Abstract
Objectives:
To detect the prevalence and pattern of use of Potentially inappropriate medications (PIMs) in hospitalized elderly patients of a tertiary care teaching hospital using Beers 2012 criteria and to compare the same with Beers 2003 criteria.
Materials and Methods:
Prescriptions of the elderly patients aged 65 years and above were collected from the medicine ward and analyzed. PIMs were identified with help of Beers 2003 and Beers 2012 criteria and comparison was made between the two criteria. Predictors associated with use of PIM were identified using bivariate and multivariate logistic regression analysis.
Results:
A total of 210 patients received 2,267 drugs. According to Beers 2003 criteria, 60 (28.57%) elderly patients received at least one PIM and 2.9% drugs were prescribed inappropriately. According to Beers 2012 criteria, 84 (40%) elderly received at least one PIM while 22 (10.47%) received multiple PIMs and about 5% drugs were prescribed inappropriately. The most commonly prescribed PIM was mineral oil-liquid paraffin (30, 14.3%) followed by spironolactone (25, 11.9%), digoxin (19, 9%), and benzodiazepines (14, 6.7%). There was a significant association between the number of patients receiving more than six drugs and the use of PIMs (P < 0.01). Use of more than 10 drugs was a significant predictor for use of PIMs in the elderly.
Conclusion:
The study shows high prevalence of prescribing PIMs in hospitalized elderly patients. Beers 2012 criteria are more effective in identifying PIMs than Beers 2003 criteria.
KEY WORDS: Beers criteria 2003, Beers criteria 2012, elderly, inappropriate prescribing, PIMs
Introduction
The world population is growing; what is new is the rapid pace of aging. The world's elderly population which was 550 million in 1996 is expected to approach 1.2 billion by the year 2025. As a result of decline in birth rate and increased life expectancy, the older population in most countries is growing faster than the population as a whole. Lesser developed nations are aging faster than their developed counterparts.[1] India's population aged 60 years and above, is projected to increase over the next decade from 8.3 to 10.7% in 2021 according to the United Nations Population Division. This is due to increased life expectancy at birth which is 67.3 years for males and 69.6 years for females. This number may also rise by almost 3 years during the next decade.[2]
The elderly population is the highest consumer of drugs. High degree of caution is required while prescribing in this vulnerable group. Due to age related changes in the physiology of elderly, these people also experience altered pharmacokinetics and dynamics of drugs. They have multiple comorbidities and are hospitalized more often which increases the chances of polypharmacy and inappropriate prescribing. Potentially inappropriate medication (PIM) is defined as “a drug in which the risk of an adverse event outweighs its clinical benefit, particularly when there is a safer or more effective alternate therapy for the same condition”.[3] Several studies have reported increased incidence of adverse drug reactions with PIMs.[4,5] Identifying potentially inappropriate medications is, thus, important to minimize the pharmacotherapy related hazards in this vulnerable population.
Several criteria have been designed for identification of PIMs. These criteria can be drug based explicit criteria like Beers[6] and Screening Tool of Older Persons’ potentially inappropriate Prescriptions (STOPP)[7] and patient based implicit criteria like Medication Appropriateness Index.[8] Beers criteria was the first set of explicit criteria for inappropriate drug use in elderly developed in 1991[9] by Mark H. Beers at the University of California. This criteria was subsequently updated in 1997[10] and 2003.[11]
Beers 2003 criteria is the most widely used explicit tool for identifying PIMs in elderly patients.[12,13] Recently, Beers 2003 criteria has been used to identify PIM use in India both in outpatient setting and hospitalized elderly.[14,15,16] With new medications being continually added to the market, a need for frequent updates of such tools is warranted.[17] Therefore, in 2011 the American Geriatrics Society (AGS) updated the Beers criteria by using an evidence-based approach after Dr. Beers passed away in 2009. The 2003 Beers criteria classified PIMs in three categories which included drugs to be avoided in elderly in general, drugs exceeding recommended dose and drugs to be avoided with specific comorbidity.[11] The latest version of the Beers criteria has undergone some major changes like addition of new drugs and deleting drugs which are no longer used. A new category of PIMs is also added for the drugs which are to be used with caution in the elderly.[18]
This study was undertaken to identify the prevalence and pattern of use of PIMs in elderly patients hospitalized in medicine department using the Beers 2003 criteria. During the course of the study, the revised Beers 2012 criteria were released, which was expected to be more relevant in identifying PIMs. Hence, a comparison between the Beers 2003 and Beers 2012 criteria was also made.
Materials and Methods
A prospective study was carried out in a tertiary care teaching hospital after obtaining approval of the Institutional Review Board. All patients aged 65 years and above were included in the study after obtaining their written consent. Patients hospitalized in the medicine wards from July 2011 to June 2012 were included. Data was collected in a case record form which included the patients’ demographic details, complete history, clinical data, and the drugs prescribed during period of hospitalization. The PIMs were identified with help of the Beers 2003 and 2012 criteria.
Statistical analysis
Data was analyzed using Statistical Package for Social Sciences (SPSS) software version 20. Association between polypharmacy and PIM use was determined using Fisher's exact test. Predictors (comorbid conditions, no. of drugs prescribed, and duration of hospital stay) associated with PIM use were identified using bivariate analysis (independent variables). Multivariate logistic regression was then applied to study the influence of these variables on PIM use. Value of P < 0.05 was considered statistically significant.
Results
A total of 210 patients were enrolled, among which 91 (43.3%) were males and 119 (56.7%) were females. The mean age was 69.34 ± 5.26 years (range 65-85 years). The total number of drugs prescribed in 210 patients was 2267 with 9.52 ± 2.75 drugs prescribed per patient. The average number of days of hospitalization in the medicine ward for elderly patient was 8.18 ± 2.89 days. The number of drugs prescribed increased significantly with the increase in hospital stay (P < 0.001). Most common disease conditions observed were (based on ICD-10 version 2010[19]) circulatory system disorders (67%) followed by respiratory system disorders (22%), infectious diseases (18%), and genitourinary system disorders (14%).
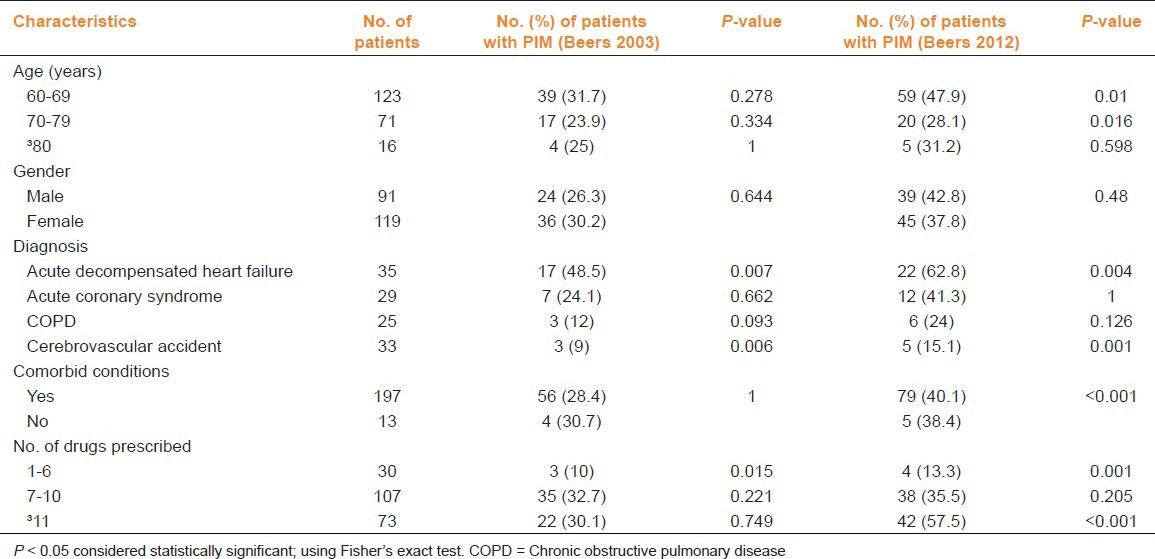
Hypertension (51.4%) was the most common comorbid condition affecting elderly followed by diabetes mellitus (24.3%), ischemic heart disease (22.9%), and chronic obstructive pulmonary disorder (16.7%). Table 1 shows pattern of PIM use compared to patient characteristics. Aspirin (58.1%) was the most frequently prescribed drug followed by ondansetron (53.8%), pantoprazole (50.95%), atorvastatin (49.05%), and clopidogrel (44.76%).
Table 1.
Pattern of potentially inappropriate medication (PIM) use and patient characteristics (n = 210)
PIMs
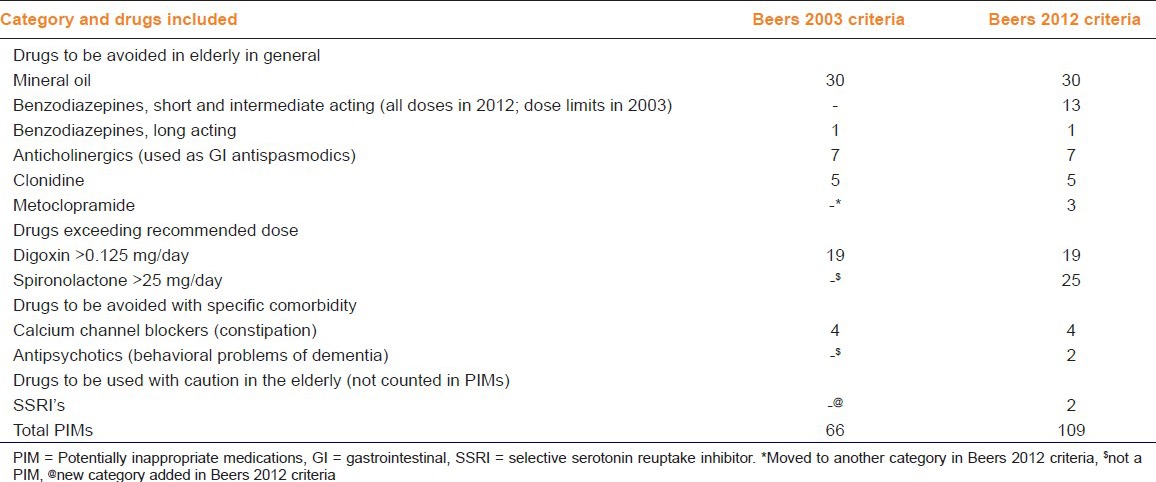
Based on Beers 2012 criteria, 109 out of the 2,267 (4.8%) drugs prescribed were inappropriate and 84 out of 210 (40%) patients received at least one PIM. Based on Beers 2003 criteria, 66 (2.9%) drugs were prescribed inappropriately and 60 (28.57%) patients received at least one PIM. The most commonly prescribed PIM was mineral oil/liquid paraffin (14.3%), followed by spironolactone (11.9%), digoxin (9%), and benzodiazepines (6.7%).
Table 2 depicts frequency of PIMs based on Beers 2003 and 2012 criteria.
Table 2.
Pattern of PIM use in the hospitalized elderly using Beers 2003 and 2012 criteria (n = 210)
Multiple PIMs
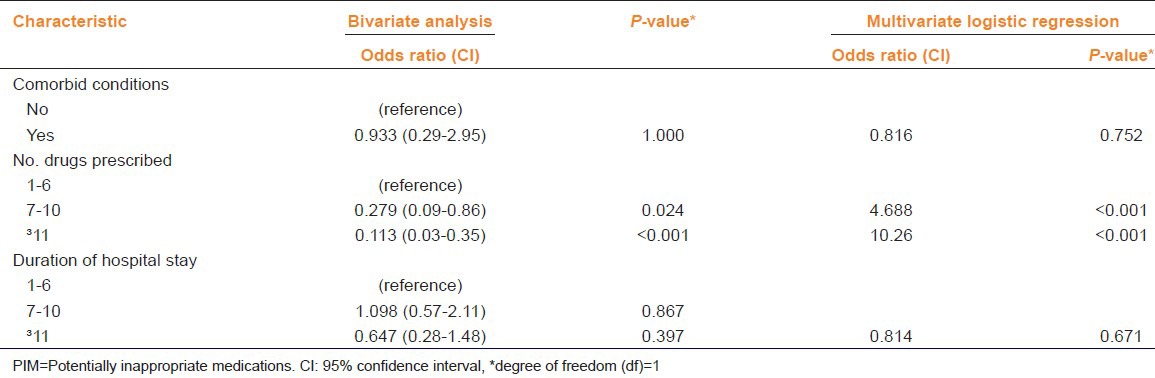
Out of the 84 patients who were prescribed PIMs considering Beers 2012 criteria, 19 (22.61%) patients received two PIMs and three (3.57%) received three PIMs. Of the 60 patients receiving PIMs as per Beers 2003 criteria, six (10%) were prescribed two PIMs. There was a significant association between the number of patients receiving more than six drugs (polypharmacy) and use of PIMs (P < 0.01). Bivariate analysis identified age 70-79 years (odds ratio (OR): 2.351; confidence interval (CI): 1.26-4.40; P = 0.009) and increased number of medications use (7-10 and ³11) during hospital stay (OR: 0.279; CI: 0.03-0.35; P < 0.05 and OR: 10.26; CI: 0.03-0.35; P < 0.001 respectively) as positive predictors of PIM use for Beers 2012 criteria. Gender, age, duration of hospital stay, and comorbid conditions did not predict PIM use. Multivariate logistic regression analysis suggested number of drugs (7-10 and ³11) as positive predictor for PIM use (OR: 4.68; P < 0.01 and OR: 10.26; P < 0.001, respectively) for Beers criteria 2012 [Table 3].
Table 3.
Bivariate analysis and multivariate logistic regression: Predictors of PIM use (Beers 2012 criteria, n = 210)
Discussion
Worldwide the number of people above 65 years is on the rise due to increased longevity. Beers criteria, one of the widely used explicit criteria for identifying PIMs, have undergone a major reformation in 2012[6] as compared to the previous version of 2003 and is expected to be more competent in identifying PIMs. Some drugs like ferrous sulfate, guanadrel, guanathedine, mesoridazine, pseudoephedrine (for hypertension), and others which are no longer used have been omitted in the Beers 2012 criteria. Others like aspirin (for primary prevention of cardiac events), some anti-arrhythmic drugs, belladonna derivatives, some benzodiazepines, antipsychotics (for behavioral problems of dementia), metoclopramide, spironolactone, and many more which are being prescribed have been added in the recent edition. Few drugs to be prescribed with caution in the elderly have also been added as a new category in the revised Beers criteria [Additional File 1].
Out of four categories of PIMs in Beers 2012 criteria, the first forms a major group where the PIMs are divided into therapeutic categories. Seventy (64.22%) PIMs in our study fell under this category. Use of mineral oil/liquid paraffin is considered as PIM according to both the criteria (2003 and 2012) due to possibility of aspiration pneumonia in elderly.[6,10] As it is still widely used in our setup, it was the most common PIM in the first category. Second category includes drugs given at inappropriate doses; from which, spironolactone and digoxin contributed around 30% of PIMs. Under the drugs that may exacerbate a preexisting condition which comprised the third category, antipsychotics (in patients with behavioral problems of dementia) and calcium channel blockers (in patients with constipation) were considered inappropriate contributing to around 5% of total PIMs. Of the drugs to be used with caution in the elderly, selective serotonin reuptake inhibitor; escitalopram were prescribed in two patients.
Beers 2003 criteria have been instrumental in revealing high prevalence of PIM use between 25 and 45% in the developed part of the world.[18,20,21] Use of PIMs has been recently reported from South India using Beers 2003 criteria where 4.1% of total drugs could be considered as potentially inappropriate as compared to 2.9% in our study. This difference could be due to difference in study population.[22] Our findings are however consistent with an earlier study which included patients from different specialties and both outdoor as well as hospitalized patients, reporting PIM use in 27.25% patients as compared to 28.57% in our study using Beers 2003 criteria;[16] but somewhat higher compared to a recent study reporting 24.6% prevalence in hospitalized elderly.[23] We have previously reported inappropriate prescribing in 23.58% of elderly patients in the outpatient setting using Beers 2003 criteria.[14]
Polypharmacy was the most significant predictor of PIM use; higher incidence of PIM use with higher number of drugs prescribed in hospitalized elderly patients. There was no statistically significant association when prevalence of PIM was correlated with variables like age, gender, duration of hospital stay, and associated comorbidities. There was a significant association between PIM prescribing and the diagnosis of acute decompensated heart failure and cerebrovascular accident according to Beers 2003 and 2012 criteria. In addition, Beers 2012 criteria also showed a significant association with age group less than 80 years and PIM prescribing.
As this study was restricted to medicine department, several drugs enlisted in Beers 2012 criteria were not prescribed like tricyclic antidepressants, antipsychotics (conventional and atypical), ergot derivatives, uterine relaxants (isoxsuprine), estrogens (with or without progestins), skeletal muscle relaxants (carisoprodol, chlorzoxazone, cyclobenzaprine, metaxalone, methocarbamol, orphenadrine), and anticancer agents (carboplatin, cisplatin, vincristine). Hence, the findings of this study are not applicable to other specialties.
To our knowledge this is the first study of PIM use with Beers 2012 criteria. As expected, we found Beers 2012 more competent than Beers 2003 criteria in identifying the PIMs-2.9% viz-a-viz 4.8% of total drugs as PIM and 28.57% viz-a-viz 40% of hospitalized elderly receiving PIM. This may be attributed to the significant changes made in the updated Beers criteria. The revised Beers criteria are definitely a superior tool compared to earlier version of 2003.
Regardless of different editions of Beers criteria used for evaluating the use of PIMs in the elderly, there is a high prevalence of PIM use in hospitalized elderly which must be brought to the attention of the clinicians.
Acknowledgement
The authors would like to express their thanks to Dr. Pankaj R. Patel, Dean, Smt. NHL Medical College and Dr. M. H. Makwana, Superintendent, V. S. Hospital for permitting me to do this work in V. S. Hospital. The authors also express gratitude to Medicine Department for support.
Footnotes
Source of Support: Nil
Conflict of Interest: No
References
- 1.Global aging into the 21st century. U. S. Census Bureau. 1996. Dec, [Last accessed on 2012 Dec 2]. Available from: http://www.census.gov/population/international/files/96wchart.pdf .
- 2.MoHFW; Report of the Technical Group on Population Projections May 2006, National Commission on Population/MoHFW and National Health Profile 2008. [Google Scholar]
- 3.Corsonello A, Pranno L, Garasto S, Fabietti P, Bustacchini S, Lattanzio F. Potentially inappropriate medication in elderly hospitalized patients. Drugs Aging. 2009;26:31–9. doi: 10.2165/11534640-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 4.Nixdorff N, Hustey FM, Brady AK, Vaji K, Leonard M, Messinger-Rapport BJ. Potentially inappropriate medications and adverse drug effects in elders in the ED. Am J Emerg Med. 2008;26:697–700. doi: 10.1016/j.ajem.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Gallagher P, O’Mahony D. STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions): Application to acutely ill elderly patients and comparison with Beers’ criteria. Age Ageing. 2008;37:673–9. doi: 10.1093/ageing/afn197. [DOI] [PubMed] [Google Scholar]
- 6.American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616–31. doi: 10.1111/j.1532-5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Mahony D, Gallagher P, Ryan C, Byrne S, Hamilton H, Barry P, et al. STOPP and START criteria: A new approach to detecting potentially inappropriate prescribing in old age. Euro Geriatr Med. 2010;1:45–51. [Google Scholar]
- 8.Britten N, Jenkins L, Barber N, Bradley C, Stevenson F. Developing a measure for the appropriateness of prescribing in general practice. Qual Saf Health Care. 2003;12:246–50. doi: 10.1136/qhc.12.4.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA division of Geriatric medicine. Arch Intern Med. 1991;151:1825–32. [PubMed] [Google Scholar]
- 10.Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly: An update. Arch Intern Med. 1997;157:1531–6. [PubMed] [Google Scholar]
- 11.Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: Results of a US consensus panel of experts. Arch Intern Med. 2003;163:2716–24. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 12.Varallo FR, Capucho HC, Planeta CS, Mastroianni Pde C. Safety assessment of potentially inappropriate medications use in older people and the factors associated with hospital admission. J Pharm Pharm Sci. 2011;14:283–90. doi: 10.18433/j3p01j. [DOI] [PubMed] [Google Scholar]
- 13.Niwata S, Yamada Y, Ikegami N. Prevalence of inappropriate medication using Beers criteria in Japanese long-term care facilities. BMC Geriatr. 2006;6:1. doi: 10.1186/1471-2318-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaveri HG, Mansuri SM, Patel VJ. Use of potentially inappropriate medicines in the elderly: A prospective study in medicine out-patient department of a tertiary care teaching hospital. Indian J Pharmacol. 2010;42:95–8. doi: 10.4103/0253-7613.64499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harugeri A, Joseph J, Parthasarathi G, Ramesh M, Guido S. Potentially inappropriate medication use in elderly patients: A study of prevalence and predictors in two teaching hospitals. J Postgrad Med. 2010;56:186–91. doi: 10.4103/0022-3859.68642. [DOI] [PubMed] [Google Scholar]
- 16.Shah RB, Gajjar BM, Desai SV. Evaluation of the appropriateness of prescribing in geriatric patients using Beers criteria and Phadke's criteria and comparison thereof. J Pharmacol Pharmacoether. 2011;2:248–52. doi: 10.4103/0976-500X.85948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lund BC, Steinman MA, Chrischilles EA, Kaboli PJ. Beers criteria as a proxy for inappropriate prescribing of other medications among older adults. Ann Pharmacother. 2011;45:1363–70. doi: 10.1345/aph.1Q361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van der Hooft CS, Jong GW, Dieleman JP, Verhamme KM, van der Cammen TJ, Stricker BH, et al. Inappropriate drug prescribing in older adults: The updated 2002 Beers criteria-a population-based cohort study. Br J Clin Pharmacol. 2005;60:137–44. doi: 10.1111/j.1365-2125.2005.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. International Classification of Diseases (ICD-10) [Last accessed on 2012 Dec 12]. Available from: http//www.who.int/classifications/icd/en .
- 20.Al-Omar HA, Al-Sultan MS, Abu-Auda HS. Prescribing of potentially inappropriate medications among the elderly population in an ambulatory care setting in a Saudi military hospital: Trend and cost. Geriatr Gerontol Int. 2013;13:616–21. doi: 10.1111/j.1447-0594.2012.00951.x. [DOI] [PubMed] [Google Scholar]
- 21.Goltz L, Kullak-Ublick GA, Kirch W. Potentially inappropriate prescribing for elderly outpatients in Germany: A retrospective claims data analysis. Int J Clin Pharmacol Ther. 2012;50:185–94. doi: 10.5414/cp201441. [DOI] [PubMed] [Google Scholar]
- 22.Shenoy S, Rao J, Sen A, Kumar V. Evaluation of drug prescribing pattern in elderly patients in tertiary care hospital. Indian J Pharmacol. 2006;38:90. [Google Scholar]
- 23.Vishwas HN, Harugeri A, Parthasarathi G, Ramesh M. Potentially inappropriate medication use in Indian elderly: Comparison of Beers’ criteria and screening tool of older persons’ potentially inappropriate prescriptions. Geriatr Gerontol Int. 2012;12:506–14. doi: 10.1111/j.1447-0594.2011.00806.x. [DOI] [PubMed] [Google Scholar]


