. doi: 10.1097/ALN.0b013e31819fb15d. [DOI] [PubMed] [Google Scholar]
- 3.Faber P, Klein A. Theoretical and practical aspects of anaesthesia for thoracic surgery. J Perioper Pract. 2008;18:121–129. doi: 10.1177/175045890801800305. [DOI] [PubMed] [Google Scholar]
- 4.Rowan KR, Kirkpatrick AW, Liu D, Forkheim KE, Mayo JR, Nicolaou S. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT- initial experience. Radiology. 2002;225:210–214. doi: 10.1148/radiol.2251011102. [DOI] [PubMed] [Google Scholar]
- 5.Tocino IM, Miller MH, Frederick PR, Bahr AL, Thomas F. CT detection of occult pneumothoraces in head trauma. Am J Roentgenol. 1984;143:987–990. doi: 10.2214/ajr.143.5.987. [DOI] [PubMed] [Google Scholar]
- 6.Wernecke K, Galanski M, Peters PE, Hansen J. Pneumothorax: evaluation by ultrasound-preliminary results. J Thorac Imag. 1987;2:76–78. doi: 10.1097/00005382-198704000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Lichtenstein D, Meziere G, Biderman P, Gepner A. The ‘‘Lung Point’’: an ultrasound sign specific to pneumothorax. Int Care Med. 2000;26:1434–1440. doi: 10.1007/s001340000627. [DOI] [PubMed] [Google Scholar]
- 8.Zhang M, Liu Z, Yang J, et al. Rapid detection of pneumothorax by ultrasound in patients with multiple trauma. Crit Care. 2006;10:844–849. doi: 10.1186/cc5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12:844–849. doi: 10.1111/j.1553-2712.2005.tb00960.x. [DOI] [PubMed] [Google Scholar]
- 10.Soldati G, Testa A, Pignataro G, et al. The ultrasonographic deep sulcus sign in traumatic pneumothorax. Ultrasound Med Biol. 2006;32:1157–1163. doi: 10.1016/j.ultrasmedbio.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Soldati G, Testa A, Sher S, et al. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest. 2008;133:204–211. doi: 10.1378/chest.07-1595. [DOI] [PubMed] [Google Scholar]
- 12.Jaffer U, McAuley D. Transthoracic ultrasonography to diagnose pneumothorax in trauma. Emerg Med J. 2005;22:504–505. doi: 10.1136/emj.2005.026542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carley S. Is ultrasound or chest X-ray best for the diagnosis of pneumothorax in the emergency department? Emerg Med J. 2009;26:434–435. doi: 10.1136/emj.2009.076216. [DOI] [PubMed] [Google Scholar]
- 14.Chan SSW. Emergency bedside ultrasound to detect pneumothorax. Acad Emerg Med. 2003;10:91–94. doi: 10.1111/j.1553-2712.2003.tb01984.x. [DOI] [PubMed] [Google Scholar]
- 15.Lichtenstein DA, Meziere G, Lascois N, et al. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005;33:1231–1238. doi: 10.1097/01.CCM.0000164542.86954.B4. [DOI] [PubMed] [Google Scholar]
- 16.Kirkpatrick AW, Sirois M, Laupland KB. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the extended focused assessment with sonography for trauma (EFAST) J Trauma. 2004;57:288–295. doi: 10.1097/01.TA.0000133565.88871.E4. [DOI] [PubMed] [Google Scholar]
- 17.American College of Emergency Physicians Policy statement. Emergency ultrasound guidelines. Ann Emerg Med. 2009;53:550–570. doi: 10.1016/j.annemergmed.2008.12.013. [DOI] [PubMed] [Google Scholar]