Abstract
Tentorial dural arteriovenous fistula (DAVF) as a cause of trigeminal neuralgia is extremely rare. Although less than 10 cases have been reported in the literature, all cases presented with ipsilateral trigeminal neuralgia. Here we report a unique case of tentorial DAVF manifesting as contralateral trigeminal neuralgia. A 58-year-old man presented with right-sided trigeminal neuralgia. Cerebral angiography revealed a left tentorial DAVF and the MR imaging demonstrated a variceal venous dilatation occupying the left lateral pontine cistern and multiple venous flow voids adjacent to the right trigeminal nerve root entry zone. Transarterial Onyx embolization resulted in near complete obliteration of the fistula with immediate resolution of facial pain. The patient remains symptom free and without evidence of recurrence during 9 months of follow-up. Transarterial Onyx embolization may be an effective treatment modality for such an usual case.
Keywords: Fistula
Background
Trigeminal neuralgia is frequently associated with vascular compression at the root entry zone of the trigeminal nerve by an aberrant loop of artery or vein. Secondary trigeminal neuralgia, although not common, may be due to tumors, aneurysms, vascular malformations, or vertebrobasilar artery ectasia.1 Dural arteriovenous fistulas (DAVFs) remain a rare cause of trigeminal neuralgia with less than 10 cases reported in the literature.1–9 However, all nine cases presented with ipsilateral trigeminal neuralgia in the territory of V2 or V3 branches of the trigeminal nerve. Among them, four cases were successfully treated by surgical excision or clipping, two cases were treated by embolization alone, two cases were treated by embolization combined with surgical intervention, and one case was treated by stereotactic radiosurgery. Trigeminal neuralgia associated with contralateral DAVFs has not been described previously.
In this paper, we report a unique case of trigeminal neuralgia from venous compression by draining veins of a contralateral tentorial DAVF. Near complete obliteration of the fistula with transarterial Onyx embolization resulted in immediate and complete resolution of facial pain.
Case presentation
A 58-year-old man had been suffering from recurrent facial pain in the second and third division of the right trigeminal nerve for 3 years. The pain was described as moderate, sharp, and electrical in the right cheek. Symptoms were initially well controlled medically. However, 6 months before admission, the frequency and severity increased despite high dose carbamazepine. The patient was referred to our department of neurosurgery for consideration of microvascular decompression. At the time of admission, he was suffering from continuous episodes of paroxysmal, lancinating pain lasting for several minutes. The pain was induced by chewing, swallowing, brushing his teeth, and even talking but without any active trigger zone. There was no history of pulsatile tinnitus or facial numbness. Neurological examination revealed no abnormal findings.
Investigations
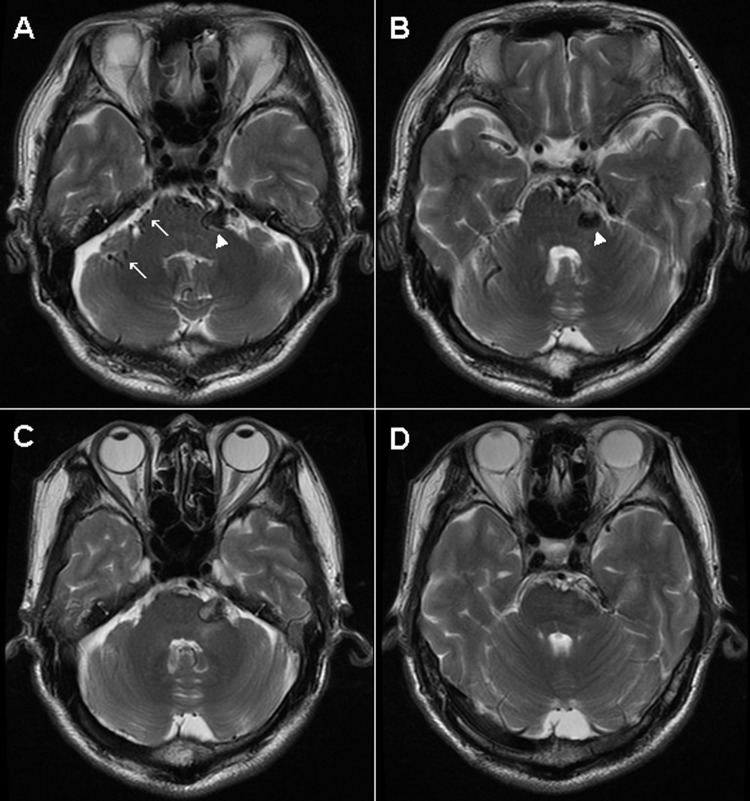
MR imaging demonstrated a variceal venous dilatation occupying the left lateral cerebellopontine cistern. There were multiple venous flow voids located at the right side of the pons adjacent to the right trigeminal nerve root entry zone (figure 1A, B).
Figure 1.
(A, B) Axial T2 weighted MR image showing a variceal venous dilatation occupying the left lateral pontine cistern (arrowhead). Note multiple venous flow voids adjacent to the right trigeminal nerve root entry zone (arrows). (C, D) Axial T2 weighted MR image, 3 months after embolization, showing a thrombosed venous varix and disappearance of any abnormal flow voids adjacent to the right trigeminal nerve root entry zone.
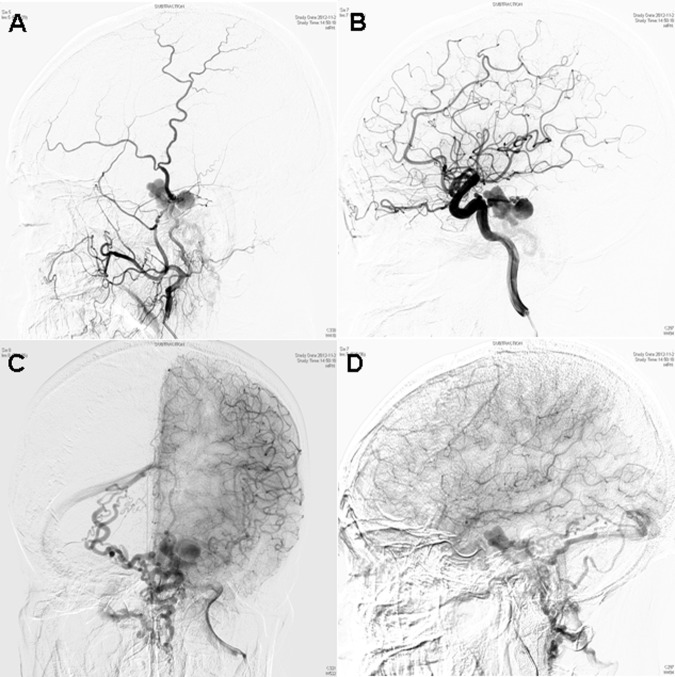
Cerebral angiography revealed a left-sided tentorial DAVF. The fistula was fed by the left middle meningeal artery (MMA) and the meningohypophyseal trunk of the left internal carotid artery. There were dilated tortuous abnormal venous structures noted with a large venous varix, draining across the transverse pontine veins, and then superiorly into the superior petrosal and superior cerebellar hemispheric veins, as well as inferiorly into the retroclival plexus and subsequently into the foramen magnum plexus (figure 2).
Figure 2.
Cerebral angiograms revealing a left-sided tentorial dural arteriovenous fistula. The fistula was fed by the left middle meningeal artery (A) and the meningohypophyseal trunk of the left internal carotid artery (B). Note a large venous varix, draining across the transverse pontine veins and then superiorly into the superior petrosal and superior cerebellar hemispheric veins, as well as inferiorly into the retroclival plexus and subsequently into the foramen magnum plexus, in the anteroposterior projection (C) and lateral projection (D).
Treatment
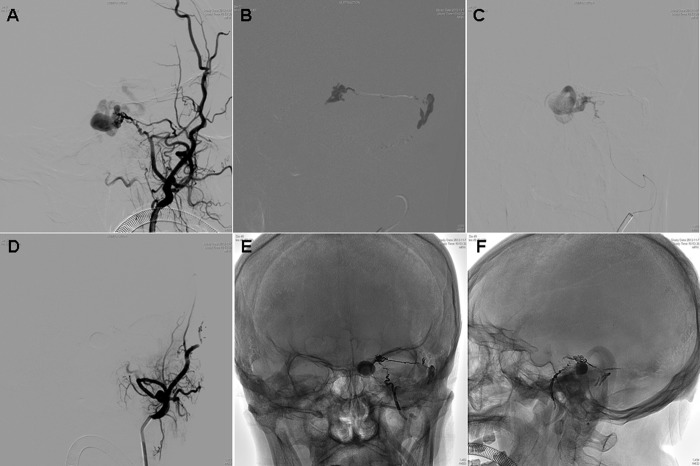
Endovascular embolization was chosen as the preferred modality of treatment over microsurgery, considering the location and bilaterality of drainage. Both branches of the left MMA were embolized with 1.8 mL of Onyx-18 (figure 3). After Onyx embolization, near complete obliteration of the fistula was achieved with mild residual filling via the meningohypophyseal trunk. Additionally, significant stagnation of the venous varix and proximal segment of the draining vein was also observed (figure 4).
Figure 3.
(A) Left external carotid artery angiograms prior to embolization. (B, C) Onyx-18 injection after catheterization via two branches of the left middle meningeal artery. (D) Left external carotid artery angiogram after Onyx embolization (total of 1.8 mL). Plain radiography in anteroposterior (E) and lateral (F) views showing the Onyx cast in the dural arteriovenous fistula.
Figure 4.
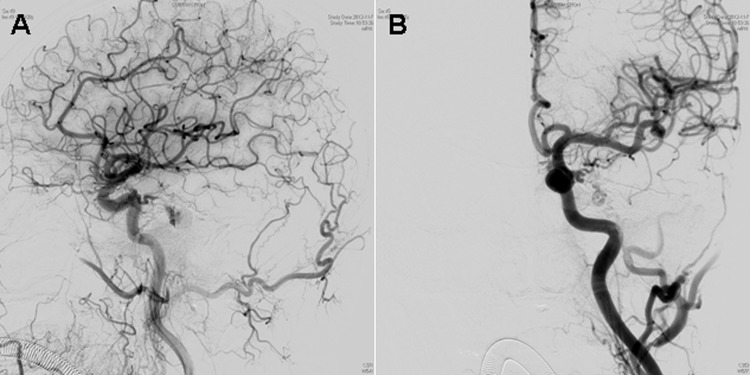
Left common carotid artery angiograms after transarterial embolization, demonstrating near complete obliteration of the fistula with mild residual filling via the meningohypophyseal trunk, in addition to significant stagnation of the venous varix. (A) Lateral projection. (B) Anteroposterior projection.
Outcome and follow-up
Postoperatively, the patient had immediate resolution of his facial pain, without facial nerve palsy. He has been free of the symptom and there was no evidence of recurrence during a follow-up period of 9 months. MR imaging showed a thrombosed venous varix and disappearance of any abnormal flow voids adjacent to the right trigeminal nerve root entry zone (figure 1C, D).
Discussion
Trigeminal neuralgia as a sole clinical manifestation of tentorial DAVFs is extremely uncommon, and the presence of cortical venous reflux makes it vulnerable to hemorrhage. Because of the characteristics of retrograde leptomeningeal venous drainage, tentorial DAVFs often present with fatal posterior fossa hemorrhage or progressive neurological deficits from mechanical neurovascular compression, or progressive venous thrombosis. Until now, tentorial DAVFs manifesting as contralateral trigeminal neuralgia have not been reported previously.
The exact etiology of trigeminal neuralgia associated with DAVFs remains unclear. As previously described,8 the dilated arterialized draining veins of the DAVFs might directly compress the trigeminal nerve at the root entry zone. In our case, multiple venous flow voids adjacent to the right trigeminal nerve root entry zone were observed on MRI scans. Postoperatively, resolution of symptoms accompanied the disappearance of these abnormal flow voids. Therefore, we postulate that trigeminal neuralgia was caused by pulsatile compression from dilated veins due to venous reflux from the contralateral tentorial DAVF. As there was no change in the position of the normal cerebellar arteries, this is in contrast with other authors who suggest that the dilated venous structures cause secondary vascular compression by displacement of the normal superior cerebellar artery.5
The optimal treatment strategy for tentorial DAVFs remains controversial because of their deep seated locations and complicated supplying arteries and draining veins. Treatment options include surgical obliteration, transarterial or transvenous embolization, stereotactic radiosurgery, or a combination of these treatments. Surgical interruption of the draining vein is recommended for Borden type III DAVFs with direct cortical venous drainage. Some authors claimed that transarterial embolization is rarely curative unless combined with surgical intervention.5 However, Ott et al4 reported a case of trigeminal neuralgia caused by a tentorial DAVF that was successfully treated by transarterial embolization with n-butyl cyanoacrylate glue (n-BCA). Du et al1 reported a successfully treated case with transarterial embolization and transvenous embolization with coils and particles. Recently, Onyx has emerged as a new embolic material for the treatment of tentorial DAVFs. The intrinsic properties of Onyx make it easier to control than n-BCA, which in turn result in high DAVF obliteration and low complications rates when compared with n-BCA.10
The availability of a sizable branch of the MMA is critical to transarterial Onyx embolization for tentorial DAVFs. Additionally, to achieve complete obliteration, the microcatheter tip should be positioned at or immediately adjacent to the fistula. Finally, complete filling of the proximal draining vein is pivotal for definitive endovascular cure of these lesions. Although stereotactic radiosurgery has been reported in the treatment of tentorial DAVFs causing trigeminal neuralgia,6 the risk of bleeding remains until complete obliteration of the fistula is obtained 3 years later or more. Thus it should not be considered a first choice for patients with high risk features, such as retrograde leptomeningeal venous drainage.
Learning points.
It is important to exclude vascular lesions in the evaluation of patients with trigeminal neuralgia.
Trigeminal neuralgia may result from compression of dilated veins due to venous reflux from a contralateral tentorial dural arteriovenous fistula (DAVF).
Transarterial Onyx embolization may be effective and safe for the treatment of tentorial DAVFs manifesting as contralateral trigeminal neuralgia.
Footnotes
Contributors: Conception and design: FX and JC. Analysis and interpretation of the data: XL, XQ, LN, and FX. Drafting the article: XL and FX. Critically revising the article: all authors. Reviewed final version of the manuscript and approved it for submission: all authors.
Competing interests: None.
Patient consent: Obtained.
Ethics approval: The study was approved by the Affiliated Hospital of Nantong University.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Du R, Binder DK, Halbach V, et al. Trigeminal neuralgia in a patient with a dural arteriovenous fistula in Meckel's cave: case report. Neurosurgery 2003;2013:216–21 [DOI] [PubMed] [Google Scholar]
- 2.Harders A, Gilsbach J, Hassler W. Dural AV malformation of the lateral and sigmoid sinuses as possible cause of trigeminal neuralgia. Case report. Acta Neurochir (Wien) 1982;2013:95–102 [DOI] [PubMed] [Google Scholar]
- 3.Mendelowitsch A, Radue EW, Gratzl O. Aneurysm, arteriovenous malformation and arteriovenous fistula in posterior fossa compression syndrome. Eur Neurol 1990;2013:338–42 [DOI] [PubMed] [Google Scholar]
- 4.Ott D, Bien S, Krasznai L. Embolization of a tentorial dural arterio-venous fistula presenting as atypical trigeminal neuralgia. Headache 1993;2013:503–8 [DOI] [PubMed] [Google Scholar]
- 5.Ito M, Sonokawa T, Mishina H, et al. Dural arteriovenous malformation manifesting as tic douloureux. Surg Neurol 1996;2013:370–5 [DOI] [PubMed] [Google Scholar]
- 6.Matsushiqe T, Nakaoka M, Ohta K, et al. Tentorial dural arteriovenous malformation manifesting as trigeminal neuralgia treated by stereotactic radiosurgery: a case report. Surg Neurol 2006;2013:519–23 [DOI] [PubMed] [Google Scholar]
- 7.Rahme R, Ali Y, Slaba S, et al. Dural arteriovenous malformation: an unusual cause of trigeminal neuralgia. Acta Neurochir (Wien) 2007;2013:937–41 [DOI] [PubMed] [Google Scholar]
- 8.Lucas Cde P, Zabramski JM. Dural arteriovenous fistula of the transverse-sigmoid sinus causing trigeminal neuralgia. Acta Neurochir (Wien) 2007;2013:1249–53 [DOI] [PubMed] [Google Scholar]
- 9.Akhaddar A, Gazzaz M, Elmostarchid B, et al. Trigeminal neuralgia and dural arteriovenous fistula in an edentulous man. Headache 2010;2013:861–2 [DOI] [PubMed] [Google Scholar]
- 10.Rabinov JD, Yoo AJ, Ogilvy CS, et al. Onyx versus n-BCA for embolization of cranial dural arteriovenous fistulas. J Neurointerv Surg 2013;2013:306–10 [DOI] [PubMed] [Google Scholar]