Abstract
These proceedings will review the role of chelation in five metals—aluminum, cadmium, chromium, cobalt, and uranium—in order to illustrate various chelation concepts. The process of “chelation” can often be oversimplified, leading to incorrect assumptions and risking patient harm. For chelation to be effective, two critical assumptions must be fulfilled: the presumed “metal toxicity” must correlate with a given body or a particular compartment burden, and reducing this compartmental or the body burden (through chelation) attenuates toxicity. Fulfilling these assumptions requires an established dose–response relationship, a validated, reproducible means of toxicity assessment (clinical, biochemical, or radiographical), and an appropriate assessment mechanisms of body or compartment burden. While a metal might “technically” be capable of chelation (and readily demonstrable in urine or feces), this is an insufficient endpoint. Clinical relevance must be affirmed. Deferoxamine is an accepted chelator for appropriately documented aluminum toxicity. There is a very minimal treatment window in order to address chelation in cadmium toxicity. In acute toxicity, while no definitive chelation benefit is described, succimer (DMSA), diethylenetriaminepentaacetate (DTPA), and potentially ethylenediaminetetraacetic acid (EDTA) have been considered. In chronic toxicity, chelation is unsupported. There is little evidence to suggest that currently available chromium chelators are efficacious. Similarly, scant human evidence exists with which to provide recommendation for cobalt chelation. DTPA has been recommended for cobalt radionuclide chelation, although DMSA, EDTA, and N-acetylcysteine have also been suggested. DTPA is unsupported for uranium chelation. Sodium bicarbonate is currently recommended, although animal evidence is conflicting.
Keywords: Aluminum, Cadmium, Chelation, Chromium, Cobalt, Uranium
Introduction
When the terms “toxic element” or “toxic metal” are used, it is important to better characterize precisely what is meant when “detoxification” or “chelating” treatments are discussed. With the noble gases, halogens, and the nonmetals eliminated, as well as the three metals (arsenic, lead, and mercury) already discussed, the task remains to review the role of chelation and the treatment of 88 or so “other” metal poisonings. While all of these elements are characterized in the periodic table of the elements as “metals” (alkali, alkali earth, rare earth, transition, or other metals), such an undertaking would be a facetious proposition. One would actually anticipate finding metals when examining biologic specimens as a consequence of routine diagnostic use—in barium esophagrams, gadolinium MRIs, or nuclear medicine scans with gallium, indium, technetium, thallium, etc. Other metals are encountered therapeutically—aluminum as hydroxide for gastric ulcers and phosphate binding, bismuth as subsalicylate for gastrointestinal disorders, lithium in psychiatry, gold for rheumatological disease, platinum chemotherapy, silver for wound healing, etc.—or taken as dietary supplements. Many of the remaining metals (calcium, chromium, cobalt, copper, iron, manganese, magnesium, molybdenum, potassium, sodium, and zinc) are critical for normal physiology, and it would be undesirable to alter their concentrations excessively. Furthermore, “sodium metal toxicity” or “potassium metal toxicity” more commonly referred to as hypernatremia and hyperkalemia, respectively, require very different strategies than simple “chelation.” These proceedings will review five metals—aluminum, cadmium, chromium, cobalt, and uranium to illustrate various chelation concepts.
General Chelation Considerations
In thinking broadly about chelation, a “reduction to absurdity” or oversimplification occurs with a construct that supposes when a chelator (ligand) is administered: (1) the sole metal of interest is simply “purged” from the organism and (2) this process is entirely beneficial, improving patient symptoms and outcomes absent any adverse effects. In practice, therapy is significantly more complicated. One must determine whether chelation is appropriate for the metal of interest. For this, (at least) two critical assumptions must be fulfilled: the presumed “metal toxicity” correlates with a given body or a particular compartment burden, and that reducing this burden (through chelation) attenuates toxicity. Fulfilling these assumptions rests upon a background of an established dose–response relationship, a validated, reproducible means of toxicity assessment (clinical, biochemical, or radiographical), and an appropriate assessment mechanism of body or compartment burden. While a metal might “technically” be capable of chelation (and readily demonstrable in urine or feces), this is an insufficient endpoint. Clinical relevance must be affirmed. An analogy is drawn from hemodialysis, in which a toxin might be technically “dialyzable,” but a large volume of distribution or other factors would preclude this measure alone from being an adequate gauge of overall hemodialysis efficacy. Similarly, alongside more nuanced assessments of aggressive gastrointestinal decontamination in the field of toxicology, which have more closely evaluated the rationale for such measures [1], an impetus to “get the metal out” at all costs, without considering the mechanism or effects of doing so, does not appropriately encompass a risk–benefit appraisal.
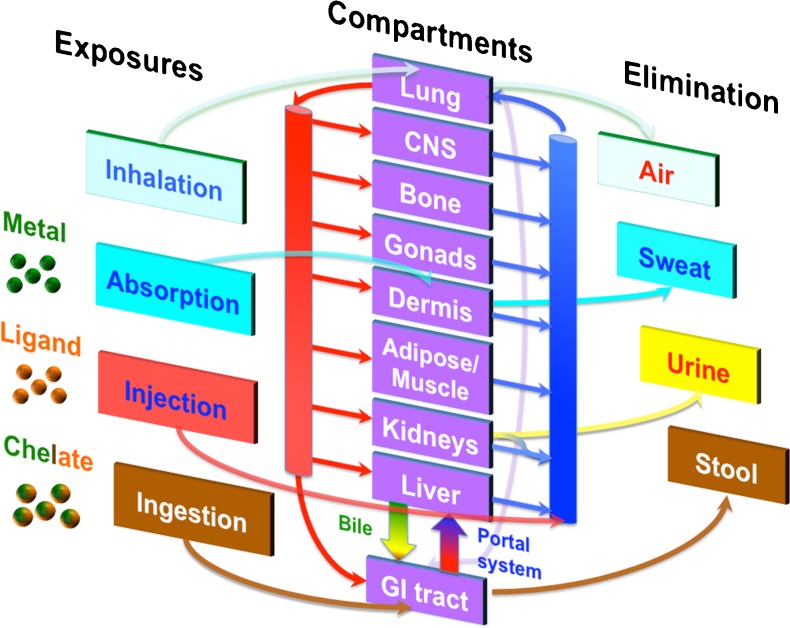
Biochemical and biophysical considerations are important in chelation. Is the metal in an inorganic, elemental, or organic form? What are the binding capacities of various chelators to these different forms? What endogenous chelators (ligands) exist within biological systems? What are the ligand effects in physiologic media (e.g., plasma or bile)? These may differ, and may demonstrate further variability in various target compartments. Additional pharmacokinetic and pharmacodynamic factors impact the toxicity of the metal (ongoing absorption, distribution, metabolism, and excretion); these must be balanced against the exposures, compartment effects, elimination, and toxicities of both the ligand and the chelate (ligand–metal complex) (Fig. 1). While hydrophilic chelators enhance renal excretion, their mainly extracellular localization limits activity to extracellular metal pools; lipophilic chelators might access and decrease intracellular stores, but may redistribute toxic metals to vulnerable compartments [2]. This may create a fundamental efficacy–safety paradox: the more lipophilic a chelator, the better its “clearing efficiency”; however, the more lipophilic the chelator, the greater its toxicity [3]. Thus, in an aggressive attempt to “mobilize” a metal from one target compartment in order to effect excretion, chelation might facilitate translocation of the metal to other organs. For example, British anti-lewisite (BAL, 2,3-dimercaptopropanol) administered for arsenic or mercury poisoning has worsened brain concentrations in experimental models [4, 5]. Furthermore, continuous exposure of the kidneys to a metal or chelate, which is filterable but reabsorbable, may induce nephrotoxicity, even though some measure of urinary excretion may be achieved and measured. Similarly, enterohepatic circulation might promote ongoing gastrointestinal exposure to a metal, ligand, or chelate in cases where fecal elimination is intended. These factors must inform a fundamental understanding of chelation effects regarding decorporation versus redistribution.
Fig. 1.
Pharmacokinetic considerations in chelation. The various effects of absorption, distribution, metabolism, and elimination must be considered for the metal, the ligand (including endogenous ligands), and the chelate as part of an evaluation of efficacy and toxicity
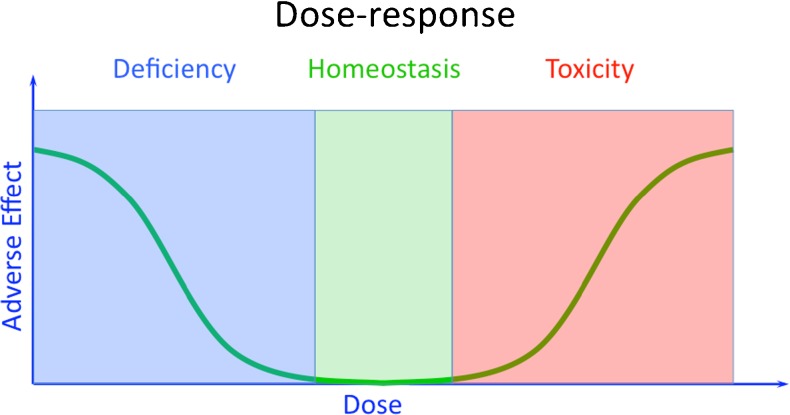
Separately, is chelation going to engender “bycatch”? A term appropriated from the fishing industry, “bycatch occurs if a fishing method is not perfectly selective….A fishing method is perfectly selective if it results in the catch and retention only of the desired size, sex, quality, and quantity of target species without other fishing-related mortality. Very few fishing methods meet this criterion” [6]. For example, fish “caught” on a line would need to be “released” (hopefully without any attendant harm) if they were protected species, juveniles, or out of season. Nets may snare marine mammals or birds. As applied to chelation therapy, bycatch occurs if a chelation method is not perfectly selective. A chelation method is perfectly selective if it results in the chelation and elimination only of the desired metal in its toxic form (metal speciation) in sufficient quantity of this target metal, without other chelation-related morbidity or mortality. Very few, if any, chelation methods meet this criterion. Toxicologists are frequently concerned with the right (toxicity) side of a nonmonotonic (hormetic, “U-shaped”) dose–response curve (Fig. 2), where greater concentrations yield greater toxicity, and lower concentrations yield less toxicity. However, if an essential metal targeted for chelation or a metal or other required nutrient is subject to “bycatch” and brought below a certain threshold concentration, harm can result from entering a deficiency state (left side of the curve). For example, the hierarchy of ethylenediaminetetraacetic acid (EDTA) relative binding affinities for metals is Cr2+ > Fe3+ > Cu2+ > Pb2+ > Zn2+ > Cd2+ > Co2+ > Fe2+ > Mn2+ > Ca2+ > Mg2+ [7]. This would place essential metals such as zinc, copper, and iron at risk for deficiency during a course of chelation. Single or combined deficiency of other essential metals might result in symptoms misattributed to the original “metal poisoning.”
Fig. 2.
A nonmonotonic dose–response curve. Both deficiency and excess may produce an adverse event
Specific Metals
Aluminum
Exposures
Aluminum exposures are ubiquitous, including in food and drinking water [8]. Aluminum is the third most abundant element in the Earth’s crust. Individuals applying antiperspirant have likely been aluminum “exposed.” A significant controversy arose regarding aluminum exposure (including via antiperspirants) and the risk of neurodegenerative disease (Alzheimer’s disease) [9, 10]. Original authors of this association later reported that it was potentially due to signal misinterpretation of other metals such as iron as aluminum, and they felt it unlikely that aluminum represented an etiologic cause of Alzheimer’s disease [11]. While some studies reported an association between breast cancer diagnosis related to more frequent use of antiperspirants/deodorants and underarm shaving, the National Cancer Institute declared there is “no conclusive research linking the use of underarm antiperspirants or deodorants and the subsequent development of breast cancer” [12]. Much of our experience with aluminum toxicity comes from renal failure patients, with aluminum exposure from phosphate binders and dialysate fluids [13]. Patients may also be exposed during treatment for bladder hemorrhage. Alum (aluminum potassium sulfate), known for its styptic and astringent properties, replaced phenol, formalin, and silver nitrate, which had their own significant toxicities [14, 15]. Total parenteral nutrition (TPN) provides an additional iatrogenic route of exposure. This is of concern in pediatric patients (particularly neonates) due to immature renal function, increased requirements of calcium and phosphorus, and smaller volumes of distribution [16]. A number of reports demonstrated how easily preparations in hospital pharmacies could introduce significant aluminum into TPN-containing solutions, which ultimately prompted federal action [17]. There are also case reports of patients with aluminum toxicity through drug abuse (e.g., boiling methadone in aluminum containing pots) [18]. Alum is an approved vaccination adjuvant.
Toxicity
There are well-defined, aluminum-associated multisystem organ toxicities, including so-called “dialysis dementia” (dialysis encephalopathy) [19]. This manifests as speech, cognitive, and occasional motor disorders. Consequential metabolic bone disease and dialysis-related bone disease (osteomalacia) may manifest as diffuse bone pain, muscle weakness, and spontaneous fractures [20]. Pediatric patients may present with osteopenia, fractures, and rickets [16]. Aluminum-associated anemia may be particularly refractory to therapy with iron and erythropoietin [21, 22]. In severe aluminum-associated dialysis cases, cardiomyopathy and cardiac failure are described, with aluminum deposits detectible within cardiac myocyte lysosomes [23].
For dialysis patients in whom aluminum-associated disease was of most concern, decade-old National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF KDOQI) guidelines opined that baseline aluminum should be <20 μg/L, that DFO testing should occur in the setting of elevated serum aluminum concentrations (60 to 200 μg/L), and that symptomatic patients with serum aluminum levels >60 g/L but <200 g/L, or a rise of aluminum after DFO of >50 g/L, should be provided DFO to treat the “aluminum overload” [24]. These guidelines have been called into question due to the lack of correlation between definitively “positive” aluminum concentrations (even at serum levels of 290 ± 7 μg/L), “positive” DFO test results (mean increment, 192 μg/L), and aluminum-associated osteomalacia [25]. More recent Kidney Disease Improving Global Outcomes guidelines for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease mineral and bone disorders neglected aluminum testing, chelation, and DFO, and adhered to KDOQI recommendations regarding bone biopsy for diagnosis of aluminum-associated bone disease [26]. Occupational exposure limits have also been suggested or created as standards to limit aluminum “potroom asthma” and pulmonary fibrosis, which would present with clinical symptoms and/or pulmonary function testing abnormalities [27–29]. Occupational asthma is not chelated.
Aluminum Chelators and Chelation Considerations
Deferoxamine (DFO), isolated from Streptomyces pilosus, is the fairly well-established aluminum chelator. DFO (C25H48N6O8; MW, 560.68) has an affinity for ferric iron almost nine orders of magnitude above that of aluminum (iron’s stability constant of 1031 vs. aluminum’s 1022) [30]. As the stability constants for calcium (102), copper (1014), nickel (1010), magnesium (104), and zinc (1011) are orders of magnitude lower, this makes it a relatively specific complexing agent [30]. However, in administrating DFO, a number of different factors must be considered. First, DFO has a significant affinity to iron, risking deficiency. Second, serum-binding proteins might affect efficacy, particularly transferrrin. DFO is incapable of removing iron from transferrin completely [30]. Similarly, aluminum already bound to transferrin is extremely difficult to eliminate. It is well established that despite DFO administration, if aluminum is bound to transferrin, it is neither dialyzable nor accessible to DFO [31]. One study found that only 1 % of all available serum aluminum was chelated as aluminoxamine (AlO), highlighting the importance of transferrin and other endogenous binding proteins [32]. Third, the potential toxicities of the unbound DFO chelator, as well as the toxicities of both chelates—AlO and ferrioxamine (FO)—must be anticipated. AlO and FO following DFO administration may persist for long periods, especially in kidney disease [32, 33].
Acute or chronic exposure will normally be evident from the clinical scenario. Is the patient dialysis dependent, who has built-up aluminum over a longer period of time, or is an acute exposure present, most commonly seen in alum administration for hemorrhagic cystitis? DFO is well described to precipitate aluminum encephalopathy as well as death in patients who are dialysis-dependent [34–36]. The mechanism is thought to be due to either DFO redistribution of mobilized aluminum to brain or the ability of the ALO-complex to cross the blood brain barrier. DFO also can cross the blood–brain barrier to then chelate aluminum, such that the ALO-complex can then be found in CSF [31]. Therefore, a number of different mechanisms exist for this real and severe toxicity.
An acute or chronic scenario and desire to minimize precipitating encephalopathy thus affect DFO dosing. Chronic dialysis patients receive DFO 5 mg/kg (or sometimes lower doses) over 1 hour, prior to a subsequent scheduled dialysis session; higher doses are used with acute exposure (e.g., 15 mg kg−1 day−1) [24]. Other DFO risks include hyperparathyroidism (potentially due to mitigation of the inhibitory effect of aluminium on parathyroid gland function upon chelation), hypocalcemia (postulated to occur due to permissive increase in bone calcium uptake following aluminum chelation), and decreased ferritin (secondary to DFO’s ferric iron-chelating effects) [37–39]. Systemic hypersensitivity reactions, adult respiratory distress syndrome, and infectious complications, specifically Mucor and Yersinia invasion, are also reported [31, 40, 41]. An additional consideration is the timing of chelation. In dialysis patients, it may take 6–8 h to have the chelate ALO appear in significant quantities in the serum [32]. For this reason, DFO is normally given at the end of dialysis prior to the next dialysis session [42, 43]. In patients who are acutely exposed and toxic with aluminum, this may influence timing considerations for adjunctive dialysis after DFO is provided [15, 44].
Other potential aluminum chelators have been considered. However, while deferiprone and deferasirox are attractive as existing agents approved for iron chelation, they are unapproved for aluminum toxicity, and incompletely evaluated [45–47]. One potential hazard might involve stoichiometry. The deferiprone compound requires a 3:1 molar ratio to form a stable, water-soluble complex with antioxidant activity, while deferasirox requires 2:1 molar ratio. Lower concentrations of deferiprone generate incomplete 1:1 and 1:2 chelator-iron complexes, with unoccupied coordination sites that can paradoxically catalyze the formation of hydroxyl radicals and other reactive oxygen species [48]. A similar concern might attend incomplete deferiprone aluminum complexes. Both deferiprone and deferasirox chelate copper and zinc and could potentially induce harm through deficiency of these trace essential nutrients. Other risks include agranulocytosis, renal failure, hepatic impairment (including hepatic fibrosis and frank failure), and gastrointestinal hemorrhage [49, 50].
Section Summary
The accepted chelator for appropriately documented aluminum toxicity is DFO. Of note, DFO’s labeled indication is acute iron intoxication and chronic iron overload. DFO demonstrates evidence of both technical efficacy (elimination can be achieved), as well as clinical efficacy (this elimination effects a clinical difference), particularly for aluminum associated bone disease in dialysis patients [37, 51–53]. Potential worsening of aluminum toxicity, including death, may occur with DFO administration, and the ability to eliminate the AlO chelate must be considered. While this is less of a concern in patients with normal renal function, it is critical in dialysis-dependent patients.
Cadmium
Exposures
Virtually all soil, rock, and water contain cadmium. Cadmium is present in most foods, with broad variation in concentrations. Although oral bioavailability of ingested cadmium is poor [54], local soil contaminant conditions, soil-to-plant transference, and use of cadmium-containing fertilizers might lead to higher overall oral cadmium dietary exposure [55]. Exposure may also occur in industry through such tasks as mining, refining (particularly as a by-product of zinc processing), and metalworking. Inhalational absorption is excellent, presenting a particular occupational hazard. Tobacco naturally accumulates relatively high concentrations of cadmium in its leaves, a significant risk for smokers [56]. Cadmium accumulates in both the hepatic and renal systems, and it has a half-life elimination on the order of years.
Toxicity
Significant renal injury with a proximal tubular distribution is well described, as well as a painful, debilitating bone disease. Metallothionein binds cadmium for storage. However, the cadmium–metallothionein complex can be released, filtered, reabsorbed, and concentrated in the proximal tubules, where metallothionein is degraded in lysosomes to release free cadmium [54]. This leads to alterations in cell–cell adhesion and cell signaling, increased excretion of low molecular weight proteins such as beta2-microglobulin early in kidney disease, and ultimately, chronic renal dysfunction [57]. The intolerably painful, so-called “ouch ouch disease” (“itai-itai byō”) is due to osteomalacia and fractures secondary to insufficient mineralization [58, 59]. Cadmium inhalation can cause respiratory tract disease through inhalation and fibrosis. This inhalational disease can progress, making cadmium atypical of other metal fume fevers [60, 61]. Cadmium and cadmium compounds are classified as International Agency for Research on Cancer (IARC) class 1 carcinogens [56].
Acute cadmium toxicity is rare. It typically follows pulmonary occupational exposure and is generally recognized on clinical grounds (with subsequent environmental or biological confirmation). Acute chemical pneumonitis, pulmonary edema, and failure of the kidneys, liver, and other organs are reported [62–65]. Acute oral exposure would precipitate gastrointestinal symptoms (nausea, emesis, diarrhea, and abdominal pain) [66]. As urinary cadmium levels do not rise significantly after acute exposure [54], they are not useful to obtain in the acute setting. Medical surveillance for chronic disease (particularly from occupational burden) is normally assessed through monitoring of low-molecular-weight biomarker proteins such as beta2-microglobulin standardized to grams of creatinine (g/Cr), urine cadmium (standardized to grams of creatinine), and/or blood cadmium (standardized to liters of whole blood), or other markers such as urinary metallothionein. Specific trigger levels and recommended actions are available elsewhere [67, 68].
Cadmium Chelators and Chelation Considerations
Several aspects must be considered when discussing chelation of cadmium. Essentially all plasma cadmium is bound to proteins or other molecules [57]. These endogenous ligands, with which administered chelators must compete, include albumin, macroglobulin, and metallothionein. In fact, some investigators have considered induction of metallothionein as a preventative measure for cadmium toxicity, although this mobilization may simply increase renal exposure [69, 70]. Numerous chelators have been tried, as well as numerous chelates resulting from these combinations. In humans, dimercaptopropane-1-sulfonic acid (DMPS) increased cadmium excretion in “mobilization tests” in healthy individuals [71]. However, cadmium concentrations in the blood did not change. EDTA was of no benefit in chronic cadmium-induced renal dysfunction [72]. This study was important because it provided 14-year follow-up of multiple patients. It provides a useful counterweight to isolated case reports, which offer a suggestion of benefit, such as one in which Ca2+EDTA and glutathione were provided as treatment [73]. Despite no change in clinical objective measures and potential worsening of redistribution due to increased blood cadmium concentrations following glutathione addition to therapy, the manuscript announced, “the patient was comforted by the fact that the cadmium was being eliminated from his body.” This underscores the fundamental misunderstanding of, and potentially dangerous psychological attraction to chelation highlighted in the section regarding general chelation considerations—demonstrating the presence of metal in excreta does not unto itself equal efficacy nor safety from adverse redistribution. Increased urinary elimination by EDTA in another single case was again complicated by methodological limitations [7].
The animal experience has been quite vast, under varying experimental conditions. Efficacy of chelation for cadmium is markedly time dependent [74–77]. Provision as “late” as 2 hours or more had the potential for absent effect. Acyclic polyamines were harmful, producing significant renal damage [78]. BAL increased renal [74] and hepatic cadmium burden [79], decreased survival [80], and enhanced nephrotoxicity [81]. The carbodithioates have been extensively evaluated and would be worthy of a review unto themselves. Carbodithioates’ outcomes were highly dependent upon the given agent and experimental conditions. Some were beneficial; others are quiet harmful in terms of redistributing cadmium to areas of concern, specifically the testes, the kidneys, and the brain [76, 82–85]. DMPS seemed to increase cadmium burden [74, 80]. Succimer (DMSA) improved survival [80], modestly decreased cadmium retention [75, 86], and provided dose-dependent survival benefit, although with increased renal burden [76]. Along with diethylenetriaminepentaacetate (DTPA), which yielded dose-dependent increased survival [76], decreased cadmium retention [75], and decreased residual cadmium [78], DMSA is probably the chelator that has shown the most benefit in animal models. d-Penicillamine was variously shown to increase renal cadmium burden [80], produce no survival benefit [76], and demonstrate lack of efficacy [87]. Although EDTA increased survival at some lower cadmium doses [88], it has been noted to increase renal cadmium burden [79] and renal damage [78]. N-Acetylcysteine (NAC) administration improved oxidative stress markers with a concomitant chelator, monoisoamyl 2,3-dimercaptosuccinate [89].
Section Summary
Source control of cadmium remains paramount. There is a very minimal treatment window in order to address cadmium toxicity. In acute toxicity, while no definitive chelation benefit is described, practitioners have considered DMSA, DTPA, and potentially EDTA. In chronic toxicity, chelation is unsupported, which is consistent with the Agency for Toxic Substances and Disease Registry (ATSDR) guidelines for cadmium [54]. The carbodithioates are entirely experimental.
Chromium
Exposures
Chromium presents a number of mechanisms for exposure. Chromium is an essential nutrient. It is involved in carbohydrate and lipid metabolism through ways that are not fully elucidated, but involve insulin receptor effects and insulin potentiation [90]. For this reason, it is popular as a supplement. Chromium is present in food and water and remains a concern with copper/chromate/arsenate pressure-treated wood, which still lingers in outdoor residential settings and playgrounds [91]. Chromium is used industrially as well as biomedically in cardiac stents. The most recent controversy has come from its use in metal-on-metal hip implants and other arthroplasties [92].
The kinetics are different depending on chromium species. Trivalent chromium (Cr3+) salts have very limited oral absorption (0.4–2.5 %), and almost 98 % is eliminated fecally following oral exposure [93]. Urinary elimination following oral absorption is rapid. Dermal absorption is poor as long as the skin is not disrupted [94]. Cellular entry is through diffusion. Hexavalent chromium (Cr6+) is particularly toxic, acting as a powerful oxidizing agent. Endogenous gastrointestinal reducing agents successfully reduce hexavalent chromium to the trivalent form prior to absorption [95]. However, overall, chromium(VI) does have a greater absorption, and it enters the cell through facilitated cellular uptake, a different mechanism than diffusion, to concentrate in liver, kidney, spleen, soft tissues, and bone. Increased chromium excretion occurs in response to stress, exercise, glucose loads, as well as in patients who have insulin resistance [96]. Pulmonary kinetics are complex, depending on exposure to a soluble or insoluble compound. Chromium(VI) trioxide (chromic acid) and soluble chromium(VI) salt aerosols may produce different health effects than insoluble particulate compounds. For example, exposure to chromium(VI) trioxide results in marked damage to the nasal mucosa and perforation of the nasal septum (so-called “chrome ulcers”), whereas exposure to insoluble(VI) compounds results in damage to the lower respiratory tract.
Toxicity
Toxicity is well described. Chromium(VI) induces a variety of DNA lesions such as single-strand breaks, alkali-labile sites, and DNA protein cross-links [97]. For this reason, and its association with both stomach as well as lung cancer, it is designated an IARC group I carcinogen [98]. Respiratory irritation and compromise from pulmonary inhalation may occur. Dermal effects include “blackjack dermatitis” from chromium containing compounds used in the felt tabletop—sensitization occurs through type I (immediate onset, IgE-mediated) and type IV (delayed, cell-mediated) mechanisms [93]—and “chrome holes,” ulcers, or sores. Ingestion is associated with significant gastrointestinal irritation, ulceration, and hemorrhage. Oligospermia, anemia, and hemolysis are also described.
Unfortunately, there is no clear correlation between measured blood and urine chromium concentrations and physiologic effects. In fact, ATSDR specifically advises that “increases in blood and urine chromium levels cannot be used to predict the kind of health effects that might develop from that exposure” [93]. Furthermore, common blood tube anticoagulants such as sodium citrate and sodium heparin increase chromium partitioning into erythrocytes, while EDTA (as an anticoagulant used to stabilize the blood tube) lowers partitioning into erythrocytes [99]. This may lead to misleading results and interpretations of the more commonly used plasma or serum concentrations. Diagnosis of chromium metal toxicity will thus rest on clinical manifestations. Acute, generally higher-level exposures are consistent with the source: gastrointestinal (GI) corrosion and multisystem failure following ingestion, and surface burns and potential systemic symptoms occur with dermal contact [100–102]. Chronic exposure is normally low-level and directed at the pulmonary system and respiratory symptoms [93].
Chromium Chelators and Chelation Considerations
Chromium(VI) is particularly problematic as a toxic exposure. It probable acts following reduction to chromium(V) intermediate species, which can generate reactive oxygen species (ROS) through a Fenton-like reaction [97]. Treatment strategies could then approach two potential mechanisms. Either chromium(VI) would require successful chelation, or sufficient reductants must be provided in order to achieve chromium(III) safely and avoid ROS production. Several such strategies have been evaluated in humans. Many of these are provided as case reports of patients who ingested chrome salts or were exposed in industry or via prostheses. BAL essentially has no effect on chromium elimination [100, 103]. EDTA yielded essentially uninterpretable increases in urinary elimination over 48 hours in one study that was significantly methodologically compromised [104]. Two other reports utilizing EDTA failed to show any benefit in increasing urinary elimination [105, 106]. A DMPS challenge failed to show any increase in chromium excretion [107]. As adjuvant therapy in patients who were exposed, NAC did not demonstrate any particular benefit, although it was without apparent toxicity [102, 108].
What else can be attempted in an ill, exposed patient? Exchange transfusion is extremely heroic, but might have some benefit [101]. The data regarding the effectiveness of hemodialysis are mixed; it also may be instituted for concurrent renal failure [101, 102, 109, 110]. Ascorbic acid has been added as a nonspecific antioxidant in addition to multiple therapeutic measures, making determination of its individual contribution difficult in humans [101, 108].
Animal experiments have evaluated a range of agents. Ascorbic acid appears to have time-dependent mortality benefits. Given early, it appears to show a benefit; provision only 3 hours later showed harm [111]. Theoretically, ascorbate could precipitate acute oxalate nephropathy. The use of alpha-lipoic acid resulted in no change in urinary clearance [112]. BAL has generally been unsubstantiated in having any benefit in increasing either urinary or fecal clearance [100, 112]. While DFO appeared promising in a pre-exposure model, in a post-exposure model, it was entirely ineffective [113]. d-Penicillamine decreased excretion and was actually harmful in terms of urinary clearance [112]. EDTA showed no benefit [112]. In one animal study, which is particularly referenced, NAC did show an increase in urinary chromium clearance. Of note, this was not due to any increase in concentration in the urine, but rather due to maintenance of the critical factors of adequate urine volume and output [114]. NAC did reduce chromium hypersensitivity dermatological reaction [115].
Section Summary
Significant chromium species differences exist. Reducing ongoing exposure to any chromium source must be rigorously addressed in the setting of chromium toxicity. There is little evidence to suggest that currently available chelators are efficacious. NAC could be considered on the basis of anecdotal human use and limited animal evaluation. It does have a familiar risk/benefit profile. Ascorbic acid has anecdotal human use. However, it also has the potential for a time-dependent risk–benefit profile: late administration could potentially cause harm and therefore is generally not recommended.
Cobalt
Exposures
Cobalt is an essential nutrient in the form of vitamin B12 (cobalamin), warding off pernicious anemia. Widely available in our environment as well as industry (e.g., in cemented tungsten carbide, as a pigment catalyst, and an aid in polishing), cobalt is also used in biomedical therapy and research. Cobalt has recently arisen as an issue with metal prostheses, due to the production of wear debris, which may produce systemic symptoms and reported death [116–119]. Cobalt is provided as an antidote for cyanide poisoning (as hydroxocobalamin). It was historically an antidote for anemia in a product called Roncovite, a cobalt and iron combination [120].
Cobalt gastrointestinal absorption is extremely variable, dependent upon iron status and age. Dermal absorption depends on disrupted dermal integrity. There is hepatic accumulation, as well as red blood cell uptake (binding to the globin moiety of hemoglobin), which may affect monitoring [121]. Urinary cobalt determinations may better reflect the extent of occupational exposures [122]. Oral exposure does lead to fecal elimination, dependent upon variable gastrointestinal absorption. Cobalt provided parenterally is primarily eliminated in urine. In pulmonary exposure, soluble cobalt has the potential to remain in the lungs for potentially extended periods of time.
Toxicity
Respiratory exposure to cobalt dusts can lead to the well described “hard metal” or “diamond polishers” pulmonary disease [123]. “Cobalt asthma” and ultimately fibrosis from “hard metal disease” may persist and progress despite cessation of occupational exposure [123, 124]. “Beer drinkers’ cardiomyopathy” is so named due to the recognition of heart failure and pericardial effusion in consumers of beer containing cobalt added as a foam-head stabilizer [125, 126]. Associated thyroid disease included both thyromegaly and hypothyroidism [127]. Neuropathy has also been described, as well as dermatitis and hypersensitivity type reactions [128]. Cobalt induces polycythemia (by stabilizing the transcriptional activator hypoxia-inducible factor to mimic hypoxia and stimulate erythropoietin production); this was the basis for its previous therapeutic use as Roncovite [129].
The US Food and Drug Administration (FDA) and the UK Medicines and Healthcare Products Regulatory Agency (MHPRA) diverge in their recommendations for cobalt metal testing in patients with metal-on-metal (MOM) hips, with the FDA unconvinced of a correlation between a metal ion concentration and the need for revision surgery [130]. MHPRA specifically recommends blood metal ion concentration testing in painful MOM hip replacements, in all asymptomatic DePuy ASR™ hip replacements, and in asymptomatic stemmed MOM hip replacements with femoral head diameters ≥36 mm [131]. A second test is advised 3 months after the first if ion concentrations exceed seven parts per billion, and revision is to be considered if imaging is abnormal and/or blood metal ion levels are rising [131].
One significant issue complicating assessment of cobalt toxicity is the fact that “toxic” concentrations of cobalt in urine and blood are not well defined [127]. National, population-based, representative biomonitoring data are available from the Centers for Disease Control; the most recent geometric mean urine cobalt concentration was 0.369 μg/L (95 % CI, 0.341–0.398 μg/L) [132]. No effect was described in thyroid or red blood cell parameters in occupational setting with blood cobalt concentrations up to 3.20 μg/dL and urinary cobalt concentrations up to 204.30 μg/g creatinine [133]. Cobalt erythrocyte uptake is also practically irreversibly [121]. The FDA advised as part of the MOM controversy that “no commercially available standardized tests to assess metal-ion levels” exist [130]. The highest cobalt urinary excretion occurs during the first 24 h after short-term exposure, and therefore, rapid testing would be required to document acute exposure [124]. Clinical findings or diagnostic testing abnormalities consistent with a documented route of exposure should support a diagnosis of cobalt toxicity, although these may be nonspecific (e.g., cardiomyopathy, pulmonary function abnormalities in cobalt lung disease, thyroid dysfunction, patch testing for sensitization, etc.). Further cobalt health and safety information are available from other resources [134].
Cobalt Chelators and Chelation Considerations
Despite the aforementioned limitations of cobalt testing and interpretation, EDTA has been the predominant chelator in limited human experience. It was used as adjuvant therapy in a case in which a prosthetic hip was leaching cobalt. It did provide short-term lowering of blood cobalt measurements; however, cobalt concentrations rebounded in a matter of days [105]. The key to treatment was to remove the deteriorated hip prosthesis that was the source of the cobalt exposure. Similarly, gastric decontamination of GI cobalt sources in oral ingestions would take on a primary role prior to chelation. In a pediatric case following ingestion of several magnets, CaNa2EDTA yielded a fourfold increase in urinary cobalt excretion, as well as clinical benefit [135]. One additional study demonstrated a small, nonsignificant increase in cobalt excretion. However, EDTA itself and cobalt were both present in the chelation admixture, making cobalt excretion almost impossible to interpret [7].
Animal studies have evaluated NAC, copper chelators (d-penicillamine and trientine), and others. Experimental studies in animals highlight the importance of metal exposure route and formulation (e.g., oral or intraperitoneal) and also the fact that the chelate itself can be potentially toxic. In one study evaluating NAC, l-cysteine, and l-methionine, l-methionine complexed to cobalt chloride (CoCl2) prior to administration actually induced mortality, which was not seen with cobalt chelated to NAC or l-cysteine [136]. Again, this emphasizes that although a compound is chelated, it might be able to dissociate, or the chelate itself could be harmful. Another murine study confirmed a lack of toxicity of a NAC–CoCl2 chelate, the lack of benefit of oral NAC after an oral LD50 dose of cobalt chloride (2.28 mmol/kg), and a mortality reduction from 45 % to 30 % with immediate postexposure provision of intraperitoneal NAC [137]. Following promising preliminary studies of EDTA in rats [138], more comprehensive testing was performed. At CoCl2 doses approximating its LD99, l-cysteine, NAC, glutathione, DMSA, DTPA, and EDTA were determined to be most effective [139]. EDTA, DTPA, and NAC were the most effective (100, 70, and 50 % survival, respectively) in follow-up studies at CoCl2 doses well above the LD99; however, this required chelator dosing at approximately one quarter of their own of LD50s [139]. Following chronic exposure to CoCl2, only NAC reduced tissue cobalt concentrations in liver and spleen [140]. A gap in animal research was readdressed due to concern for security threats from radioactive cobalt. Intravenous l-glutathione (GSH) and l-cysteine (Cys) seemed to show a benefit in 60Co elimination following intravenous exposure [141]. d-Penicillamine and trientine were administered at roughly human-equivalent dosing. d-Penicillamine failed to show benefit, while trientine increased cobalt blood levels and elimination without lowering kidney, liver, muscle, lung, spleen, stomach, or intestine tissue concentrations [142]. When significantly higher d-penicillamine and trientine doses were provided, single dose d-penicillamine increased elimination, while trientine produced significant redistribution [143]. Overall, relatively low amounts of cobalt were chelated. Application to humans is limited by the different chelator dosing routes.
Section Summary
In summary, identification of organ system toxicity attributable to cobalt, and addressing and eliminating the cobalt source are critical. There is little human evidence with which to provide recommendation for cobalt chelation. The National Council on Radiation Protection and Measurements and the Radiation Emergency Assistance Center/Training Site recommend DTPA for cobalt radionuclide chelation, although they also indicate that DMSA (succimer), EDTA, and NAC can be considered [144, 145]. For nonradiologic exposure, other sources suggest that both NAC and EDTA can be considered, without definitive recommendation.
Uranium
Exposures
Uranium is present naturally in virtually all soil, rock, and water. Significant exposure may occur through environmental remediation of soil, mine, or waste contaminated with uranium, industrial milling, mining, and refining uranium, and in nuclear fuel fabrication and processing [146]. This topic has become a significant issue of late in military conflict, whether that is from depleted uranium (DU) munitions assembly, combat where DU was employed, DU shrapnel exposure, or fighting fires in vehicles struck with DU, which may generate uranium dust.
Uranium exposure in the natural environment occurs most commonly via the oral route from contaminated food or drinking water [147]. Uranium has poor absorption when ingested (<0.1–6 %) [148]. Inhalation, the primary occupational exposure route, results in pulmonary retention lasting from weeks to years, depending upon the solubility of the uranium compound. DU shrapnel has been a concern, due to persistence and prolonged renal exposure via elimination [149]. Some accumulation occurs in skeletal, renal, and hepatic locations. Elimination is >50 % within 24 h following parenteral exposure, and there is significant fecal elimination after oral exposure.
Toxicity
Uranium itself is classified as group 3 (not classifiable as to carcinogenicity in humans) by IARC. The exposure of concern is radon, a daughter isotope (decay product). Thus, while 238U, 235U, and 234U are radioactive, their half-lives are on the order of billions, millions, and thousands of years (respectively), making them primarily chemical toxicants. This mitigates considerations as to the uranium source (e.g., natural, depleted, or enriched), as the chemical toxicities of uranium species and forms with variant isotopic ratios are identical.
Hexavalent uranium U(VI), as the dioxo uranyl cation [UO2]2+, is the most stable state in vivo [150, 151]. This creates some stereo-chemical hindrance to chelation. It is a water-soluble, renal tubular epithelial toxin, at a mostly proximal site [152]. If inhaled, significant respiratory irritation may occur, as well as hepatic dysfunction, anemia, and myocarditis.
The Environmental Protection Agency (EPA), under the Safe Drinking Water Act, limits uranium to 30 μg/L in drinking water [153]. Under the Clean Air Act, the EPA standard for the maximum radiation dose to an individual from airborne uranium is 10 mrem. Occupationally, because soluble uranium compounds are absorbed significantly more than insoluble forms, the Occupational Safety and Health Administration permissible exposure level for airborne soluble uranium in the workplace is five times lower than that for insoluble uranium at 0.05 mg/m3 as a time-weighted average (average exposure in any 8-h work shift of a 40-h work week) [154]. The US Nuclear Regulatory Commission action level is 15 μg/L urinary uranium for occupational exposure [155]. The US population geometric mean urine uranium concentration (absolute and creatinine corrected) was 0.007 μg/L (95 % CI, 0.006–0.008 μg/L) in 2009–2010 [132]. By comparison, a series of US soldiers who may have been exposed to DU by inhalation, ingestion, or wound contamination, but without embedded shrapnel, had mean urinary uranium concentrations of 0.066 μg/g creatinine, much lower than those with embedded DU shrapnel (median urinary uranium concentrations of 2.61 μg/g creatinine) [156]. Despite DU shrapnel persistence and long-term ongoing urinary elimination, renal dysfunction or cellular toxicity have been unimpressive [149].
Diagnostic considerations for uranium metal toxicity focus on clinical and laboratory assessments for nephrotoxicity. Detectable urinary uranium does not directly imply causation of an adverse health effect, and most naturally occurring uranium exposures do not warrant monitoring or treatment [147]. Acute uranium exposure and sequelae are evaluated through measurement of urine uranium concentrations and markers of renal toxicity (urinary catalase, proteinuria, aminoaciduria, alkaline phosphatase, and clearance of beta2-microglobulin relative to creatinine) [148]. As the majority of uranium is rapidly cleared, high urinary uranium concentrations (>100 μg/L) reflect current or recent exposures, while lower concentrations (<40 μg/L) most likely represent past exposures or typical background exposures [147]. The Radiation Emergency Assistance Center/Training Site at the Oak Ridge Institute for Science and Education is available to consultation for medical management in radiological materials incidents (865-576-1005) [157].
Uranium Chelators and Chelation Considerations
Research on uranium(VI) solubility and speciation highlights the importance of considering the effects of various physiologic media. Uranium solubility and speciation vary markedly between biological fluids (bile, interstitial, and other human biological sources) due to differences in fluid composition, ionic strength, pH, and starting concentrations, and the contribution of hydroxide, phosphate, and carbonate forms [158]. Weak binding to albumin as well as transferrin and other plasma proteins occurs.
Calcium trisodium and zinc trisodium DTPA were evaluated in many cases because DTPA was used in treatment of human mixed oxide exposures, which contained plutonium as well as uranium oxide. As DTPA has negligible GI absorption, it must be administered parenterally. DTPA is cleared by glomerular filtration. Unfortunately, DTPA has not demonstrated any benefit at all in enhancing uranium clearance [3]. In fact, the package inserts for both calcium DTPA and zinc DPTA state that “treatments are not expected to be effective for uranium and neptunium” [159, 160]. This is based on a fairly large body of literature. DTPA is nephrotoxic, teratogenic, embryotoxic, and associated with suppressed hematopoiesis [50]. DPTA is associated with significant bycatch of numerous other endogenous substances (calcium, zinc, magnesium, manganese, and metalloproteinase depletion).
In porcine models, uranium DTPA caused instant cardiac arrest [161]. This was felt to be due to calcium bycatch because animals provided calcium did not similarly succumb. Numerous other animal models have shown increased urinary elimination of calcium, copper, iron, zinc, and manganese, and concomitant inter-tissue distribution as opposed to decorporation [162–164]. Tiron (tiferron) has been evaluated as a potential chelator. It achieved a favorable removal of uranium, but this was limited by the large molar ratios required (2:1 molar ratios), which limited its practical value [151, 165]. The hydroxypyridonates (HOPOs) are either a tetradentate or ocatadentate chelators of uranium that have shown some promise in animal models [166–168]. Animal studies regarding efficacy must be interpreted in light of fed or fasting state [151], although in comparison to DTPA, the HOPOs show significant ability to decorporate uranium. The potentially beneficial effects of sodium bicarbonate were reported in 1916 in dogs [169]. Alkaline urine precludes dissociation of the uranium-bicarbonate complex, such that the renal tubular epithelium is protected from reactive uranyl ion exposure [147]. Although later studies cast doubt on sodium bicarbonate efficacy [170], it is recommended by the National Council on Radiation Protection following uranium exposure [144, 145].
Section Summary
DTPA is unsupported for use in uranium chelation. Sodium bicarbonate is currently recommended, although the animal evidence is poor. One might consider dialysis [145]. The HOPOs are considered experimental.
Conclusions
Chelation considerations for metals are complex. They must account for dose–response relationships, a means of toxicity assessment, and an assessment of the metal species, the chelator, and the chelate. Decorporation, even if successful, risks renal exposure to these entities. Multiple chelators may produce potentially harmful bycatch. A carefully considered risk-benefit assessment and consultation with Poison Centers and others with toxicological expertise is recommended in these particularly challenging cases.
Acknowledgments
ATSDR Disclaimer
This publication was supported by the cooperative agreement award number 1U61TS000117-04 from the Agency for Toxic Substances and Disease Registry (ATSDR). Its contents are the responsibility of the authors and do not necessarily represent the official views of the Agency for Toxic Substances and Disease Registry (ATSDR).
Author Disclaimer
Within the medical literature, pharmaceuticals, pharmaceutical combinations, and other products are used off-label as antidotal therapies; off-label uses are referred to in these proceedings. This is for discussion purposes only and does not constitute endorsement of off-label use by the author or any of the author's affiliations.
Conflict delineations
For the work under consideration for publication, Dr. Smith received an honorarium and reimbursement for travel through the ACMT/ATSDR Cooperative Agreement. In addition, a grant submission is under consideration to Dr. Smith’s institution from the US Department of Health and Human Services, Office of the Assistant Secretary for Preparedness and Response. Grant submission is under: Funding Opportunity Title: Assistant Secretary for Preparedness and Response Grants to Support, Scientific Research Related to Recovery from Hurricane Sandy, Funding Opportunity Number EP-HIT-13-001.
References
- 1.Benson BE, Hoppu K, Troutman WG, Bedry R, Erdman A, Hojer J, et al. Position paper update: gastric lavage for gastrointestinal decontamination. Clin Toxicol. 2013;51(3):140–146. doi: 10.3109/15563650.2013.770154. [DOI] [PubMed] [Google Scholar]
- 2.Hegde ML, Bharathi P, Suram A, Venugopal C, Jagannathan R, Poddar P, et al. Challenges associated with metal chelation therapy in Alzheimer’s disease. J Alzheimers Dis. 2009;17(3):457–468. doi: 10.3233/JAD-2009-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bergeron RJ, Wiegand J, Singh S. Desferrithiocin analogue uranium decorporation agents. Int J Radiat Biol. 2009;85(4):348–361. doi: 10.1080/09553000902781089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aposhian HV, Maiorino RM, Gonzalez-Ramirez D, Zuniga-Charles M, Xu Z, Hurlbut KM, et al. Mobilization of heavy metals by newer therapeutically useful chelating agents. Toxicology. 1995;97(1–3):23–38. doi: 10.1016/0300-483x(95)02965-b. [DOI] [PubMed] [Google Scholar]
- 5.Andersen O, Aaseth J. Molecular mechanisms of in vivo metal chelation: implications for clinical treatment of metal intoxications. Environ Health Perspect. 2002;110(Suppl 5):887–890. doi: 10.1289/ehp.02110s5887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Managing the nation’s bycatch: priorities, programs and actions for the National Marine Fisheries Service. Washington: Department of Commerce; 1998. [Google Scholar]
- 7.Waters RS, Bryden NA, Patterson KY, Veillon C, Anderson RA. EDTA chelation effects on urinary losses of cadmium calcium, chromium, cobalt, copper, lead, magnesium, and zinc. Biol Trace Elem Res. 2001;83(3):207–221. doi: 10.1385/BTER:83:3:207. [DOI] [PubMed] [Google Scholar]
- 8.Yokel RA, Hicks CL, Florence RL. Aluminum bioavailability from basic sodium aluminum phosphate, an approved food additive emulsifying agent, incorporated in cheese. Food Chem Toxicol. 2008;46(6):2261–2266. doi: 10.1016/j.fct.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Graves AB, White E, Koepsell TD, Reifler BV, van Belle G, Larson EB. The association between aluminum-containing products and Alzheimer’s disease. J Clin Epidemiol. 1990;43(1):35–44. doi: 10.1016/0895-4356(90)90053-r. [DOI] [PubMed] [Google Scholar]
- 10.Rondeau V. A review of epidemiologic studies on aluminum and silica in relation to Alzheimer’s disease and associated disorders. Rev Environ Health. 2002;17(2):107–121. doi: 10.1515/reveh.2002.17.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perl DP, Moalem S. Aluminum and Alzheimer’s disease, a personal perspective after 25 years. J Alzheimers Dis. 2006;9(3 Suppl):291–300. doi: 10.3233/jad-2006-9s332. [DOI] [PubMed] [Google Scholar]
- 12.National Cancer Institute. Antiperspirants/deodorants and breast cancer (2013) http://www.cancer.gov/cancertopics/factsheet/Risk/AP-Deo. Accessed 14 Aug 2013
- 13.Kirschbaum BB, Schoolwerth AC. Acute aluminum toxicity associated with oral citrate and aluminum-containing antacids. Am J Med Sci. 1989;297(1):9–11. doi: 10.1097/00000441-198901000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Schootstra R, van Driel MF, Hassankhan R, van de Werff R, Oremus ET, Uges DR, Mensink HJ. The use of an alum irrigation in the treatment of massive bladder haemorrhage. Pharmaceutisch weekblad. Sci Ed. 1989;11(5):175–178. doi: 10.1007/BF01959467. [DOI] [PubMed] [Google Scholar]
- 15.Phelps KR, Naylor K, Brien TP, Wilbur H, Haqqie SS. Encephalopathy after bladder irrigation with alum: case report and literature review. Am J Med Sci. 1999;318(3):181–185. doi: 10.1097/00000441-199909000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Wier HA, Kuhn RJ. Aluminum toxicity in neonatal parenteral nutrition: what can we do? Ann Pharmacother. 2012;46(1):137–140. doi: 10.1345/aph.1Q399. [DOI] [PubMed] [Google Scholar]
- 17.Food and Drug Administration, Health and Human Services (2011) 21 Code of Federal Regulation §201.323 Aluminum in large and small volume parenterals used in total parenteral nutrition. FDA, Silver Spring
- 18.Yong RL, Holmes DT, Sreenivasan GM. Aluminum toxicity due to intravenous injection of boiled methadone. N Engl J Med. 2006;354(11):1210–1211. doi: 10.1056/NEJMc053341. [DOI] [PubMed] [Google Scholar]
- 19.Alfrey AC, LeGendre GR, Kaehny WD. The dialysis encephalopathy syndrome. Possible aluminum intoxication. New Engl J Med. 1976;294(4):184–188. doi: 10.1056/NEJM197601222940402. [DOI] [PubMed] [Google Scholar]
- 20.D’Haese PC, Couttenye MM, De Broe ME. Diagnosis and treatment of aluminium bone disease. Nephrol Dial Transplant. 1996;11(Suppl 3):74–79. doi: 10.1093/ndt/11.supp3.74. [DOI] [PubMed] [Google Scholar]
- 21.Kwack C, Balakrishnan VS. Managing erythropoietin hyporesponsiveness. Semin Dial. 2006;19(2):146–151. doi: 10.1111/j.1525-139X.2006.00141.x. [DOI] [PubMed] [Google Scholar]
- 22.Swartz R, Dombrouski J, Burnatowska-Hledin M, Mayor G. Microcytic anemia in dialysis patients: reversible marker of aluminum toxicity. Am J Kidney Dis. 1987;9(3):217–223. doi: 10.1016/s0272-6386(87)80058-6. [DOI] [PubMed] [Google Scholar]
- 23.Roth A, Nogues C, Galle P, Drueke T. Multiorgan aluminium deposits in a chronic haemodialysis patient. Electron microscope and microprobe studies. Virchows Arch A Pathol Anat Histopathol. 1984;405(1):131–140. doi: 10.1007/BF00694931. [DOI] [PubMed] [Google Scholar]
- 24.National Kidney Foundation K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42(Suppl 3):S1–S202. [PubMed] [Google Scholar]
- 25.Diskin CJ, Thomas CE. Is it time to reexamine KDOQI aluminum guidelines? Am J Kidney Dis. 2006;48(5):876–877. doi: 10.1053/j.ajkd.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 26.Kidney Disease: Improving Global Outcomes (KDIGO) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease—mineral and bone disorder (CKD-MBD) Am J Kidney Dis. 2009;76(Suppl 113):S1–S130. doi: 10.1038/ki.2009.188. [DOI] [PubMed] [Google Scholar]
- 27.Riihimaki V, Aitio A. Occupational exposure to aluminum and its biomonitoring in perspective. Crit Rev Toxicol. 2012;42(10):827–853. doi: 10.3109/10408444.2012.725027. [DOI] [PubMed] [Google Scholar]
- 28.Malo JL, Vandenplas O. Definitions and classification of work-related asthma. Immunol Allergy Clin N Am. 2011;31(4):645–662. doi: 10.1016/j.iac.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Methods Development Team, Industrial Hygiene Chemistry Division, OSHA Salt Lake Technical Center (2001) Aluminum oxide in workplace atmospheres. T-ID109SG-PV-02-0110-M. Occupational Safety and Health Administration (OSHA), US Department of Labor, Sandy
- 30.Keberle H. The biochemistry of desferrioxamine and its relation to iron metabolism. Ann NY Acad Sci. 1964;119:758–768. doi: 10.1111/j.1749-6632.1965.tb54077.x. [DOI] [PubMed] [Google Scholar]
- 31.Yokel RA. Aluminum chelation principles and recent advances. Coord Chem Rev. 2002;228(2):97–113. [Google Scholar]
- 32.Andriani M, Nordio M, Saporiti E. Estimation of statistical moments for desferrioxamine and its iron and aluminum chelates: contribution to optimisation of therapy in uremic patients. Nephron. 1996;72(2):218–224. doi: 10.1159/000188845. [DOI] [PubMed] [Google Scholar]
- 33.Verpooten GA, D’Haese PC, Boelaert JR, Becaus I, Lamberts LV, De Broe ME. Pharmacokinetics of aluminoxamine and ferrioxamine and dose finding of desferrioxamine in haemodialysis patients. Nephrol Dial Transplant. 1992;7(9):931–938. doi: 10.1093/ndt/7.9.931. [DOI] [PubMed] [Google Scholar]
- 34.Lillevang ST, Pedersen FB. Exacerbation of aluminium encephalopathy after treatment with desferrioxamine. Nephrol Dial Transplant. 1989;4(7):676. [PubMed] [Google Scholar]
- 35.McCauley J, Sorkin MI. Exacerbation of aluminium encephalopathy after treatment with desferrioxamine. Nephrol Dial Transplant. 1989;4(2):110–114. [PubMed] [Google Scholar]
- 36.Sherrard DJ, Walker JV, Boykin JL. Precipitation of dialysis dementia by deferoxamine treatment of aluminum-related bone disease. Am J Kidney Dis. 1988;12(2):126–130. doi: 10.1016/s0272-6386(88)80007-6. [DOI] [PubMed] [Google Scholar]
- 37.Kan WC, Chien CC, Wu CC, Su SB, Hwang JC, Wang HY. Comparison of low-dose deferoxamine versus standard-dose deferoxamine for treatment of aluminium overload among haemodialysis patients. Nephrol Dialysis Transplant. 2010;25(5):1604–1608. doi: 10.1093/ndt/gfp649. [DOI] [PubMed] [Google Scholar]
- 38.Gonzalez-Suarez I, Alvarez-Hernandez D, Carrillo-Lopez N, Naves-Diaz M, Luis Fernandez-Martin J, Cannata-Andia JB. Aluminum posttranscriptional regulation of parathyroid hormone synthesis: a role for the calcium-sensing receptor. Kidney Int. 2005;68(6):2484–2496. doi: 10.1111/j.1523-1755.2005.00724.x. [DOI] [PubMed] [Google Scholar]
- 39.Klein GL, Snodgrass WR, Griffin MP, Miller NL, Alfrey AC. Hypocalcemia complicating deferoxamine therapy in an infant with parenteral nutrition-associated aluminum overload: evidence for a role of aluminum in the bone disease of infants. J Pediatr Gastroenterol Nutr. 1989;9(3):400–403. doi: 10.1097/00005176-198910000-00024. [DOI] [PubMed] [Google Scholar]
- 40.Desferal®. deferoxamine mesylate for injection USP. Prescribing Information. East Hanover: Novartis Pharmaceuticals Corporation; 2011. [Google Scholar]
- 41.EXJADE® (deferasirox) tablets for oral suspension. Prescribing information. East Hanover: Novartis Pharmaceuticals Corporation; 2011. [Google Scholar]
- 42.Barata JD, D’Haese PC, Pires C, Lamberts LV, Simoes J, De Broe ME. Low-dose (5 mg/kg) desferrioxamine treatment in acutely aluminium-intoxicated haemodialysis patients using two drug administration schedules. Nephrol Dial Transplant. 1996;11(1):125–132. [PubMed] [Google Scholar]
- 43.Douthat WG, Acuna Aguerre G, Fernandez Martin JL, Mouzo R, Cannata Andia JB. Treatment of aluminium intoxication: a new scheme for desferrioxamine administration. Nephrol Dial Transplant. 1994;9(10):1431–1434. [PubMed] [Google Scholar]
- 44.Nakamura H, Rose PG, Blumer JL, Reed MD. Acute encephalopathy due to aluminum toxicity successfully treated by combined intravenous deferoxamine and hemodialysis. J Clin Pharmacol. 2000;40(3):296–300. doi: 10.1177/00912700022008847. [DOI] [PubMed] [Google Scholar]
- 45.Kontoghiorghes GJ. Comparative efficacy and toxicity of desferrioxamine, deferiprone and other iron and aluminium chelating drugs. Toxicol Lett. 1995;80(1–3):1–18. doi: 10.1016/0378-4274(95)03415-h. [DOI] [PubMed] [Google Scholar]
- 46.Saljooghi AS. Chelation of aluminum by combining deferasirox and deferiprone in rats. Toxicol Ind Health. 2012;28(8):740–745. doi: 10.1177/0748233711422731. [DOI] [PubMed] [Google Scholar]
- 47.Liu P, Yao YN, Wu SD, Dong HJ, Feng GC, Yuan XY. The efficacy of deferiprone on tissues aluminum removal and copper, zinc, manganese level in rabbits. J Inorg Biochem. 2005;99(8):1733–1737. doi: 10.1016/j.jinorgbio.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 48.Jirasomprasert T, Morales NP, Limenta LM, Sirijaroonwong S, Yamanont P, Wilairat P, et al. Pharmaco/ferrokinetic-related pro-oxidant activity of deferiprone in beta-thalassemia. Free Radic Res. 2009;43(5):485–491. doi: 10.1080/10715760902870611. [DOI] [PubMed] [Google Scholar]
- 49.FERRIPROX® (deferiprone) tablets, for oral use. Prescribing information. Rockville: ApoPharma USA; 2011. [Google Scholar]
- 50.Blanusa M, Varnai VM, Piasek M, Kostial K. Chelators as antidotes of metal toxicity: therapeutic and experimental aspects. Curr Med Chem. 2005;12(23):2771–2794. doi: 10.2174/092986705774462987. [DOI] [PubMed] [Google Scholar]
- 51.Van de Vyver FL, Silva FJ, D’Haese PC, Verbueken AH, De Broe ME. Aluminum toxicity in dialysis patients. Contrib Nephrol. 1987;55:198–220. doi: 10.1159/000413420. [DOI] [PubMed] [Google Scholar]
- 52.Brown DJ, Dawborn JK, Ham KN, Xipell JM. Treatment of dialysis osteomalacia with desferrioxamine. Lancet. 1982;2(8294):343–345. doi: 10.1016/s0140-6736(82)90544-x. [DOI] [PubMed] [Google Scholar]
- 53.Arze RS, Parkinson IS, Cartlidge NE, Britton P, Ward MK. Reversal of aluminium dialysis encephalopathy after desferrioxamine treatment. Lancet. 1981;2(8255):1116. doi: 10.1016/s0140-6736(81)91324-6. [DOI] [PubMed] [Google Scholar]
- 54.Toxicological profile for cadmium. Atlanta: Department of Health and Human Services, Public Health Service; 2012. [Google Scholar]
- 55.Satarug S. Long-term exposure to cadmium in food and cigarette smoke, liver effects and hepatocellular carcinoma. Curr Drug Metab. 2012;13(3):257–271. doi: 10.2174/138920012799320446. [DOI] [PubMed] [Google Scholar]
- 56.IARC monographs on the evaluation of carcinogenic risks to humans. Beryllium, cadmium, mercury, and exposures in the glass manufacturing industry. Lyons: International Agency for Research on Cancer; 1993. [PMC free article] [PubMed] [Google Scholar]
- 57.Prozialeck WC, Edwards JR. Mechanisms of cadmium-induced proximal tubule injury: new insights with implications for biomonitoring and therapeutic interventions. J Pharmacol Exp Ther. 2012;343(1):2–12. doi: 10.1124/jpet.110.166769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tsuchiya K. Causation of Ouch-Ouch Disease (Itai-Itai Byo)–an introductory review. I. Nature of the disease. Keio J Med. 1969;18(4):181–194. doi: 10.2302/kjm.18.181. [DOI] [PubMed] [Google Scholar]
- 59.Tsuchiya K. Causation of Ouch-Ouch Disease (Itai-Itai Byo)–an introductory review. II. Epidemiology and evaluation. Keio J Med. 1969;18(4):195–211. doi: 10.2302/kjm.18.195. [DOI] [PubMed] [Google Scholar]
- 60.Ando Y, Shibata E, Tsuchiyama F, Sakai S. Elevated urinary cadmium concentrations in a patient with acute cadmium pneumonitis. Scand J Work Environ Health. 1996;22(2):150–153. doi: 10.5271/sjweh.124. [DOI] [PubMed] [Google Scholar]
- 61.Davison AG, Fayers PM, Taylor AJ, Venables KM, Darbyshire J, Pickering CA, et al. Cadmium fume inhalation and emphysema. Lancet. 1988;1(8587):663–667. doi: 10.1016/s0140-6736(88)91474-2. [DOI] [PubMed] [Google Scholar]
- 62.Okuda B, Iwamoto Y, Tachibana H, Sugita M. Parkinsonism after acute cadmium poisoning. Clin Neurol Neurosurg. 1997;99(4):263–265. doi: 10.1016/s0303-8467(97)00090-5. [DOI] [PubMed] [Google Scholar]
- 63.Fernandez MA, Sanz P, Palomar M, Serra J, Gadea E. Fatal chemical pneumonitis due to cadmium fumes. Occup Med (Lond) 1996;46(5):372–374. doi: 10.1093/occmed/46.5.372. [DOI] [PubMed] [Google Scholar]
- 64.Blejer HP, Caplan PE, Alcocer AE. Acute cadmium fume poisoning in welders—a fatal and a nonfatal case in California. Calif Med. 1966;105(4):290–296. [PMC free article] [PubMed] [Google Scholar]
- 65.Beton DC, Andrews GS, Davies HJ, Howells L, Smith GF. Acute cadmium fume poisoning. Five cases with one death from renal necrosis. Br J Ind Med. 1966;23(4):292–301. doi: 10.1136/oem.23.4.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hung YM, Chung HM. Acute self-poisoning by ingestion of cadmium and barium. Nephrol Dial Transplant. 2004;19(5):1308–1309. doi: 10.1093/ndt/gfh169. [DOI] [PubMed] [Google Scholar]
- 67.Occupational Safety and Health Administration (OSHA) (1993) Cadmium. US Department of Labor, Washington. https://ww.osha.gov/Publications/3136-08R-2003-English.html#requirements_medical. Accessed 3 September 2013
- 68.National Institute for Occupational Safety and Health (NIOSH) (2013) Workplace safety & health topics. Cadmium. Centers for Disease Control and Prevention, Atlanta. http://www.cdc.gov/niosh/topics/cadmium/. Accessed 4 Sept 2013
- 69.Suzuki CA, Ohta H, Albores A, Koropatnick J, Cherian MG. Induction of metallothionein synthesis by zinc in cadmium pretreated rats. Toxicology. 1990;63(3):273–284. doi: 10.1016/0300-483x(90)90190-r. [DOI] [PubMed] [Google Scholar]
- 70.Chan HM, Cherian MG. Mobilization of hepatic cadmium in pregnant rats. Toxicol Appl Pharmacol. 1993;120(2):308–314. doi: 10.1006/taap.1993.1116. [DOI] [PubMed] [Google Scholar]
- 71.Dimaval RJ. Scientific product monograph. Berlin: HEYL Chemisch-pharmazeutische Fabrik GmbH und Co. KG; 2009. [Google Scholar]
- 72.Wu X, Su S, Zhai R, Chen K, Jin T, Huang B, et al. Lack of reversal effect of EDTA treatment on cadmium induced renal dysfunction: a fourteen-year follow-up. Biometals Int J Role Met Ions Biol Biochem Med. 2004;17(4):435–441. doi: 10.1023/b:biom.0000029440.23884.d6. [DOI] [PubMed] [Google Scholar]
- 73.Gil HW, Kang EJ, Lee KH, Yang JO, Lee EY, Hong SY. Effect of glutathione on the cadmium chelation of EDTA in a patient with cadmium intoxication. Hum Exp Toxicol. 2011;30(1):79–83. doi: 10.1177/0960327110369818. [DOI] [PubMed] [Google Scholar]
- 74.Rau W, Planas-Bohne F. Enhancement of the kidney Cd burden by SH-containing chelating agents. Biol Trace Elem Research. 1989;21:227–231. doi: 10.1007/BF02917257. [DOI] [PubMed] [Google Scholar]
- 75.Saric MM, Blanusa M, Juresa D, Saric M, Varnai VM, Kostial K. Combined early treatment with chelating agents DMSA and CaDTPA in acute oral cadmium exposure. Basic Clin Pharmacol Toxicol. 2004;94(3):119–123. doi: 10.1111/j.1742-7843.2004.pto940304.x. [DOI] [PubMed] [Google Scholar]
- 76.Eybl V, Sykora J, Koutensky J, Caisova D, Schwartz A, Mertl F. Interaction of chelating agents with cadmium in mice and rats. Environ Health Perspect. 1984;54:267–273. doi: 10.1289/ehp.8454267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cantilena LR, Jr, Klaassen CD. Decreased effectiveness of chelation therapy with time after acute cadmium poisoning. Toxicol Appl Pharmacol. 1982;63(2):173–180. doi: 10.1016/0041-008x(82)90038-2. [DOI] [PubMed] [Google Scholar]
- 78.Jones MM, Xu C, Singh PK, Walker EM., Jr Cadmium mobilization by nitrogen donor chelating agents. J Toxicol Environ Health. 1996;48(1):71–80. doi: 10.1080/009841096161474. [DOI] [PubMed] [Google Scholar]
- 79.McGivern J, Mason J. The effect of chelation on the fate of intravenously administered cadmium in rats. J Comp Pathol. 1979;89(1):1–9. doi: 10.1016/0021-9975(79)90002-1. [DOI] [PubMed] [Google Scholar]
- 80.Basinger MA, Jones MM, Holscher MA, Vaughn WK. Antagonists for acute oral cadmium chloride intoxication. J Toxicol Environ Health. 1988;23(1):77–89. doi: 10.1080/15287398809531095. [DOI] [PubMed] [Google Scholar]
- 81.Lyle WH, Green JN, Gore V, Vidler J (1968) Enhancement of cadmium nephrotoxicity by penicillamine in the rat. Postgrad Med J Suppl:18–21 [PubMed]
- 82.Walker EM, Jr, Gale GR, Fody EP, Atkins LM, Smith AB, Jones MM. Comparative antidotal effects of diethyldithiocarbamate, dimercaptosuccinate, and diethylenetriaminepentaacetate against cadmium-induced testicular toxicity in mice. Res Commun Chem Pathol Pharmacol. 1986;51(2):231–244. [PubMed] [Google Scholar]
- 83.Kargacin B, Kostial K, Arezina R, Singh PK, Jones MM, Cikrt M. Influence of age and time of administration of dithiocarbamate analogues on cadmium retention in rats. JAT. 1991;11(4):273–277. doi: 10.1002/jat.2550110408. [DOI] [PubMed] [Google Scholar]
- 84.Kargacin B, Kostial K, Arezina R, Singh PK, Jones MM, Cikrt M. Dithiocarbamate analog N-(4-methoxybenzyl)-N-dithiocarboxy-D-glucamine reduces the retention of ingested cadmium in rats. JAT. 1991;11(5):313–315. doi: 10.1002/jat.2550110503. [DOI] [PubMed] [Google Scholar]
- 85.Cantilena LR, Jr, Irwin G, Preskorn S, Klaassen CD. The effect of diethyldithiocarbamate on brain uptake of cadmium. Toxicol Appl Pharmacol. 1982;63(3):338–343. doi: 10.1016/0041-008x(82)90262-9. [DOI] [PubMed] [Google Scholar]
- 86.Blanusa M, Kostial K, Restek-Samarzija N, Piasek M, Jones MM, Singh PK. Mobilisation of cadmium by meso- and racemic-2,3-dimercaptosuccinic acid (DMSA) in rats. Pharmacol Toxicol. 2000;87(4):179–181. doi: 10.1034/j.1600-0773.2000.d01-70.x. [DOI] [PubMed] [Google Scholar]
- 87.Andersen O, Nielsen JB. Oral cadmium chloride intoxication in mice: effects of penicillamine, dimercaptosuccinic acid and related compounds. Pharmacol Toxicol. 1988;63(5):386–389. doi: 10.1111/j.1600-0773.1988.tb00973.x. [DOI] [PubMed] [Google Scholar]
- 88.Cantilena LR, Jr, Klaassen CD. The effect of ethylenediaminetetraacetic acid (EDTA) and EDTA plus salicylate on acute cadmium toxicity and distribution. Toxicol Appl Pharmacol. 1980;53(3):510–514. doi: 10.1016/0041-008x(80)90363-4. [DOI] [PubMed] [Google Scholar]
- 89.Tandon SK, Singh S, Prasad S, Khandekar K, Dwivedi VK, Chatterjee M, Mathur N. Reversal of cadmium induced oxidative stress by chelating agent, antioxidant or their combination in rat. Toxicol Lett. 2003;145(3):211–217. doi: 10.1016/s0378-4274(03)00265-0. [DOI] [PubMed] [Google Scholar]
- 90.Drake TC, Rudser KD, Seaquist ER, Saeed A. Chromium infusion in hospitalized patients with severe insulin resistance: a retrospective analysis. Endocr Pract. 2012;18(3):394–398. doi: 10.4158/EP11243.OR. [DOI] [PubMed] [Google Scholar]
- 91.Hamula C, Wang Z, Zhang H, Kwon E, Li XF, Gabos S, Le XC. Chromium on the hands of children after playing in playgrounds built from chromated copper arsenate (CCA)-treated wood. Environ Health Perspect. 2006;114(3):460–465. doi: 10.1289/ehp.8521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Goode AE, Perkins JM, Sandison A, Karunakaran C, Cheng H, Wall D, et al. Chemical speciation of nanoparticles surrounding metal-on-metal hips. Chem Commun (Camb) 2012;48(67):8335–8337. doi: 10.1039/c2cc33016d. [DOI] [PubMed] [Google Scholar]
- 93.Toxicological profile for chromium. Atlanta: Department of Health and Human Services, Public Health Service; 2012. [Google Scholar]
- 94.Matey P, Allison KP, Sheehan TM, Gowar JP. Chromic acid burns: early aggressive excision is the best method to prevent systemic toxicity. J Burn Care Rehab. 2000;21(3):241–245. doi: 10.1067/mbc.2000.106066. [DOI] [PubMed] [Google Scholar]
- 95.Kerger BD, Finley BL, Corbett GE, Dodge DG, Paustenbach DJ. Ingestion of chromium(VI) in drinking water by human volunteers: absorption, distribution, and excretion of single and repeated doses. J Toxicol Environ Health. 1997;50(1):67–95. doi: 10.1080/009841097160618. [DOI] [PubMed] [Google Scholar]
- 96.Bahijri SM, Alissa EM. Increased insulin resistance is associated with increased urinary excretion of chromium in non-diabetic, normotensive Saudi adults. J Clin Biochem Nutr. 2011;49(3):164–168. doi: 10.3164/jcbn.10-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liu KJ, Shi X. In vivo reduction of chromium (VI) and its related free radical generation. Mol Cell Biochem. 2001;222(1–2):41–47. [PubMed] [Google Scholar]
- 98.IARC monographs on the evaluation of carcinogenic risks to humans. A review of human carcinogens. Part C: arsenic, metals, fibres, and dusts. Lyons: International Agency for Research on Cancer; 2012. [PMC free article] [PubMed] [Google Scholar]
- 99.Afolaranmi GA, Tettey JN, Murray HM, Meek RM, Grant MH. The effect of anticoagulants on the distribution of chromium VI in blood fractions. J Arthroplasty. 2010;25(1):118–120. doi: 10.1016/j.arth.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 100.Ellis EN, Brouhard BH, Lynch RE, Dawson EB, Tisdell R, Nichols MM, Ramirez F. Effects of hemodialysis and dimercaprol in acute dichromate poisoning. J Toxicol Clin Toxicol. 1982;19(3):249–258. doi: 10.3109/15563658209025729. [DOI] [PubMed] [Google Scholar]
- 101.Meert KL, Ellis J, Aronow R, Perrin E. Acute ammonium dichromate poisoning. Ann Emerg Med. 1994;24(4):748–750. doi: 10.1016/s0196-0644(94)70288-8. [DOI] [PubMed] [Google Scholar]
- 102.Lin CC, Wu ML, Yang CC, Ger J, Tsai WJ, Deng JF. Acute severe chromium poisoning after dermal exposure to hexavalent chromium. J Chin Med Assoc. 2009;72(4):219–221. doi: 10.1016/S1726-4901(09)70059-0. [DOI] [PubMed] [Google Scholar]
- 103.Walpole IR, Johnston K, Clarkson R, Wilson G, Bower G. Acute chromium poisoning in a 2 year old child. Aust Paediatr J. 1985;21(1):65–67. doi: 10.1111/j.1440-1754.1985.tb00126.x. [DOI] [PubMed] [Google Scholar]
- 104.Anderson RA, Bryden NA, Waters R. EDTA chelation therapy does not selectively increase chromium losses. Biol Trace Elem Res. 1999;70(3):265–272. doi: 10.1007/BF02783835. [DOI] [PubMed] [Google Scholar]
- 105.Pazzaglia UE, Apostoli P, Congiu T, Catalani S, Marchese M, Zarattini G. Cobalt, chromium and molybdenum ions kinetics in the human body: data gained from a total hip replacement with massive third body wear of the head and neuropathy by cobalt intoxication. Arch Orthop Trauma Surg. 2011;131(9):1299–1308. doi: 10.1007/s00402-011-1268-7. [DOI] [PubMed] [Google Scholar]
- 106.Kolacinski Z, Kostrzewski P, Kruszewska S, Razniewska G, Mielczarska J. Acute potassium dichromate poisoning: a toxicokinetic case study. J Toxicol Clin Toxicol. 1999;37(6):785–791. doi: 10.1081/clt-100102458. [DOI] [PubMed] [Google Scholar]
- 107.Torres-Alanis O, Garza-Ocanas L, Bernal MA, Pineyro-Lopez A. Urinary excretion of trace elements in humans after sodium 2,3-dimercaptopropane-1-sulfonate challenge test. J Toxicol Clin Toxicol. 2000;38(7):697–700. doi: 10.1081/clt-100102382. [DOI] [PubMed] [Google Scholar]
- 108.Hantson P, Van Caenegem O, Decordier I, Haufroid V, Lison D. Hexavalent chromium ingestion: biological markers of nephrotoxicity and genotoxicity. Clin Toxicol. 2005;43(2):111–112. [PubMed] [Google Scholar]
- 109.Schiffl H, Weidmann P, Weiss M, Massry SG. Dialysis treatment of acute chromium intoxication and comparative efficacy of peritoneal versus hemodialysis in chromium removal. Miner Electrolyte Metabol. 1982;7(1):28–35. [PubMed] [Google Scholar]
- 110.Baresic M, Gornik I, Radonic R, Zlopasa O, Gubarev N, Gasparovic V. Survival after severe acute chromic acid poisoning complicated with renal and liver failure. Int Med. 2009;48(9):711–715. doi: 10.2169/internalmedicine.48.1943. [DOI] [PubMed] [Google Scholar]
- 111.Bradberry SM, Vale JA. Therapeutic review: is ascorbic acid of value in chromium poisoning and chromium dermatitis? J Toxicol Clin Toxicol. 1999;37(2):195–200. doi: 10.1081/clt-100102419. [DOI] [PubMed] [Google Scholar]
- 112.Nowak-Wiaderek W. Influence of various drugs on excretion and distribution of chromium-51 in acute poisoning in rats. Pol J Med Pharm. 1975;7(4):308–310. [PubMed] [Google Scholar]
- 113.Molina-Jijon E, Zarco-Marquez G, Medina-Campos ON, Zatarain-Barron ZL, Hernandez-Pando R, Pinzon E, et al. Deferoxamine pretreatment prevents Cr(VI)-induced nephrotoxicity and oxidant stress: role of Cr(VI) chelation. Toxicology. 2012;291(1–3):93–101. doi: 10.1016/j.tox.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 114.Banner W, Jr, Koch M, Capin DM, Hopf SB, Chang S, Tong TG. Experimental chelation therapy in chromium, lead, and boron intoxication with N-acetylcysteine and other compounds. Toxicol Appl Pharmacol. 1986;83(1):142–147. doi: 10.1016/0041-008x(86)90331-5. [DOI] [PubMed] [Google Scholar]
- 115.Wang BJ, Guo YL, Chang HY, Sheu HM, Pan MH, Lee YH, Wang YJ. N-acetylcysteine inhibits chromium hypersensitivity in coadjuvant chromium-sensitized albino guinea pigs by suppressing the effects of reactive oxygen species. Exp Dermatol. 2010;19(8):e191–e200. doi: 10.1111/j.1600-0625.2009.01045.x. [DOI] [PubMed] [Google Scholar]
- 116.Tower SS. Arthroprosthetic cobaltism: neurological and cardiac manifestations in two patients with metal-on-metal arthroplasty: a case report. J Bone Joint Surg. 2010;92(17):2847–2851. doi: 10.2106/JBJS.J.00125. [DOI] [PubMed] [Google Scholar]
- 117.Oldenburg M, Wegner R, Baur X. Severe cobalt intoxication due to prosthesis wear in repeated total hip arthroplasty. J Arthroplasty. 2009;24(5):825.e815. doi: 10.1016/j.arth.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 118.Jacobs JJ, Skipor AK, Patterson LM, Hallab NJ, Paprosky WG, Black J, Galante JO. Metal release in patients who have had a primary total hip arthroplasty. A prospective, controlled, longitudinal study. J Bone Joint Surg. 1998;80(10):1447–1458. doi: 10.2106/00004623-199810000-00006. [DOI] [PubMed] [Google Scholar]
- 119.Zywiel MG, Brandt JM, Overgaard CB, Cheung AC, Turgeon TR, Syed KA. Fatal cardiomyopathy after revision total hip replacement for fracture of a ceramic liner. Bone Joint J. 2013;95-B(1):31–37. doi: 10.1302/0301-620X.95B1.30060. [DOI] [PubMed] [Google Scholar]
- 120.Washburn TC, Kaplan E. Cobalt therapy and goiter. Clin Pediatr. 1964;3:89–92. doi: 10.1177/000992286400300207. [DOI] [PubMed] [Google Scholar]
- 121.Simonsen LO, Brown AM, Harbak H, Kristensen BI, Bennekou P. Cobalt uptake and binding in human red blood cells. Blood Cells Mol Dis. 2011;46(4):266–276. doi: 10.1016/j.bcmd.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 122.Ichikawa Y, Kusaka Y, Goto S. Biological monitoring of cobalt exposure, based on cobalt concentrations in blood and urine. Int Arch Occup Environ Health. 1985;55(4):269–276. doi: 10.1007/BF00377685. [DOI] [PubMed] [Google Scholar]
- 123.Sauni R, Linna A, Oksa P, Nordman H, Tuppurainen M, Uitti J. Cobalt asthma—a case series from a cobalt plant. Occup Med. 2010;60(4):301–306. doi: 10.1093/occmed/kqq023. [DOI] [PubMed] [Google Scholar]
- 124.Toxicological profile for cobalt. Atlanta: US Department of Health and Human Services, Public Health Service; 2004. [Google Scholar]
- 125.McDermott PH, Delaney RL, Egan JD, Sullivan JF. Myocardosis and cardiac failure in men. JAMA. 1966;198(3):253–256. [PubMed] [Google Scholar]
- 126.Weber KT. A Quebec quencher. Cardiovasc Res. 1998;40(3):423–425. doi: 10.1016/s0008-6363(98)00243-0. [DOI] [PubMed] [Google Scholar]
- 127.Barceloux DG. Cobalt. J Toxicol Clin Toxicol. 1999;37(2):201–206. doi: 10.1081/clt-100102420. [DOI] [PubMed] [Google Scholar]
- 128.Fischer T, Rystedt I. Cobalt allergy in hard metal workers. Contact Dermatitis. 1983;9(2):115–121. doi: 10.1111/j.1600-0536.1983.tb04316.x. [DOI] [PubMed] [Google Scholar]
- 129.Simonsen LO, Harbak H, Bennekou P. Cobalt metabolism and toxicology—a brief update. Sci Total Environ. 2012;432:210–215. doi: 10.1016/j.scitotenv.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 130.US Food and Drug Administration (2013) Metal-on-metal hip implants. US Department of Health & Human Services. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/MetalonMetalHipImplants/default.htm. Accessed 19 Aug 2013
- 131.U.K. Medicines and Healthcare Products Regulatory Agency (MHRA) (2012) Medical device alert. All metal-on-metal (MoM) hip replacements. Ref: MDA/2010/036. Department of Health, Medicines and Healthcare Products Regulatory Agency, London. http://www.mhra.gov.uk/home/groups/dts-bs/documents/medicaldevicealert/con155767.pdf. Accessed 3 Sept 2013
- 132.Fourth National Report on Human Exposure to Environmental Chemicals, Updated Tables. Atlanta: Department of Health and Human Services; 2013. [Google Scholar]
- 133.Lantin AC, Mallants A, Vermeulen J, Speybroeck N, Hoet P, Lison D. Absence of adverse effect on thyroid function and red blood cells in a population of workers exposed to cobalt compounds. Toxicol Lett. 2011;201(1):42–46. doi: 10.1016/j.toxlet.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 134.National Institute for Occupational Safety and Health (NIOSH) (2013) Workplace safety & health topics. Cobalt. Centers for Disease Control and Prevention, Atlanta. http://www.cdc.gov/niosh/topics/cobalt/. Accessed 4 Sept 2013
- 135.Henretig F, Shannon M. An 11-year-old boy develops vomiting, weakness, weight loss and a neck mass. Int J Med Toxicol. 1988;1(2):13–15. [Google Scholar]
- 136.Domingo JL, Llobet JM. Treatment of acute cobalt intoxication in rats with L-methionine. Rev Esp Fisiol. 1984;40(4):443–448. [PubMed] [Google Scholar]
- 137.Domingo JL, Llobet JM, Tomas JM. N-acetyl-L-cysteine in acute cobalt poisoning. Arch Farmacol Toxicol. 1985;11(1):55–62. [PubMed] [Google Scholar]
- 138.Domingo JL, Llobet JM, Corbella J. The effects of EDTA in acute cobalt intoxication in rats. Toxicol Eur Res. 1983;5(6):251–255. [PubMed] [Google Scholar]
- 139.Llobet JM, Domingo JL, Corbella J. Comparison of antidotal efficacy of chelating agents upon acute toxicity of Co(II) in mice. Res Commun Chem Pathol Pharmacol. 1985;50(2):305–308. [PubMed] [Google Scholar]
- 140.Llobet JM, Domingo JL, Corbella J. Comparative effects of repeated parenteral administration of several chelators on the distribution and excretion of cobalt. Res Commun Chem Pathol Pharmacol. 1988;60(2):225–233. [PubMed] [Google Scholar]
- 141.Levitskaia TG, Morris JE, Creim JA, Woodstock AD, Luders T, Curry TL, Thrall KD. Aminothiol receptors for decorporation of intravenously administered (60)Co in the rat. Health Phys. 2010;98(1):53–60. doi: 10.1097/HP.0b013e3181b9dbbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Levitskaia TG, Creim JA, Curry TL, Luders T, Morris JE, Woodstock AD, et al. Evaluation of Cuprimine and Syprine for decorporation of (60)Co and (210)Po. Health Phys. 2010;98(3):471–479. doi: 10.1097/HP.0b013e3181bcdf4f. [DOI] [PubMed] [Google Scholar]
- 143.Levitskaia TG, Creim JA, Curry TL, Luders T, Peterson JM, Thrall KD, Levinson B. Evaluation of Cuprimine(R) and Syprine(R) for decorporation of radioisotopes of cesium, cobalt, iridium and strontium. Health Phys. 2011;101(2):118–127. doi: 10.1097/HP.0b013e318208ceb6. [DOI] [PubMed] [Google Scholar]
- 144.Management of persons contaminated with radionuclides: handbook. Bethesda: National Council on Radiation Protection and Measurements; 2008. [Google Scholar]
- 145.The medical aspects of radiation incidents. Oak Ridge: REAC/TS; 2013. [Google Scholar]
- 146.Gavrilescu M, Pavel LV, Cretescu I. Characterization and remediation of soils contaminated with uranium. J Hazard Mater. 2009;163(2–3):475–510. doi: 10.1016/j.jhazmat.2008.07.103. [DOI] [PubMed] [Google Scholar]
- 147.Agency for Toxic Substances Disease Registry (ATSDR) (2009) Case Studies in Environmental Medicine (CSEM). Uranium toxicity. US Department of Health and Human Services, Public Health Service, Atlanta. http://www.atsdr.cdc.gov/csem/uranium/docs/uranium.pdf. Accessed 19 Aug 2013
- 148.Toxicological profile for uranium. Atlanta: US Department of Health and Human Services, Public Health Service; 2013. [Google Scholar]
- 149.McDiarmid MA, Engelhardt SM, Dorsey CD, Oliver M, Gucer P, Gaitens JM, et al. Longitudinal health surveillance in a cohort of Gulf War veterans 18 years after first exposure to depleted uranium. J Toxicol Environ Health. 2011;A74(10):678–691. doi: 10.1080/15287394.2011.539138. [DOI] [PubMed] [Google Scholar]
- 150.Pavlakis N, Pollock CA, McLean G, Bartrop R. Deliberate overdose of uranium: toxicity and treatment. Nephron. 1996;72(2):313–317. doi: 10.1159/000188862. [DOI] [PubMed] [Google Scholar]
- 151.Durbin PW, Lauriston S. Taylor Lecture: the quest for therapeutic actinide chelators. Health Phys. 2008;95(5):465–492. doi: 10.1097/01.HP.0000326345.41816.c2. [DOI] [PubMed] [Google Scholar]
- 152.Leggett RW. The behavior and chemical toxicity of U in the kidney: a reassessment. Health Phys. 1989;57(3):365–383. doi: 10.1097/00004032-198909000-00001. [DOI] [PubMed] [Google Scholar]
- 153.Environmental Protection Agency National primary drinking water regulations; radionuclides; final rule. Fed Regist. 2000;65(236):76708–76753. [Google Scholar]
- 154.Occupational Safety and Health Administration (OSHA) (2006) Regulations. Occupational safety and health standards. 29 CFR 1910.1000 Table Z-1. Table Z-1 Limits for Air Contaminants. US Department of Labor, Washington. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=9992. Accessed 3 Sept 2013
- 155.U.S. Nuclear Regulatory Commission (NRC) Guide 8.22—bioassay at uranium mills. Washington: US NRC; 1978. [Google Scholar]
- 156.Gwiazda RH, Squibb K, McDiarmid M, Smith D. Detection of depleted uranium in urine of veterans from the 1991 Gulf War. Health Phys. 2004;86(1):12–18. doi: 10.1097/00004032-200401000-00004. [DOI] [PubMed] [Google Scholar]
- 157.(ORISE) ORIfSaE (2013) Radiation Emergency Assistance Center/Training Site (REAC/TS). Oak Ridge Institute for Science and Education, Oak Ridge. http://orise.orau.gov/reacts/. Accessed 4 Sept 2013
- 158.Sutton M, Burastero SR. Uranium(VI) solubility and speciation in simulated elemental human biological fluids. Chem Res Toxicol. 2004;17(11):1468–1480. doi: 10.1021/tx049878k. [DOI] [PubMed] [Google Scholar]
- 159.Pentetate zinc trisodium injection. Package insert—instruction for use. Hameln: Hameln Pharmaceuticals GmbH; 2004. [Google Scholar]
- 160.Pentetate calcium trisodium injection. Package insert—instruction for use. Hameln: Hameln Pharmaceuticals GmbH; 2004. [Google Scholar]
- 161.Smith VH, Ragan HA (1996) Chelates as contrast media: uranium-DTPA. BNWL-480. BNWL. US Atomic Energy Commission 105–106 [PubMed]
- 162.Khandelwal S, Kachru DN, Tandon SK. Chelation in metal intoxication. IX. Influence of amino and thiol chelators on excretion of manganese in poisoned rabbits. Toxicol Lett. 1980;6(3):131–135. doi: 10.1016/0378-4274(80)90180-0. [DOI] [PubMed] [Google Scholar]
- 163.Tandon SK, Jain VK, Mathur AK. Effect of metal chelators on excretion and tissue levels of essential trace elements. Environ Res. 1984;35(1):237–245. doi: 10.1016/0013-9351(84)90132-4. [DOI] [PubMed] [Google Scholar]
- 164.Cantilena LR, Jr, Klaassen CD. The effect of chelating agents on the excretion of endogenous metals. Toxicol Appl Pharmacol. 1982;63(3):344–350. doi: 10.1016/0041-008x(82)90263-0. [DOI] [PubMed] [Google Scholar]
- 165.Stradling GN, Gray SA, Moody JC, Ellender M. Efficacy of tiron for enhancing the excretion of uranium from the rat. Hum Exp Toxicol. 1991;10(3):195–198. doi: 10.1177/096032719101000308. [DOI] [PubMed] [Google Scholar]
- 166.Abergel RJ, Durbin PW, Kullgren B, Ebbe SN, Xu J, Chang PY, et al. Biomimetic actinide chelators: an update on the preclinical development of the orally active hydroxypyridonate decorporation agents 3,4,3-LI(1,2-HOPO) and 5-LIO(Me-3,2-HOPO) Health Phys. 2010;99(3):401–407. doi: 10.1097/HP.0b013e3181c21273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Abergel RJ, Raymond KN. Multidentate terephthalamidate and hydroxypyridonate ligands: towards new orally active chelators. Hemoglobin. 2011;35(3):276–290. doi: 10.3109/03630269.2011.560771. [DOI] [PubMed] [Google Scholar]
- 168.Raymond KN, Scarrow RC, White DL (1987) Assignee: The United States of America as represented by the United States. Hydroxypyridonate chelating agents. United States Patent 4698431
- 169.Goto K. A study of the acidosis, blood urea, and plasma chlorides in uranium nephritis in the dog, and of the protective action of sodium bicarbonate. J Exp Med. 1917;25(5):693–719. doi: 10.1084/jem.25.5.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Fukuda S, Ikeda M, Nakamura M, Katoh A, Yan X, Xie Y, Kontoghiorghes GJ. The effects of bicarbonate and its combination with chelating agents used for the removal of depleted uranium in rats. Hemoglobin. 2008;32(1–2):191–198. doi: 10.1080/03630260701727093. [DOI] [PubMed] [Google Scholar]