Abstract
The development of Fournier's gangrene in an 80-year-old male patient with diabetes after a routine outpatient haemorrhoid banding procedure is described. Four days following the procedure, the patient noticed an increasing amount of pain and swelling of the perianal region. When the patient presented to the emergency department 18 days later, immediate radical debridement of ischiorectal necrotic tissue was performed. A defunctioning loop sigmoid colostomy was also formed. Subsequent operations required excision of the scrotum and abdominoperineal excision of the rectum. Histology studies later confirmed the presence of necrotising fasciitis. The case acts as a reminder that clinicians should maintain a high index of suspicion for high-risk patients still suffering from problems following the procedure.
Background
Fournier's gangrene is a rare condition characterised by a rapidly spreading necrotising infection involving the perineum, genitalia and perianal regions. Early clinical recognition of the condition and immediate surgical intervention is essential to avoid patient mortality that has been reported at 22–40%.1
Fournier's gangrene is largely caused by facultative organisms (Escherichia coli, Klebsiella and enterococci) and anaerobes such as Bacteroides, Fusobacterium and Clostridium.2 The anorectal region is plentiful in numbers of such bacterial flora and thus any disruption to the mucosal lining such as that caused by transanal procedures can potentially cause a necrotising infection.
Haemorrhoids are a common condition affecting 4% of the adult population.3 Haemorrhoid rubber band ligation is the most commonly used technique for treating symptomatic internal haemorrhoids refractory to conservative treatment measures.4 It is a favoured technique because of its high success rate of 70–80%5 and low risk of complications.
There have been published reports of sepsis developing following rubber band ligation.6–9 This case describes the development of severe sepsis and Fournier's gangrene in an elderly patient with diabetes and the devastating consequences that occurred as a result. We hope with this case to highlight the need for clinicians to carefully monitor high-risk patients following this commonly performed procedure.
Case presentation
An 80-year-old retired van driver was seen in the outpatient clinic following a history of perianal irritation and pruritus. The patient had previously been investigated for iron-deficiency anaemia and the ensuing endoscopy had demonstrated the presence of diverticulosis and haemorrhoids. On examination at the clinic he was found to have three internal haemorrhoids that were subsequently banded. The patient did not report any discomfort or pain at the time of the procedure.
Four days following the procedure the patient noticed an increasing amount of perianal pain. Eighteen days postprocedure the patient contacted the out-of-hours general practitioner who was concerned that the pain and swelling of the perianal region had increased dramatically. The patient was also becoming febrile and was subsequently sent to the accident and emergency department.
Significant medical history included diet-controlled type 2 diabetes, hypertension and coronary artery bypass and valve replacement surgery in 2009. The patient was an ex-smoker and did not drink any alcohol.
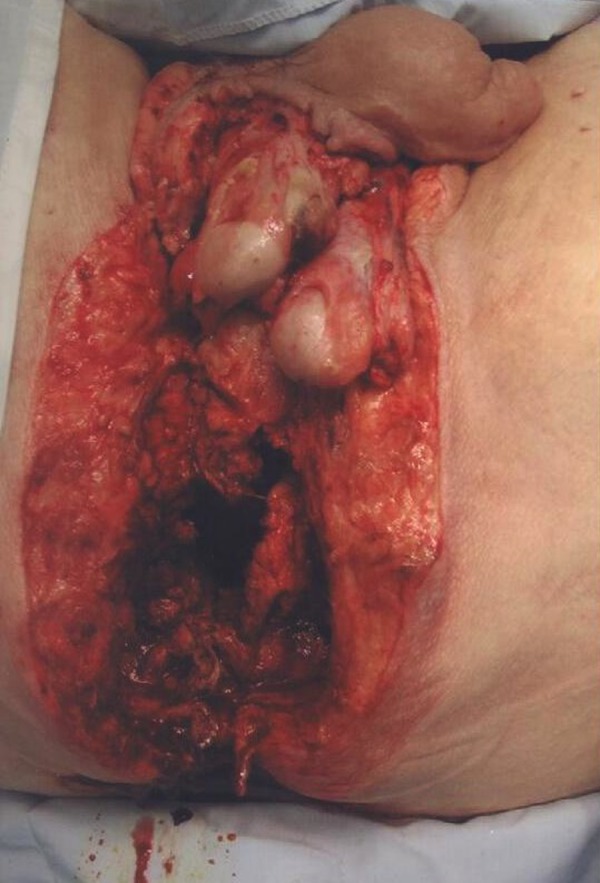
On admission his abdomen was soft and distended with generalised tenderness. Bowel sounds were normal. On examination of his rectum, his anus was noted to be grossly swollen with an approximately sized 10×10 cm right-sided perianal abscess containing necrotic tissue (figure 1). No crepitus was noted.
Figure 1.

Photograph of perineal region taken at initial inspection in lithotomy position before operative intervention. Note the presence of a grossly oedematous anus and presence of necrotic tissue from the 7 to 9 o'clock position with an underlying abscess (approximately 10×10 cm).
Investigations
Initial blood tests taken from the patient at the time of admission are shown in figure 2. Abnormal haematological blood results included a raised white cell count 36.8×109/L, a neutrophil count 34.6×109/L, haemoglobin 12.3 g/L and a raised platelet count 470×109/L. An acute renal failure was demonstrated with an estimated glomerular filtration rate of 32 mL/min. The international normalisation ratio was also mildly elevated at 1.4. No creatine kinase level was performed on admission.
Figure 2.
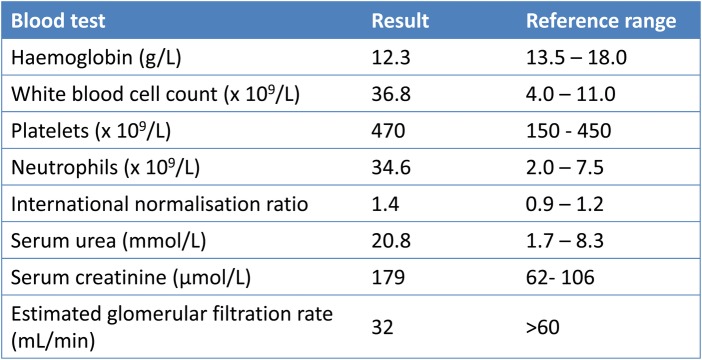
Table outlining blood results of the patient on admission.
Histological analysis of specimens obtained from the initial wound debridement showed large areas of necrosis in the subcutaneous fat (figure 3) and smooth muscle layers (figure 4) with surrounding neutrophil polymorphs. The appearances were consistent with those of necrotising fasciitis. There was no evidence of malignancy. Subsequent samples obtained from the abdominoperineal resection confirmed the distal rectum and anus to also be necrotic.
Figure 3.
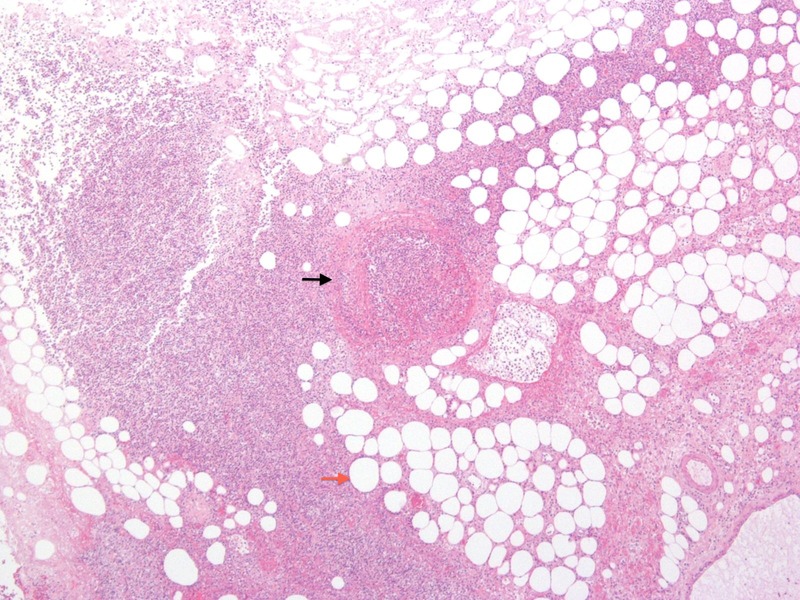
Photomicrograph of necrotic perianal tissue from a subcutaneous layer biopsy. Surrounding neutrophils can be seen around non-viable adipocytes (red arrow). A thrombosed central vessel is present within the necrotic soft tissue (black arrow).
Figure 4.
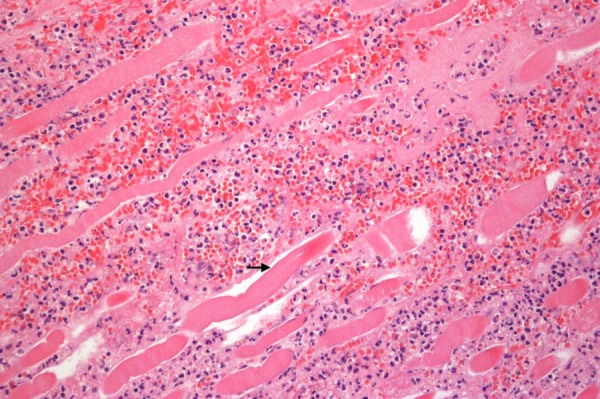
Photomicrograph from the initial wound debridement demonstrating necrotising fasciitis of the smooth muscle layer. Non-viable myocytes (black arrow) are seen with broad bands of polymorphonuclear cell infiltrate along the major fascial planes.
Microbiological analysis confirmed the growth of Escherichia coli and anaerobes.
Differential diagnosis
The diagnosis of necrotising fasciitis is primarily clinical and was obvious in this case due to the presence of gangrene on physical examination (figure 1). Another necrotising condition to consider following disruption to the bowel lining is gas gangrene (Clostridial myonecrosis). The condition typically results from the introduction of organisms of the Clostridium species directly into deep tissue layers causing severe muscle necrosis. Certain features in the history, physical examination and investigations can help distinguish the two conditions but treatment for both diseases essentially remains the same.
An elderly patient with diabetes will be at an increased risk of developing a severe, necrotising infection following an anorectal procedure. Other recognised risk factors include chronic renal failure, hepatic failure, AIDS, malignancy and obesity.10 Features in the history suggestive of Fournier's gangrene include presenting symptoms such as severe perianal pain (commonly out of proportion to physical examination findings), fever and urinary retention.11–14 Gas gangrene typically involves sudden onset of severe pain at the site of injury together with a rapid decline in systemic health as shock and multiple organ failure develops.15
Both Fournier's gangrene and gas gangrene can cause the presence of crepitus on physical examination. Gas gangrene also causes characteristic skin changes that involve an initially pale appearance that then rapidly turns bronze, followed by a red or purple discolouration.15
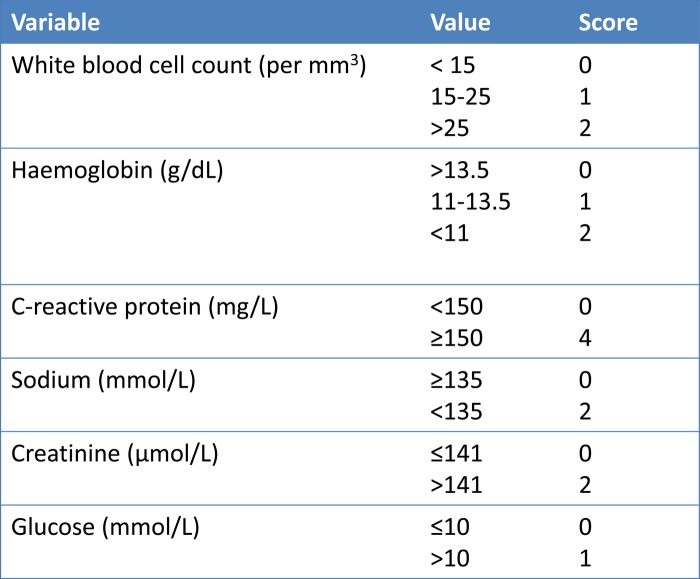
In the absence of overt necrotic tissue it can be difficult to distinguish a necrotising condition from a severe cellulitis. In this scenario, haematological and biochemical results on admission may help. Laboratory findings for Fournier's gangrene may include leukocytosis, coagulopathy, and elevations in the serum creatine kinase and lactate levels although these are generally non-specific.10 The Laboratory Risk Indicator for Necrotizing Fasciitis Score16 (LRINEC) takes into account laboratory findings (figure 5) to help identify necrotising fasciitis where the clinical diagnosis is not immediately obvious. A LRINEC Score of ≥6 was found to have a positive predictive value of 92% and a negative predictive value of 96%.16
Figure 5.
The Laboratory Risk Indicator for Necrotizing Fasciitis Scoring System (LRINEC). Patients with a LRINEC score of ≥6 have a positive predictive value of 92% and a negative predictive value of 96% for necrotising fasciitis.16
Radiological studies can help determine whether gas is spreading along fascial planes or whether deeper muscle tissue is involved, but should not delay surgical intervention. Imaging also cannot reliably distinguish cellulitis from necrotising fasciitis or gas gangrene and hence if there is a clinical suspicion for these latter two conditions, radiographic imaging should not delay surgical intervention.15
Treatment for Fournier's gangrene and gas gangrene consists of urgent supportive therapy, surgical debridement and antibiotic therapy. Both diseases may also require multiple debridements over the course of several days. Definitive diagnosis of either condition requires histopathology testing. Typically gas gangrene involves the absence of acute inflammatory cells from infected tissues, as the arriving polymorphonuclear leucocytes do not cross the vascular endothelium.15 As seen in figures 3 and 4, necrotising fasciitis characteristically does involve the infiltration of acute inflammatory cells.
Treatment
The patient was given intravenous tazobactam, clindamycin and vancomycin as per trust policy for the treatment of necrotising fasciitis.
After initial fluid resuscitation, the patient was immediately taken to the theatre for urgent wound debridement. The initial incision was made over the palpable abscess to the right side of the anus (figure 1) and there was a subsequent release of foul-smelling pus. Necrotic tissue was found in the right ischiorectal tissue and this was excised back to healthy, bleeding tissue. The muscles, genitalia and rectal wall appeared healthy. The wound cavity was packed with ribbon gauze. A defunctioning loop sigmoid colostomy was then formed to help prevent further bacterial translocation into the affected area.
The patient was admitted to the intensive care unit following the operation. Twenty-four hours later the patient returned to theatre for a re-evaluation of the wound. The extent of sepsis appeared to have spread from the initial site with extensive dead tissue, foul-smelling gas and crepitus appearing to involve the scrotal subcutaneous tissue with tracking towards both groins (figure 6). The urology team was involved to excise the scrotum with the testicles left intact.
Figure 6.

Photograph of perineal region taken 24 h following initial presentation. Note the presence of necrotic tissue superior to the anus. There was associated foul-smelling gas and crepitus.
The patient returned to theatre 48 h following the initial presentation. Necrotic tissue was again found to have spread into the right as well as the left ischiorectal fossa and now included the rectal wall. An abdominoperineal excision of the rectum was subsequently performed (figure 7).
Figure 7.
Photograph of perineal region taken 48 h after initial presentation. Necrotic tissue was found to involve the scrotal subcutaneous tissue, rectal wall and both ischiorectal fossae. Subsequently the scrotum was excised (leaving both testicles intact) and an abdominoperineal excision of rectum was performed.
The patient returned to the theatre a fourth time 1 day later and on this occasion no further necrotic tissue was found. The wound was subsequently packed and left open.
Outcome and follow-up
The patient required a refashioning of the colostomy 2 weeks later. He also developed acute renal failure secondary to sepsis. For this he was treated in the intensive care unit with renal replacement therapy and he has since been transferred to a specialist renal ward.
He has made steady progress over the following weeks and is awaiting plastic surgery reconstruction for when he is deemed fit enough for the procedure.
Discussion
Patients with symptomatic haemorrhoids often have relief with conservative measures such as the addition of fibre to the diet or the use of various analgesia creams, hydrocortisone suppositories and sitz baths.4 Patients who continue to experience symptoms despite these measures are candidates for outpatient procedures, such as injection sclerotherapy and rubber band ligation, and day case surgical haemorrhoidectomy.
As discussed previously, banding is the most commonly used technique for the treatment of internal haemorrhoids refractory to conservative treatment. The procedure has been in use since the 1960s and is favoured because of the low costs of treatment, the ease of use, and the lack of anaesthetic requirement.4 In a study by Iyer et al5 involving 805 patients, banding treatment was considered successful in 71% after initial treatment and 80% in those undergoing repeat treatment.
The most frequent complications are pain (8%), delayed haemorrhage 2–4 days following the procedure, localised infection, or very rarely fulminant sepsis.4 It is recommended that only one column of haemorrhoids is treated in a single session to minimise the risk of tissue necrosis although Khubchandani17 found that as many as three bands in a single column may be safely performed.
A number of cases of severe sepsis or ‘pelvic cellulitis’ have been reported that have normally developed 3–10 days following banding for haemorrhoids6–9 but none of these to the extent that has caused the development of a necrotising infection requiring radical surgery to the extent described in this case report.
Fournier's gangrene can result from any breach in the integrity of the gastrointestinal or urethral mucosa.1 It is well recognised that the condition most commonly occurs in older men, particularly in those with diabetes.10
There have been several reported cases of Fournier's gangrene developing following conventional haemorrhoidectomy11–14 and even injection sclerotherapy.18 Cases in the literature make note of the aforementioned presenting symptoms such as fever, urinary retention and perianal pain normally within the first week following surgery. McCloud et al19 did however report a case that occurred 39 days postprocedure. Necrotising infection should be considered in patients exhibiting these clinical features in addition to the presence of crepitus on clinical examination.
It is well recognised that early and aggressive surgical exploration and debridement of necrotic tissue, together with broad spectrum antibiotic therapy and haemodynamic support is indicated with a clinical suspicion of necrotising fasciitis. Radiological studies can help determine whether muscle tissue is involved, but should not delay surgical intervention. The primary goal of surgery is to ensure that all the necrotic tissues are debrided until healthy, bleeding tissues are reached. If antibiotics are used without surgery, mortality for necrotising fasciitis approaches 100%.20
Debrided tissue should always be sent for histological and microbiological analysis to confirm the diagnosis and to help tailor antibiotic therapy. Typical histological findings are those demonstrated in the case: ‘extensive tissue destruction, thrombosis of blood vessels, abundant bacteria spreading along fascial planes and infiltration of acute inflammatory cells’10 (figures 3 and 4).
In the setting of Fournier's gangrene, a cystostomy, colostomy or orchidectomy may be required and the patient should be consented as such for these procedures. The wound should be covered with a sterile dressing and should then be re-evaluated in the theatre within 24 h time.21 Only then should the wound be closed after all the necrotic tissues are completely debrided. Plastic surgery intervention may well be required to cover the defect.
Learning points.
Although uncommon, potentially devastating complications do result from routine procedures for managing haemorrhoids particularly in patients with recognised risk factors such as diabetes, chronic renal failure, hepatic failure, AIDS, malignancy and obesity. As a result, clinicians should maintain a high index of clinical suspicion for such patients still suffering from problems following the procedure.
Banding of only a single column of haemorrhoids should be performed at each session to minimise the risk of sepsis developing. Up to three bands in a single column may be safely performed.17
Following a transanal procedure, patients should always be warned to seek urgent medical attention if any of the following features develop: increasing perianal discomfort, fever or urinary retention. In the absence of obvious clinical signs of necrotising fasciitis, the Laboratory Risk Indicator for Necrotizing Fasciitis Score (LRINEC)16 may be calculated from laboratory findings to aid diagnosis (figure 5).
Any patient suspicious of developing Fournier's gangrene should immediately be started on broad-spectrum antibiotics and admitted to the theatre for aggressive wound debridement until healthy, bleeding tissue is reached.
If gangrenous tissue is found on the initial admission to theatre, a relook inspection should always be performed in 24 h. The patient should be warned as such in the initial consenting procedure, which should also include for the possibilities of permanent stoma formation, cystostomy and orchidectomy.
Footnotes
Contributors: KH, KZ, and MU were the contributing surgeons and provided feedback for treatment and discussion sections.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Stephens BJ, Lathrop JC, Rice WT, et al. Fournier's gangrene: historic (1764–1978) versus contemporary (1979–1988) differences in etiology and clinical importance. Am Surg 1993;59:149. [PubMed] [Google Scholar]
- 2.Eke N. Fournier's gangrene: a review of 1726 cases. Br J Surg 2000;87:718. [DOI] [PubMed] [Google Scholar]
- 3.McCloud JM, Jameson JS, Scott AN. Life-threatening sepsis following treatment for haemorrhoids: a systematic review. Colorectal Dis 2006;8:748–55 [DOI] [PubMed] [Google Scholar]
- 4.Bleday R, Breen E. Treatment of haemorrhoids. Philadelphia, PA: Wolters Kluwer Health, 2012 [Google Scholar]
- 5.Iyer VS, Shrier I, Gordon PH. Long-term outcome of rubber band ligation for symptomatic primary and recurrent internal hemorrhoids. Dis Colon Rectum 2004;47:1364. [DOI] [PubMed] [Google Scholar]
- 6.Scarpa FJ, Hillis W, Sabetta JR. Pelvic cellulitis: a life-threatening complication of hemorrhoidal banding. Surgery 1988;103:383. [PubMed] [Google Scholar]
- 7.Wechter DG, Luna GK. An unusual complication of rubber band ligation of hemorrhoids. Dis Colon Rectum 1987;30:137. [DOI] [PubMed] [Google Scholar]
- 8.Clay LD, III, White JJ, Jr, Davidson JT, et al. Early recognition and successful management of pelvic cellulitis following hemorrhoidal banding. Dis Colon Rectum 1986;29:579–81 [DOI] [PubMed] [Google Scholar]
- 9.Russell TR, Donohue JH. Hemorrhoidal banding. A warning. Dis Colon Rectum 1985;28:291–3 [DOI] [PubMed] [Google Scholar]
- 10.Stevens DL, Baddour LM. Necrotizing soft tissue infections. Philadelphia, PA: Wolters Kluwer Health, 2013 [Google Scholar]
- 11.Bönner C, Prohm P, Störkel S. Fournier gangrene as a rare complication after stapler hemorrhoidectomy. Case report and review of the literature. Chirurg 2001;72:1464–6 [DOI] [PubMed] [Google Scholar]
- 12.Giebel GD. Comment on Bonner et al. Fournier gangrene as a rare complication after stapler hemorrhoidectomy. Case report and review of the literature. Chirurg 2002;73:288. [DOI] [PubMed] [Google Scholar]
- 13.Gurfinkel R, Slovik Y, Glezinger R, et al. Fournier's gangrene as a delayed complication of closed hemorrhoidectomy. Harefuah 2005;144:394–6 456, 455 [PubMed] [Google Scholar]
- 14.Lehnhardt M, Steinstraesser L, Druecke D, et al. Fournier's gangrene after Milligan-Morgan hemorrhoidectomy requiring subsequent abdominoperineal resection of the rectum: report of a case. Dis Colon Rectum 2004;47:1729–33 [DOI] [PubMed] [Google Scholar]
- 15.Stevens D, Bryant B. Clostridial myonecrosis. Philadelphia, PA: Wolters Kluwer Health, 2012 [Google Scholar]
- 16.Wong CH, Khin LW, Heng KS, et al. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med 2004;32:1535–41 [DOI] [PubMed] [Google Scholar]
- 17.Khubchandani IT. A randomized comparison of single and multiple rubber band ligations. Dis Colon Rectum 1983;26:705–8 [DOI] [PubMed] [Google Scholar]
- 18.Kaman L, Aggarwal S, Kumar R, et al. Necrotizing fascitis after injection sclerotherapy for hemorrhoids: report of a case. Dis Colon Rectum 1999;42:419–20 [DOI] [PubMed] [Google Scholar]
- 19.McCloud JM, Doucas H, Scott ADN, et al. Delayed presentation of life-threatening perineal sepsis following stapled haemorrhoidectomy: a case report. Ann R Coll Surg Engl 2007;89:301–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: diagnosis and management. Clin Infect Dis 2007;44:705. [DOI] [PubMed] [Google Scholar]
- 21.Sudarsky LA, Laschinger JC, Coppa GF, et al. Improved results from a standardized approach in treating patients with necrotizing fasciitis. Ann Surg 1987;206:661. [DOI] [PMC free article] [PubMed] [Google Scholar]