Abstract
Self-expandable stents are widely available for the treatment of perforation of the gastrointestinal tract. Because of the risk of migration, there has been no report of the use of self-expandable stents for the treatment of perforation of the colon or rectum. This is a report of successful treatment of iatrogenic colonic perforation during balloon dilatation of anastomotic stricture with a fully covered stent. Fully covered, self-expandable metallic stents can be considered useful tools for management of this condition.
Keywords: Colon, Intestinal perforation, Stents
INTRODUCTION
Considerable experience has been reported for the treatment of perforations of the gastrointestinal tract with self-expandable metallic stents (SEMSs). However, to the best of our knowledge, no reports yet exist on the use of covered SEMSs for the treatment of perforation of the colon or rectum. We report a patient with iatrogenic perforation during dilatation of a colonic anastomotic stricture, which was successfully treated with a fully covered SEMS.
CASE REPORT
An 82-year-old man was admitted to our institution for treatment of a colonic anastomotic stricture. He had undergone a laparoscopic left hemicolectomy for cancer of the descending colon. One week after surgery, anastomosis leakage developed, and loop ileostomy was performed. Three months after ileostomy, a colonoscopic exam was performed prior to ileostomy repair, which revealed a stricture at the site of the end to end anastomosis, 17 cm from the anal verge, measuring approximately 3 mm in diameter and 8 mm in length. The patient showed no symptoms.
After bowel enema, the anastomotic stricture was dilated under endoscopic and fluoroscopic guidance, and a guide wire was inserted endoscopically through the stricture site. The controlled radial expansion balloon (5.6 cm in length; CRE Wireguided Balloon Dilator, Boston Scientific Co., Natick, MA, USA) traversed the stricture under fluoroscopic guidance, and the balloon was inflated to a diameter of 15 mm. Just after balloon dilatation, sigmoidoscopy revealed a perforation adjacent to the anastomotic site (Fig. 1). A simple abdominal X-ray showed free air below the diaphragm. A guide wire was inserted via the scope (TTS) method, and a fully covered, colonic, SEMS, 8 cm in length and 20 mm in diameter (Hanarostent, MI Tech Co., Seoul, Korea) was inserted across the stricture under fluoroscopic guidance to completely cover the perforation (Figs. 2 and 3). After the procedure, the patient complained of abdominal pain with no evidence of peritonitis. The patient was managed conservatively with intravenous antibiotics. An endoscopic examination 2 days after the insertion of the stent showed satisfactory re-establishment of luminal continuity (Fig. 4). After 4 days of fasting after the procedure, the abdominal pain resolved and gas was gone. The patient was then put on a diet and remained symptom free. Eight days after the procedure, the patient was discharged.
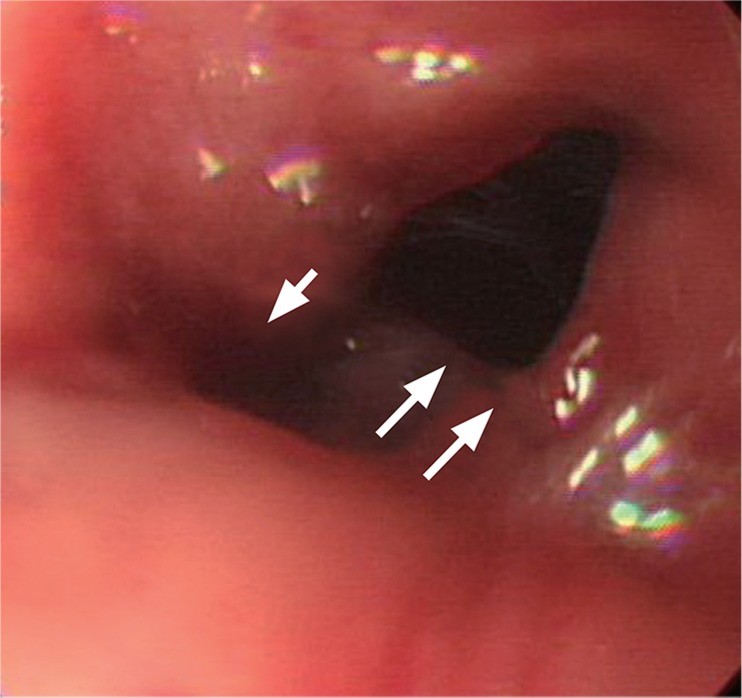
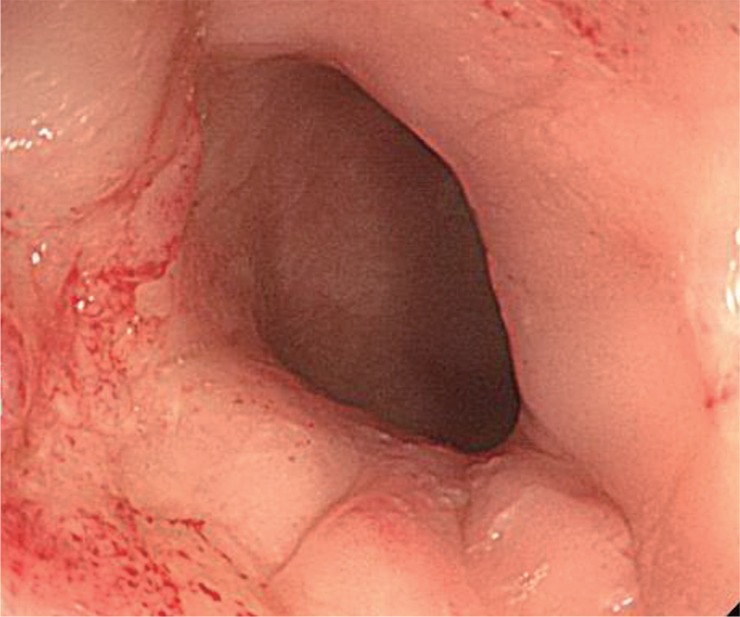
Figure 1.
The 4 mm perforation after balloon dilatation (single arrow); the true lumen of the anastomotic site is noted (double arrows).
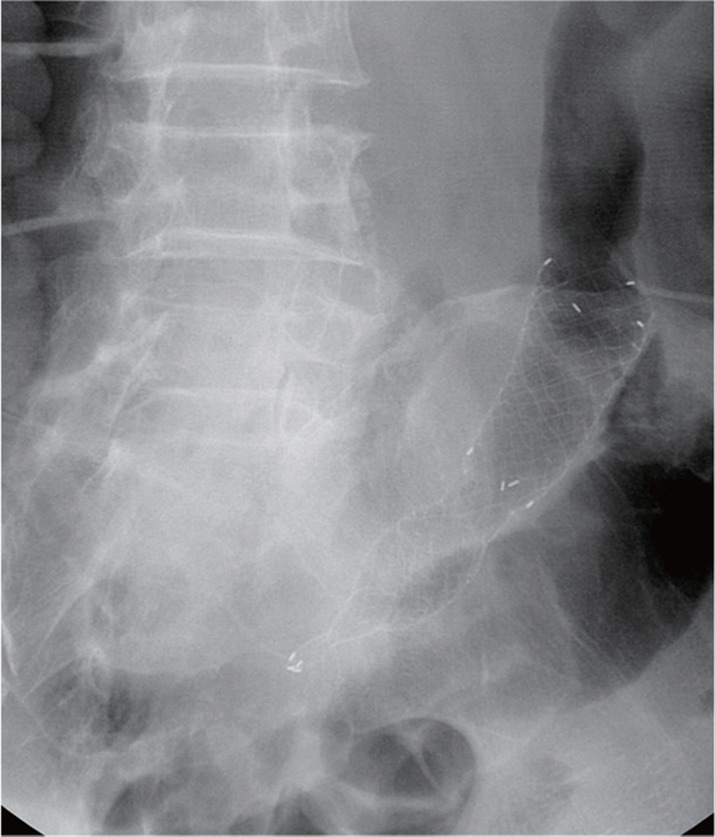
Figure 2.
Successful insertion of a covered colonic metal stent at the site of perforation.
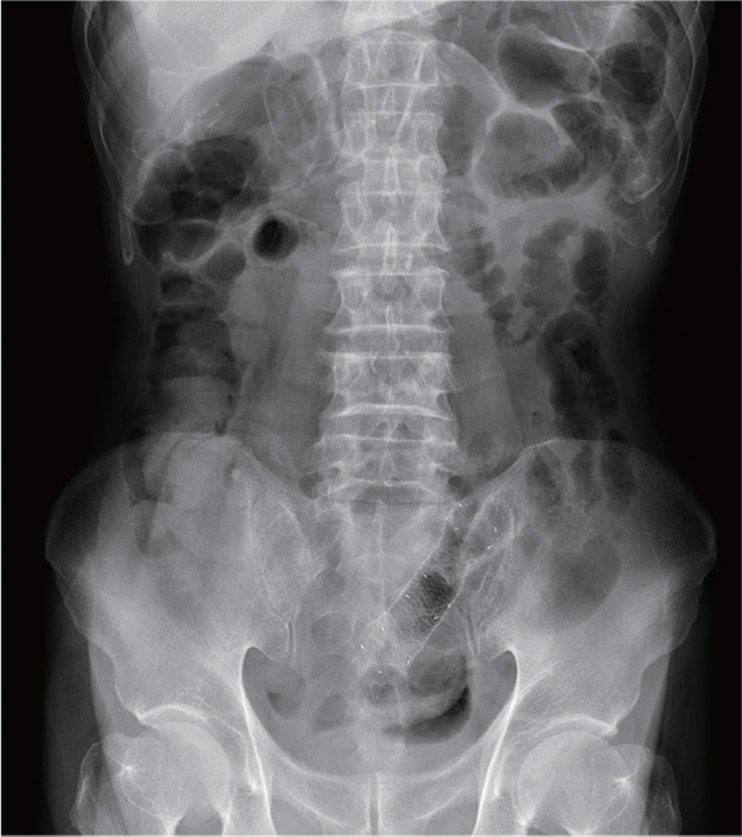
Figure 3.
Successful placement of covered metal stent.
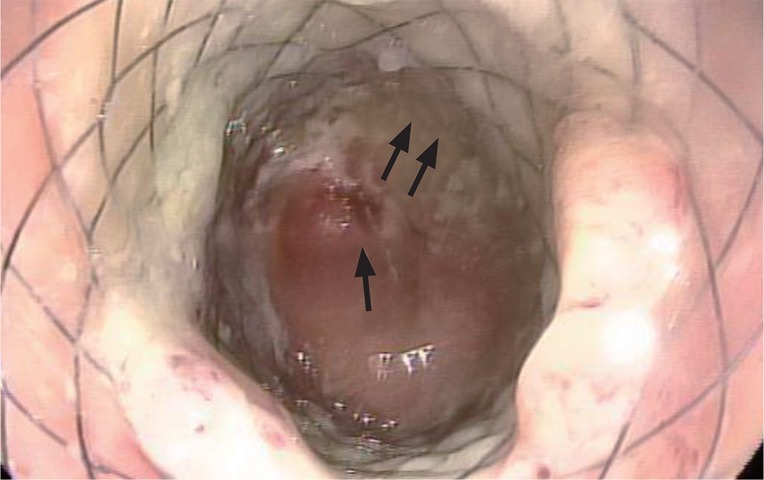
Figure 4.
Follow-up sigmoidoscopy showed a covered metal stent with patent lumen (single arrow) at previous perforation site (double arrows).
The stent was successfully removed 3 weeks after placement, with no complications. Follow-up sigmoidoscopy showed that the perforation had healed completely (Fig. 5). Two months after the procedure, repair of the ileostomy was performed. The patient did not complain of any difficulty with defecation, and there was no evidence of recurrence of the anastomotic stricture.
Figure 5.
Sigmoidoscopy 3 weeks after stent insertion showed completely healed perforation.
DISCUSSION
Traditionally, surgery has been the standard treatment for iatrogenic perforation [1]. Iatrogenic perforation of the colon is a rare but serious and feared complication. A review of endoscopic dilatation procedures showed that bowel perforation was reported in 2% of patients [2]. Recently, endoscopic intervention has become popular as a noninvasive method for closing the site of an iatrogenic colon perforation with clean bowel perforation [3].
Fully covered SEMSs have been used in patients with obstructive colorectal cancer as a palliative procedure and a bridge to surgery [4]. Fully covered SEMSs are removable after the resolution of obstruction, in contrast to partially covered or uncovered stents. Removing partially covered or uncovered SEMSs is itself a risk for perforation or laceration of the colon. Therefore, fully covered SEMS can be a good option for the treatment of colonic perforation. However, the efficacy and associated complications of fully covered SEMSs for the treatment of iatrogenic perforation have not been fully clarified. Because the diameter of the bowel is large, the migration of a fully covered stent is more likely to occur, as compared to uncovered or partially covered stents.
In our patient, no stent migration occurred after its placement to rectify a colonic anastomotic stricture. The straight shape of the lower colon and the perpendicular plane of the anastomosis site may have held the stent effectively. It seems that the short stricture and low anastomosis in this patient were the optimal circumstances to impede migration. In the case of minor colonic perforation, conservative treatments are often sufficient, but for this patient, who showed obvious perforation detected by endoscope, medical treatment with SEMS insertion, fasting, and antibiotics seemed to be adequate. Operative management may be the treatment of choice in most cases, but considering our patient's age and perioperative risk, we performed SEMS insertion instead of operative management. SEMS insertion is a useful, minimally invasive therapy that can be effectively used to treat an iatrogenic colon perforation. However, there is a probability of migration of the stent and subsequent colonic perforation due to the stent [5]. SEMS insertion can only be applied to distal colon perforations with anastomotic stricture. Minimal perforation, which can be treated by conservative measures, and perforation without stricture or perforation of the proximal colon are not candidates for fully covered SEMSs.
In summary, this is a case in which the placement of a SEMS effectively managed a colon perforation in a patient with colonic stricture of benign etiology. It is not certain that SEMSs can be utilized in all colonic perforations because of the high probability of migration. However, anastomotic stricture and low positioning may have prevented stent migration in this case. Therefore, fully covered SEMSs can be considered useful tools for the management of iatrogenic colonic perforations with anastomotic stricture. More cases regarding the use of fully covered SEMSs in various circumstances will be necessary to reveal its usefulness and limitations.
Footnotes
No potential conflict of interest relevant to this article is reported.
References
- 1.Luning TH, Keemers-Gels ME, Barendregt WB, Tan AC, Rosman C. Colonoscopic perforations: a review of 30,366 patients. Surg Endosc. 2007;21:994–997. doi: 10.1007/s00464-007-9251-7. [DOI] [PubMed] [Google Scholar]
- 2.Delaunay-Tardy K, Barthelemy C, Dumas O, Balique JG, Audigier JC. Endoscopic therapy of benign colonic post-operative strictures: report on 27 cases. Gastroenterol Clin Biol. 2003;27:610–613. [PubMed] [Google Scholar]
- 3.Celestino C, Harz C, Decaestecker J, Saenz R. Endoscopic treatment of an iatrogenic perforation of the colon by using endoloop. Gastrointest Endosc. 2006;64:653–654. doi: 10.1016/j.gie.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 4.Khot UP, Lang AW, Murali K, Parker MC. Systematic review of the efficacy and safety of colorectal stents. Br J Surg. 2002;89:1096–1102. doi: 10.1046/j.1365-2168.2002.02148.x. [DOI] [PubMed] [Google Scholar]
- 5.Namdar T, Raffel AM, Topp SA, et al. Complications and treatment of migrated biliary endoprostheses: a review of the literature. World J Gastroenterol. 2007;13:5397–5399. doi: 10.3748/wjg.v13.i40.5397. [DOI] [PMC free article] [PubMed] [Google Scholar]