Abstract
Temporomandibular joint dislocation is defined as the movement of condyle out of the fossa and the advancement of the posterior surface of the condyle in front of the articular eminence. If this condition becomes chronic, surgical treatment is the only option. The goal of surgical treatment is to reposition the condyle and prevent further recurrences. In this study, a retrospective analysis is presented examining 73 patients and 83 joints that were treated with hook-shaped miniplates and miniscrews fixed to otolog bone grafts. Records were obtained from archives of the Uludag University Medical Faculty, Plastic, Reconstructive and Aesthetic Surgery Department. The duration of postoperative follow-up was 3–30 months. In one case, the miniplate was fractured, and in two cases, abscesses existed. This study aims to emphasize that using miniplates and otolog bone grafts is more cost effective.
Keywords: Temporomandibular joint, Recurrent dislocation, Bone graft, Miniplate and miniscrews
Introduction
The temporomandibular joint (TMJ) is formed between the mandibular recess, the articular protrusion of the temporal bone and the condyle of the mandible. The TMJ is a group of synovial and movable joints. The TMJ is associated with certain movements, such as protraction (sliding of the mandible head to the front), retraction (sliding of the mandible head to the back), elevation (closing of the jaw), depression (opening of the jaw) and lateralization.
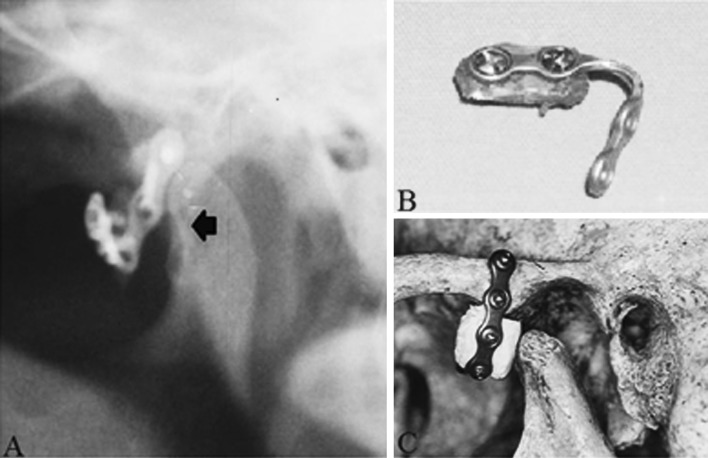
TMJ dislocation occurs when the condyle moves out of the fossa, and the posterior articulating surface of the condyle advances in front of the articular eminence (Fig. 1). If this dislocation occurs as a chronic or recurrent condition, conservative treatment is not successful in a majority of patients, and surgical treatment remains the only option [1–4]. The treatment of recurrent TMJ dislocation has been varied and is aimed at repositioning the condyle and preventing further recurrences.
Fig. 1.
Left TMJ dislocation. Cadaver image (A). Panogram image (B) of condyle (white arrow) and articular eminence (black arrow)
Materials and Methods
A retrospective analysis of 73 patients and 83 joints that were treated with calvarial or iliac bone grafts and hook-shaped miniplates with miniscrews between June 2004 and June 2010 is presented in this study. The records of the Uludag University Medical Faculty, Plastic, Reconstructive and Aesthetic Surgery Department archive were used. Of a total of 73 patients, 59 were females, and 14 were males. The patients’ mean age was estimated at 31.8, ranging from 15 to 76. After a diagnostic physical examination, a panoramic mandible radiograph was performed. Inclusion criteria for surgery were the limitation of jaw movements or regional pain while eating, prominent dislocation on a panoramic mandible radiograph while speaking or smiling, each time the mouth was opened, and failure of conservative treatment methods and dislocation of the TMJ each time the mouth was opened.
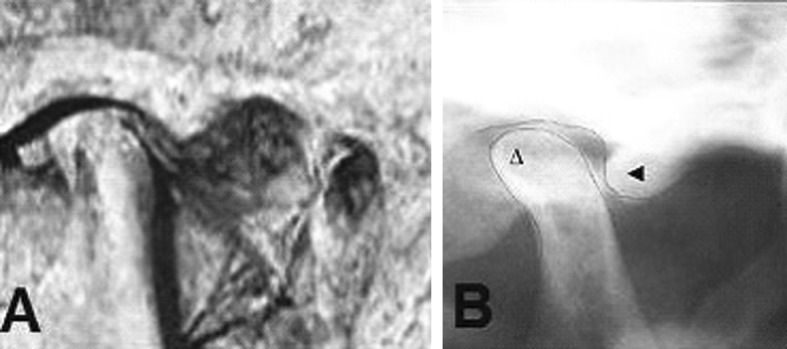
Surgery was performed under general anesthesia with a preauricular approach using a technique similar to that previously described by Ellis and Zide [5]. A miniplate was shaped like a hook, and a bone graft, harvested from the iliac or calvarial bone, was placed and fixed into the concave site of the hook-shaped miniplate with miniscrews. The articular eminence periosteum was elevated with a bone dissector. The miniplate was fixed to the anteroinferior of the articular eminence. With a forced opening of the mouth, the condyle was unable to advance beyond the articular eminence (Fig. 2).
Fig. 2.
Blockade of left condyle. Panoramic image of left condyle (black arrow) (A), bone graft fixed to miniplate (B), Cadaver image of block (C)
Results
The duration of the postoperative follow-up period was 3–30 months. The mean maximal mouth opening (MMO) was estimated at 38 mm (Fig. 3). A number of the patients experienced pain, which subsided with analgesics. In one case, the miniplate was fractured, and a second operation was performed. In two cases, abscesses existed. In one case, although there were two surgical operations, the complaints did not subside, and steroids were injected into the joint. Although in one case, a temporary paralysis of the frontal branch of the facial nerve was observed for 3 months, permanent facial nerve paralysis was not observed in any case. Performing substantial postoperative physiotherapy prevented osteoarthrosis of the TMJ. A permanent joint sound was not observed at 1 year of follow-up.
Fig. 3.
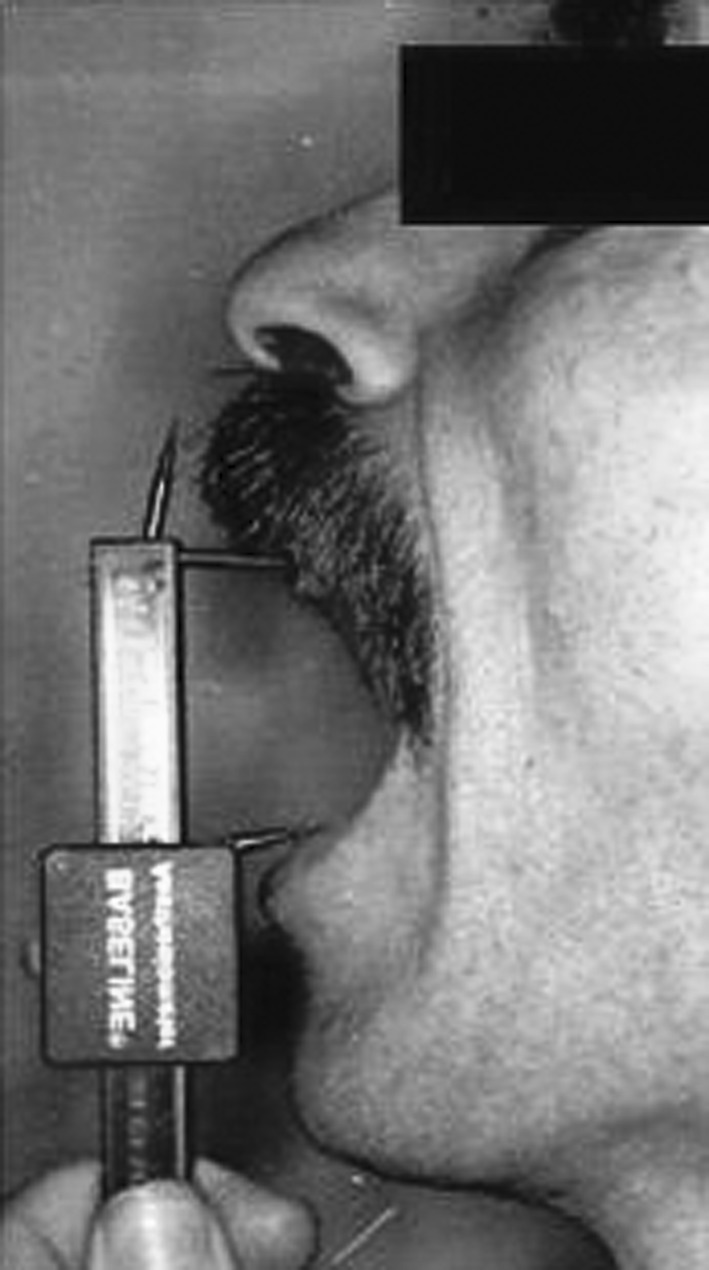
Maximal mouth opening (MMO)
Discussion
Recurrent TMJ dislocation is a common disease of TMJ. The primary treatment is the removal of the etiological factors of dislocation such as occlusion and psychological problems. Recurrent TMJ dislocations cause the surrounding tissue and bone structure to degenerate. In such a situation, conservative treatment is not successful. For the treatment of recurrent TMJ dislocation, many methods are attempted for the articular eminence, condyle or soft tissue [3–13].
According to the literature, capsulorrhaphy, meniscectomy, eminectomy, capsular ligament placation and shortening are useful methods for the treatment of TMJ dislocation. However, after a period of time, the dislocation can relapse. Condylectomies, mandibular shortening and ankylosis, and the down-fracture of the zygomatic arch have complications, such as facial asymmetry and a limited degree of jaw movement [2, 14, 15].
A block prepared with miniplates, screws and otolog bone grafts that are harvested from the temporal or iliac bones is fixed to the articular eminence with miniplates. The forward excursion of the condylar head is limited with this implant. Otolog bone grafts reduce rejection. However, the miniplate is a foreign body and has a cost. Additionally, the presence of facial nerve paralysis is a disadvantage of this technique. A miniplate fixed to the articular eminence decreases MMO, which is another disadvantage.
When conservative treatment methods are ineffective for a recurrent TMJ dislocation, surgery is the only option. Treatment with otolog bone grafts and miniplates is more cost-effective than other operation techniques that can relapse.
References
- 1.Greenberg SA, Jacobs JS, Bessette RW. Temporomandibular joint dysfunction: evaluation and treatment. Clin Plast Surg. 1989;16:707–724. [PubMed] [Google Scholar]
- 2.Zide BM. The temporomandibular joint. In: McCarthy JG, editor. Plastic surgery. Philadelphia: W B Saunders Company; 1991. pp. 247–270. [Google Scholar]
- 3.David LR, Marks MW, Argenta LC. Temporalis fascialis sling—a surgical technique for the treatment of recurrent dislocation of the temporomandibular joint. Eur J Plast Surg. 1998;21:411–414. doi: 10.1007/s002380050130. [DOI] [Google Scholar]
- 4.Georgiade DDS. The surgical correction of chronic luxation of the mandibular condyle. Plast Reconstr Surg. 1965;36:339–342. doi: 10.1097/00006534-196509000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Ellis E, Zide MF. Surgical approaches to the facial skeleton. Media: Lippincott Williams & Wilkins; 1995. [Google Scholar]
- 6.Karaca C, Barutçu A, Atabey A, Özaksoy D, Menderes A. Treatment of temporomandibular joint ankylosis with inverted T-shaped silicone implants. Eur J Plast Surg. 1996;19:112–113. doi: 10.1007/BF00207931. [DOI] [Google Scholar]
- 7.Zins JE, Smith JD, James DR. Surgical correction of temporomandibular joint ankylosis. Clin Plast Surg. 1989;16:725–732. [PubMed] [Google Scholar]
- 8.Hale RH. Treatment of recurrent dislocation of the mandible: review of literature and report of cases. J Oral Surg. 1972;14:527–530. [PubMed] [Google Scholar]
- 9.Buckley MJ, Terry BC. Use of bone plates to manage chronic mandibular dislocation: report of cases. J Oral Maxillofac Surg. 1988;46:998–1002. doi: 10.1016/0278-2391(88)90337-0. [DOI] [PubMed] [Google Scholar]
- 10.Karabouta I. Increasing the aticular eminence by the use of blocks of porous coralline hydroxylapatite for treatment of recurrent TMJ dislocation. J Craniomaxfac Surg. 1990;18:107–113. doi: 10.1016/S1010-5182(05)80325-7. [DOI] [PubMed] [Google Scholar]
- 11.Puelacher WC, Waldhart E. Miniplate eminoplasty: a new surgical treatment for TMJ-dislocation. J Craniomaxfac Surg. 1993;21:176–178. doi: 10.1016/S1010-5182(05)80109-X. [DOI] [PubMed] [Google Scholar]
- 12.Sevin K, Saray A, Askar İ. Treatment of temporomandibular dislocation. Ann Plast Surg. 1998;40:569–570. doi: 10.1097/00000637-199805000-00025. [DOI] [PubMed] [Google Scholar]
- 13.Undt G, Kemer C, Rasse M. Treatment of recurrent mandibular dislocation 2. Eminectomy. Int J Oral Maxillofac Surg. 1997;26:98–102. doi: 10.1016/S0901-5027(05)80825-2. [DOI] [PubMed] [Google Scholar]
- 14.Georgiade NG. Disturbances of the temporomandibular joint. In: Converse JM, editor. Reconstructive plastic surgery. Philadelphia: W B Saunders Company; 1977. pp. 1438–1452. [Google Scholar]
- 15.Jacobs JS, Bessette R. Temporomandibular joint deformities. In: Smith JW, Aston SJ, editors. Grabb and Smith’s plastic surgery. Boston: Little, Brown and Company; 1991. pp. 247–270. [Google Scholar]