Abstract
Background
Total hip (THA) and knee arthroplasty (TKA) are common procedures in elderly persons, who are at potential increased risk of postoperative fall due to loss of muscle strength and impaired balance. Fast-track surgery with early mobilization and opioid-sparing analgesia have improved outcomes after these procedures, but early mobilization and short hospitalization length of stay (LOS) could potentially increase the risk of falls after discharge. We investigated injuries, circumstances, and the timing of fall-related hospital admissions 90 days after fasttrack THA and TKA.
Methods
This was a prospective, descriptive multicenter study on fall-related hospital admissions, in 5145 elective fast-track THA and TKA patients, with complete 90-day follow up through the Danish National Patient registry and medical charts.
Results
Of 83 (1.6%) fall-related hospital admissions, 43 (51.8%) were treated in the Emergency Room and 40 (48.2%) were admitted to a regular ward. The median LOS after surgery was 3 days (interquartile range [IQR]: 2–3) in fallers versus (vs) 2 days (IQR: 2–3) (P=0.022) in patients without falls. Injuries were classified as “none” or minor in 39.8%, moderate in 9.6%, and major in 50.6%. Most falls (54.8%) occurred within 1 month of discharge. Falls due to physical activity (12.0%) and extrinsic factors (14.5%) occurred later than did surgery-related falls (73.5%), contributing to 40% of all falls >30 days after discharge. In multivariate analysis, age (odds ratio [OR]: 1.05; 95% confidence interval [CI]: 1.0–1.08) (P=0.001), living alone (OR: 2.09; 95% CI: 1.20–3.62) (P=0.009), and psychiatric disease (OR: 2.80; 95% CI: 1.42–5.50) (P=0.001) were associated with surgery-related falls, whereas the use of a walking aid (OR: 1.20; 95% CI: 0.67–2.16) (P=0.544) and LOS ≤4 days (OR:1.19; 95% CI: 0.52–1.28) (P=0.680) was not.
Conclusion
Hospital admissions due to falls are most frequent within the first month after fast-track THA and TKA. The overall incidence of surgery-related falls amongst these patients is low, declines after the first month, and is related to patient characteristics rather than short LOS. The effect of interventions aimed at surgery-related falls should focus on the first 30 days after surgery and differentiate between the causes of falling.
Keywords: orthopedic, risk, falls, postoperative, osteoarthrosis
Introduction
Falls are common in the elderly, both in and out of hospital,1–7 with potential severe consequences, including fractures and other injuries, as well as more lasting effects, such as disability and fear of falling.2,8 Studies have found in-hospital fall rates after elective orthopedic surgery of about 1%,1,2,4 related to age, gender, and comorbidity1,4 or the use of femoral local anesthetic neural blockade.1,9 Several studies have tried to identify patient characteristic and circumstances associated with falling,3,5,10 to develop strategies for fall-prevention in community dwellers and medical patients3,11 but not in elective arthroplasty patients after discharge. During recent years, length of hospital stay (LOS) after elective total hip arthroplasty (THA) and total knee arthroplasty (TKA) has decreased steadily,12 despite an increasing number of elderly patients with increasing burden of comorbidity.12,13 The approach, known as “fast-track” surgery, has been shown to decrease LOS without increasing overall readmission rate after surgery,14 including THA and TKA.15–17 The implementation of fast-track protocols for elective THA and TKA in Denmark has resulted in a national decline of LOS from about 10 days in 2000 to 4 days in 2009,18 with the majority of departments using fast-track principles for all patients regardless of age and comorbidity.17,18
Early and persistent muscle loss occurs after THA and TKA,19 and as impaired balance and poor walking ability is associated with falling,7,20 patients could be at increased risk of falling within the first months of these surgeries. In this context, there is concern that early mobilization and short LOS could potentially further increase the risk of falls after discharge, just as there are concerns about other serious complications.21 However, as fast-track surgery has been shown to improve recovery, it could also be speculated that a faster return to everyday life could result in a number of falls being related to increased level of activity rather than the surgery per se. Such a distinction would also be of importance for studies on fall interventions, to further improve outcome after fast-track THA and TKA.
The aim of this study was to conduct a detailed analysis on falls resulting in hospital admission ≤90 days after fasttrack THA and TKA, with regards to the length of time after the index surgery, the circumstances leading to falling, and to fall-related injuries. We also attempted to identify risk factors for falls considered related to surgery, using multiple logistic regression.
Material and methods
The Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement database prospectively collects data on preoperative patient characteristics in consecutive unselected patients receiving fast-track elective primary THA and TKA at seven participating departments. Data are collected using a questionnaire, which is completed within 1 month before surgery by the patient (with assistance from staff if needed).17 All departments are high-volume centers (>400 operations/year), with similar perioperative procedures, including spinal anesthesia, multimodal opioid-sparing analgesia without the standard use of peripheral nerve blocks, early mobilization, and functional discharge criteria and discharge to home.22 Adherence to the fast-track protocol is the standard of care in all the departments, and thus, all patients are treated according to fast-track principles, regardless of age and comorbidity. Data on the index admission, with regards to LOS, and data on 90-day readmissions and mortality were acquired from the Danish National Patient Register, which registers all hospitalizations and procedures performed at any Danish hospital, thus ensuring complete follow up.24 The discharge papers were evaluated for relevance to the index surgery, and if this was insufficient to determine the cause of readmission, the entire medical record was evaluated by the first author, with assistance from the senior author (HK) in cases of doubt.
For this study we analyzed all hospital admissions, including Emergency Room visits where fall was mentioned as the cause of admission in the discharge papers, for patients who had previous primary elective unilateral THA or TKA between Feb 1, 2010 and Dec 1, 2011 in the six participating departments. We also investigated the medical records on possibly fall-related readmissions (ie, hip displacements of unspecified causes) in order to not overlook any falls. A fall was defined as “an event that results in a person coming to rest inadvertently on the ground or other lower level and other than as a consequence of the following: sustaining a violent blow; falling out of bed while sleeping; loss of consciousness; or sudden onset of paralysis, as in a stroke or an epileptic seizure.”8 Falls were categorized according to the type of subsequent injury, as: no injury, minor injury (minor cuts, minor bleeding from abrasions, swelling, and minor contusions), moderate injury (bleeding requiring cauterization, lacerations requiring suturing, temporary loss of consciousness, and soft tissue trauma), or severe injury (fractures, dislocation, major head trauma, injury requiring additional surgery, cardiac arrest, and death).2 Additionally, the patients were classified into three groups based on the circumstances of the falls (from information contained in the medical charts): surgery-related falls (falls due to sudden muscle weakness or indisposition and any fall during normal daily activities, such as walking around the house, going to the bathroom, etc), falls related to more pronounced physical activity (activities with increased physical demand, such as ladder climbing, strenuous exercise, bicycling, etc), and falls related to extrinsic factors (slippery surfaces, pushed by closing doors, alcohol intoxication, etc). In cases where no information regarding the fall circumstances was available, the fall was assumed to have happened during normal daily activities and therefore considered to be a surgery-related fall. This was done to avoid underestimating the number of falls due to surgery.
The need for informed consent for completion of the study questionnaire was waivered by the Scientific Ethics Committee Central Region as the questionnaire is part of the standard preoperative procedure. Permission was acquired from the Danish National Board of Health and the Danish Data Protection Agency to review and keep medical records, without patient consent. The Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement database is registered as an ongoing observational study and registry.23
Data were analyzed using the Mann-Whitney U-test and t-test for continuous data. Chi-squared test and Fisher’s exact test were used for categorical data as appropriate. Logistic regression analysis, using surgery-related falls as the dependent variable, was initially done using univariate analysis on patient characteristics. Female gender, living with others, THA and absence of walking aids, smoking, disease, etc were considered as reference for categorical variables, while age and body mass index (BMI) were considered as continuous variables. Any variable with a P-value<0.25 was included in a backwards stepwise multiple logistic regression model. For all final analyses, a P-value of<0.05 was considered statistically significant. Analyses were done using SPSS v 20 (IBM Corporation, Armonk, NY, USA).
Results
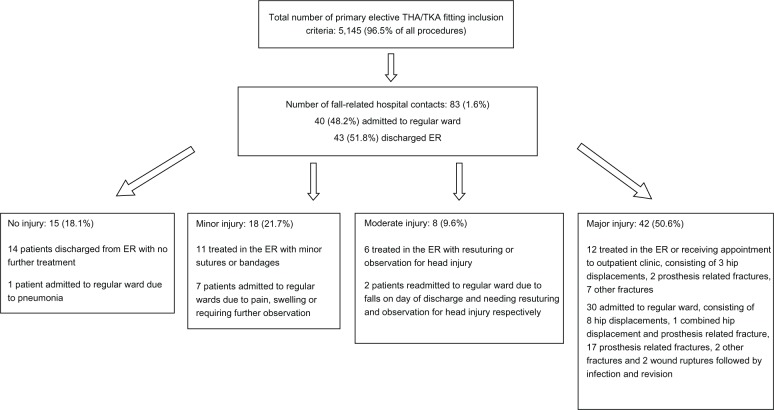
A total of 5145 (2696 THA, 2449 TKA) procedures were performed. Of these patients, 83 (1.6%) were admitted to hospital due to a postsurgery fall, with two patients being admitted twice. Another 12 falls were excluded from analyses as these were due to primary loss of consciousness, falling from bed during sleep, etc (Figure 1).
Figure 1.
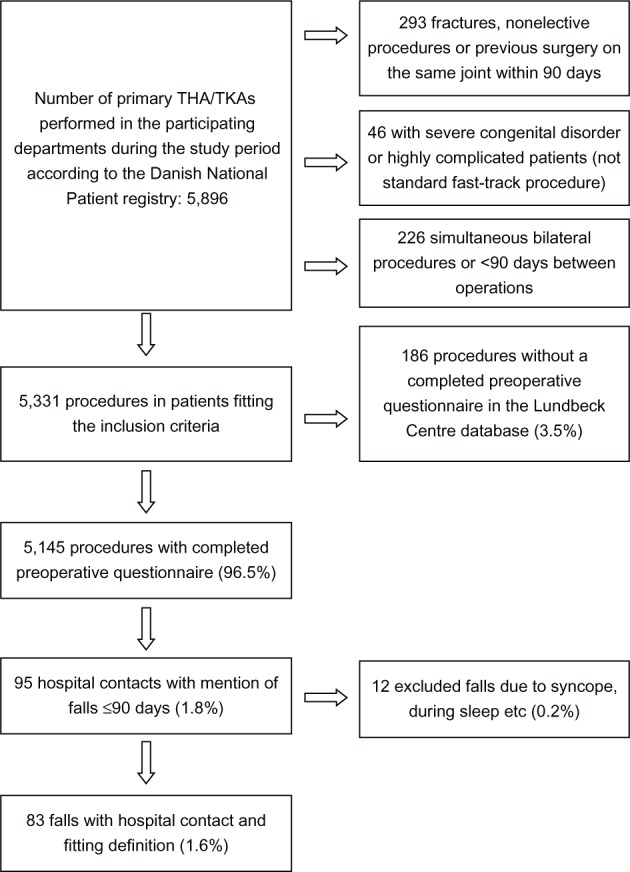
Flow chart of the study population.
Abbreviations: THA, total hip arthroplasty; TKA, total knee arthroplasty.
The mean age of patients who fell was 70.8 yrs (range 39–96) versus (vs) 67.3 (range 18–97) (P=0.004) without falls, and a larger fraction of fallers lived alone (55.4% vs 33.3%) (P<0.001) and used walking aids (41.2% vs 25.8%) (P=0.002). The median LOS during the primary admission was 3 days (interquartile range [IQR]: 2–3) in fallers vs 2 days (IQR: 2–3) in patients without falls (P=0.022) (Table 1).
Table 1.
Patient characteristics
| Variablea | Fallers (n=83) |
Nonfallers (n=5,062) |
P-value |
|---|---|---|---|
| Age mean (range; SD) |
70.8 yrs (39–96; 12.0) |
67.3 yrs (18–97; 10.8) |
0.004 |
| Gender | 0.704 | ||
| Females | 49 (59) | 2,883 (57) | |
| Males | 34 (41) | 2,179 (43) | |
| BMI mean (range; SD) |
27.3 (18.1–51.6; 5.7) |
28.4 (14.3–60.8; 5.1) |
0.064 |
| Missing | 1 (1.2) | 26 (0.5) | |
| Joint | 0.578 | ||
| THA | 46 (55.4) | 2,650 (52.4) | |
| TKA | 37 (44.6) | 2,412 (47.6) | |
| Use of walking aid | 0.002 | ||
| Yes | 33 (41.2) | 1,273 (25.8) | |
| No | 47 (58.8) | 3,663 (74.2) | |
| Missing | 3 (3.6) | 126 (2.5) | |
| Social situation | <0.001 | ||
| Living with others | 35 (42.2) | 3,327 (65.7) | |
| Living alone | 46 (55.4) | 1,687 (33.3) | |
| Nursing home, etc | 2 (2.4) | 48 (0.9) | |
| Alcohol >2 units daily | 0.695 | ||
| Yes | 5 (6.3) | 371 (7.4) | |
| No | 75 (93.8) | 4,639 (92.6) | |
| Missing | 3 (3.6) | 52 (1.0) | |
| Diabetes | 0.104 | ||
| Yes | 14 (17.1) | 570 (11.3) | |
| No | 68 (82.9) | 4,531 (88.6) | |
| Missing | 1 (1.2) | 29 (0.6) | |
| Treatment for CD | 0.284 | ||
| Yes | 7 (8.5) | 621 (12.5) | |
| No | 75 (91.5) | 4,359 (87.5) | |
| Missing | 1 (1.2) | 82 (1.6) | |
| Treatment for PD | 0.606 | ||
| Yes | 5 (6.1) | 382 (7.6) | |
| No | 77 (93.9) | 4,633 (92.4) | |
| Missing | 1 (1.2) | 47 (0.9) | |
| Treatment for PsD | <0.001 | ||
| Yes | 16 (20.0) | 346 (6.9) | |
| No | 64 (80.0) | 4,672 (93.1) | |
| Missing | 3 (3.6) | 44 (0.9) | |
| Primary LOS | 0.022 | ||
| Median (IQR) | 3 (2–3) | 2 (2–3) | |
| Mean (range) | 3.1 (1–7) | 2.9 (1–34) |
Note:
Results presented as number of cases (%) unless otherwise specified.
Abbreviations: BMI, body mass index; CD, cardiac disease; IQR, interquartile range; LOS, length of hospital stay; PD, pulmonary disease; PsD, psychiatric disease; SD, standard deviation; THA, total hip arthroplasty; TKA, total knee arthroplasty; yrs, years.
According to the medical charts, 61 (73.5%) falls were classified as surgery-related falls, 12 (14.5%) were caused by extrinsic factors, and ten (12.0%) were related to physical activity (Table 2). In 43 (51.8%) cases, the falls were treated in the Emergency Room without transfer to a regular ward, while 40 (48.2%) required at least one overnight admission to a ward. In 42 (50.6% of all falls) cases, the fall resulted in major injury, although 12 of these patients were discharged directly from the Emergency Room with either no further treatment or an outpatient appointment (Figure 2). Major injuries were the most common consequence of falling, regardless of circumstances, consisting of 45.9%, 66.7%, and 60.0% of the surgery-related, extrinsic factors-related, and physical activity–related falls groups, respectively. Moderate injury was least frequent (9.6% of all falls), and with five in the surgery-related (8.2% of surgery-related falls), one in the extrinsic factors–related (8.3% of extrinsic factors–related falls), and two in the physical activity–related falls group (20% of physical activity–related falls). We found 18 (21.7% of all falls) falls resulting in minor injuries, of which 15 were surgery related (24.6% of surgery-related falls), two were due to extrinsic factors (16.7% of extrinsic factor–related falls), and one was due to physical activity (10.0% of physical activity–related falls). There were 13 falls resulting in no injury in the surgery-related falls group (21.3% of surgery-related falls) and only one in both the extrinsic factors-related (8.3%) and physical activity–related falls groups (10.0%), respectively. We found no overall difference between the severity of injury and the circumstances of falling (P=0.587).
Table 2.
Causes of falling
| Physical activity-related | Extrinsic factors-related | Surgery-related |
|---|---|---|
| Bicycle fall, n=2 | Intoxicated, n=4 | Bathroom related, n=7 |
| Fall from exercise bike, n=1 | Slipped on ice, n=4 | Sudden indisposition, n=3 |
| Fall from ladder, n=2 | Pushed by closing doors, n=2 | Sudden muscle-weakness, n=3 |
| Fall from rooftop, n=1 Fall from motorized vehicle, n=1 |
Slippery floor, n=1 Accidentally pushed by others, n=1 |
Slipping during daily activities, n=14 |
| Fall while gardening, n=1 | Insufficient information, n=34 | |
| Fall due to exhaustion after prolonged walking, n=1 | ||
| Total, n=10 | Total, n=12 | Total, n=61 |
Figure 2.
Falls according to treatment (emergency room vs regular ward) and injury type.
Abbreviations: ER, Emergency Room; THA, total hip arthroplasty; TKA, total knee arthroplasty; vs, versus.
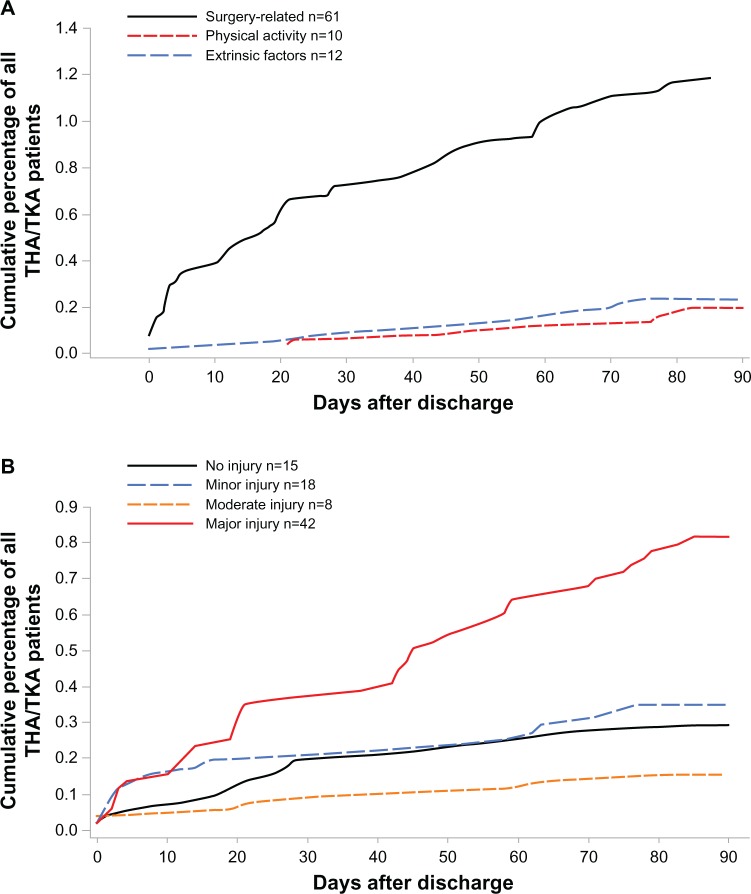
Falls were most frequent during the early discharge period, with 24.1% occurring within the first week and 51.8% within the first month. Although there was no difference in the occurrence of major injuries (35% vs 57%, respectively) (P=0.084), we found more minor injuries (40% vs 16%) (P=0.023) during the first week (Figure 3A and B). The surgery-related falls occurred from the day of discharge and throughout the study period, while falls related to extrinsic factors and physical activity generally had a later onset (Figure 3A). However, there were two very early falls due to extrinsic factors, caused by a slippery floor (day of discharge) and an accidental push (13 days after discharge) respectively. Correspondingly, the fraction of surgery-related falls declined from 19/20 (95.5% of all falls) during the first week to 18/23 (78.3%) between days 8–30 and to 24/40 (60.0%) between days 31–90 after discharge.
Figure 3.
Cumulated incidence of falls: (A) according to circumstances and (B) according to injury.
Abbreviations: THA, total hip arthroplasty; TKA, total knee arthroplasty.
Univariate logistic regression analyses on the 61 surgery-related falls found the following variables to be included in the stepwise multiple logistic regression analysis: age, BMI, use of walking aids, social situation, diabetes, and pharmacologically treated psychiatric disease. After excluding nonsignificant variables, the final model was based on 5098 patients with 59 falls and the following variables found to be related to falling: age (odds ratio [OR]: 1.05), living alone (OR: 2.09), and pharmacologically treated psychiatric disease (OR: 2.80). The preoperative use of walking aids and LOS ≤4 days were not found to be associated with surgery-related falls, in multiple logistic regression analysis (Table 3).
Table 3.
Logistic regression analysis of surgery-related falls only
| Variable | Univariate analysis OR (95% CI) | P-value | Multivariate analysisa OR (95% CI) | P-value |
|---|---|---|---|---|
| Age/yrs | 1.05 (1.03–1.08) | <0.001 | 1.05 (1.02–1.08) | 0.001 |
| Females vs males | 1.34 (0.79–2.27) | 0.272 | – | – |
| BMI | 0.96 (0.91–1.01) | 0.115 | 0.97 (0.92–1.02) | 0.248 |
| THA vs TKA | 1.00 (0.61–1.66) | 0.993 | – | – |
| Use of walking aid | 2.18 (1.29–3.67) | 0.004 | 1.20 (0.67–2.16) | 0.544 |
| Social situationb | – | 0.001 | – | 0.033 |
| Living alone | 2.75 (1.64–4.61) | ,0.001 | 2.09 (1.20–3.62) | 0.009 |
| Nursing home, etc | 2.72 (0.36–20.51) | 0.331 | 1.48 (0.19–11.68) | 0.709 |
| Alcohol >2 units daily | 0.67 (0.21–2.15) | 0.499 | – | – |
| Diabetes | 1.96 (1.04–3.71) | 0.039 | 1.69 (0.87–3.29) | 0.122 |
| Pharmacologically treated CD | 0.93 (0.42–2.06) | 0.861 | – | – |
| Pharmacologically treated PD | 0.64 (0.20–2.05) | 0.449 | – | – |
| Pharmacologically treated PsD | 3.06 (1.58–5.95) | 0.001 | 2.80 (1.42–5.50) | 0.001 |
| LOS ≤4 days | 0.63 (0.30–1.33) | 0.223 | 1.19 (0.52–2.77) | 0.680 |
| Primary LOS/days | 1.02 (0.92–1.13) | 0.723 | – | – |
Notes:
Number of falls in the final model was 59, due to missing data
living with others as reference.
Abbreviations: BMI, body mass index; CD, cardiac disease; CI, confidence interval; LOS, length of hospital stay; OR, odds ratio; PD, pulmonary disease; PsD, psychiatric disease; THA, total hip arthroplasty; TKA, total knee arthroplasty; yrs, years.
Discussion
This prospective study on causes and circumstances of falls ≤90 days after fast-track THA and TKA reveals several new aspects on falls in the immediate postoperative period. The first of these is that the incidence of fall-related hospital admissions was about 1.6% but resulted in admission to a regular ward in <1%. Secondly, about one-fourth of all fall-related hospital admissions did not appear to be directly related to surgery, and thirdly, short LOS did not increase the risk of surgery-related falls.
The low incidence of falls resulting in admission to a regular ward suggests readmissions due to falls do not compose a major safety problem within 90 days of fast-track THA and TKA. There have been several studies investigating the incidence of falls in the community-dwelling elderly5,8,25 and after discharge in medical and mixed patient groups.26,27 However, we are not aware of studies on falls after discharge in specific elective surgical populations, except for those related to muscle weakness after peripheral nerve blocks, which often find falls to be more frequent.9
Importantly, although the incidence of falls decreased with time after discharge, with 24% occurring within the first week and more than half during the first month, this was not related to LOS ≤4 days, consistent with findings in patients discharged from medical wards.27 About 40% of falls ≤1 week after surgery resulted in less serious injury, while the number of falls resulting in major injuries remained stable during the study period. This difference may be due to patients being most worried about fall-related injuries in the early postoperative period but could also be a consequence of the return to preoperative level of activity, as the physical activity-related falls often resulted in major injuries. In this context, it must be considered that although almost 50% of falls were treated in the Emergency Room only, more than half resulted in major injuries, often with long LOS and serious morbidity in those patients who required additional surgery due to fractures, wound infections, etc (≈36%).
Another important finding of our study was that 12.0% and 14.5% of all falls were due to physical activity and extrinsic factors, respectively, and that these generally occurred later than the surgery-related falls. Paradoxically these falls could be a consequence of success, as the intention of fast-track surgery is to enhance postoperative recovery, hereby enhancing return to a normal level of activity. It seems unlikely that postoperative interventions targeting falls related to postoperative muscle weakness and impaired balance would be effective in preventing physical activity– and extrinsic factor-related falls. Whether postoperative restrictions, which are usually meant to reduce risk of hip dislocation and excessive prosthetic wear (although neither is evidence based),28 would reduce the number of falls related to physical activity and extrinsic factors is speculative and seems unreasonable considering the rarity of these events. More importantly, as up to 30% and 80% reductions in muscle strength has been found after THA and TKA, respectively,19,29 intensive physiotherapy in the early postoperative phase may be indicated as a rational intervention for reducing surgery-related falls. This seems both rational, with regards to reducing muscle weakness and balance impairment,30 and safe as the feasibility of early progressive strength training has been demonstrated in TKA.31
The fact that about 25% of all falls and 40% of the late falls were found to be unrelated to surgery is important in itself, considering that studies using large databases for risk-factor identification4 rarely have such detailed data to distinguish between the specific circumstances resulting in adverse events.32
Whether the falls caused by extrinsic factors, such as slippery surfaces and closing doors, should be categorized as surgery-related falls can be debated as postoperative balance impairment could make these patients more vulnerable to falling. Also, one could argue that patients with alcohol use >2 units daily should be identified and treated preoperatively as this could reduce falls related to alcohol intoxication. However, whether patients are more prone to falling on slippery surfaces due to recent surgery is uncertain, and only one of the four patients who fell while intoxicated had reported a preoperative alcohol use of >2 units daily. Consequently, it is unlikely that perioperative risk stratification or intervention would be able to predict and prevent these falls.
In multiple regression analysis on surgery-related falls, we found that increasing age, living alone, and pharmacologically treated psychiatric disease increased the risk of a surgery-related fall. As impaired balance and physical fitness are common in the elderly,33 this is not surprising, especially considering that the consequences of falling are more severe in the oldest people.25 However, in this context, it is interesting that the regular use of walking aids ceased to be a significant risk factor after multivariate adjustments. Neither LOS ≤4 days nor total LOS were related to the surgery-related falls, suggesting that early discharge, per se, does not increase the risk of falling upon return to the home environment. The relationship between pharmacologically treated psychiatric disease and falls is consistent with previous findings of these drugs being associated with falls.10,33 As this was the most important predictor of falling, it raises the question of a possible benefit of a critical evaluation of psychiatric medication in the early postoperative period; however, falls only happened in about 4% of these patients. Finally, the association between falls and living alone is also consistent with previous findings of increased severity of falls when lying on the floor for a longer period25 and with a higher fraction of the oldest patients living alone. The results regarding those living in institutions are inconclusive due to limited numbers, although studies with participants from care homes commonly report high fall rates.5,11,25
Our study has some limitations, primarily with regard to the detection and classification of falls. Patients falling after discharge sustaining no or minor injury may not have contacted a hospital and were thus not included in the analysis, making underreporting of falls a potential bias and skewing the severity of fall-related injuries. Also, if falls were not mentioned in the discharge papers, it would not be registered. This is especially important with regards to Emergency Room contacts, where the level of details registered is often limited. We did try to minimize the impact of this by investigating the complete medical records of all readmissions that could potentially be due to falling and believe this approach to be superior to using administrative data alone. Secondly, our classification on falls was entirely dependent on details from medical records with differences in level of detail. However, this was why we chose to categorize falls with insufficient information for classification as surgery-related falls, thus avoiding underestimating the number of falls due to fasttrack surgery. Regarding patient characteristics, we did not analyze the type or dose of pharmacological psychiatric treatment. This could be problematic as there may have been differences among those using low-dose antidepressants and highly potent antipsychotic medicine. Also, although we have not found major between-hospital differences in patient characteristics, and despite all departments having a similar fast-track procedure, such differences could still have influenced the results of the multiple regression analysis. However, the limited number of events prevented more detailed analysis. The strengths of our study include: prospective data on patient characteristics, a well-defined fast-track procedure, and complete 90-day follow up through the Danish National Patient Registry.
Despite the limitations, we believe that our results show that falls leading to hospital contact and readmission after fast-track THA and TKA are conclusive with regards to the safety of early discharge. Future studies on preoperative risk stratification should differentiate between the causes of falling when attempting to identify patients at risk and focus on the potential preventive effect of improvements in muscle function30 and balance.7
Acknowledgments
The study was sponsored by a grant from the Lundbeck Foundation (R25-A2702). The Lundbeck Foundation had no influence on any stage of the study process or on the manuscript.
The members of the Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement Collaborative Group were clinical investigators of this study and helped with implementation of the study procedures at their respective institutions and with critical revision of the manuscript: Kjeld Soeballe, Orthopedic Department, Århus University Hospital; Torben B Hansen, Orthopedic Department, Holstebro Hospital; Henrik Husted, Orthopedic Department, Hvidovre Hospital; Mogens B Laursen, Farsoe Clinic, Orthopedic Department, Aalborg University Hospital; and Lars T Hansen, Orthopedic Department, Sydvestjysk Hospital Grindsted; Per Kjaersgaard-Andersen, Orthopedic Department, Vejle Hospital.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Mandl LA, Lyman S, Quinlan P, Bailey T, Katz J, Magid SK. Falls among patients who had elective orthopaedic surgery: a decade of experience from a musculoskeletal specialty hospital. J Orthop Sports Phys Ther. 2013;43(2):91–96. doi: 10.2519/jospt.2013.4349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ackerman DB, Trousdale RT, Bieber P, Henely J, Pagnano MW, Berry DJ. Postoperative patient falls on an orthopedic inpatient unit. J Arthroplasty. 2010;25(1):10–14. doi: 10.1016/j.arth.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 3.Health Quality Ontario Prevention of falls and fall-related injuries in community-dwelling seniors: an evidence-based analysis. Ont Health Technol Assess Ser. 2008;8(2):1–78. [PMC free article] [PubMed] [Google Scholar]
- 4.Memtsoudis SG, Dy CJ, Ma Y, Chiu YL, Della Valle AG, Mazumdar M. In-hospital patient falls after total joint arthroplasty: incidence, demographics, and risk factors in the United States. J Arthroplasty. 2012;27(6):823–828.e1. doi: 10.1016/j.arth.2011.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robinovitch SN, Feldman F, Yang Y, et al. Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet. 2013;381(9860):47–54. doi: 10.1016/S0140-6736(12)61263-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morris ME. Preventing falls in older people. BMJ. 2012;345:e4919. doi: 10.1136/bmj.e4919. [DOI] [PubMed] [Google Scholar]
- 7.Clemson L, Fiatarone Singh MA, Bundy A, et al. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ. 2012;345:e4547. doi: 10.1136/bmj.e4547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ. Fear of falling and restriction of mobility in elderly fallers. Age Ageing. 1997;26(3):189–193. doi: 10.1093/ageing/26.3.189. [DOI] [PubMed] [Google Scholar]
- 9.Johnson RL, Kopp SL, Hebl JR, Erwin PJ, Mantilla CB. Falls and major orthopaedic surgery with peripheral nerve blockade: a systematic review and meta-analysis. Br J Anaesth. 2013;110(4):518–528. doi: 10.1093/bja/aet013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mion LC, Chandler AM, Waters TM, et al. Is it possible to identify risks for injurious falls in hospitalized patients? Jt Comm J Qual Patient Saf. 2012;38(9):408–413. doi: 10.1016/s1553-7250(12)38052-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oliver D, Connelly JB, Victor CR, et al. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2007;334(7584):82. doi: 10.1136/bmj.39049.706493.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirksey M, Chiu YL, Ma Y, et al. Trends in in-hospital major morbidity and mortality after total joint arthroplasty: United States 1998–2008. Anesth Analg. 2012;115(2):321–327. doi: 10.1213/ANE.0b013e31825b6824. [DOI] [PubMed] [Google Scholar]
- 13.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308(12):1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248(2):189–198. doi: 10.1097/SLA.0b013e31817f2c1a. [DOI] [PubMed] [Google Scholar]
- 15.Malviya A, Martin K, Harper I, et al. Enhanced recovery program for hip and knee replacement reduces death rate. Acta Orthop. 2011;82(5):577–581. doi: 10.3109/17453674.2011.618911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kehlet H. Fast-track hip and knee arthroplasty. Lancet. 2013;381(9878):1600–1602. doi: 10.1016/S0140-6736(13)61003-X. [DOI] [PubMed] [Google Scholar]
- 17.Jørgensen CC, Kehlet H, Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement Collaborative Group Role of patient characteristics for fast-track hip and knee arthroplasty. Br J Anaesth. 2013;110(6):972–980. doi: 10.1093/bja/aes505. [DOI] [PubMed] [Google Scholar]
- 18.Husted H, Jensen CM, Solgaard S, Kehlet H. Reduced length of stay following hip and knee arthroplasty in Denmark 2000–2009: from research to implementation. Arch Orthop Trauma Surg. 2012;132(1):101–104. doi: 10.1007/s00402-011-1396-0. [DOI] [PubMed] [Google Scholar]
- 19.Holm B, Thorborg K, Husted H, Kehlet H, Bandholm T. Surgery-induced changes and early recovery of hip-muscle strength, leg-press power, and functional performance after fast-track total hip arthroplasty: a prospective cohort study. PLoS One. 2013;8(4):e62109. doi: 10.1371/journal.pone.0062109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwendimann R, Bühler H, De Geest S, Milisen K. Characteristics of hospital inpatient falls across clinical departments. Gerontology. 2008;54(6):342–348. doi: 10.1159/000129954. [DOI] [PubMed] [Google Scholar]
- 21.Pulido L, Parvizi J, Macgibeny M, et al. In hospital complications after total joint arthroplasty. J Arthroplasty. 2008;23(6 Suppl 1):139–145. doi: 10.1016/j.arth.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 22.Husted H, Solgaard S, Hansen TB, Søballe K, Kehlet H. Care principles at four fast-track arthroplasty departments in Denmark. Dan Med Bull. 2010;57(7):A4166. [PubMed] [Google Scholar]
- 23.Rigshospitalet Length of Stay and Complications in High-risk Patients Receiving Fast-track Total Hip (THA) or Knee- Alloplasty (TKA) Available from http://clinicaltrials.gov/ct2/show/NCT01515670. NLM identifier: NCT01515670Accessed February 1, 2013
- 24.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(Suppl 7):30–33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 25.Fleming J, Brayne C, Cambridge City Over-75s Cohort (CC75C) Study Collaboration Inability to get up after falling, subsequent time on floor, and summoning help: prospective cohort study in people over 90. BMJ. 2008;337:a2227. doi: 10.1136/bmj.a2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vogler CM, Sherrington C, Ogle SJ, Lord SR. Reducing risk of falling in older people discharged from hospital: a randomized controlled trial comparing seated exercises, weight-bearing exercises, and social visits. Arch Phys Med Rehabil. 2009;90(8):1317–1324. doi: 10.1016/j.apmr.2009.01.030. [DOI] [PubMed] [Google Scholar]
- 27.Mahoney JE, Palta M, Johnson J, et al. Temporal association between hospitalization and rate of falls after discharge. Arch Intern Med. 2000;160(18):2788–2795. doi: 10.1001/archinte.160.18.2788. [DOI] [PubMed] [Google Scholar]
- 28.Swanson EA, Schmalzried TP, Dorey FJ. Activity recommendations after total hip and knee arthroplasty: a survey of the American Association for Hip and Knee Surgeons. J Arthroplasty. 2009;24(Suppl 6):120–126. doi: 10.1016/j.arth.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 29.Holm B, Kristensen MT, Bencke J, Husted H, Kehlet H, Bandholm T. Loss of knee-extension strength is related to knee swelling after total knee arthroplasty. Arch Phys Med Rehabil. 2010;91(11):1770–1776. doi: 10.1016/j.apmr.2010.07.229. [DOI] [PubMed] [Google Scholar]
- 30.Bandholm T, Kehlet H. Physiotherapy exercise after fast-track total hip and knee arthroplasty: time for reconsideration? Arch Phys Med Rehabil. 2012;93(7):1292–1294. doi: 10.1016/j.apmr.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 31.Jakobsen TL, Husted H, Kehlet H, Bandholm T. Progressive strength training (10 RM) commenced immediately after fast-track total knee arthroplasty: is it feasible? Disabil Rehabil. 2012;34(12):1034–1040. doi: 10.3109/09638288.2011.629019. [DOI] [PubMed] [Google Scholar]
- 32.Davis CL, Pierce JR, Henderson W, et al. Assessment of the reliability of data collected for the Department of Veterans Affairs national surgical quality improvement program. J Am Coll Surg. 2007;204(4):550–560. doi: 10.1016/j.jamcollsurg.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 33.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–935. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]