Abstract
The external knee adduction moment is considered a surrogate measure for the medial tibiofemoral contact force and is commonly used to quantify the load reducing effect of orthopedic interventions. However, only limited and controversial data exist about the correlation between adduction moment and medial force. The objective of this study was to examine whether the adduction moment is indeed a strong predictor for the medial force by determining their correlation during gait. Instrumented knee implants with telemetric data transmission were used to measure tibiofemoral contact forces in nine subjects. Gait analyses were performed simultaneously to the joint load measurements. Skeletal kinematics, as well as the ground reaction forces and inertial parameters, were used as inputs in an inverse dynamics approach to calculate the external knee adduction moment. Linear regression analysis was used to analyze the correlation between adduction moment and medial force for the whole stance phase and separately for the early and late stance phase. Whereas only moderate correlations between adduction moment and medial force were observed throughout the whole stance phase (R2 = 0.56) and during the late stance phase (R2 = 0.51), a high correlation was observed at the early stance phase (R2 = 0.76). Furthermore, the adduction moment was highly correlated to the medial force ratio throughout the whole stance phase (R2 = 0.75). These results suggest that the adduction moment is a surrogate measure, well-suited to predicting the medial force ratio throughout the whole stance phase or medial force during the early stance phase. However, particularly during the late stance phase, moderate correlations and high inter-individual variations revealed that the predictive value of the adduction moment is limited. Further analyses are necessary to examine whether a combination of other kinematic, kinetic or neuromuscular factors may lead to a more reliable prediction of the force magnitude.
Introduction
Osteoarthritis (OA) of the knee joint is a common disease which is accompanied by pain and impaired mobility. Among others, joint loading is one factor that can influence the development and progression of OA [1], [2]. The increased incidence of medial compartment OA is therefore thought to result from higher loading of the medial compartment [3].
A common indirect measure of the medial tibiofemoral contact force (Fmed) is the external knee adduction moment (EAM). This moment is mainly determined by the ground reaction force and its lever arm to the knee joint center. By passing medially to the knee joint center, the force vector creates an adduction moment that is thought to increase the medial compartment load [4]. Studies have shown that the EAM is related to limb alignment [5]–[8], bone mineral density of the proximal tibia [6] and the progression of OA [7], [9]. Due to these findings and a lack of methods for a direct assessment of Fmed, numerous studies have assessed the effect of OA treatments such as laterally wedged shoes, valgus braces and high tibial osteotomies, by analyzing changes of the EAM [7], [10], [11]. However, while there is indirect evidence that the EAM and the actual loads transferred through the medial tibiofemoral compartment are related, the quantitative relationship between EAM and Fmed is not well established.
Using an analytical computer model, Shelbourne and co-workers compared EAM reduction when walking with braces and wedged shoes to the associated changes of Fmed and found that the relative reduction of the peak EAM was 2–3 times higher than that of Fmed [12]. However, accurate consideration of muscle co-contraction and validation of such modeling approaches to determine the tibiofemoral contact forces remain challenging [13], [14]. Using an instrumented knee implant, medial contact forces were measured in one patient in vivo by Zhao and co-workers and compared to the EAM [15]. In this elderly male patient, the study found a moderate correlation between EAM and Fmed during the stance phase of gait with a coefficient of determination R2 that varied between 0.53 and 0.75. Further analyses in the same subject sought to determine whether a reduction of the peak EAM correlates to a reduction of the peak medial force [16], [17]. Using an intervention shoe with greater lateral sole stiffness, the 1st and 2nd peak values of the EAM during the stance phase were found to be reduced by 13% and 22%, respectively, and the reduction of the 1st peak EAM correlated significantly to the reduction of Fmed (R2 = 0.67) [16]. However, this finding could not be confirmed in another study on the same subject in which the gait patterns were modified using walking poles and a ‘medial thrust’ gait [17]. Although the 1st peak EAM was reduced by 32–33%, these reductions did not correspond to reductions of the 1st peak Fmed. These contradictory results highlight the need for further investigation on the predictive value of the EAM for the medial compartment load. Moreover, these parameters were measured in only one subject. The results from more comprehensive in vivo measurements clearly demonstrated substantial inter-individual variation of the tibiofemoral joint contact forces [18]–[20]. Furthermore, we found considerable inter-individual variation in force reductions that resulted from load-altering interventions, such as valgus braces or wedged shoes [21], [22]. To determine whether this inter-subject variability is reflected by the EAM, analyses in a larger sample of subjects are needed.
Therefore, the aim of this study was to examine whether the EAM is a strong predictor for Fmed by analyzing the correlation between both measures during gait in a larger sample of subjects with telemetric knee implants.
Materials and Methods
Instrumented knee implant
Instrumented knee implants with telemetric data transmission were used to measure the tibiofemoral contact forces and moments in vivo [23]. The implants are based on the Innex FIXUC system (Zimmer GmbH, Winterthur, Switzerland), a cruciate sacrificing design with an ultracongruent tibial inlay. The tibial component was modified and equipped with six strain gauges to measure the load-dependent strains in the implant. All signals are sensed and transmitted by a custom-made, inductively powered telemetry circuit [24]. After calibration of each implant, three force components (Fz: axial force, Fx: medio-lateral shear force, Fy: antero-posterior shear force) and three moment components (Mx: flexion-extension, My: varus-valgus, Mz: internal-external rotation) can be measured at a sampling rate of 100 Hz.
The axial force Fz, is transferred by the medial and lateral compartment. Since the moment My is caused by the axial force acting eccentrically on the tibia, with a lever arm in the medio-lateral direction, the medial contact force Fmed can be calculated as follows:
 l: distance between the medial and lateral condyle
l: distance between the medial and lateral condyle
Accuracy tests showed that Fmed can be determined with an error below 3% for forces |Fz|>1000 N [20]. Therefore, Fmed was only analyzed during the stance phase of gait and values of |Fz|>1000 N. Furthermore, the medial force ratio (MR) Fmed/|Fz|, i.e., the percentage of the axial force that is transferred by the medial compartment, was calculated.
Ethics statement
This study was approved by the ethics committee of the Charité – Universitätsmedizin Berlin. Nine patients with osteoarthritis provided written informed consent to the procedures and received an instrumented knee implant (Table 1).
Table 1. Subject data.
| Subject | K1L | K2L | K3R | K4R | K5R | K6L | K7L | K8L | K9L |
| Sex | m | m | m | f | m | f | f | m | m |
| Age [years] | 64 | 74 | 71 | 67 | 62 | 67 | 76 | 72 | 76 |
| Body mass [kg] | 100 | 90 | 92 | 102 | 95 | 81 | 69 | 78 | 108 |
| Height [m] | 1.77 | 1.71 | 1.75 | 1.70 | 1.75 | 1.74 | 1.66 | 1.74 | 1.66 |
| Tibio-femoral angle [degree] | 3.0 varus | 5.0 varus | 3.5 varus | 4.5 valgus | 1.0 varus | 4.0 valgus | 6.5 varus | 4.0 varus | 7.0 varus |
Gait analysis
Gait analysis was performed simultaneously with the in vivo force measurement at 27±13 months after surgery. All subjects were walking barefoot at a self-selected comfortable speed on a 10 m long walkway. Ground reaction forces were measured using two 6 degrees of freedom force plates (AMTI, Watertown, MA). Three-dimensional kinematics of the lower limb were tracked at 120 Hz using a 10-camera motion capture system (Vicon, Oxford, UK). A set of 46 reflective markers was used [25]. The complete procedure to determine the skeletal kinematics conditions has been described previously [13]. The segment and joint kinematics, as well as the ground reaction forces and inertial parameters, were used as inputs in an inverse dynamics approach to yield the inter-segmental resultant moments [26], [27]. To calculate the gait velocity, the instances of heel contacts were determined based on the heel marker trajectories.
Data evaluation
A total of 54 trials (6 trials per subject) were analyzed. Joint contact and ground reaction forces were normalized to bodyweight (%BW) and moments to bodyweight and height (%BWHt).
Regression analysis (SPSS Inc., Chicago, IL, version 18) was used to determine the correlation between EAM and Fmed and the correlation between EAM and MR. To describe the correlation, coefficients of determination (R2) and root-mean-square (RMS) errors between the predicted and observed values of Fmed were calculated. A linear relationship was assumed between EAM and Fmed and between EAM and MR, for regression analysis. Because the medial force ratio cannot exceed 100% or fall below 0%, the following arcus tangent function with asymptotic boundaries at 0 and 100% was additionally used for modeling the relationship between EAM and MR:
The correlation between EAM and Fmed was analyzed throughout the whole stance phase (for |Fz|>1000 N), followed by a separate analysis of the early and late stance phase. The local minimum of the axial ground reaction force at mid stance was taken to distinguish early from late stance phases. Furthermore, the correlations between EAM and Fmed or MR were analyzed at the two instants of peak medial forces. The correlations were tested for significance considering α = 0.05. A correlation was rated to be good, moderate or poor for a coefficient of determination of R2≥0.75, R2<0.75 and >0.5, and R2≤0.5, respectively.
In order control for the potentially confounding influence of gait velocity and static frontal plane (varus-valgus) limb alignment, further hierarchical multiple regression analyses were performed, where either gait velocity (model i) or alignment (model ii) or both (model iii) were considered as covariates with the EAM as independent and Fmed as dependent variable.
Results
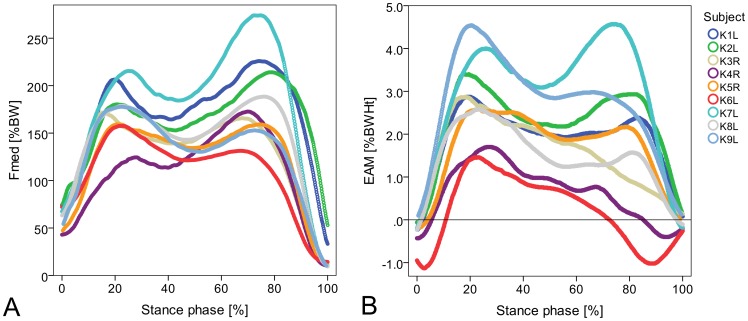
The subjects were walking with an average gait velocity of 1.13 m/s (range: 0.90–1.23 m/s). Clearly discernible peaks of Fmed occurred at 23±4% and 73±4% of the stance phase of gait (Figure 1A). On average, the peak medial forces during late stance (187±44%BW) were somewhat larger than those observed during early stance (176±27%BW). The pattern of the EAM did not generally resemble the pattern of Fmed. Whereas a first distinct peak of the EAM was observed in all subjects at early stance, only six subjects also exhibited a clearly discernible peak at late stance (Figure 1B). At the time of the 1st and 2nd peak of Fmed, EAM values of 2.9±1.0%BWHt and 2.1±1.3%BWHt were determined, respectively.
Figure 1. Medial contact forces Fmed (A) and external adduction moments EAM (B) during the stance phase of gait.
Forces are given in % of bodyweight (BW) and moments in %BW times height (Ht). Average curves from 6 repeated trials per subject were calculated using a dynamic time warping procedure [36].
Correlation between external moments and internal forces throughout the stance phase
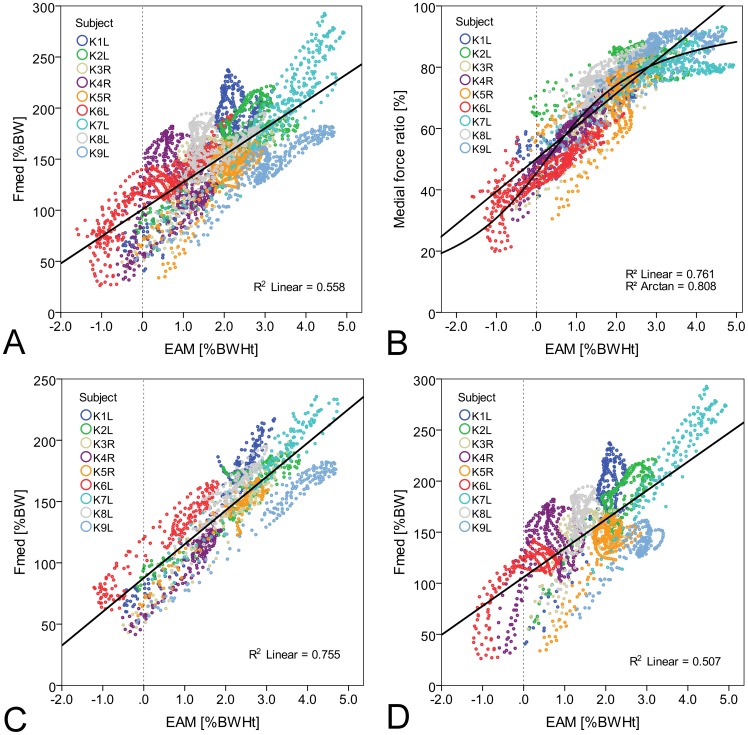
Throughout the whole stance phase (Figure 2A) the coefficient of determination was moderate (R2 = 0.56) and the RMS error amounted to 28%BW. When analyzing the correlation between EAM and Fmed separately for each subject, good correlations were observed in three subjects, moderate correlations in four subjects and poor correlations in the remaining two subjects (Table 2). Moreover, the slopes of the regression lines, the y-intercept values and the RMS errors varied strongly between the subjects.
Figure 2. Correlation between external adduction moments EAM and medial contact forces Fmed during gait.
Correlation between EAM and Fmed during the whole (A), early (C) and late (D) stance phase of gait and correlation between EAM and medial force ratio (B) during the whole stance phase (6 trials per subject).
Table 2. Correlations between external adduction moment and medial contact force during gait.
| Whole stance phase | Early stance | Late stance | ||||||||||
| Subject | R2 | RMS error [%BW] | a [%BW] | b | R2 | RMS error [%BW] | a [%BW] | b | R2 | RMS error [%BW] | a [%BW] | b |
| K1L | 0.72 | 24 | 78 | 49 | 0.94 | 11 | 76 | 42 | 0.76 | 21 | 44 | 74 |
| K2L | 0.66 | 20 | 89 | 34 | 0.85 | 12 | 87 | 28 | 0.80 | 15 | 75 | 45 |
| K3R | 0.54 | 21 | 92 | 27 | 0.94 | 9 | 62 | 36 | 0.25 | 22 | 108 | 21 |
| K4R | 0.09 | 34 | 109 | 17 | 0.90 | 8 | 57 | 39 | 0.25 | 30 | 115 | 36 |
| K5R | 0.71 | 16 | 61 | 38 | 0.90 | 9 | 72 | 32 | 0.65 | 17 | 36 | 52 |
| K6L | 0.78 | 15 | 108 | 32 | 0.92 | 9 | 105 | 31 | 0.61 | 18 | 106 | 35 |
| K7L | 0.86 | 17 | 54 | 44 | 0.94 | 9 | 77 | 34 | 0.91 | 14 | 23 | 55 |
| K8L | 0.25 | 20 | 125 | 20 | 0.90 | 7 | 75 | 38 | 0.42 | 18 | 70 | 68 |
| K9L | 0.90 | 9 | 55 | 28 | 0.97 | 6 | 56 | 27 | 0.71 | 11 | 34 | 36 |
| Mean | 0.61 | 20 | 86 | 32 | 0.92 | 9 | 74 | 34 | 0.60 | 18 | 68 | 47 |
| All | 0.56 | 28 | 101 | 26 | 0.76 | 20 | 88 | 28 | 0.51 | 31 | 106 | 28 |
a = y-intercept of the linear regression line, b = slope of the linear regression line.
When analyzing only the early stance phase (Figure 2C), high correlations between EAM and Fmed were observed for individuals (R2 = 0.85 to 0.97) and for all subjects combined (R2 = 0.76). Especially when analyzing each subject individually RMS errors were small (6–12%BW). Moreover, the y-intercepts and slopes of the individual regression lines exhibited only small deviations across the subjects.
In contrast, only a moderate correlation between EAM and Fmed for all subjects (R2 = 0.51) and high inter-individual variations were observed at the late stance phase (Figure 2D). The inter-individual variation is reflected by a wide scatter. For example, at an EAM value of 1.0%BWHt, individual forces Fmed between 58 and 174%BW were measured. When analyzing the correlation for each individual, three subjects each displayed good, moderate and poor correlations and the RMS errors ranged between 11 and 30%BW.
A good correlation was observed between EAM and MR throughout the whole stance phase (Figure 2B). The coefficient of determination was slightly higher when assuming an arcus tangent function (b1 = 0.55, b2 = 0.14) instead of a linear function (y = 10.7x+50).
Correlation between external moments and internal medial peak forces
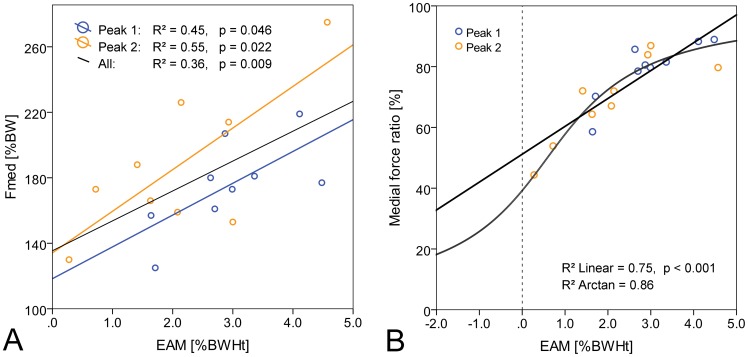
Peak values of Fmed and the corresponding EAM values were significantly correlated at early and late stance phase (Figure 3A). However, the coefficients of determination were only moderate to poor. A good correlation was observed between EAM and MR, which were both measured at the time of peak Fmed (Figure 3B). Again, the coefficient of determination was slightly higher when assuming an arcus tangent function (b1 = 0.60, b2 = 0.35) instead of a linear function (y = 9.2x+51).
Figure 3. Correlation between peak medial forces Fmed and external adduction moments EAM.
Correlation between peak values of Fmed (A) or medial force ratios (B) and EAM at early stance (peak 1) and late stance phase (peak 2). Average peak values of nine subjects.
Correlation between external moments and internal medial peak forces considering the co-variates gait velocity and static limb alignment
Both gait velocity and limb alignment were significantly correlated to the peak medial force at the early stance phase (Table 3). When considering both variables (velocity and alignment) the regression model significantly predicted Fmed with an R2 value of 0.76. The hierarchical regression analyses showed no significant change in R2 for early stance when considering the EAM and either gait velocity and limb alignment alone or both covariates together were already accounted for (Table 3).
Table 3. Correlations between external adduction moment and medial contact force the early stance phase considering the co-variates gait velocity and static frontal plane (varus-valgus) limb alignment.
| model | R2 | adjusted R2 | change in R2 | significance of F change | model significance |
| velocity | 0.49 | 0.42 | - | - | 0.04 |
| i) velocity, EAM | 0.69 | 0.58 | 0.20 | 0.10 | 0.03 |
| alignment | 0.60 | 0,54 | - | - | 0.01 |
| ii) alignment, EAM | 0.61 | 0.49 | 0.01 | 0.64 | 0.06 |
| velocity, alignment | 0.76 | 0.68 | - | - | 0.01 |
| iii) velocity, alignment, EAM | 0.77 | 0.63 | 0.01 | 0.72 | 0.049 |
At late stance neither velocity nor alignment were significantly correlated to the medial peak force (Table 4). The consideration of the EAM resulted in a significant change in R2 beyond the values reached when gait velocity was the only covariate accounted for (change in R2: 0.51, p = 0.04). However, none of the regression models accounting for the influence of covariates significantly predicted Fmed at the late stance phase (p>0.05).
Table 4. Correlations between external adduction moment and medial contact force during the late stance phase considering the co-variates gait velocity and static frontal plane (varus-valgus) limb alignment.
| model | R2 | adjusted R2 | change in R2 | significance of F change | model significance |
| velocity | 0.05 | −0.09 | - | - | 0.58 |
| i) velocity, EAM | 0.56 | 0.41 | 0.51 | 0.04 | 0.09 |
| alignment | 0.27 | 0.17 | - | - | 0.15 |
| ii) alignment, EAM | 0.58 | 0.44 | 0.31 | 0.08 | 0.07 |
| velocity, alignment | 0.27 | 0.03 | - | - | 0.38 |
| iii) velocity, alignment, EAM | 0.58 | 0.33 | 0.31 | 0.12 | 0.19 |
Discussion
This study aimed to examine the quantitative relationship between the external knee adduction moment and the medial knee contact force during gait. The results obtained from the analysis of nine subjects with telemetric knee implants confirmed a general correlation between EAM and Fmed throughout the stance phase of gait and between peak medial forces and corresponding EAM values. However, the variable coefficients of determination as well as high RMS errors reveal the need for a careful interpretation of the EAM.
The correlation of EAM and Fmed differed substantially between early and late stance phases. Whereas the high linear correlations during the early stance phase suggest that the EAM is a strong predictor for Fmed, moderate to poor correlations during the late stance phase and high inter-individual variance show that this statement cannot be generalized.
In the current literature, controversy exists regarding how the EAM should be analyzed. Whereas many studies focus on the overall peak value of the EAM within the stance phase, others analyze peak EAMs separately at early and late stances or even consider the EAM impulse to provide more information on medial knee joint loading [11], [28]. Considering the inter-individual variance observed in our study, it becomes apparent that the predictive value of the EAM during the late stance is limited. However, the peak medial force during the late stance phase was slightly higher than that observed during the early stance phase. Therefore, force reduction at this later instant may be beneficial or even crucial for reducing pain or slowing down OA progression. As in vivo load measurements have shown, some interventions tended to affect joint contact forces at late stance rather than during early stance [17], [21], [22], [37]. By analyzing only the early stance phase, these important differences in the actual loads transferred at the knee joint cannot be detected.
In addition to the coefficients of determination, the regression lines provide valuable information about the relationship between EAM and Fmed. The slopes and y-intercepts of the linear regression lines reveal that a relative EAM reduction is always higher than the corresponding relative reduction of Fmed. Determined across all subjects, relative EAM reductions within the stance phase were about two times higher than the resulting relative reduction of Fmed. A reduction of the EAM by 10% for example would lead to an average reduction of Fmed by only 4.6% at early stance and 5.5% at late stance. However, the slopes and y-intercepts of the regression lines differed strongly between the subjects, especially during the late stance phase (Table 2). An EAM reduction of 10% would lead to individual reductions of Fmed between 3.6 and 5.5% during the early stance phase and 2.7 to 7.6% during the late stance phase. These high inter-individual differences of the regression lines reveal that the same EAM reduction may lead to individually different reductions of Fmed, especially during the late stance phase of gait and indicate that a certain objective, e.g., pain reduction, cannot generally be achieved by a distinct predefined relative EAM reduction.
In the analysis of the relationship between EAM and Fmed it is important to also consider the potential role of gait velocity as well as static limb alignment. Other studies have already demonstrated that gait velocity mainly influences the peak EAM at the early stance phase [11], [38]. By providing insight into the relationship between gait velocity and Fmed directly, the results of the current study demonstrate a good correlation between EAM and Fmed during the early stance phase. However, further hierarchical regression analysis revealed that the EAM did not explain any further variance in Fmed when gait velocity and static limb alignment were already considered (Table 3). This finding suggests not only that measurement of only two parameters, which are easy to implement clinically (static limb alignment and free walking velocity alone) can already provide a proxy for Fmed at the early stance phase of gait, but also highlights the need to control for their influence in any study evaluating interventions aiming to modify Fmed. Whilst a substantial amount of the variation in Fmed expected at the first peak during walking might thus efficiently captured, this is not true for the typically higher forces at the late stance phase. No regression model was identified which significantly predicted peak Fmed from either EAM or velocity and alignment. Because muscle forces are the major determinants of the loads transferred across the knee, consideration of further analysis techniques such as EMG to assess muscle activation patterns and conditions of co-contraction would appear to be critical to derive improved indirect measures of medial joint loading.
Other than the medial force magnitude, the medio-lateral force distribution across the joint is also an important biomechanical variable. Our results show that the EAM is a stronger predictor for the medial force ratio than for the magnitude of Fmed. These results support the claims of former studies that suggested the EAM represents the relative medio-lateral force distribution rather than the actual force on the medial compartment [4], [29]. This statement was also confirmed by other in vivo load measurements. In a single subject with an instrumented knee implant, a good correlation between EAM and Fmed or medial force ratio was found [15]. However, similar to our findings, the R2 values were higher between EAM and MR than between EAM and Fmed within the stance phase. This higher correlation between EAM and MR can be explained by considering muscle co-contraction. A change in the level of muscle co-contraction may not influence the medio-lateral force distribution, but may substantially increase the magnitude of Fmed. Therefore, interventions will only be successful in reducing Fmed by reducing the total joint force or by shifting the force laterally without evoking additional muscle co-contraction. It is possible that interventions that modify the neuromuscular control patterns and the level of co-contraction, but do not change the EAM, can still have the potential to reduce the force magnitudes and can therefore also have a positive effect on OA disease progression, for example. Further investigations on the unloading mechanisms of interventions and gait modifications are necessary to address this issue.
Although our study is unique in that it provides the first analysis of the quantitative relationship between EAM and Fmed during gait in a larger sample of subjects, the interpretation of our results should also consider potential limitations. While most previous studies concerned with the EAM focused on patients with early to end stage OA, our subjects had total knee replacements. The axial joint force and its medio-lateral distribution are influenced by various interacting factors such as muscle forces, joint kinematics and limb alignment. Following total knee replacement, these factors might be altered. Higher EAM values are more frequent in patients with greater varus alignment or severe OA compared to healthy or less severe OA subjects [5], [30]–[32]. Following total knee replacement, the EAM magnitude can be reduced by correcting varus malalignment [33], [34]. In this study, however, a broad EAM spectrum with individual peak values between 1.6 and 4.6%BWHt was measured and therefore also covered the EAM magnitudes reported for patients with OA [30], [35]. In this study the correlation between EAM and Fmed was analyzed during free gait, and no interventions aimed at the reduction of either EAM or Fmed were considered here. The analysis of peak medial forces and corresponding EAM values across all subjects revealed a significant, though poor-to-moderate correlation. However, to analyze the effect of OA treatments, such as laterally wedged shoes, valgus braces or high tibial osteotomies, changes of the peak EAM within one subject are crucial and commonly quantified. In this study, the range of peak EAM values within one subject was too small to determine the effect on intra-individual changes of Fmed.
In the current literature, evidence for the correlation of peak EAM and Fmed values is limited. In a previous study, the correlation between peak medial forces and peak EAM values was analyzed in a single subject with an instrumented knee implant [16]. In that study a “variable-stiffness shoe” was used as intervention. At early stance, changes of the peak EAM were significantly correlated with changes of peak medial forces. Contradictory results were published in a second study with the same subject performing different gait modifications [17]. To understand the exact mechanisms resulting in either a reduction of the EAM or Fmed further analyses aiming at the active manipulation of these variables with a larger sample of subjects are necessary. Only though a more detailed understanding of the underlying mechanisms will it become possible to derive and efficiently monitor the outcome of more targeted interventions for reducing Fmed in a clinical setting.
In conclusion, this study showed that the EAM is a surrogate measure, well-suited to predict the medio-lateral force distribution in the knee joint throughout the stance phase of gait. Although a good correlation between EAM and Fmed was found during the early stance phase, only moderate correlations and high inter-individual variations during the late stance phase revealed that the predictive value of the EAM is limited. Whether the additional consideration of neuromuscular, kinematic or kinetic factors could help to further improve the prediction of the medial joint contact force remains to be determined.
Acknowledgments
The authors thank all subjects for their great contribution, as well as Jörn Dymke, Verena Schwachmeyer and Alexander Wurl for technical support.
Funding Statement
This study was funded by the German Research Foundation (DFG Be 804/18-1, www.dfg.de), Zimmer GmbH (www.zimmer.com), Deutsche Arthrose-Hilfe e.V. (www.arthrose.de) and the European Union Seventh Framework Programme (FP7/2007-2013 ICT-2009.5.2 MXL 248693, cordis.europa.eu). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Funding was received from Zimmer GmbH, Winterthur, Switzerland for the development of instrumented knee implants. This does not alter the authors' adherence to all the PLOS ONE policies on sharing data and materials.
References
- 1. Andriacchi TP, Mündermann A, Smith RL, Alexander EJ, Dyrby CO, et al. (2004) A Framework for the in Vivo Pathomechanics of Osteoarthritis at the Knee. Annals of Biomedical Engineering 32: 447–457. [DOI] [PubMed] [Google Scholar]
- 2. Heijink A, Gomoll A, Madry H, Drobnič M, Filardo G, et al. (2012) Biomechanical considerations in the pathogenesis of osteoarthritis of the knee. Knee Surgery, Sports Traumatology, Arthroscopy 20: 423–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jackson B, Wluka A, Teichtahl A, Morris M, Cicuttini F (2004) Reviewing knee osteoarthritis - a biomechanical perspective. Journal of Science and Medicine in Sport 7: 347–357. [DOI] [PubMed] [Google Scholar]
- 4. Schipplein OD, Andriacchi TP (1991) Interaction between active and passive knee stabilizers during level walking. Journal of Orthopaedic Research 9: 113–119. [DOI] [PubMed] [Google Scholar]
- 5. Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP (2002) The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. Journal of Orthopaedic Research 20: 101–107. [DOI] [PubMed] [Google Scholar]
- 6. Wada M, Maezawa Y, Baba H, Shimada S, Sasaki S, et al. (2001) Relationships among bone mineral densities, static alignment and dynamic load in patients with medial compartment knee osteoarthritis. Rheumatology 40: 499–505. [DOI] [PubMed] [Google Scholar]
- 7. Foroughi N, Smith R, Vanwanseele B (2009) The association of external knee adduction moment with biomechanical variables in osteoarthritis: A systematic review. The Knee 16: 303–309. [DOI] [PubMed] [Google Scholar]
- 8. Heller M, Taylor W, Perka C, Duda G (2003) The influence of alignment on the musculo-skeletal loading conditions at the knee. Langenbeck's Archives of Surgery 388: 291–297. [DOI] [PubMed] [Google Scholar]
- 9. Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, et al. (2002) Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Annals of the Rheumatic Diseases 61: 617–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Radzimski AO, Mündermann A, Sole G (2012) Effect of footwear on the external knee adduction moment - A systematic review. The Knee 19: 163–175. [DOI] [PubMed] [Google Scholar]
- 11. Simic M, Hinman RS, Wrigley TV, Bennell KL, Hunt MA (2011) Gait modification strategies for altering medial knee joint load: A systematic review. Arthritis Care & Research 63: 405–426. [DOI] [PubMed] [Google Scholar]
- 12. Shelburne KB, Torry MR, Steadman JR, Pandy MG (2008) Effects of foot orthoses and valgus bracing on the knee adduction moment and medial joint load during gait. Clinical Biomechanics 23: 814–821. [DOI] [PubMed] [Google Scholar]
- 13. Trepczynski A, Kutzner I, Kornaropoulos E, Taylor WR, Duda GN, et al. (2012) Patellofemoral joint contact forces during activities with high knee flexion. Journal of Orthopaedic Research 30: 408–415. [DOI] [PubMed] [Google Scholar]
- 14. Taylor WR, Heller MO, Bergmann G, Duda GN (2004) Tibio-femoral loading during human gait and stair climbing. Journal of Orthopaedic Research 22: 625–632. [DOI] [PubMed] [Google Scholar]
- 15. Zhao D, Banks SA, Mitchell KH, D'Lima DD, Colwell CW Jr, et al. (2007) Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. Journal of Orthopaedic Research 25: 789–797. [DOI] [PubMed] [Google Scholar]
- 16. Erhart JC, Dyrby CO, D'Lima DD, Colwell CW, Andriacchi TP (2010) Changes in in vivo knee loading with a variable-stiffness intervention shoe correlate with changes in the knee adduction moment. Journal of Orthopaedic Research 28: 1548–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Walter JP, D'Lima DD, Colwell CW, Fregly BJ (2010) Decreased knee adduction moment does not guarantee decreased medial contact force during gait. Journal of Orthopaedic Research 28: 1348–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kutzner I, Heinlein B, Graichen F, Bender A, Rohlmann A, et al. (2010) Loading of the knee joint during activities of daily living measured in vivo in five subjects. Journal of Biomechanics 43: 2164–2173. [DOI] [PubMed] [Google Scholar]
- 19. Heinlein B, Kutzner I, Graichen F, Bender A, Rohlmann A, et al. (2009) ESB Clinical Biomechanics Award 2008: Complete data of total knee replacement loading for level walking and stair climbing measured in vivo with a follow-up of 6–10 months. Clinical Biomechanics (Bristol, Avon) 24: 315–326. [DOI] [PubMed] [Google Scholar]
- 20. Halder A, Kutzner I, Graichen F, Heinlein B, Beier A, et al. (2012) Influence of leg alignment on mediolateral loading in TKR – in-vivo measurements in five patients. Journal of Bone and Joint Surgery Am 94: 1023–1029. [DOI] [PubMed] [Google Scholar]
- 21. Kutzner I, Damm P, Heinlein B, Dymke J, Graichen F, et al. (2011) The effect of laterally wedged shoes on the loading of the medial knee compartment-in vivo measurements with instrumented knee implants. Journal of Orthopaedic Research 29: 1910–1915. [DOI] [PubMed] [Google Scholar]
- 22. Kutzner I, Küther S, Heinlein B, Dymke J, Bender A, et al. (2011) The effect of valgus braces on medial compartment load of the knee joint - in vivo load measurements in three subjects. Journal of Biomechanics 44: 1354–1360. [DOI] [PubMed] [Google Scholar]
- 23. Heinlein B, Graichen F, Bender A, Rohlmann A, Bergmann G (2007) Design, calibration and pre-clinical testing of an instrumented tibial tray. J Biomech 40 Suppl 1S4–10. [DOI] [PubMed] [Google Scholar]
- 24. Graichen F, Arnold R, Rohlmann A, Bergmann G (2007) Implantable 9-channel telemetry system for in vivo load measurements with orthopedic implants. IEEE Transactions on Biomedical Engineering 54: 253–261. [DOI] [PubMed] [Google Scholar]
- 25. Taylor WR, Kornaropoulos EI, Duda GN, Kratzenstein S, Ehrig RM, et al. (2010) Repeatability and reproducibility of OSSCA, a functional approach for assessing the kinematics of the lower limb. Gait & Posture 32: 231–236. [DOI] [PubMed] [Google Scholar]
- 26. Deuretzbacher G, Rehder U (1995) A CAE (computer aided engineering) approach to dynamic whole body modeling—the forces in the lumbar spine in asymmetrical lifting. Biomedizinische Technik 40: 93–98. [DOI] [PubMed] [Google Scholar]
- 27. Andrews J (1974) Biomechanical analysis of human motion. Kinesiology 4: 32–42. [Google Scholar]
- 28. Kean CO, Hinman RS, Bowles KA, Cicuttini F, Davies-Tuck M, et al. (2012) Comparison of peak knee adduction moment and knee adduction moment impulse in distinguishing between severities of knee osteoarthritis. Clinical Biomechanics 27: 520–523. [DOI] [PubMed] [Google Scholar]
- 29. Andriacchi TP (2013) Editorial: Valgus alignment and lateral compartment knee osteoarthritis: A biomechanical paradox or new insight into knee osteoarthritis? Arthritis & Rheumatism 65: 310–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mündermann A, Dyrby CO, Andriacchi TP (2005) Secondary gait changes in patients with medial compartment knee osteoarthritis: Increased load at the ankle, knee, and hip during walking. Arthritis & Rheumatism 52: 2835–2844. [DOI] [PubMed] [Google Scholar]
- 31. Mündermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP (2004) Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: Reduced walking speed. Arthritis & Rheumatism 50: 1172–1178. [DOI] [PubMed] [Google Scholar]
- 32.Sharma L, Hurwitz DE, Andriacchi TP (1998) Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis & Rheumatism 41: 1233–1240. [DOI] [PubMed] [Google Scholar]
- 33. Mandeville D, Osternig LR, Lantz BA, Mohler CG, Chou L-S (2008) The effect of total knee replacement on the knee varus angle and moment during walking and stair ascent. Clinical Biomechanics 23: 1053–1058. [DOI] [PubMed] [Google Scholar]
- 34. Hilding MB, Lanshammar Hk, Ryd L (1995) A relationship between dynamic and static assessments of knee joint load:Gait analysis and radiography before and after knee replacement in 45 patients. Acta Orthopaedica 66: 317–320. [DOI] [PubMed] [Google Scholar]
- 35. Kaufman KR, Hughes C, Morrey BF, Morrey M, An K-N (2001) Gait characteristics of patients with knee osteoarthritis. Journal of Biomechanics 34: 907–915. [DOI] [PubMed] [Google Scholar]
- 36. Bender A, Bergmann G (2012) Determination of typical patterns from strongly varying signals. Computer Methods in Biomechanics and Biomedical Engineering 15: 761–769. [DOI] [PubMed] [Google Scholar]
- 37. Kinney AL, Besier TF, Silder A, Delp SL, D'Lima DD, et al. (2013) Changes in in vivo knee contact forces through gait modification. J Orthop Res 31: 434–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. van den Noort JC, Schaffers I, Snijders J, Harlaar J (2013) The effectiveness of voluntary modifications of gait pattern to reduce the knee adduction moment. Human Movement Science 32: 412–424. [DOI] [PubMed] [Google Scholar]