Abstract
Background/Aims
Osteoprotegerin (OPG) and fetuin-A are vascular calcification regulators that may be related to high cardiovascular (CV) mortality in hemodialysis (HD) patients. We evaluated the relationship between OPG, fetuin-A, and pulse wave velocity (PWV), a marker of vascular stiffness, and determined whether OPG and fetuin-A were independent predictors of CV events in HD patients.
Methods
We conducted a prospective observational study in 97 HD patients. OPG and fetuin-A were measured at baseline and arterial stiffness was evaluated by PWV. All patients were stratified into tertiles according to serum OPG levels.
Results
A significant trend was observed across increasing serum OPG concentration tertiles for age, HD duration, systolic blood pressure, cholesterol, triglycerides, and PWV. Multiple linear regression analysis revealed that diabetes (β = 0.430, p = 0.000) and OPG levels (β = 0.308, p = 0.003) were independently associated with PWV. The frequency of new CV events was significantly higher in the upper OPG tertiles compared with those in the lower OPG tertiles. In Cox proportional hazards analysis, upper tertiles of OPG levels were significantly associated with CV events (hazard ratio = 4.536, p = 0.011).
Conclusions
Serum OPG, but not fetuin-A, levels were closely associated with increased vascular stiffness, and higher OPG levels may be independent predictors of new CV events in HD patients.
Keywords: Osteprotegerin, Vascular stiffness, Cardiovascular diseases
INTRODUCTION
Cardiovascular (CV) disease is a major cause of death in uremic patients. Earlier studies have reported that vascular calcification is associated with increased arterial stiffness and may contribute to high CV mortality in end-stage renal disease (ESRD) patients [1,2]. Aortic pulse wave velocity (PWV), which is an index of arterial distensibility, is the gold standard measure of arterial stiffness [3].
Osteoprotegerin (OPG), a soluble decoy receptor of the osteoclast activator, acts as an important regulatory molecule in vascular calcification, independent of classical risk factors [4,5]. Fetuin-A (a2-Heremans-Schmidt glycoprotein) is a systemic inhibitor of ectopic mineral deposition, particularly in chronic kidney disease (CKD) patients, who suffer from progressive arterial calcification [6]. Serum OPG and fetuin-A levels have been associated with the stiffening of large vessel walls, which may contribute to the high CV mortality observed in hemodialysis (HD) patients [7-9]. However, conflicting data on their impact on vascular measures and CV mortality in maintenance HD patients remains to be resolved [10-13].
In this study, we evaluated the link between OPG, fetuin-A and vascular stiffness, and determined whether OPG and fetuin-A levels were associated with the onset of new CV events and all-cause mortality in HD patients.
METHODS
Patients
Ninety-seven patients on chronic HD (54 males, 43 females; mean age, 56.5 ± 12.2 years; range, 28 to 77 years) from the two dialysis units of the University Department of Nephrology at Gangnam Severance Hospital, Seoul, Korea and CHA Bundang Medical Center, CHA University, Seongnam, Korea were enrolled in this prospective observational study between January and March 2008. All participants had been on HD > 3 months (mean dialysis duration, 46 months; range, 6 to 227) and were clinically stable. This study was approved by the Institutional Review Board for human research at Yonsei University College of Medicine, Seoul, Korea, and all participants provided their written informed consent prior to study entry. Patients were followed for a median of 40 months (range, 14 to 42). Medical records were reviewed for clinical history and prior CV events. Primary endpoints were newly developed CV events defined as ischemic heart disease, heart failure, cerebrovascular disease, peripheral vascular disease, and sudden death. Ischemic heart disease (angina pectoris or myocardial infarction) was diagnosed by any of the following: typical angina symptoms, ischemic changes in electrocardiogram or echocardiogram, or coronary artery stenosis confirmed by catheterization. Heart failure was defined by typical symptoms, such as dyspnea, shortness of breath, or raised jugular venous pressure with systolic or diastolic dysfunction by echocardiography in accordance with the guidelines of the European Society of Cardiology [14]. Cerebrovascular disease (transient ischemic attack, cerebral infarction, or cerebral hemorrhage) was confirmed both by typical symptoms with physical findings and by computed tomography (CT) or magnetic resonance imaging. Peripheral vascular disease was diagnosed when the patient had typical symptoms, abnormal ankle brachial pressure index, positive CT or CT angiography findings, or peripheral artery stenosis confirmed by catheterization.
Biochemical measurements
Baseline biochemical parameters, including fasting glucose, lipid profiles, calcium, phosphate, and intact parathyroid hormone (iPTH), were collected prior to midweek dialysis at the time of arterial stiffness measurements. Serum OPG and fetuin-A levels were measured by ELISA using a commercially available kit (R&D Systems, Minneapolis, MN, USA).
Assessment of arterial stiffness
Heart-femoral PWV, which represents aortic stiffness by measuring the time delay between the rapid upstroke of the feet of simultaneously recorded pulse waves in the heart and the femoral arteries [15], was calculated with a VP-2000 pulse wave unit (Nippon Colin Ltd., Komaki, Japan). After a 5-minute rest period, the PWV was measured in a supine position. Carotid and femoral artery pressure waveforms were recorded in multielement tonometry sensors at the left carotid and the left femoral arteries. The electrocardiogram was monitored by electrodes on both wrists. The heart sounds S1 and S2 were detected by a microphone on the left edge of the sternum at the third intercostal space. The waveform analyzer measured the time intervals between S2 and the notch of the carotid pulse wave (Thc), and again between the carotid and femoral artery pulse waves (Tcf). The sum of Thc and Tcf gave the time required for pulse waves to travel from the heart (aortic orifice) to the femoral artery (Thf). The hfPWV was calculated from the equation Lhf / (Thc + Tcf), where Lhf is the distance from the heart to the femoral artery [16].
Statistical analysis
All values are expressed as means ± SD. Pearson correlation analysis was performed to estimate the correlations between OPG, fetuin-A, and other variables. One-way analysis of variance was used to compare each baseline variable among OPG tertile groups. Multiple linear regression analysis was used to evaluate independent predictors of vascular stiffness. Survival was evaluated by Kaplan-Meier curves, and compared using the log-rank test. To estimate the relationship of OPG levels on CV events and all-cause mortality, Cox proportional hazard regression analyses were used. Hazard ratios (HR) are presented with their 95% confidence intervals (CIs) in parentheses. Values of p < 0.05 were considered to indicate statistical significance. Statistical analysis was performed using SPSS version 19.0 for Windows (IBM Co., Armonk, NY, USA).
RESULTS
Baseline characteristics and biochemical data
Fifty-six percent of the study subjects were males. Their ages ranged from 28 to 77 years (mean age, 56.5 ± 12.2). Sixty percent of the patients were diabetic. The causes of ESRD were diabetes (n = 44), hypertension (n = 34), glomerulonephritis (n = 12), polycystic kidney disease (n = 2), and other/unknown (n = 5). The mean OPG concentration was 2,407.0 ± 1,072.5 pg/mL (range, 232 to 5,155). The mean fetuin-A level was 152.4 ± 155.9 mg/mL (range, 7 to 1,372). Twenty patients (20.6%) were smokers. Eighty-two patients (84.5%) received angiotensin-converting enzyme inhibitors or angiotensin-II receptor blockers. Forty-four patients (45.3%) received statin treatment and 33 patients (34.0%) took calcium-based phosphate-binding agents and/or activated vitamin D3. Twenty-four patients (24.7%) had a history of CV disease.
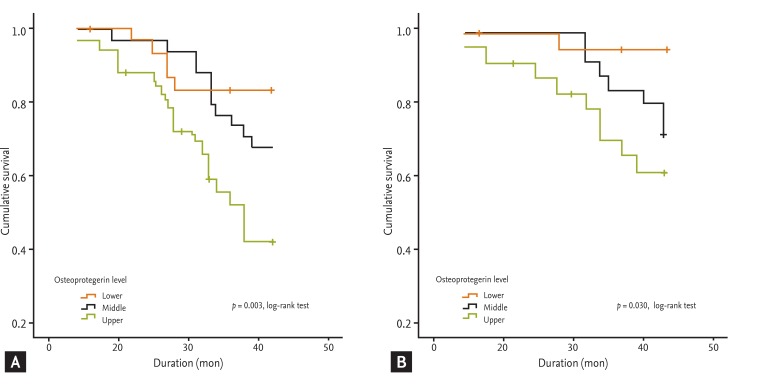
Patients were stratified into tertiles according to serum OPG levels (lower tertile ≤ 1,907 pg/mL; middle tertile 1,908 to 2,737 pg/mL; upper tertile ≥ 2,738 pg/mL). A significant trend of increasing serum OPG concentrations was observed across the tertiles for age (p = 0.000), HD duration (p = 0.009), systolic blood pressure (p = 0.007), cholesterol (p = 0.011), triglycerides (p = 0.012), and PWV (p = 0.034). No significant differences were observed in any other variables across the serum OPG level tertiles (Table 1).
Table 1.
Comparison of biochemical and demographic data according to tertile of osteoprotegerin
Values are presented as mean ± SD or number (%). Serum OPG levels were classified into three groups: ≤ 1,907 pg/mL (lower OPG), 1,908 to 2,737 pg/mL (middle OPG), ≥ 2,738 pg/mL (upper OPG). Analysis of variance between OPG tertiles was performed.
OPG, osteoprotegerin; BMI, body mass index; HD, hemodialysis; DM, diabetes mellitus; SBP, systolic blood pressure; DBP, diastolic blood pressure; iPTH, intact parathyroid hormone; CRP, C-reactive protein; HDL-C, high density lipid cholesterol; LDL-C, low density lipid cholesterol; PWV, pulse wave velocity; CVD, cardiovascular disease; CV, cardiovascular.
ap < 0.05.
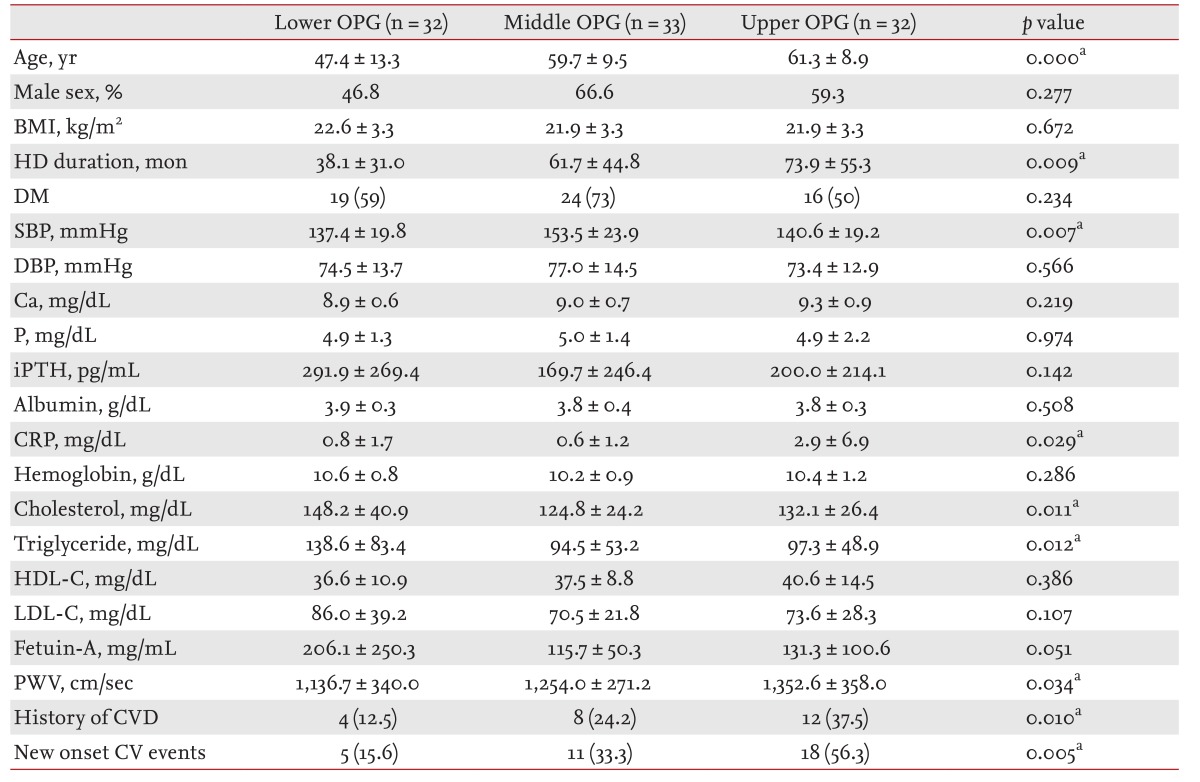
Serum OPG levels showed a linear increase with age (r = 0.486, p = 0.000), HD duration (r = 0.212, p = 0.038), and C-reactive protein (CRP) (r = 0.212, p = 0.040). Moreover, increasing OPG levels were associated with increased PWV (r = 0.291, p = 0.004). Fetuin-A showed no correlations with variables other than total cholesterol (r = 0.227, p = 0.025) and low density lipid cholesterol (LDL-C) (r = 0.223, p = 0.028) (Table 2).
Table 2.
Association between osteoprotegerin, fetuin-A, and biochemical parameters
All associations were tested by means of Pearson correlation analyses.
OPG, osteoprotegerin; iPTH, intact parathyroid hormone; CRP, C-reactive protein; HDL-C, high density lipid cholesterol; LDL-C, low density lipid cholesterol; PWV, pulse wave velocity.
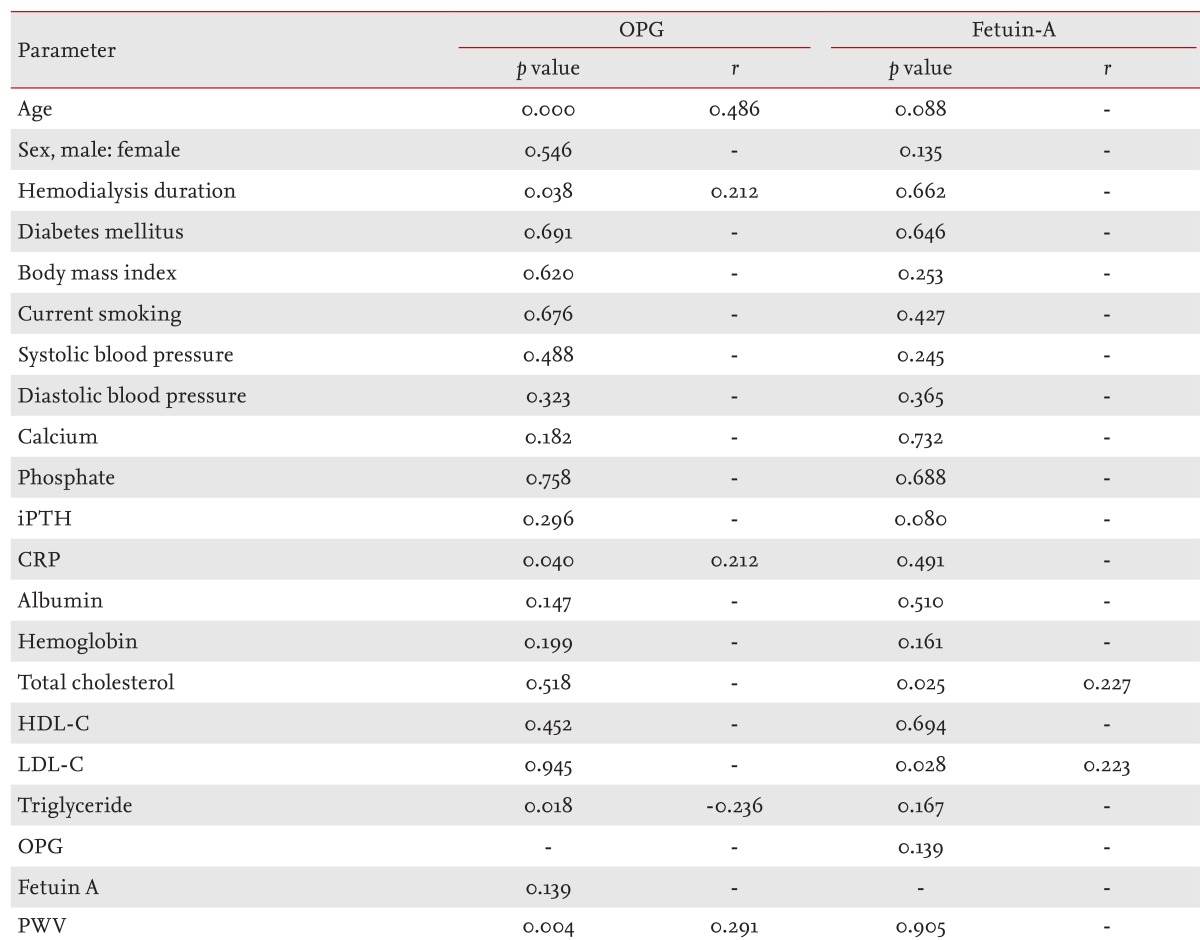
Independent predictors of PWV
In univariate analysis, PWV was positively associated with age (β = 0.319, p = 0.001), diabetes (β = 0.391, p = 0.000), hypertension (β = 0.270, p = 0.007), and OPG levels (β = 0.291, p = 0.004) and negatively associated with hemoglobin levels (β = -0.207, p = 0.042). Among these variables, only diabetes and OPG levels were independently associated with PWV (β = 0.430, p = 0.000; β = 0.308, p = 0.003, respectively) in a multivariate linear regression model (Table 3).
Table 3.
Multiple linear regression analysis of risk factors associated with pulse wave velocity
DM, diabetes mellitus; OPG, osteoprotegerin; CRP, C-reactive protein.
ap < 0.05.
Association between OPG, fetuin-A levels, and CV events
During the 3.5-year follow-up period, 34 patients had 45 new CV events, which included ischemic heart disease (n = 16), heart failure (n = 14), cerebrovascular disease (n = 11), peripheral vascular disease (n = 3), and sudden death (n = 1). Of these 34 patients, seven experienced more than one CV event. During the study period, 18 patients (18.6%) died. Eleven (61.1%) of them were due to CV causes; coronary heart disease (n = 6, 54.5%), heart failure (n = 3, 27.3%), cerebrovascular hemorrhage (n = 1, 9.1%), and sudden cardiac death (n = 1, 9.1%). Non-CV deaths (38.9%) consisted of septic shock (n = 4, 57.1%), gastrointestinal bleeding (n = 1, 14.3%), and malignancy (n = 2, 28.6%).
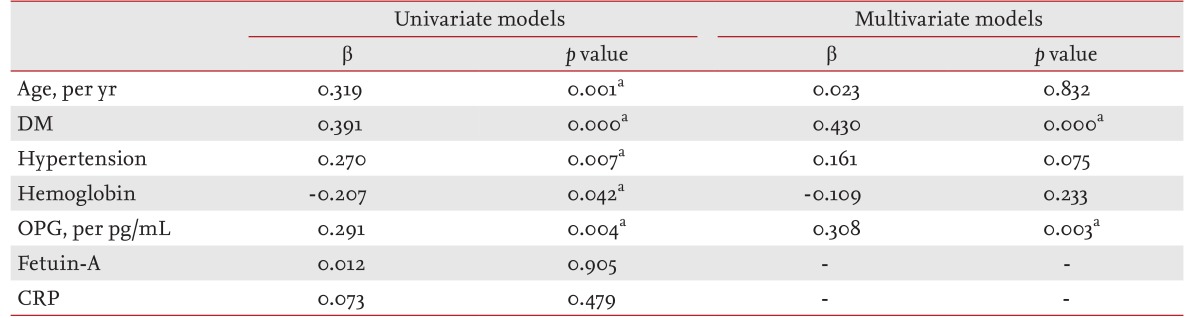
Kaplan-Meier analysis showed that CV events and all-cause mortality were significantly more frequent in the upper OPG tertiles compared with the lower OPG tertiles (p = 0.003 and p = 0.030, respectively, log-rank test) (Fig. 1). In univariate Cox proportional hazard models, the following variables were related to CV events: age (HR = 1.452, p = 0.008), the presence of diabetes (HR = 1.590, p = 0.003), CRP (HR = 1.071, p = 0.003), upper OPG tertiles (HR = 4.342, p = 0.004), and PWV (HR = 1.001, p = 0.047). By contrast, gender, smoking, body mass index, blood pressure, lipid profile, and bone mineral markers were not significantly associated with CV events. In multivariate analysis, only upper tertiles of serum OPG remained a significant predictor of new onset CV events (HR = 4.536, p = 0.011) (Table 4). In univariate analysis for all-cause mortality, associated factors were age (HR = 1.300, p = 0.015), the presence of diabetes (HR = 1.230, p = 0.035), increased PWV (HR = 1.001, p = 0.045), and upper OPG tertiles (HR = 1.550, p = 0.033). In the multivariate Cox hazard models, age was a significant predictor of all-cause death (HR = 1.132, p = 0.010) (Table 5). Furthermore, Kaplan-Meier analysis and Cox proportional hazard models indicated no difference in the frequencies of CV events and all-cause mortality according to fetuin-A level (data not shown).
Figure 1.
Kaplan-Meier analysis of cardiovascular (A) event survival and (B) all-cause mortality in tertiles of serum osteoprotegerin levels.
Table 4.
Cox proportional hazard model for analysis of the risk factors associated with new-onset cardiovascular events
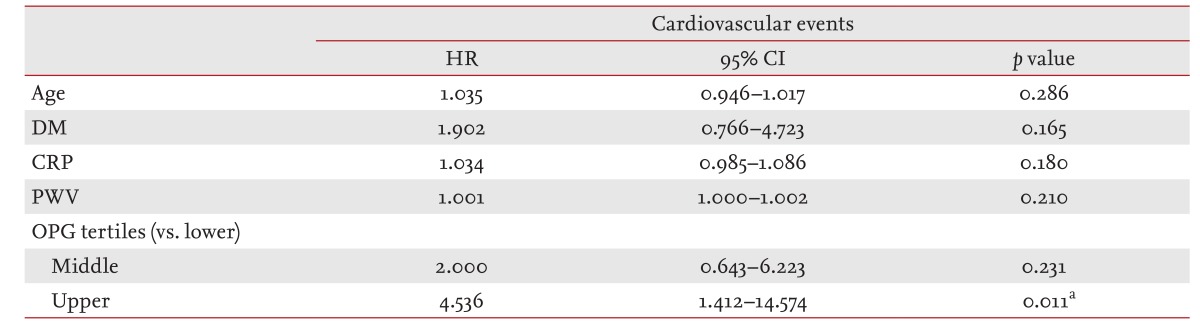
HR, hazard ratio; CI, confidence interval; DM, diabetes mellitus; CRP, C-reactive protein; PWV, pulse wave velocity; OPG, osteoprotegerin.
ap < 0.05.
Table 5.
Cox proportional hazard model for analysis of the risk factors associated with all-cause mortality
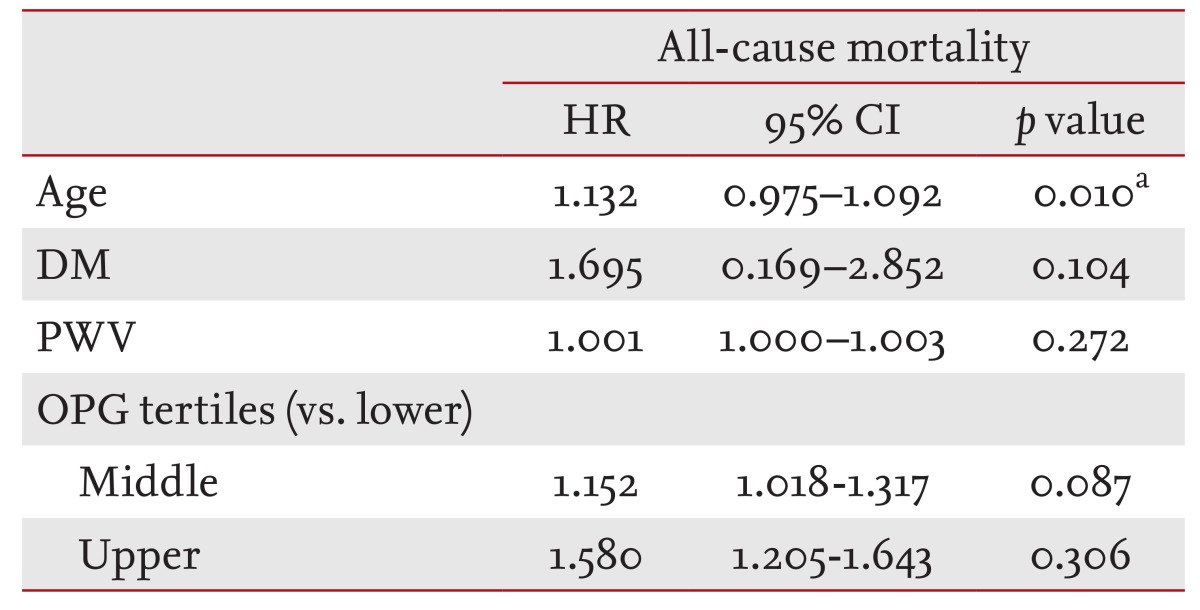
HR, hazard ratio; CI, confidence interval; DM, diabetes mellitus; PWV, pulse wave velocity; OPG, osteoprotegerin.
ap < 0.05.
DISCUSSION
The results of this study indicate that serum OPG levels were associated with arterial stiffness represented by PWV, and that higher OPG levels predict the onset of new CV events in HD patients. In contrast, fetuin-A showed no associations with PWV or CV events in these HD patients.
Recent studies indicate that OPG is associated with PWV in CKD patients [9,10]. However, the data regarding associations of fetuin-A with PWV or CV mortality in these patients are conflicting [8,11,17]. Hermans et al. [11] found no association between circulating fetuin-A and PWV and suggested that fetuin-A was not an independent predictor of aortic stiffness measured by PWV [17]. Here, we assessed serum fetuin-A simultaneously with serum OPG and PWV in HD patients. Several clinical factors such as age, high blood pressure, inflammation, and diabetic status are known to influence vascular stiffness in CKD patients. After adjustment for these factors in this study, only OPG and diabetic status were significantly associated with PWV. These findings support the hypothesis that OPG is significantly associated with arterial stiffness in HD patients. Furthermore, elevated OPG levels were associated with vascular calcification in HD patients [18,19], and vascular calcification of the large arteries was associated with increased risk of CV mortality in these dialysis patients [20]. Sigrist et al. [8] suggested that elevated OPG was associated with a negative outcome in stages four and five CKD patients. Nakashima et al. [9] also showed that OPG was associated with CV mortality, as well as arterial stiffness in normalbuminemic Japanese HD patients. Moreover, high serum OPG was reported to be an independent predictor of CV events in new HD patients [7]. The present study corroborates these earlier findings that significantly associate higher OPG with the onset of new CV events in dialysis patients. This supports the use of serum OPG levels as a predictive marker of vascular stiffness and risk of CV events in HD patients. However, our study failed to show an association between OPG levels and all-cause mortality. This discrepancy may be due to the small sample size of the study, as well as the patients' characteristics, which consisted of younger and more stable patients than in previous studies. Forty-two percent of the patients in our study experienced onset of new CV events; 18% of these patients died within 40 months. In contrast, Nishiura et al. [7] and Nakashima et al. [9] recorded 21% and 26% total deaths, respectively. Thus, the low death rate reported here may have skewed the all-cause morality results, which may differ upon further investigation using a larger sample size with a longer follow-up period.
Fetuin-A is a circulating glycoprotein synthesized in human liver tissue. As a negative acute phase protein in vivo [21], the serum concentration of fetuin-A decreases during both acute and chronic inflammation, such as in dialysis patients [22]. In addition, fetuin-A inhibits systemic calcification, and low circulating fetuin-A levels are associated with high serum phosphate levels in the general population [23,24]. A recent study reported that the fetuin-A level is associated with PWV and calcification [17]. However, Hermans et al. [11] reported that after adjusting for age, gender, mean arterial pressure, and diabetic status, there was no significant relationship between fetuin-A and PWV in dialysis patients. Other reports have failed to correlate fetuin-A and PWV in stage four and five CKD patients [8], similar to the results of this study. The data associating fetuin-A and mortality are also contradictory. Low serum fetuin-A levels were significantly associated with all-cause and CV mortality in ESRD patients [25,26] but not with all-cause mortality and CV mortality in nondiabetic CKD patients [12]. Our results also suggest that fetuin-A was not associated with CV mortality among dialysis patients. Therefore, fetuin-A is not predictive of arterial stiffness and CV mortality in HD patients.
Interestingly, we found that fetuin-A was associated with total cholesterol and LDL-C levels. This finding is consistent with a previous report of positive associations of fetuin-A with LDL-C and nonhigh density lipid cholesterol in nondiabetic HD patients [27]. This association may be due to an inhibitory effect of fetuin-A on adipose tissue, which leads to lipolysis and free fatty acid efflux and suggests that fetuin-A could be a good predictive marker of visceral adiposity in HD patients.
We found no evidence correlating serum OPG levels and mineral metabolism factors, such as calcium, phosphate, and iPTH, as reported previously [28]. These findings suggest that circulating OPG levels might not be indicative of active bone resorption. Furthermore, mineral metabolism factors were not associated with PWV in our study. Previous reports showed a significant association between these two factors [20,29], while another study failed to demonstrate an association [30]. Considering the cross-sectional design of this study, a causal relationship cannot be determined based on one-time measurement of these parameters. Thus, future repeated measurements are warranted to clarify the relationship between OPG levels and mineral metabolism.
There are reports suggesting a strong association between OPG and CRP [31,32]. Morena et al. [33] reported that high OPG levels were a vascular risk factor only in dialysis patients who have high CRP levels. Those findings suggested that OPG might be predictive of poor outcomes only in the presence of inflammation. In our study, OPG and CRP were directly correlated in a univariate analysis. However, after adjustment, OPG levels were not significantly associated with CRP levels. Accordingly, we cautiously suggest that OPG is not a general marker of inflammation.
Our study has several limitations. First, the sample size was relatively small and few patients developed CV mortality during the follow-up period. Thus, a larger patient cohort is necessary to confirm our findings. Secondly, this study was of a cross-sectional design and lacks repeated measurements of both OPG levels and PWV, limiting our ability to determine a causal relationship between OPG and arterial stiffness. However, since we adjusted for multiple risk factors in our analysis, these limitations do not affect our conclusions.
In conclusion, our data suggest that the serum OPG, but not fetuin-A, level was associated with arterial stiffness in HD patients. Moreover, we determined that higher serum OPG levels were independent predictors of the onset of new CV events in HD patients. These findings suggest that serum OPG may be a clinically useful marker for predicting vascular stiffness and that its measurement could facilitate evaluation of the risk of CV events in HD patients.
KEY MESSAGE
1. Serum osteoprotegerin (OPG) and fetuin-A are related to high cardiovascular (CV) mortality in hemodialysis (HD) patients.
2. In our study, serum OPG level, not fetuin-A, was associated with increased vascular stiffness and was independent predictors of new CV events in HD patients.
3. Therefore, we suggest serum OPG may be a useful marker for evaluating the risk of CV events in HD patients.
Acknowledgments
This work was supported in part by a research grant from Korean Institute of Medicine in 2010 to H.C.P.
Footnotes
No potential conflict of interest relevant to this article is reported.
References
- 1.Guerin AP, London GM, Marchais SJ, Metivier F. Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transplant. 2000;15:1014–1021. doi: 10.1093/ndt/15.7.1014. [DOI] [PubMed] [Google Scholar]
- 2.Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM. Arterial calficications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension. 2001;38:938–942. doi: 10.1161/hy1001.096358. [DOI] [PubMed] [Google Scholar]
- 3.Asmar R, Benetos A, Topouchian J, et al. Assesment of arterial distensibility by automatic pulse wave velocity measurement: validation and clinical application studies. Hypertension. 1995;26:485–490. doi: 10.1161/01.hyp.26.3.485. [DOI] [PubMed] [Google Scholar]
- 4.Lacey DL, Dunstan CR, Kelley M, et al. Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell. 1997;89:309–319. doi: 10.1016/s0092-8674(00)80209-3. [DOI] [PubMed] [Google Scholar]
- 5.Lacey DL, Timms E, Tan HL, et al. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998;93:165–176. doi: 10.1016/s0092-8674(00)81569-x. [DOI] [PubMed] [Google Scholar]
- 6.Westenfeld R, Jahnen-Dechent W, Ketteler M. Vascular calcification and fetuin-A deficiency in chronic kidney disease. Trends Cardiovasc Med. 2007;17:124–128. doi: 10.1016/j.tcm.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Nishiura R, Fujimoto S, Sato Y, et al. Elevated osteoprotegerin levels predict cardiovascualr events in new hemodialysis patients. Am J Nephrol. 2009;29:257–263. doi: 10.1159/000157629. [DOI] [PubMed] [Google Scholar]
- 8.Sigrist MK, Levin A, Er L, McIntyre CW. Elevated osteoprotegerin is associated with all-cause mortality in CKD stage 4 and 5 patients in addition to vascular calcification. Nephrol Dial Transplant. 2009;24:3157–3162. doi: 10.1093/ndt/gfp253. [DOI] [PubMed] [Google Scholar]
- 9.Nakashima A, Carrero JJ, Qureshi AR, et al. Plasma osteoprotegerin, arterial stiffness, and mortality in normoalbuminemic Japanese hemodialysis patients. Osteoporos Int. 2011;22:1695–1701. doi: 10.1007/s00198-010-1377-0. [DOI] [PubMed] [Google Scholar]
- 10.Speer G, Fekete BC, El Hadj Othmane T, et al. Serum osteoprotegerin level, carotid-femoral pulse wave velocity and cardiovascular survival in haemodialysis patients. Nephrol Dial Transplant. 2008;23:3256–3262. doi: 10.1093/ndt/gfn242. [DOI] [PubMed] [Google Scholar]
- 11.Hermans MM, Brandenburg V, Ketteler M, et al. Study on the relationship of serum fetuin-A concentration with aortic stiffness in patients on dialysis. Nephrol Dial Transplant. 2006;21:1293–1299. doi: 10.1093/ndt/gfk045. [DOI] [PubMed] [Google Scholar]
- 12.Ix JH, Shlipak MG, Sarnak MJ, et al. Fetuin-A is not associated with mortality in chronic kidney disease. Kidney Int. 2007;72:1394–1399. doi: 10.1038/sj.ki.5002549. [DOI] [PubMed] [Google Scholar]
- 13.Ketteler M, Bongartz P, Westenfeld R, et al. Association of low fetuin-A (AHSG) concentrations in serum with cardiovascular mortality in patients on dialysis: a cross-sectional study. Lancet. 2003;361:827–833. doi: 10.1016/S0140-6736(03)12710-9. [DOI] [PubMed] [Google Scholar]
- 14.Swedberg K, Cleland J, Dargie H, et al. Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology: guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): the task force for the diagnosis and treatment of chronic heart failure of the European Society of Cardiology. Eur Heart J. 2005;26:1115–1140. doi: 10.1093/eurheartj/ehi204. [DOI] [PubMed] [Google Scholar]
- 15.O'Rourke MF, Staessen JA, Vlachopoulos C, Duprez D, Plante GE. Clinical application of arterial stiffness: definitions and reference values. Am J Hypertens. 2002;15:426–444. doi: 10.1016/s0895-7061(01)02319-6. [DOI] [PubMed] [Google Scholar]
- 16.Park S, Kim JB, Shim CY, et al. The influence of serum aldosterone and the aldosterone-renin ratio on pulse wave velocity in hypertensive patients. J Hypertens. 2007;25:1279–1283. doi: 10.1097/HJH.0b013e3280f31b6e. [DOI] [PubMed] [Google Scholar]
- 17.Kuzniar J, Porazko T, Klinger M. Relationship between fetuin-A concentration, elevated levels of inflammatory markers, and arterial wall stiffness in end stage kidney disease. J Ren Nutr. 2008;18:83–86. doi: 10.1053/j.jrn.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 18.Nitta K, Akiba T, Uchida K, et al. The progression of vascular calcification and serum osteoprogerin levels in patients on long-term hemodialysis. Am J Kidney Dis. 2003;42:303–309. doi: 10.1016/s0272-6386(03)00655-3. [DOI] [PubMed] [Google Scholar]
- 19.Barreto DV, Barreto FC, Carvalho AB, et al. Coronary calcification in hemodialysis patients: the contribution of traditional and uremia-related risk factors. Kidney Int. 2005;67:1576–1582. doi: 10.1111/j.1523-1755.2005.00239.x. [DOI] [PubMed] [Google Scholar]
- 20.London GM, Guerin AP, Verbeke FH, et al. Mineral metabolism and arterial functions in end-stage renal disease: potential role of 25-hydroxyvitamin D deficiency. J Am Soc Nephrol. 2007;18:613–620. doi: 10.1681/ASN.2006060573. [DOI] [PubMed] [Google Scholar]
- 21.Lebreton JP, Joisel F, Raoult JP, Lannuzel B, Rogez JP, Humbert G. Serum concentration of human alpha 2 HS glycoprotein during the inflammatory process: evidence that alpha 2 HS glycoprotein is a negative acute-phase reactant. J Clin Invest. 1979;64:1118–1129. doi: 10.1172/JCI109551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stenvinkel P, Wang K, Qureshi AR, et al. Low fetuin-A levels are associated with cardiovascular death: impact of variations in the gene encoding fetuin. Kidney Int. 2005;67:2383–2392. doi: 10.1111/j.1523-1755.2005.00345.x. [DOI] [PubMed] [Google Scholar]
- 23.Luo G, Ducy P, McKee MD, et al. Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature. 1997;386:78–81. doi: 10.1038/386078a0. [DOI] [PubMed] [Google Scholar]
- 24.Schinke T, Amendt C, Trindl A, Poschke O, Muller-Esterl W, Jahnen-Dechent W. The serum protein alpha 2-HS glycoprotein/fetuin inhibits apatite formation in vitro and in mineralizing calvaria cells: a possible role in mineralization and calcium homeostasis. J Biol Chem. 1996;271:20789–20796. doi: 10.1074/jbc.271.34.20789. [DOI] [PubMed] [Google Scholar]
- 25.Metry G, Stenvinkel P, Qureshi AR, et al. Low serum fetuin-A concentration predicts poor outcome only in the presence of inflammation in prevalent haemodialysis patients. Eur J Clin Invest. 2008;38:804–811. doi: 10.1111/j.1365-2362.2008.02032.x. [DOI] [PubMed] [Google Scholar]
- 26.Honda H, Qureshi AR, Heimburger O, et al. Serum albumin, C-reactive protein, interleukin 6, and fetuin a as predictors of malnutrition, cardiovascular disease, and mortality in patients with ESRD. Am J Kidney Dis. 2006;47:139–148. doi: 10.1053/j.ajkd.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 27.Chen HY, Chiu YL, Hsu SP, et al. Association of serum fetuin A with truncal obesity and dyslipidemia in non-diabetic hemodialysis patients. Eur J Endocrinol. 2009;160:777–783. doi: 10.1530/EJE-08-0813. [DOI] [PubMed] [Google Scholar]
- 28.Scialla JJ, Leonard MB, Townsend RR, et al. Correlates of osteoprotegerin and association with aortic pulse wave velocity in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2011;6:2612–2619. doi: 10.2215/CJN.03910411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Raggi P, Bellasi A, Ferramosca E, Islam T, Muntner P, Block GA. Association of pulse wave velocity with vascular and valvular calcification in hemodialysis patients. Kidney Int. 2007;71:802–807. doi: 10.1038/sj.ki.5002164. [DOI] [PubMed] [Google Scholar]
- 30.Haydar AA, Covic A, Colhoun H, Rubens M, Goldsmith DJ. Coronary artery calcification and aortic pulse wave velocity in chronic kidney disease patients. Kidney Int. 2004;65:1790–1794. doi: 10.1111/j.1523-1755.2004.00581.x. [DOI] [PubMed] [Google Scholar]
- 31.Hjelmesaeth J, Ueland T, Flyvbjerg A, et al. Early posttransplant serum osteoprotegerin levels predict long-term (8-year) patient survival and cardiovascular death in renal transplant patients. J Am Soc Nephrol. 2006;17:1746–1754. doi: 10.1681/ASN.2005121368. [DOI] [PubMed] [Google Scholar]
- 32.Kiechl S, Schett G, Wenning G, et al. Osteoprotegerin is a risk factor for progressive atherosclerosis and cardiovascular disease. Circulation. 2004;109:2175–2180. doi: 10.1161/01.CIR.0000127957.43874.BB. [DOI] [PubMed] [Google Scholar]
- 33.Morena M, Terrier N, Jaussent I, et al. Plasma osteoprotegerin is associated with mortality in hemodialysis patients. J Am Soc Nephrol. 2006;17:262–270. doi: 10.1681/ASN.2005030260. [DOI] [PubMed] [Google Scholar]