Summary
Background and objectives
Hispanic patients undergoing chronic dialysis are less likely to receive a kidney transplant compared with non-Hispanic whites. This study sought to elucidate disparities in the path to receipt of a deceased donor transplant between Hispanic and non-Hispanic whites.
Design, setting, participants, & measurements
Using the US Renal Data System, 417,801 Caucasians who initiated dialysis between January 1, 1995 and December 31, 2007 with follow-up through 2008 were identified. This study investigated time from first dialysis to first kidney transplantation, time from first dialysis to waitlisting, and time from waitlisting to kidney transplantation. Multivariable Cox regression estimated cause-specific hazard ratios (HRCS) and subdistribution (competing risk) hazard ratios (HRSD) for Hispanics versus non-Hispanic whites.
Results
Hispanics experienced lower adjusted rates of deceased donor kidney transplantation than non-Hispanic whites (HRCS, 0.77; 95% confidence interval [95% CI], 0.75 to 0.80) measured from dialysis initiation. No meaningful differences were found in time from dialysis initiation to placement on the transplant waitlist. Once waitlisted, Hispanics had lower adjusted rates of deceased donor kidney transplantation (HRCS, 0.66; 95% CI, 0.64 to 0.68), and the association attenuated once accounting for competing risks (HRSD, 0.79; 95% CI, 0.77 to 0.81). Additionally controlling for blood type and organ procurement organization further reduced the disparity (HRSD, 0.99; 95% CI, 0.96 to 1.02).
Conclusions
After accounting for geographic location and controlling for competing risks (e.g., Hispanic survival advantage), the disparity in access to deceased donor transplantation was markedly attenuated among Hispanics compared with non-Hispanic whites. To overcome the geographic disparities that Hispanics encounter in the path to transplantation, organ allocation policy revisions are needed to improve donor organ equity.
Introduction
For most patients with ESRD, kidney transplantation is the optimal treatment providing a longer life expectancy and improved quality of life at a lower cost compared with long-term dialysis (1–4). Yet, although more than 70,000 Americans are placed on the waitlist for a kidney transplant, fewer than 18,000 receive a transplant per year (5). Inequities in access to kidney transplantation among racial and ethnic minorities have been recognized for many years. Although these disparities have been extensively documented in African Americans (6–10), other studies have shown that Asians, American Indians, and Hispanics experience decreased access to kidney transplantation as well (11–14).
In an effort to reduce disparities among racial and ethnic groups, changes to the allocation algorithm for kidneys from deceased donors were implemented to lessen the importance of HLA matching (15,16). However, racial and ethnic disparities persist due to the limited organ supply, patient-level factors (socioeconomic, immunologic risk factors) (17–20), transplant program practices (waitlist practices, use of extended criteria donor kidneys, organ acceptance) (21), and the variation in organ supply and demand in different organ procurement organizations (OPOs) (22,23).
Hispanics represent the largest minority group in the United States (comprising 16.3% of the population) and are almost twice as likely to develop kidney failure compared with non-Hispanic whites (24,25). Among ESRD patients in the United States, the proportion of Hispanics newly added to the transplant waiting list has increased from 11.3% to 16.7% within the last 10 years, whereas the proportions of newly listed Caucasians, African Americans, and Asians have remained the same or started to slightly decline (26). Prior observational studies have found that Hispanics were less likely to be placed on the transplant waiting list (11,14), experienced longer waiting times (27), or were less likely to receive a transplant compared with non-Hispanic whites (11,14). However, few studies have analyzed the effect of competing risks (e.g., death) and geographic residence in potentially perpetuating the disparate access to kidney transplantation among Hispanics.
In this study, we investigated differences in the pathway to deceased donor transplantation among Hispanics compared with non-Hispanic whites and specifically examined the effect of ethnic differences in patient demographics, comorbidities, and geographic location (i.e., designated OPO).
Materials and Methods
Study Population
From the US Renal Data System (USRDS), the national registry of individuals with ESRD, we identified all adult (aged 18–75 years) Caucasian patients who initiated dialysis between January 1, 1995 and December 31, 2007 and were followed through 2008. We excluded patients who did not survive or who received a transplant within the first 90 days. We also excluded patients who were preemptively waitlisted. We obtained kidney transplant data from the United Network for Organ Sharing (UNOS) Kidney Wait List file and Kidney Transplant files. Among patients who received more than one kidney transplant, only the first transplant was included in our analysis.
Patient Characteristics
All patient characteristics were obtained from the Centers for Medicare and Medicaid Services Medical Evidence Report (MER; form CMS-2728-U3), which is completed for every patient initiating treatment for ESRD. In addition to sociodemographic characteristics, information regarding dialysis modality, certain comorbid conditions, and few biometric data are recorded on this form.
We obtained patient-level information including designated OPO, time to placement on the transplant waitlist, and kidney transplantation from the UNOS Kidney Wait List file and Kidney Transplant File. We assigned a proxy OPO to patients not waitlisted based on the shortest distance from their residences to transplant facilities.
We obtained information on the date and causes of death from the Cause of Death form (Form 2746) and the USRDS Standard Patients File.
Variables of Interest
Exposure: Hispanic Ethnicity.
A patient’s Hispanic ethnicity was identified if the provider checked the box indicating Hispanic, Hispanic Mexican, or Hispanic other (item 8) on the MER (version 1995). In the updated MER (version 2005), Hispanics were identified if the provider checked Hispanic or Latino (item 9), otherwise the patient was categorized as non-Hispanic.
Outcomes.
We abstracted patient files for one of three potential events: deceased donor transplant, living donor transplant, and death. All patients were administratively censored on January 1, 2009 regardless of the outcome. We considered patients lost to follow-up if the last date observed in the claims or treatment history files was before January 1, 2009. Time from the start of dialysis to receipt of the first deceased donor kidney transplant (with placement on the waitlist) was the primary event of interest. We considered living donor transplant, deceased donor kidney transplant without placement on the waitlist, death, and loss to follow-up as “competing events.”
To further characterize the transition from dialysis initiation to transplantation, we examined two distinct steps on the path to deceased donor transplantation: (1) time from dialysis initiation to transplant waitlisting, and (2) time from waitlisting to deceased donor transplantation among patients waitlisted.
Covariables
Demographic and Health Characteristics.
We defined each patient’s age at initiation of dialysis (categorized for stratified analyses into 18–39, 40–59, 60–75 years), sex, dialysis modality (hemodialysis versus peritoneal dialysis), body mass index (BMI; in kg/m2, categorized into <18.5, 18.5–24.9, 25.0–29.9, 30.0–39.9, ≥40.0, missing), and insurance payer status (health maintenance organization, Medicare primary part A and B, Medicare primary other, Medicare secondary payer with or without employer group health plan, 90-day waiting period, and other). Selected comorbid conditions included the reported presence of diabetes, history of hypertension, congestive heart failure, atherosclerotic heart disease, cerebrovascular disease, peripheral vascular disease, chronic obstructive lung disease, cancer, alcohol dependence, drug dependence, and tobacco use. We were only able to obtain blood type information from patients placed on the kidney transplant waitlist. We also generated an indicator of low functional status if the MER indicated the presence of the inability to ambulate or transfer.
Statistical Analyses
We assessed differences in patient characteristics among Hispanics and non-Hispanics via a two-sample t test for continuous variables and a chi-squared test for independence for categorical variables.
We estimated unadjusted and adjusted cause-specific hazard ratios (HRCS) with 95% confidence intervals (95% CI) from time to event of interest analyses. The HRCS is interpreted as the relative hazard of waitlisting and transplantation in the presence of the competing events, (i.e., as observed in the population). The HRCS was estimated using Cox proportional hazards methods, censoring patients at the time of the competing event. To account for competing events, we also estimated subdistribution hazard ratios (HRSD). The HRSD can be interpreted as the relative hazard of waitlisting and transplantation if the competing events did not exist. Because the only censoring performed was administrative censoring, the HRSD was also estimated using a Cox proportional hazards method, censoring those who had experienced a competing event at the administrative censoring date of January 1, 2009 (Supplemental Appendix) (28).
We fit four models to estimate both the HRCS and HRSD: model 1 estimated unadjusted HRs; model 2 adjusted for continuous age, sex, and year at start of dialysis; model 3 additionally adjusted for all comorbidities, dialysis modality, insurance payer status, BMI, and patient blood type (blood type data were only available for patients on the transplant waitlist); and model 4 additionally stratified on assigned OPO. We tested for violation of proportional hazards by stratification and inspection of Schoenfeld residuals. Mainly due to the large sample size, we identified nominally significant effect modification by age. Because the age-stratified analyses showed similar results, we chose to present our analysis not stratified by age.
Ten percent of the data were missing for BMI and dialysis modality, in a nondifferential pattern between Hispanics and non-Hispanics. Subsequently, we performed a complete-case analysis.
Analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC) and R 2.14 (The R Project for Statistical Computing, Vienna, Austria) software.
This work was approved by the institutional review board of Stanford University School of Medicine and conducted under a data use agreement between W.C.W. and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). A NIDDK officer reviewed the manuscript for privacy content and approved it before submission.
Results
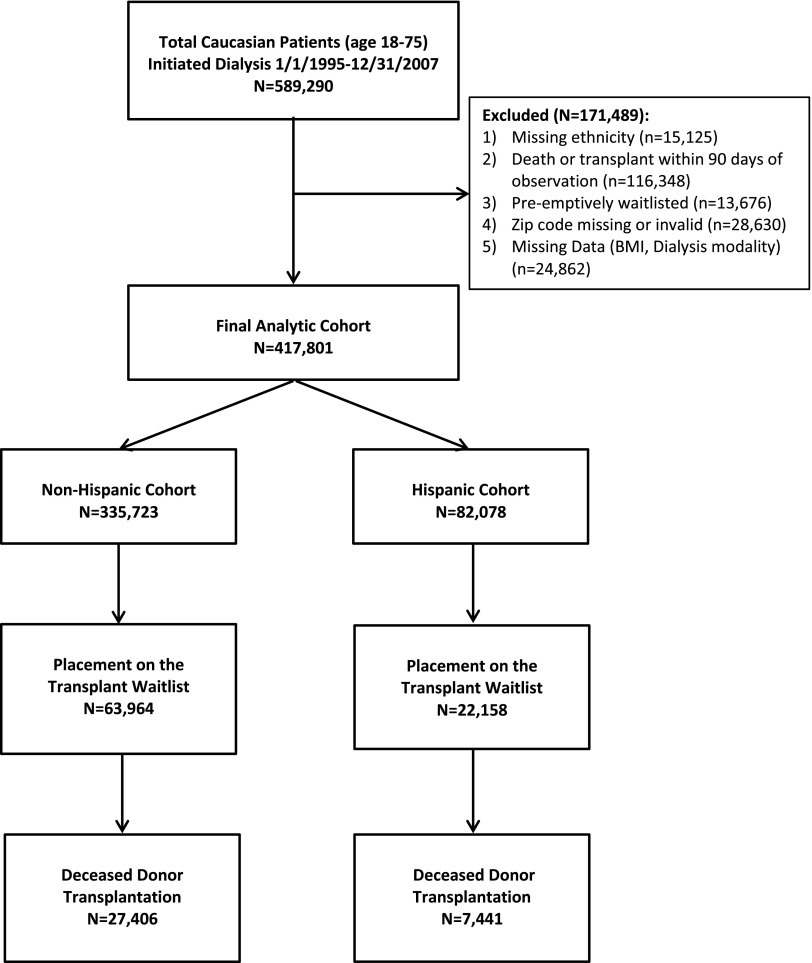
We identified 589,290 Caucasian patients aged between 18 and 75 years who initiated dialysis between January 1, 1995 and December 31, 2007 in the continental United States and Puerto Rico. We excluded patients who had missing ethnicity information, had died or received a transplant within 90 days of the first service date, had preemptive waitlisting, had a missing or invalid zip code, or had missing patient data (Figure 1). The final study cohort of 417,801 included 82,078 Hispanic patients (19.6%) and 335,723 non-Hispanic patients (80.4%). Hispanics were younger than non-Hispanics at the initiation of dialysis (56.2±13.0 versus 60.1±12.3; P<0.001) and were more likely to start dialysis treatment using hemodialysis (92.5% versus 88.8%; P<0.001; Table 1). Among the comorbidities, Hispanics had more reported diabetes and hypertension, whereas all other comorbidities were more prevalent among non-Hispanics. Regarding distribution of insurance payer status, Hispanics were less likely to have Medicare Parts A and B at the time of first dialysis (36.8% versus 51.9%; P<0.001), but were more likely to be listed under the Medicare 90-day waiting period (40.1% versus 26.3%; P<0.001). Among waitlisted patients, Hispanics were more likely to have blood type O (17.2% versus 9.5%; P<0.001). Supplemental Table 1 provides age-stratified comparisons of these characteristics.
Figure 1.
Cohort selection flow diagram. Note: Several of the exclusion criteria were not mutually exclusive. BMI, body mass index.
Table 1.
Characteristics of Hispanic and non-Hispanic whites initiating dialysis in the United States (1995–2007)
| Sociodemographic Variable | All Patients | Non-Hispanic Patients | Hispanic Patients | P Value |
|---|---|---|---|---|
| Participants | 417,801 (100) | 335,723 (80.4) | 82,078 (19.6) | |
| Age at incidence of ESRD (yr) | 59.3±12.5 | 60.1±12.3 | 56.2±13.0 | <0.001 |
| Age groups (yr) | <0.001 | |||
| 18–39 | 35,830 (8.6) | 26,030 (7.8) | 9800 (11.9) | |
| 40–59 | 140,748 (33.7) | 106,989 (31.9) | 33,759 (41.1) | |
| 60–75 | 241,223 (57.7) | 202,704 (60.4) | 38,519 (46.9) | |
| Male sex | 237,578 (56.9) | 191,687 (57.1) | 45,894 (55.9) | <0.001 |
| Dialysis modality | <0.001 | |||
| Hemodialysis | 374,149 (89.6) | 298,243 (88.8) | 75,906 (92.5) | |
| Peritoneal dialysis | 43,652 (10.4) | 37,480 (11.2) | 6172 (7.5) | |
| Missing | 454 (<0.1) | 407 (<0.1) | 47 (<0.1) | |
| Comorbidities | ||||
| Diabetes | 233,349 (55.9) | 179,740 (53.5) | 53,609 (65.3) | <0.001 |
| Hypertension | 325,639 (77.9) | 259,325 (77.2) | 66,314 (80.8) | <0.001 |
| Heart failure | 133,743 (32.0) | 111,097 (33.1) | 22,646 (27.6) | <0.001 |
| Atherosclerotic heart disease | 117,738 (28.2) | 102,055 (30.4) | 15,683 (19.1) | <0.001 |
| Cerebrovascular disease | 37,052 (8.9) | 31,760 (9.5) | 5292 (6.4) | <0.001 |
| Peripheral vascular disease | 69,109 (16.5) | 58,631 (17.5) | 10,478 (12.8) | <0.001 |
| Chronic obstructive lung disease | 37,274 (8.9) | 34,976 (10.4) | 2298 (2.8) | <0.001 |
| Cancer | 23,694 (5.7) | 21,827 (6.5) | 1867 (2.3) | <0.001 |
| Alcohol dependence | 5494 (1.3) | 4547 (1.4) | 947 (1.2) | 0.88 |
| Drug dependence | 2289 (0.5) | 1757 (0.5) | 532 (0.6) | <0.001 |
| Tobacco use | 28,837 (6.9) | 26,802 (8.0) | 2035 (2.5) | <0.001 |
| Unable to transfer or ambulate | 17,555 (4.2) | 14,757 (4.4) | 2798 (3.4) | <0.001 |
| Body mass index (kg/m2) | <0.001 | |||
| <18.5 | 20,229 (4.8) | 16,682 (5.0) | 3547 (4.3) | |
| 18.5–24.9 | 140,265 (33.6) | 111,330 (33.2) | 28,935 (35.3) | |
| 25.0–29.9 | 121,076 (29.0) | 94,857 (28.3) | 26,219 (31.9) | |
| 30.0–39.9 | 106,777 (25.6) | 87,629 (26.1) | 19,148 (23.3) | |
| ≥40.0 | 29,454 (7.0) | 25,225 (7.5) | 4229 (5.2) | |
| Missing | 24,408 (5.5) | 19,871 (5.6) | 4537 (5.2) | |
| Blood typea | <0.001 | |||
| O | 46,120 (11.0) | 32,000 (9.5) | 14,120 (17.2) | |
| A | 36,575 (8.8) | 29,339 (8.7) | 7236 (8.8) | |
| B | 9955 (2.4) | 7571 (2.3) | 2384 (2.9) | |
| AB | 3328 (0.8) | 2769 (0.8) | 559 (0.7) | |
| Payer of health care | <0.001 | |||
| Medicare primary, Part A and B | 204,392 (48.9) | 174,175 (51.9) | 30,217 (36.8) | |
| Medicare primary, other | 9477 (2.3) | 6642 (2.0) | 2835 (3.5) | |
| Medicare secondary with EGHP | 26,513 (6.3) | 23,806 (7.1) | 2707 (3.3) | |
| Medicare secondary, no EGHP | 2963 (0.7) | 2681 (0.8) | 282 (0.3) | |
| Medicare 90-day waiting period | 121,029 (29.0) | 88,142 (26.3) | 32,887 (40.1) | |
| Health maintenance organization | 28,582 (6.8) | 22,366 (6.7) | 6216 (7.6) | |
| Other/unknown | 24,849 (5.9) | 17,915 (5.3) | 6934 (8.4) |
Data are presented as n (%) or mean ± SD. EGHP, employer group health plan.
Blood type information was only available among patients on the waitlist (n=86,122).
A total of 250,889 patients (60.0%) died during 1,327,038 person-years of follow-up. Death occurred in 48.7% of Hispanic and in 62.8% of non-Hispanic patients. A total of 21,512 (5.1%) patients received a living kidney transplant, including 5.1% of Hispanic patients and 5.2% of non-Hispanic patients. A total of 39,016 patients (9.3%) were lost to follow-up, including 15.1% of Hispanic patients and 7.9% of non-Hispanic patients (Supplemental Figure 1 and Supplemental Table 2).
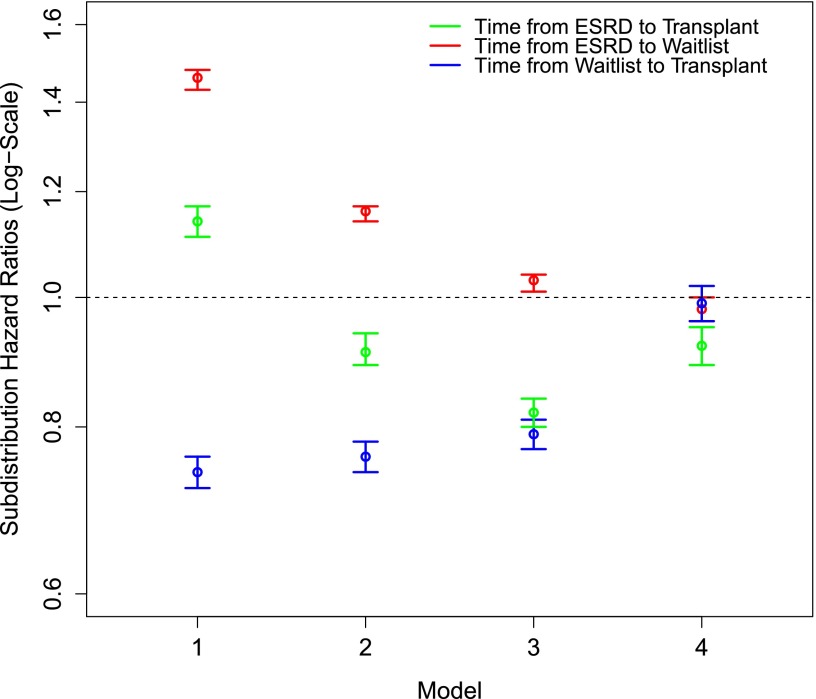
Analyses of Time to Deceased Donor Transplantation
In the unadjusted model, the time from ESRD to kidney transplantation from a deceased donor was significantly shorter for non-Hispanics (HRCS, 0.87; 95% CI, 0.85 to 0.90; Table 2). After taking into account that Hispanics were younger (model 2) and relatively healthier (model 3) at time of ESRD, the disparity increased (HRCS, 0.68; 95% CI, 0.66 to 0.69; Figure 2). We found that Hispanics were less likely to receive a living donor kidney transplant and less likely to die, though more likely to be lost to follow-up (Supplemental Table 2). On the basis of the differential rates of competing events (especially death) among Hispanics compared with non-Hispanic whites, the HRSD of 0.82 showed a 44% attenuation in the relative rate of transplantation (95% CI, 0.80 to 0.84). Moreover, once we accounted for geographic variability by stratifying on OPO (model 4), the difference in transplantation rates was further attenuated by an additional 56% (HRSD, 0.92; 95% CI, 0.89 to 0.95).
Table 2.
Relative rates of transplant waitlisting and decreased kidney transplantation in Hispanic compared with non-Hispanic whites
| Time Period | Model 1 | Model 2 | Model 3 | Model 4 | ||||
|---|---|---|---|---|---|---|---|---|
| HRCS | HRSD | HRCS | HRSD | HRCS | HRSD | HRCS | HRSD | |
| ESRD to transplant (n =417,801) | 0.87 (0.85 to 0.90) | 1.14 (1.11 to 1.17) | 0.73 (0.71 to 0.75) | 0.91 (0.89 to 0.94) | 0.68 (0.66 to 0.69) | 0.82 (0.80 to 0.84) | 0.77 (0.75 to 0.80) | 0.92 (0.89 to 0.95) |
| ESRD to waitlisting (n=417,801) | 1.31 (1.29 to 1.33) | 1.46 (1.43 to 1.48) | 1.06 (1.04 to 1.08) | 1.16 (1.14 to 1.17) | 0.96 (0.94 to 0.97) | 1.03 (1.01 to 1.04) | 0.92 (0.90 to 0.94) | 0.98 (0.96 to 1.00) |
| Waitlisting to transplant (n=86,122)a | 0.62 (0.60 to 0.63) | 0.74 (0.72 to 0.76) | 0.63 (0.62 to 0.65) | 0.76 (0.74 to 0.78) | 0.66 (0.64 to 0.68) | 0.79 (0.77 to 0.81) | 0.86 (0.84 to 0.89) | 0.99 (0.96 to 1.02) |
Data are presented as hazard ratios (95% confidence interval). Model 1 is unadjusted; model 2 is adjusted for age, sex, and year of dialysis initiation; model 3 is further adjusted for all comorbidities, dialysis modality, payer status, body mass index, and blood type; and model 4 is further adjusted for organ procurement organization. HRCS, cause-specific hazard ratio; HRSD, subdistribution hazard ratio.
Blood type was only available among patients on the transplant waitlist and was therefore incorporated in the model analyzing time from waitlist placement to receipt of a transplant.
Figure 2.
Subdistribution hazard ratios for time from ESRD to transplant from a deceased donor, ESRD to transplant waitlisting, and transplant waitlisting to kidney transplantation from a deceased donor in Hispanics compared with non-Hispanic whites. Model 1 is unadjusted; model 2 is adjusted for age, sex, and year of dialysis initiation; model 3 is further adjusted for all comorbidities, dialysis modality, insurance payer status, and body mass index; and model 4 is further stratified for organ procurement organization.
Analyses of Time to Waitlist and Time from Waitlist to Deceased Donor Transplantation
To further characterize the transition from dialysis initiation to kidney transplantation, we defined waitlisting as an intermediary event and separately analyzed the time from dialysis initiation to waitlisting and time from waitlisting to transplantation. Once accounting for competing events and adjusting for patient demographics, comorbidities, and OPO, there was minimal difference in the time to waitlisting between Hispanics and non-Hispanics (HRSD, 0.98; 95% CI, 0.96 to 1.00; Table 2). Moreover, once placed on the transplant waitlist and further adjusted for patient blood type, no statistical difference in time to transplantation existed between Hispanics and non-Hispanics (HRSD, 0.99; 95% CI, 0.96 to 1.02). Of note, the sample size of the cohort observed at time from waitlisting to transplantation was smaller (n=86,122) because only waitlisted transplant patients were included.
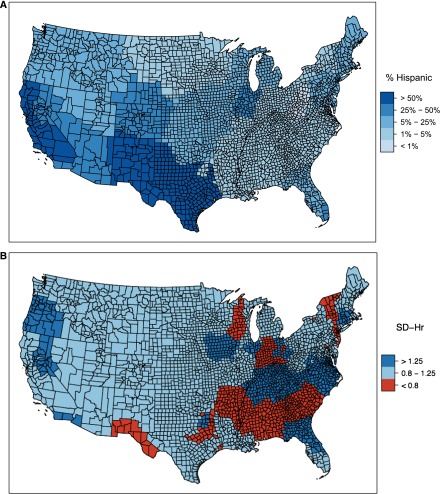
Regional Variability
We formally tested whether inclusion of OPO into the regression model significantly improved model fit. A likelihood ratio test was highly significant (P<0.001). We then explored regional variability in relative time to deceased donor kidney transplantation between Hispanics and non-Hispanics. Figure 3A illustrates the geographic distribution of Hispanics as a proportion among white ESRD patients by OPO. After adjusting for sociodemographic data, patient comorbidities, and competing risks, Figure 3B illustrates the geographic variability of HRSD stratified by OPO for Hispanics versus non-Hispanic whites within each US county for time from dialysis initiation to deceased donor kidney transplantation. Effect modification was present between Hispanic ethnicity and OPO (P=0.01). We performed a sensitivity analysis by restricting the analysis to OPOs consisting of at least 2% Hispanics, and excluded small OPOs containing less than a total of 100 Hispanic or non-Hispanic patients. We also restricted our analysis to patients in the continental United States and performed the analyses stratified on different age groups (Supplemental Table 3). Results from all sensitivity analyses were comparable with the main analyses.
Figure 3.
Geographic variation in ESRD incidence and access to deceased donor kidney transplantation among Hispanics. (A) Percentage of Hispanics among all incident white ESRD patients, by US county. (B) Subdistribution hazard ratio of kidney transplantation between Hispanic and non-Hispanic whites, by organ procurement organization. Note: Subdistribution hazard ratios (SD-hr) are the time from ESRD to kidney transplantation.
Discussion
Overall, we found that Hispanics with ESRD were less likely to receive a deceased donor kidney transplant compared with non-Hispanic whites. However, when examining the distinct steps to transplantation, Hispanics were as likely to be placed on the transplant waitlist, but experienced a lower likelihood of undergoing deceased donor kidney transplantation. Interestingly, after stratifying for geographic residence (i.e., residence within the catchment area of a specific OPO) and accounting for blood type and competing events, the disparity in deceased donor kidney transplantation was reduced substantially; this is informative and indicates that the rapidly growing Hispanic population tends to concentrate in highly populated OPOs with limited organ availability.
By using a competing risks framework, we were able to elucidate different components of the Hispanics’ differential access to kidney transplantation. As observed in regular clinical practice (HRCS), Hispanics are transplanted at a lower rate compared with non-Hispanics even after accounting for demographics, comorbidities, and geography. However, when considering death as a competing event (HRSD), the observed Hispanic survival suggests that sicker, non-Hispanic patients may be more likely to die, enriching the non-Hispanic cohort with more transplant-eligible patients. In addition, because blood type differs between Hispanic and non-Hispanic individuals and is a determinant of receipt of a deceased donor kidney transplant, its absence in the ESRD to transplant analyses best explains the slightly reduced rate of transplant among Hispanics, which was not observed when examining the two distinct steps to deceased donor transplantation separately. Overall, once differences in blood type, geographic location, and competing risks were taken into account, the transplant disparity among Hispanics reduced substantially and can be explained by these factors: (1) the tendency for Hispanics to reside in OPOs with longer waiting times; (2) the Hispanic survival advantage, which is also well documented in the literature (29–31); and (3) the higher likelihood of blood type O in the Hispanic population.
Few reports have described the reduced access to kidney transplantation among the Hispanic ESRD population. In 2004, a small study (N=1335) performed by Sequist et al. found that Hispanics living in Arizona and New Mexico were less likely than whites to be placed on the transplant waitlist (relative risk [RR], 0.68; 95% CI, 0.50 to 0.88) and receive a transplant (RR, 0.58; 95% CI, 0.39 to 0.86) (14). In a more recent study analyzing the determinants of deceased donor kidney transplantation across several US racial and ethnic groups using a comprehensive national registry, Hispanics were found to be less likely to be placed on the transplant waitlist and the overall likelihood of deceased donor transplantation was lower (HR, 0.72; 95% CI, 0.70 to 0.74) compared with the Caucasian population (11). Similar to our analysis, Hall et al. found that geographic variation as well as linguistic isolation played an important role in possibly explaining the disparity in kidney transplantation among Hispanics as well as other minority groups (11). Lastly, in a single-center study analyzing time from dialysis initiation to placement on the waitlist, Hispanics (N=452) were found to experience significantly longer waiting time compared with non-Hispanic whites (27).
In 1998, in an effort to address the geographic boundaries in organ allocation, the Department of Health and Human Services issued the Final Rule to the Organ Procurement and Transplantation Network (OPTN) and UNOS requiring the implementation of new deceased donor organ allocation policies to distribute organs over as wide of a geographic area as possible on the basis of medical necessity (32). Realization of a national allocation system could not be achieved primarily due to concerns of increased transportation costs of organ procurement and prolonging cold ischemia time raising the probability of organ nonfunction after transplantation (33).
Geographic variability in access to the kidney transplant waiting list and deceased donor transplantation has been well described in a few studies (22,34). In the 2010 OPTN annual data report, the median waiting times for deceased donor kidney transplant varied widely, ranging from <2 years to nearly 7 years (26). To better understand the national demand for kidney transplantation, Mathur et al. measured the ESRD incidence across the United States and, not surprisingly, found that kidney transplant rates were lower in high ESRD incidence areas (RR, 0.63; 95% CI, 0.61 to 0.65) (23). Interestingly, the waitlist rates were not affected in the comparison of high to low ESRD incidence regions (RR, 1.02; 95% CI, 1.00 to 1.04), which may be explained by supersaturation in a high ESRD incidence region and by the practice patterns of local providers. For example, in OPOs with longer median waiting times, transplant providers may be more inclined to place their patients on the waitlist earlier to accrue waiting time.
According to the 2010 US Census Data, the geographic distribution of Hispanics is primarily concentrated in the West (41%) and the South (36%), which exceeds the national level of 16% (35). Figure 3A illustrates the geographic distribution of Hispanics among all whites with ESRD in the United States, which parallels the national census data. Interestingly, after accounting for competing risks and adjusting for sociodemographic data, patient comorbidities, and designated OPO, we found that Hispanics were actually as likely and, at times, more likely to receive a kidney transplant compared with non-Hispanic whites in regions of the country heavily populated by Hispanics, with the exception of Texas, Arkansas, and New Mexico (Figure 3B). To address linguistic and cultural barriers in regions of the country composed of a large Hispanic community, medical centers may be better equipped with more efficient interpretation services and may distribute culturally appropriate educational materials to increase CKD and transplantation awareness. Among first-generation immigrants, approximately 53% of all foreign-born residents in 2010 were from Central and South America—of those, Hispanics of Mexican origin were least likely to undergo US naturalization (36). Therefore, states more heavily populated by Hispanics of Mexican origin (including Texas, New Mexico, Arizona, and Arkansas) are probably more likely to experience limited financial and social support, resulting in kidney transplantation disparities.
Our study’s strengths included the analysis of large, national cohort of ESRD patients with comprehensive, long-term follow-up for transplantation and death in the Hispanic population. However, our study does have several limitations. First, the Hispanic population is a heterogeneous population with subgroups that differ culturally and genetically resulting in variable mortality and morbidity outcomes. Second, we were unable to ascertain health status at the time of waitlisting, dynamic changes in comorbid risk factors, and reasons for transplant waitlist removal. Third, accuracy of ethnicity reporting on the MER has not been validated. In addition, a recent study demonstrated some shortcomings in the reporting of patient comorbidities that likely resulted in nondifferential misclassification (37). Forth, in order to maintain a consistent study population and avoid race-related confounding, we chose to exclude patients with reported race other than white (constituting <6% of initial Hispanic cohort) as well as patients who received a preemptive deceased donor transplant. Fifth, although both cohorts experienced <16% loss to follow-up, differential loss to follow-up was observed. Sixth, we were unable to obtain reliable panel reactive antibody levels at the time of waitlisting, limiting the inclusion of this potential confounder. Seventh, information on blood type was only available for waitlisted patients. Eighth, we were unable to reliably identify “waitlist inactivity” for patients on the transplant waitlist. Finally, we did not assess socioeconomic status and linguistic isolation, which could also affect access to transplantation.
In summary, the observed disparity in deceased donor transplantation among Hispanics is largely explained by regional variability of organ supply among various OPOs across the country. Given the increased prevalence and incidence of ESRD among Hispanics and geographic disparities in access to transplantation, health policy reforms focusing on methods to increase the effective organ supply to areas with endemic ESRD could have a tremendous effect on improving organ equity without necessarily diminishing the utility of the donated organ. Our findings highlight the tremendous need for organ allocation policy reforms to overcome the geographic disparities that Hispanics encounter in the path to deceased donor kidney transplantation.
Disclosures
W.C.W. reports having served as a scientific advisor or consultant to Affymax, Amgen, Bayer, Fibrogen, and GlaxoSmithKline.
Supplementary Material
Acknowledgments
The data reported herein were supplied by the USRDS. Interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as official policy or interpretation of the US government.
C.M.A. was supported by an underrepresented minority supplement to Grant T32 DK007357-26 from the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.01560213/-/DCSupplemental.
References
- 1.Evans RW, Manninen DL, Garrison LP, Jr, Hart LG, Blagg CR, Gutman RA, Hull AR, Lowrie EG: The quality of life of patients with end-stage renal disease. N Engl J Med 312: 553–559, 1985 [DOI] [PubMed] [Google Scholar]
- 2.Port FK, Wolfe RA, Mauger EA, Berling DP, Jiang K: Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant recipients. JAMA 270: 1339–1343, 1993 [PubMed] [Google Scholar]
- 3.Stange PV, Sumner AT: Predicting treatment costs and life expectancy for end-stage renal disease. N Engl J Med 298: 372–378, 1978 [DOI] [PubMed] [Google Scholar]
- 4.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, Port FK: Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 341: 1725–1730, 1999 [DOI] [PubMed] [Google Scholar]
- 5.US Renal Data System : USRDS 2011 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2011 [Google Scholar]
- 6.Alexander GC, Sehgal AR: Barriers to cadaveric renal transplantation among blacks, women, and the poor. JAMA 280: 1148–1152, 1998 [DOI] [PubMed] [Google Scholar]
- 7.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM: The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med 341: 1661–1669, 1999 [DOI] [PubMed] [Google Scholar]
- 8.Epstein AM, Ayanian JZ, Keogh JH, Noonan SJ, Armistead N, Cleary PD, Weissman JS, David-Kasdan JA, Carlson D, Fuller J, Marsh D, Conti RM: Racial disparities in access to renal transplantation–clinically appropriate or due to underuse or overuse? N Engl J Med 343: 1537–1544, 2 p preceding 1537, 2000 [DOI] [PMC free article] [PubMed]
- 9.Patzer RE, Amaral S, Wasse H, Volkova N, Kleinbaum D, McClellan WM: Neighborhood poverty and racial disparities in kidney transplant waitlisting. J Am Soc Nephrol 20: 1333–1340, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez RA, Sen S, Mehta K, Moody-Ayers S, Bacchetti P, O’Hare AM: Geography matters: Relationships among urban residential segregation, dialysis facilities, and patient outcomes. Ann Intern Med 146: 493–501, 2007 [DOI] [PubMed] [Google Scholar]
- 11.Hall YN, Choi AI, Xu P, O’Hare AM, Chertow GM: Racial ethnic differences in rates and determinants of deceased donor kidney transplantation. J Am Soc Nephrol 22: 743–751, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall YN, O’Hare AM, Young BA, Boyko EJ, Chertow GM: Neighborhood poverty and kidney transplantation among US Asians and Pacific Islanders with end-stage renal disease. Am J Transplant 8: 2402–2409, 2008 [DOI] [PubMed] [Google Scholar]
- 13.Hall YN, Sugihara JG, Go AS, Chertow GM: Differential mortality and transplantation rates among Asians and Pacific Islanders with ESRD. J Am Soc Nephrol 16: 3711–3720, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Sequist TD, Narva AS, Stiles SK, Karp SK, Cass A, Ayanian JZ: Access to renal transplantation among American Indians and Hispanics. Am J Kidney Dis 44: 344–352, 2004 [DOI] [PubMed] [Google Scholar]
- 15.Gaston RS, Ayres I, Dooley LG, Diethelm AG: Racial equity in renal transplantation. The disparate impact of HLA-based allocation. JAMA 270: 1352–1356, 1993 [PubMed] [Google Scholar]
- 16.Roberts JP, Wolfe RA, Bragg-Gresham JL, Rush SH, Wynn JJ, Distant DA, Ashby VB, Held PJ, Port FK: Effect of changing the priority for HLA matching on the rates and outcomes of kidney transplantation in minority groups. N Engl J Med 350: 545–551, 2004 [DOI] [PubMed] [Google Scholar]
- 17.Axelrod DA, Dzebisashvili N, Schnitzler MA, Salvalaggio PR, Segev DL, Gentry SE, Tuttle-Newhall J, Lentine KL: The interplay of socioeconomic status, distance to center, and interdonor service area travel on kidney transplant access and outcomes. Clin J Am Soc Nephrol 5: 2276–2288, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hall EC, Massie AB, James NT, Garonzik Wang JM, Montgomery RA, Berger JC, Segev DL: Effect of eliminating priority points for HLA-B matching on racial disparities in kidney transplant rates. Am J Kidney Dis 58: 813–816, 2011 [DOI] [PubMed] [Google Scholar]
- 19.Hata Y, Cecka JM, Takemoto S, Ozawa M, Cho YW, Terasaki PI: Effects of changes in the criteria for nationally shared kidney transplants for HLA-matched patients. Transplantation 65: 208–212, 1998 [DOI] [PubMed] [Google Scholar]
- 20.Keith D, Ashby VB, Port FK, Leichtman AB: Insurance type and minority status associated with large disparities in prelisting dialysis among candidates for kidney transplantation. Clin J Am Soc Nephrol 3: 463–470, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schold JD, Harman JS, Chumbler NR, Duncan RP, Meier-Kriesche HU: The pivotal impact of center characteristics on survival of candidates listed for deceased donor kidney transplantation. Med Care 47: 146–153, 2009 [DOI] [PubMed] [Google Scholar]
- 22.Ashby VB, Kalbfleisch JD, Wolfe RA, Lin MJ, Port FK, Leichtman AB: Geographic variability in access to primary kidney transplantation in the United States, 1996-2005. Am J Transplant 7: 1412–1423, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Mathur AK, Ashby VB, Sands RL, Wolfe RA: Geographic variation in end-stage renal disease incidence and access to deceased donor kidney transplantation. Am J Transplant 10: 1069–1080, 2010 [DOI] [PubMed] [Google Scholar]
- 24.Humes KR, Jones NA, Ramirez RR: Overview of Race and Hispanic Origin: 2010, 2010 Census Briefs, Washington, DC, US Department of Commerce, Economics and Statistics Administration, US Census Bureau, 2011 [Google Scholar]
- 25.Peralta CA, Shlipak MG, Fan D, Ordoñez J, Lash JP, Chertow GM, Go AS: Risks for end-stage renal disease, cardiovascular events, and death in Hispanic versus non-Hispanic white adults with chronic kidney disease. J Am Soc Nephrol 17: 2892–2899, 2006 [DOI] [PubMed] [Google Scholar]
- 26.Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR): OPTN/SRTR 2011 Annual Data Report, Rockville, MD, Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation, 2012 [Google Scholar]
- 27.Joshi S, Gaynor JJ, Bayers S, Guerra G, Eldefrawy A, Chediak Z, Companioni L, Sageshima J, Chen L, Kupin W, Roth D, Mattiazzi A, Burke GW, 3rd, Ciancio G: Disparities among blacks, Hispanics, and whites in time from starting dialysis to kidney transplant waitlisting. Transplantation 95: 309–318, 2013 [DOI] [PubMed] [Google Scholar]
- 28.Bakoyannis G, Touloumi G: Practical methods for competing risks data: A review. Stat Methods Med Res 21: 257–272, 2012 [DOI] [PubMed] [Google Scholar]
- 29.Arce CM, Goldstein BA, Mitani AA, Winkelmayer WC: Trends in relative mortality between Hispanic and non-Hispanic whites initiating dialysis: A retrospective study of the US Renal Data System. Am J Kidney Dis 62: 312–321, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murthy BV, Molony DA, Stack AG: Survival advantage of Hispanic patients initiating dialysis in the United States is modified by race. J Am Soc Nephrol 16: 782–790, 2005 [DOI] [PubMed] [Google Scholar]
- 31.Yan G, Norris KC, Yu AJ, Ma JZ, Greene T, Yu W, Cheung AK: The relationship of age, race, and ethnicity with survival in dialysis patients. Clin J Am Soc Nephrol 8: 953–961, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Medicare & Medicaid Services (CMS), HHS : Medicare program; hospital conditions of participation: Requirements for approval and re-approval of transplant centers to perform organ transplants. Final rule. Fed Regist 72: 15197–15280, 2007 [PubMed] [Google Scholar]
- 33.Van Meter CH: The organ allocation controversy: How did we arrive here? Ochsner J 1: 6–11, 1999 [PMC free article] [PubMed] [Google Scholar]
- 34.Ellison MD, Edwards LB, Edwards EB, Barker CF: Geographic differences in access to transplantation in the United States. Transplantation 76: 1389–1394, 2003 [DOI] [PubMed] [Google Scholar]
- 35.Ennis SR, Rios-Vargas M, Albert NG: The Hispanic Population: 2010, 2010 Census Briefs, Washington, DC, US Department of Commerce, Economics and Statistics Administration, US Census Bureau, 2011 [Google Scholar]
- 36.Acosta YD, de la Cruz GP: The Foreign Born from Latin America and the Caribbean: 2010, American Community Survey Briefs, Washington, DC, US Department of Commerce, Economics and Statistics Administration, US Census Bureau, 2011 [Google Scholar]
- 37.Kim JP, Desai M, Chertow GM, Winkelmayer WC: Validation of reported predialysis nephrology care of older patients initiating dialysis. J Am Soc Nephrol 23: 1078–1085, 2012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.