Abstract
Students who teach less experienced students within the same educational program are known as near-peer teachers. A number of studies have shown that near-peers are effective teachers in preclinical courses such as anatomy and physical examination. We hypothesized that near-peers could also be effective teachers in a clinical clerkship. We report on a pilot study in which near-peers participated in a training session and then taught a brief problem-focused skills curriculum to third-year students during a required ambulatory medicine rotation. The clerkship students assigned high ratings to the near-peer teachers, both on an absolute scale and relative to faculty. The results suggest that including near-peers as teachers in a clinical clerkship may be appropriate and that this concept deserves further investigation.
Keywords: near-peer teaching, medical clerkship, student facilitator
Introduction
A near-peer has been defined as “a trainee who is one or more years senior to another trainee on the same level of medical education training (i.e., medical students teaching other medical students, residents teaching other residents)” [1]. We report on the implementation of near-peer teaching in a single session, problem-focused patient examination curriculum in a third-year ambulatory medicine clerkship at the Yale School of Medicine (YSM). We also discuss the history and theoretical basis of near-peer teaching.
Background
In 1986, Hendelman et al. implemented peer teaching in a gross anatomy laboratory at the University of Ottawa’s Faculty of Health Sciences. Compared with staff teaching, peer teaching resulted in similar knowledge acquisition among learners, as well as improved study habits and communication skills and better attitudes [2]. Such themes are not unique to such historical studies but actually inform theoretical frameworks that support the contemporary implementation of near-peer teaching.
If we view learning, or the organization of knowledge in long-term memory, as a cognitive network of concepts and relations, continuously added to, modified, and tuned, it is sensible to conclude that experts have a different, more complex knowledge structure than that of the novices they teach. Cornwall et al. first proposed that a teacher with a more similar network would better understand the cognitive problems encountered by the student [3]. Further, minimizing the distance between what is known and what needs to be learned, the “zone of proximal development,” optimizes learning [4]. Lockspeiser et al. provided support for this “cognitive congruence theory” in near-peer teaching settings with a quantitative analysis of survey scores from first-year medical students taught by second-year students in the Medical Scholars Program at the University of California, San Francisco [5]. This study showed that near-peer teachers could empathize with their students, teach at an appropriate level, and anticipate learning problems, thereby reframing their teaching methods to accommodate.
Similarly, “social congruence” has also been postulated as a beneficial effect of near-peer teaching. In this setting, the near-peer teacher lacks the authority held by a faculty expert, and rather than doling out reward or punishment according to the behavior of the learner, the near-peer teacher instead offers support as a friend and role model [6]. “Role theory” suggests that a near-peer teacher with sufficient knowledge may facilitate learning more so than a senior faculty member. Mitigation of the pressure felt by the student may actually improve motivation to study and lower inhibition to reveal ignorance or cognitive errors, thus allowing for enhanced correction by the near-peer teacher compared with that from an authority figure [7]. Students have even reported feeling that their near-peer teachers were more interested in their daily lives and personalities compared with faculty [8]. Seeing the success of these role models can alleviate the anxiety felt by junior students about the future and help them build confidence that they can similarly succeed in their medical studies [5]. Finally, senior students as teachers also offer the benefit of being able to pass down the so-called “hidden curriculum,” or the unwritten rules on how to get through medical school not typically taught in the lecture hall [6].
Along with benefits to the learner, near-peer teaching offers secondary positive effects on the student serving as the teacher. These students often report a greater understanding of the topic they had prepared to teach compared with the knowledge acquired from standard staff teaching [2]. Further, it has been shown that students who teach achieve significantly higher United States Medical Licensing Examination (USMLE) step 1 and 2 scores as well as final medical school grade point averages compared to those who do not [9]. Ten Cate et al. describe the Bales’ Learning Pyramid, an often-cited but not well-founded hierarchy of teaching methods, which suggests that while listening to lectures only results in 5 percent recall of subject material, teaching others leads to 80 percent recall [6]. This may occur because when students prepare to teach, they process the information in a goal-oriented way: to choose how the content should be explained and to anticipate what questions the learners may have. It is argued that this type of information processing optimizes memory retrieval of the subject matter better than when preparing for what an expert teacher may ask on a test [10]. Likewise, verbalization and recitation have long been regarded as key learning methods and certainly contribute to the benefits of student teaching [6]. A qualitative study of student tutor-led problem-based learning groups in a physiotherapy program showed that the senior students felt they had improved their facilitation and communication skills through the program [11].
In reciprocal peer teaching (RPT), classmates rotate the roles of teacher and learner. Bentley et al. described the implementation of RPT in an anatomy course in which students could perform dissection only when they were acting as “teachers” [15]. Many students felt that they had insufficient hands-on experience because they could not perform dissection when they were acting as “learners.” Another study instead used the near-peer facilitator method with fourth-year medical students teaching anatomy to first and second years. This method circumvented the aforementioned limitations of RPT because all of the lower class students taking the course were able to dissect in every session, and the senior students gained advanced teaching skills and improved knowledge of anatomy [12]. Even in settings where there is a low faculty-to-student ratio, near-peer teaching in anatomy allows for increased small-group educational opportunities and interactions with teachers [13]. Other uses for near-peer teaching include classroom-based tutorials and physical exam sessions for preclinical students, which have been shown to help the junior students better consolidate newly learned medical information and improve end-of-module written examination scores [14,15].
There is a paucity of objective data in the literature assessing the acceptance and outcomes of near-peer teaching programs in medical schools, and the literature is scarce regarding the implementation of near-peer teaching for advanced students during their clinical (typically third) year; however, there are a few published studies reporting the effects. One study demonstrated the benefits of having fourth-year students practice clinical cases with third-years to help them prepare for the USMLE Step 2 Clinical Skills exam. There were no statistically significant differences in ratings of student preceptors versus faculty preceptors, and junior students reported valuing the feedback provided to them through the workshop [16]. Interestingly, another study found that third-year students taught surgical skills by fourth-year students performed better in an objective exercise, which included entering the operating room, performing a pelvic exam on a pelvic simulator, and beginning an abdominal hysterectomy using a simulated patient, compared to those taught by obstetrics and gynecology residents. The authors speculated that the junior students may have found the near-peer environment to be less threatening and more informal, and thus more comfortable and suitable for learning [17]. Studies such as the above suggest that near-peers can be effective teachers in the clinical clerkships. We explored this hypothesis with a pilot study in which we trained four near-peers to be facilitators alongside of faculty in an established two-hour problem-focused examination curriculum taught within a required third-year clerkship. We compared the learners’ evaluations of the near-peers with those of faculty and also asked the near-peers to reflect upon their experience.
Methods
In the Ambulatory Medicine Clerkship at the YSM, students are assigned to outpatient practices 3.5 days each week for 4 weeks. The other 1.5 days are devoted to small group didactic and experiential “workshops” addressing topics such as hypertension and low back pain that students are likely to encounter at their clinical sites. Three years ago, one of the authors (FH) originated a new workshop in problem-focused patient examination, with the goal of helping students acquire skills for performing an efficient and effective outpatient visit. A model called the problem-focused pathway was constructed that included the major steps and sub-divisions of a focused interview and physical examination. This course seeks to expand students’ knowledge and understanding of patient history taking as well as teaches physical exam skills. The workshop begins with a brief discussion of goals and objectives and an explanation of the pathway. The learners are then divided into breakout groups consisting of two to three students and a facilitator. In the breakout groups, students practice the model using a series of structured role plays guided by the facilitator who hands out scripts and checklists, keeps time, leads a debrief, distributes case notes, provides instructional feedback, and coaches students on their communication, reasoning, and physical examination skills. The innovation was to replace a few members of the faculty with senior (fourth- and fifth-year) medical students who served as near peer teachers. To prepare for their teaching responsibility, all four near peers were required to attend a 2-hour group training led by faculty in June 2012. The training included discussions and hands-on practice with a number of different topics, including the problem-focused model, the logistics or flow of learning activities during the workshop, small group teaching skills, knowledge pertaining to the four clinical cases, and review of relevant clinical skills. Facilitators were also presented with literature pertaining to the workshop content as well as teaching skills [1,5,18]. Before facilitating the sessions on their own, near-peer teachers first observed one complete workshop between June and November, after which they were able to sign up as facilitators for future dates. Student facilitators were expected to lead at least two workshops over the course of the academic year. At the end of each workshop, the clerkship students completed an anonymous evaluation form on which they were asked to rate the overall value, quality of the workshop cases, background material, and effectiveness of the facilitator on a scale of 0 (lowest) through 10 (highest) and comment on the overall value of the workshop with suggestions as to how it might be improved. This study was conducted in an established educational setting involving normal educational practices and was thus exempt from Institutional Review Board review.
Results
Between June 1, 2012, and January 31, 2013, four near-peers completed the training and taught in a total of nine workshops. Students in each group ranged from two to three, with a mean of 2.67 and a median of 3. One hundred percent of evaluations were completed, as this was a requirement before leaving the session. Evaluations were completed anonymously. Twenty-four evaluations from nine workshop breakout groups led solely by near-peer facilitators have been completed. Mean scores from the surveys were 9.75 ± 0.53 for overall value, 9.58 ± 0.65 for quality of the workshop cases, 9.17 ± 1.30 for background material, and 9.96 ± 0.20 for effectiveness of the facilitators. The highest scores were for the two categories most relevant to teaching: overall value and effectiveness of the facilitator. In accordance with these scores, the participants of the workshop commented that they “really enjoyed having student facilitators for teaching” and “found student facilitators to be very helpful.” They also noted that the facilitators did “wonderful work with solid feedback” and that it was “nice to have an SMD (student MD) perspective.”
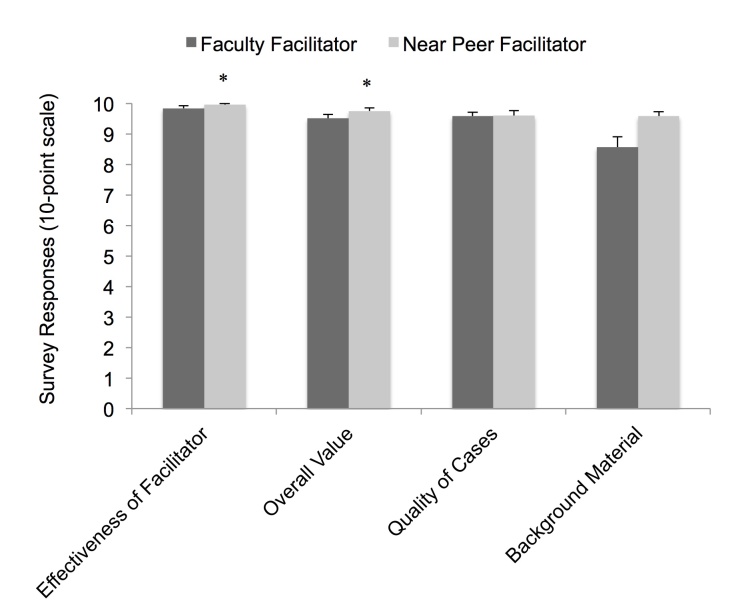
The evaluations of near-peer facilitators with those of faculty facilitators in the four quantitatively measurable categories — overall value, quality of the workshop cases, background material, and effectiveness of the facilitators ― were also compared. A total of 43 faculty evaluations from 18 breakout groups were tabulated and compared with the 24 near-peer evaluations from nine breakout groups across the measured categories using the student’s t test with p < 0.05 being significant (Figure 1). There were no significant differences between the student ratings of the near-peer facilitators and faculty facilitators in the quality of cases (9.58 ± 0.65 vs. 9.58 ± 0.79; p = 0.68) and background material categories (9.17 ± 1.30 vs. 8.56 ± 2.24; p = 0.14). The ratings of the near-peers were significantly higher than those of faculty in the perceived overall value of the workshop (9.75 ± 0.53 vs. 9.51 ± 0.77; p = 0.02) and the effectiveness of the facilitator categories (9.96 ± 0.20 vs. 9.84 ± 0.53; p = 0.03).
Figure 1.
Evaluation of near-peer teaching experience by student learners. Error bars represent standard deviations. *p < 0.05.
Discussion
In this pilot study, we explored the hypothesis that near-peers could be effective teachers in a structured clinical skills curriculum within a required third-year clerkship. The results show that teaching by near-peers was highly rated and compared favorably with that of faculty. The four near-peers were drawn to participate in this pilot study by the opportunity to participate in the development of an innovative program for helping students to become better teachers, in keeping with the expectation of the Accreditation Council of Graduate Medical Education that residents will educate students, peers, and other health care professionals. The near-peer educators were in the unique position of being able to help more junior students in areas with which they had struggled in the recent past. The student learners reported feeling more comfortable with near-peer facilitators and were very open to asking questions and engaging in dialogue. This was particularly important in an environment where students were practicing the clinical examination on each other, an activity that is often associated with some discomfort and insecurity. Such negative feelings may have been further amplified by the workshop taking place during the third year, a time when many students believe that they should already have mastery over the clinical examination. If faculty preceptors were present, they may have been less likely to ask questions given their perception of the material as “basic” or “something everyone should know by now.”
Limitations
Limitations to our study include the following:
The absence of randomization might have resulted in highly motivated students volunteering as near-peers or highly motivated learners being assigned to near-peer facilitators. The sample, therefore, may not have been representative of the student body.
Student performance was not measured as an objective outcome, for example, by using a psychometric test or direct observation in the clinic. In this pilot study, the questionnaires were used to assess the general acceptance of the near-peer program by the medical students and to provide qualitative comments about strengths and areas for future improvement.
This study did not control for student biases in the evaluations of facilitators. Such biases may arise from an affinity that peers may feel toward one another or a respect for faculty. These biases could potentially “inflate” the ratings given to both types of facilitators. However, to minimize the impact of these biases and potential inflation, all evaluations were filled out anonymously and collected by administrative staff after the facilitators had left the room.
Conclusions
We participated in the design, implementation, and evaluation of a near-peer teaching program for third-year students at YSM, which was received favorably by the students and earned strong reviews. It also provided an opportunity for medical students to improve their teaching skills prior to residency. We have provided some suggestions on how to develop a near-peer teaching workshop for medical students in the clinical years (Table 1). Future research investigating the effectiveness of faculty and near-peer facilitators with an objective outcome measure may be helpful to better address whether learners benefit as much from near-peers as from faculty facilitators.
Table 1. Yale School of Medicine: Suggestions for Near-Peer Teaching*.
| 1. Near-peer teachers should be students who have recently completed the course. This provides enough cognitive congruence to facilitate the peer-to-peer learning process as well as sufficient incongruence in order to ensure that it is an instructional process rather than a purely collaborative process. |
| 2. Near-peer teachers should be actively included in the design and implementation of the near-peer portion of the education curriculum. |
| 3. Prior to the initial teaching session, near-peer educators should be oriented to areas that past students have found challenging and encouraged to provide input in areas that they themselves perceived as difficult. |
| 4. A low teacher:pupil ratio should be maintained. In our case, the ratio was approximately 1:3; however, other studies of near-peer teaching have used ratios as high as 1:10 and 1:15 [13]. |
| 5. Individual educator and curriculum evaluations should be used to further the growth of the near-peer educators and assess the success of the near-peer curriculum. |
*These suggestions were compiled from written and verbal feedback from students, near-peer educators, and faculty who participated in this pilot teaching program.
Abbreviations
- RPT
reciprocal peer teaching
- USMLE
United States Medical Licensing Examination
- YSM
Yale School of Medicine
Author contributions
Ms. Meller, Ms. Chen, and Mr. Chen contributed in the conception and design of the manuscript as well as drafting of the manuscript. Ms. Meller wrote the introduction, background, and abstract; Ms. Chen wrote the near-peer perspective section, conclusions, and suggestions for how to develop a near-peer workshop; Mr. Chen wrote the sections describing the innovation and the student learner perspective and performed the initial data collection. Dr. Haeseler supervised drafting of the manuscript. All authors contributed in analysis and interpretation of data and in revising the manuscript critically for intellectual content.
Disclosures
The authors of this paper voluntarily participated as faculty and near-peer teachers in the program discussed.
References
- Bulte C, Betts A, Garner K, Durning S. Student teaching: views of student near-peer teachers and learners. Med Teach. 2007;29(6):583–590. doi: 10.1080/01421590701583824. [DOI] [PubMed] [Google Scholar]
- Hendelman WJ, Boss M. Reciprocal peer teaching by medical students in the gross anatomy laboratory. J Med Educ. 1986;61(8):674–680. doi: 10.1097/00001888-198608000-00007. [DOI] [PubMed] [Google Scholar]
- Cornwall M. Students as teachers: peer teaching in higher education. Technical report. Centrum voor Onderzoek van Wetenschappelijk Onderwijs, University of Amsterdam; 1979. p. 7906-01. [Google Scholar]
- Ten Cate O, Snell L, Mann K, Vermunt J. Orienting teaching toward the learning process. Acad Med. 2004;79:219–228. doi: 10.1097/00001888-200403000-00005. [DOI] [PubMed] [Google Scholar]
- Lockspeiser TM, O’Sullivan P, Teherani A, Muller J. Understanding the experience of being taught by peers: the value of social and cognitive congruence. Adv Health Sci Educ Theory Pract. 2006;13(3):361–372. doi: 10.1007/s10459-006-9049-8. [DOI] [PubMed] [Google Scholar]
- Ten Cate O, Durning S. Dimensions and psychology of peer teaching in medical education. Med Teach. 2007;29(6):546–552. doi: 10.1080/01421590701583816. [DOI] [PubMed] [Google Scholar]
- Topping K. Trends in peer learning. Educ Psych. 2005;25:631–645. [Google Scholar]
- Moust JHC, Schmidt HG. Facilitating small-group learning: a comparison of student and staff tutors’ behavior. Instruct Sci. 1995;22:287–301. [Google Scholar]
- Wong JG, Waldrep TD, Smith TG. Formal peer-teaching in medical school improves academic performance: the MUSC supplemental instructor program. Teach Learn Med. 2007;19(3):216–220. doi: 10.1080/10401330701364551. [DOI] [PubMed] [Google Scholar]
- Bruner J. The act of discovery. Harvard Educ Rev. 1961;(31):21–32. [Google Scholar]
- Solomon P, Crowe J. Perceptions of student peer tutors in a problem-based learning programme. Med Teach. 2001;23(2):181–186. doi: 10.1080/01421590020031101. [DOI] [PubMed] [Google Scholar]
- Evans DJ, Cuffe T. Near-peer teaching in anatomy: an approach for deeper learning. Anat Sci Educ. 2009;2(5):227–233. doi: 10.1002/ase.110. [DOI] [PubMed] [Google Scholar]
- Duran CE, Bahena EN, Rodriguez M, Baca GJ, Uresti AS, Elizondo-Omana RE. et al. Near-peer teaching in an anatomy course with a low faculty-to-student ratio. Anat Sci Educ. 2012;5(3):171–176. doi: 10.1002/ase.1269. [DOI] [PubMed] [Google Scholar]
- Jackson TA, Evans DJ. Can medical students teach? A near-peer-led teaching program for year 1 students. Adv Physiol Educ. 2012;36(3):192–196. doi: 10.1152/advan.00035.2012. [DOI] [PubMed] [Google Scholar]
- Dickson JM, Harrington R, Carter MJ. Teaching clinical examination using peer-assisted learning amongst graduate-entry students. Clin Teach. 2011;8(1):8–12. doi: 10.1111/j.1743-498X.2010.00417.x. [DOI] [PubMed] [Google Scholar]
- Colaco SM, Chou CL, Hauer KE. Near-peer teaching in a formative clinical skills examination. Med Educ. 2006;40(11):1129–1130. doi: 10.1111/j.1365-2929.2006.02593.x. [DOI] [PubMed] [Google Scholar]
- Graziano SC. Randomized surgical training for medical students: resident versus peer-led teaching. Am J Obstet Gynecol. 2011;204(6):542-e1. doi: 10.1016/j.ajog.2011.01.038. [DOI] [PubMed] [Google Scholar]
- Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130(5):1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]