Abstract
Objectives:
The aim of this study was to investigate the efficacy of dezocine (DEZ) versus placebo control (CON) and 2% lidocaine (LID) in prevention of injection pain due to DEZ.
Materials and Methods:
A prospective randomized double-blind, placebo-CON study was conducted in 75 adults, American Society of Anesthesiologists physical status I or II, scheduled to undergo an elective surgery. A total of 25 patients were randomly assigned to one of the three groups, thus CON, group LID and group DEZ. The groups received either 2 ml of normal saline or 2 ml 2% LID or 2 mg/2 ml DEZ, respectively, as pre-treatment. Propofol was injected 1 min later. A blinded researcher assessed the patient's pain level using a four point verbal rating scale.
Results:
Less patients experienced pain due to propofol injection in the LID (40%) and DEZ (28%) groups compared with the CON (84%) group (P < 0.05). Six patients (24%) in the CON group reported severe pain during propofol injection but none in the other two groups.
Conclusion:
Pre-treatment with DEZ decreases propofol injection pain as effectively as LID.
KEY WORDS: Dezocine, injection pain, lidocaine, propofol
Introducstion
Patient satisfaction with perioperative care is getting importance in recent years. Propofol is an intravenous general anesthetic and it is associated with the pain on intravenous injection in 40-86% of patients.[1] Lidocaine (LID) pre-treatment is most commonly used to the decrease pain due to injection of propofol.[2,3,4] However, it was reported that the addition of LID may destabilize the emulsion formulation of propofol with a potential risk of causing pulmonary fat embolism.[5] Pre-treatment with opioids may prevent the pain due to propofol injection through either a central or peripheral effect.[3,6,7,8,9,10] Dezocine (DEZ), an opioid drug with agonist-antagonist effect, binds with stereospecific receptors at many sites within the central nervous system (CNS) affecting the perception of pain and the emotional response to pain.
The aim of this study was to investigate the efficacy of DEZ 2 mg in comparison with placebo (normal saline) and LID.
Materials and Methods
This was a randomized, double-blind placebo-controlled (CON) study.
Ethics Committee approval was obtained and a written informed consent was taken from all patients was included in the study. A total of 75 patients of both genders, aged between 16 and 65 years, American Society of Anesthesiologists (ASA) grades I and II, scheduled for elective surgery under general anesthesia were recruited for the study. Patients with a history of renal or hepatic insufficiency, hypersensitivity to the study drugs, neurological or cardiovascular disease and patients with obesity, difficult airway, pregnant patients and patients on medication with pain modifying drugs were excluded from the study. Group randomization was done according to the computer software generated random numbers. Group CON (n = 25 patients) received 2 ml normal saline, group LID (n = 25 patients) received 2 ml of 40 mg LID (Beijing Yimin Pharmaceutical CO., China) and group DEZ (n = 25 patients) received 2 ml of 2 mg DEZ (Yangtze River Pharmaceutical CO., China). All three drug solutions (normal saline, LID and DEZ) looked identical. All patients were explained about the verbal rating scale (VRS) for pain assessment on propofol injection. Patient allocation is represented as a consort flow diagram [Figure 1].
Figure 1.
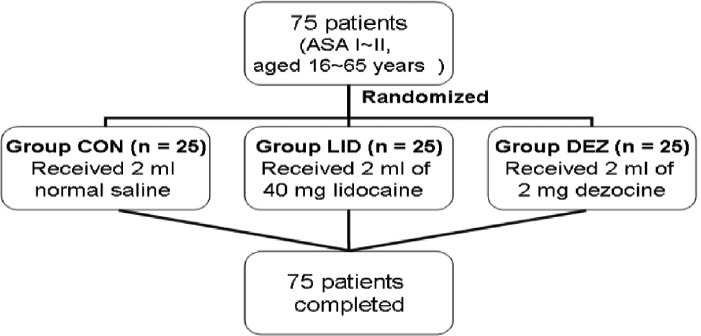
Dezocine in propofol injection induced pain: Consort flow diagram
Patients received 0.1 g of phenobarbital intramuscularly 30 min before induction of anesthesia. On arrival at the operating room, an 18 G intravenous cannula was placed in the largest vein on the dorsum of the hand and lactated Ringer's infusion was started. The study drug was injected, 1 min after was followed by 50 mg of propofol were administrated over 20 s. An Anesthesiologist blinded to the intervention evaluated the pain according to VRS during injection of propofol. Patients were asked to grade pain or discomfort from 0 to 3 in accordance to a four-point scale: 0, 1, 2 and 3, as no pain, mild, moderate and severe pain.[3] The remainder of the calculated (2 mg/kg) propofol dose was then administered followed by induction of anesthesia.
Patient characteristics were compared between the groups using analysis of variance. Data are presented as the mean ± standard deviation or frequency of occurrence with percentages. The categorical variables were analyzed using γ2 test. P < 0.05 was considered to be significant. Statistical analysis was performed with the statistical package for the social sciences 10.0 program (SPSS Inc., Chicago, Illinois, USA).
Results
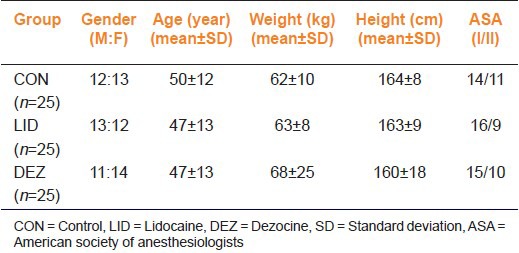
All patients completed the study. Treatment groups were similar with respect to age, gender, weight, height and ASA grade [Table 1].
Table 1.
Patient characteristics in the CON, LID and DEZ groups
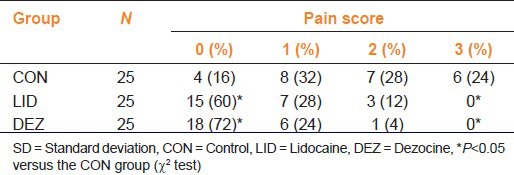
The total incidence of propofol injection pain was 84% (21 patients) in the CON group, 40% (10) in the LID group and 28% (7) in the DEZ group. Data analyses showed that both LID and DEZ significantly reduced propofol injection pain more than placebo (P < 0.05). There was no statistically significant difference in incidence of propofol injection pain between these groups with respect to the mild and moderate pain (P > 0.05). Six patients (24%) in the CON group reported severe pain during propofol injection, but none in the other two groups (P < 0.05), [Table 2].
Table 2.
Incidence of propofol induced pain: A comparison between CON LID and DEZ groups
Discussion
Our study demonstrated that pre-treatment with 2 mg DEZ or 40 mg LID reduced the incidence and severity of pain due to propofol injection.
Propofol can irritate the skin, mucous membrane and venous intima. Peripheral veins are innervated with polymodal nociceptors which mediate the pain response to the injection of certain anesthetic agents.[11] The incidence and severity of pain during propofol injection may be related to the formulation of the drug.[12,13] Larsen et al.[12] reported that a new formulation of propofol (a 10% fat emulsion formulated with long- and medium-chain triglycerides) may be associated with less pain upon injection. Microemulsion of propofol produces more frequent and severe pain upon injection than lipid emulsion propofol.[12]
Opioids (fentanyl, remifentanil and alfentanil) have been used to alleviate the pain of propofol intravenous administration.[3,6,7,8,9,10] Pre-treatment with either of these opioids should not only decrease the pain from propofol injection but also reduce the post-operative pain, post-operative nausea and vomiting and the need for post-operative opioids.[14,15] The reduction in pain due to propofol injection has been attributed to the interaction with peripheral μ-opioid receptors.[3,7] It has also been suggested that prevention of propofol injection pain by opioids may be mediated via central opioid receptors. DEZ may act primarily as a partial agonist at the μ receptor. It binds with stereospecific receptors at many sites within the CNS to alter processes affecting both the perception of pain and the emotional response to pain. At least two of these types of receptors (μ and k) mediate analgesia. We assumed that the pain-reducing action of DEZ was primarily central since a tourniquet technique was not used. Moreover, it has been reported that intravenous opioids administered with tourniquet block prior to propofol injection failed to show analgesic efficacy.[8]
The limitation of this study is the lack of power analysis. Furthermore, in this study different doses of DEZ were not used and hence, the lowest dose of DEZ, efficacious to prevent pain during propofol injection remains unknown.
However, it is concluded that pre-treatment with DEZ decreases propofol injection pain as effectively as LID and can be an alternative to other drugs used for the same purpose.
Footnotes
Source of Support: National Natural Science Foundation of China. (No. 81100105)
Conflict of Interest: No
References
- 1.Angst MS, Mackey SC, Zupfer GH, Tataru CD, Brock-Utne JG. Reduction of propofol injection pain with a double lumen i.v. set. J Clin Anesth. 1997;9:462–6. doi: 10.1016/s0952-8180(97)00101-3. [DOI] [PubMed] [Google Scholar]
- 2.Bachmann-Mennenga B, Ohlmer A, Boedeker RH, Mann M, Mühlenbruch B, Heesen M. Preventing pain during injection of propofol: Effects of a new emulsion with lidocaine addition. Eur J Anaesthesiol. 2007;24:33–8. doi: 10.1017/S0265021506000974. [DOI] [PubMed] [Google Scholar]
- 3.Kwak K, Kim J, Park S, Lim D, Kim S, Baek W, et al. Reduction of pain on injection of propofol: Combination of pretreatment of remifentanil and premixture of lidocaine with propofol. Eur J Anaesthesiol. 2007;24:746–50. doi: 10.1017/S026502150600233X. [DOI] [PubMed] [Google Scholar]
- 4.Massad IM, Abu-Ali HM, Abu-Halaweh SA, Badran IZ. Venous occlusion with lidocaine for preventing propofol induced pain. A prospective double-blind randomized study. Saudi Med J. 2006;27:997–1000. [PubMed] [Google Scholar]
- 5.Davies AF, Vadodaria B, Hopwood B, Dexter T, Conn D. Efficacy of microfiltration in decreasing propofol-induced pain. Anaesthesia. 2002;57:557–61. doi: 10.1046/j.1365-2044.2002.02602.x. [DOI] [PubMed] [Google Scholar]
- 6.Pang WW, Mok MS, Huang S, Hwang MH. The analgesic effect of fentanyl, morphine, meperidine, and lidocaine in the peripheral veins: A comparative study. Anesth Analg. 1998;86:382–6. doi: 10.1097/00000539-199802000-00031. [DOI] [PubMed] [Google Scholar]
- 7.Iyilikci L, Balkan BK, Gökel E, Günerli A, Ellidokuz H. The effects of alfentanil or remifentanil pretreatment on propofol injection pain. J Clin Anesth. 2004;16:499–502. doi: 10.1016/j.jclinane.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 8.Wrench IJ, Girling KJ, Hobbs GJ. Alfentanil-mediated analgesia during propofol injection: No evidence for a peripheral action. Br J Anaesth. 1996;77:162–4. doi: 10.1093/bja/77.2.162. [DOI] [PubMed] [Google Scholar]
- 9.Lee JR, Jung CW, Lee YH. Reduction of pain during induction with target-controlled propofol and remifentanil. Br J Anaesth. 2007;99:876–80. doi: 10.1093/bja/aem293. [DOI] [PubMed] [Google Scholar]
- 10.Chae YJ, Min SK, Park SK, Kim SM, Won YJ, Cho HB. Reduction of microemulsion propofol-induced injection pain via target-controlled remifentanil infusion. J Int Med Res. 2011;39:2151–7. doi: 10.1177/147323001103900611. [DOI] [PubMed] [Google Scholar]
- 11.Klement W, Arndt JO. Pain on i.v. injection of some anaesthetic agents is evoked by the unphysiological osmolality or pH of their formulations. Br J Anaesth. 1991;66:189–95. doi: 10.1093/bja/66.2.189. [DOI] [PubMed] [Google Scholar]
- 12.Larsen B, Beerhalter U, Biedler A, Brandt A, Doege F, Brün K, et al. Less pain on injection by a new formulation of propofol? A comparison with propofol LCT. Anaesthesist. 2001;50:842–5. doi: 10.1007/s00101-001-0234-0. [DOI] [PubMed] [Google Scholar]
- 13.Sim JY, Lee SH, Park DY, Jung JA, Ki KH, Lee DH, et al. Pain on injection with microemulsion propofol. Br J Clin Pharmacol. 2009;67:316–25. doi: 10.1111/j.1365-2125.2008.03358.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marret E, Kurdi O, Zufferey P, Bonnet F. Effects of nonsteroidal antiinflammatory drugs on patient-controlled analgesia morphine side effects: Meta-analysis of randomized controlled trials. Anesthesiology. 2005;102:1249–60. doi: 10.1097/00000542-200506000-00027. [DOI] [PubMed] [Google Scholar]
- 15.Kakinohana M, Higa Y, Sasara T, Saikawa S, Miyata Y, Tomiyama H, et al. Addition of ketamine to propofol-fentanyl anaesthesia can reduce post-operative pain and epidural analgesic consumption in upper abdominal surgery. Acute Pain. 2004;5:75–9. [Google Scholar]


