Abstract
Background
Acinetobacter baumannii, an opportunistic nosocomial pathogen that can cause significant morbidity and mortality, has emerged as a worldwide problem. The aim of this study was to evaluate the risk factors for mortality in patients with A. baumannii bacteremia.
Materials and Methods
We retrospectively evaluated 118 patients who had A. baumannii bacteremia between July 2003 and December 2011. The aim of this study was to identify the 30-day mortality in patients with A. baumannii bacteremia and relevant risk factors.
Results
The bacteremia-related 30-day mortality rate was 34.1%. Univariate analysis revealed that the risk factors for mortality included malignancy, longer hospital stay before bacteremia, intensive care unit (ICU) stay at the time of bacteremia, mechanical ventilation, use of a central venous catheter, unknown origin of bacteremia, bacteremia due to pneumonia, antimicrobial resistance to carbapenems, and elevated Acute Physiology and Chronic Health Evaluation II and Pitt bacteremia scores. Multivariate logistic regression analysis revealed that resistance to carbapenems (odds ratio [OR]: 4.01, 95% confidence interval [CI]: 1.51 to 0.68, P = 0.005), need for mechanical ventilation (OR: 3.97, 95% CI: 1.41 to 11.13, P = 0.005), and presence of malignancy (OR: 4.40, 95% CI: 1.60 to 12.08, P = 0.004) were significantly related to mortality risk.
Conclusions
Risk factors such as resistance to carbapenems, mechanical ventilation, and presence of malignancy were found to be associated with high mortality rates in the patients with A. baumannii bacteremia.
Keywords: Acinetobacter baumannii, Bacteremia, Mortality
Introduction
Acinetobacter species are nonfermenting aerobic gram-negative bacteria that have become important nosocomial pathogens. According to Korean Nosocomial Infections Surveillance System (KONIS) data, Acinetobacter baumannii accounts for 32% (450/1,405) of nosocomial gram-negative bacilli infections, and the pathogen is particularly common in intensive care unit (ICU) cases [1]. Previously, this organism was considered to have low virulence, generally more capable of colonizing than infecting. However, it has emerged as an invasive and life-threatening pathogen, especially in critically ill patients [2-5]. A. baumannii infection is now a common worldwide problem that can lead to increased morbidity and prolonged hospital stays.
Carbapenems are usually the antimicrobial agents of choice for the treatment of serious A. baumannii infection. However, carbapenem-resistant A. baumannii (CRAB) isolates have been reported with increasing frequency worldwide in recent years. KONIS data show that imipenem-resistant strains of A. baumannii infection represented 86.9% of infections with the pathogen during 2010 and 2011 in university hospitals throughout the Republic of Korea (ROK) [1]. Generally, patients with CRAB infection have higher mortality rates, longer duration of hospitalization, and higher healthcare costs than those infected with carbapenem-susceptible A. baumannii (CSAB) [6-9].
Despite the increasing prevalence of A. baumannii bacteremia and the degree to which it has become a clinically significant concern, there are limited data on A. baumannii bacteremia in the ROK. Therefore, the aim of this study was to evaluate the clinical features and outcomes of patients with A. baumannii bacteremia in the ROK to help identify risk factors for A. baumannii infection-related mortality.
Materials and Methods
1. Study population
We performed an observational retrospective study. We reviewed the medical records, including clinical, microbiological, and laboratory data, and analyzed the outcomes and characteristics of all patients with A. baumannii bacteremia at a 750-bed tertiary medical center in the ROK (between July 2003 and December 2011). The demographic characteristics, clinical care information, microbiological data, treatments provided, and outcomes of 118 patients with 123 episodes of clinically significant A. baumannii bacteremia were reviewed.
The following data were collected: age, sex, underlying diseases, duration of hospital stay before bacteremia, ICU stay at the time of bacteremia, invasive procedures, antimicrobial susceptibility of A. baumannii, severity of illness (as determined by Acute Physiology and Chronic Health Evaluation II [APACHE II] and Pitt scores) at the time of bacteremia, and the initial empirical antibiotic agents administered.
2. Identification and antimicrobial susceptibility testing
Blood specimens were cultured using the BACTEC blood culture system (Becton Dickinson, Sparks, MD, USA). Identification and antimicrobial susceptibility tests for Acinetobacter were performed with the Microscan Walk Away-96 plus system (Siemens, Deerfield, IL, USA). The susceptibility results were interpreted according to the guidelines of the Clinical and Laboratory Standards Institute [10]. Isolates with intermediate susceptibility or resistance to the antibiotics were considered to be resistant.
3. Definitions
Significant bacteremia was defined as the isolation of A. baumannii from one or more blood culture specimens, and the presence of clinical features consistent with infection (e.g., fever or leukocytosis). If more than 14 days had passed without a positive blood culture result, the subsequent isolation of A. baumannii from blood was deemed to be a separate episode. Nosocomial bacteremia was defined as the isolation of one or more A. baumannii isolates from blood cultures after 48 hours of admission [11]. CRAB was defined as in vitro resistance to imipenem and/or meropenem. Appropriate antibiotic therapy was defined as the use of drugs with in vitro activity at therapeutic dosages (as determined using the results of sensitivity tests within 3 days of the bacteremic episode) that were delivered by an approved route and for an approved duration. When antimicrobial therapy did not meet these conditions, it was considered to be inappropriate.
4. Statistical analysis
Continuous variables are expressed as mean (SD) and were compared using the Student's t-test or Mann-Whitney U-test. Categorical variables were compared with the Chi-square test or Fisher's exact test when the expected values were below 5. Predictors for 30-day mortality were identified using logistic regression. All clinical and laboratory parameters were a priori tested. Parameters with P < 0.1 and those with potentially important biological meaning were analyzed in a multivariate logistic regression model. All P-values were 2-tailed, and P < 0.05 was considered to be statistically significant. SPSS for Windows (Version 14.0, SPSS Inc., Chicago, IL, USA) was used for these analyses.
Results
1. Demographic and clinical characteristics
A total of 123 episodes in 118 patients with significant bacteremia between July 2003 and December 2011 were identified in this study. All the 123 cases were reviewed;114 (92.7%) were cases of nosocomial infection. The mean age for all the patients was 62.54 (15.80) years, and 53% (63/118) patients were male. Of the 118 patients, 86.2% had underlying comorbidities. The most common underlying disease was malignancy, which was present in 35.8% (44/123) of the patients. Central venous catheterization was the most common invasive procedure (49.6%; 61/123) performed during hospitalization. The proportion of patients who were confined in the ICU at the time of identifying their bacteremia was 49.6%, and the mean duration of hospital stay before bacteremia was 38.02 (62.46) days. Twenty-eight bacteremia cases (22.8%) were of unknown origin. CRAB bacteremia accounted for 42.3% of the cases. Only 42 of the 123 patients received appropriate antibiotic therapy. The disease-related characteristics of the patients with A. baumannii bacteremia are shown in Table 1.
Table 1.
Comparisons of the demographic and clinical characteristics according to survival state at 30 days in patients with Acinetobacter baumannii bacteremia
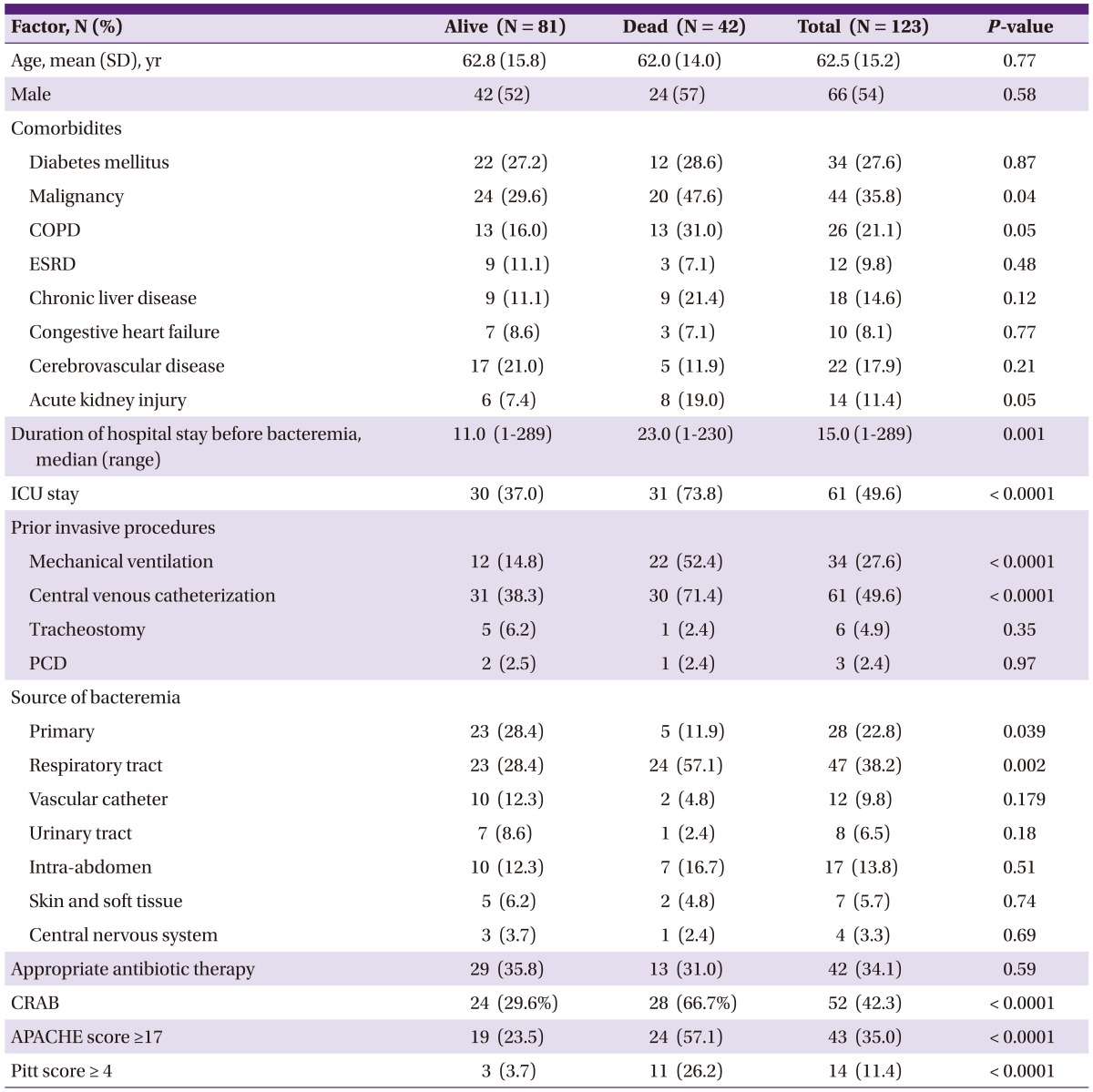
COPD, chronic obstructive pulmonary disease; ESRD, end stage renal disease; ICU, intensive care unit; PCD, percutaneous catheter drainage; CRAB, carbapenem-resistant A. baumannii; APACHE, acute physiology and chronic health evaluation.
2. Clinical outcomes and risk factors for mortality
The mortality rate 30 days after the onset of A. baumannii bacteremia was 34.1%. The results of the univariate analysis of bacteremia-related 30-day mortality in the patients with A. baumannii bacteremia are shown in Table 1. The multivariate analysis showed that the independent risk factors for bacteremia-related 30-day mortality were carbapenem resistance (odds ratio [OR]: 4.01, 95% confidence interval [CI]: 1.51 to 10.68, P = 0.005), mechanical ventilation (OR: 3.97, 95% CI: 1.41 to 11.13, P = 0.009), and presence of malignancy (OR: 4.22, 95% CI: 1.60 to 12.08, P = 0.004; Table 2).
Table 2.
Multivariate logistic regression analysis for predictors of mortality
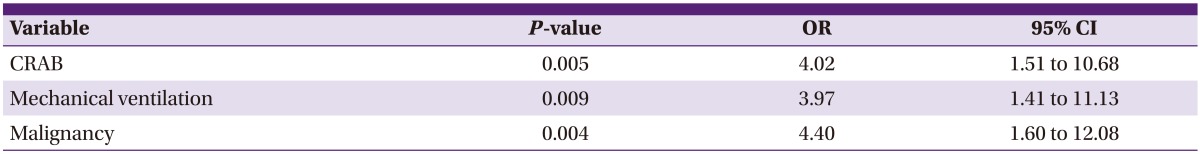
CRAB, carbapenem-resistant A. baumannii; OR, odds ratio; CI, confidence interval.
Discussion
A. baumannii has become a problematic nosocomial pathogen, partly due to clonal spread, particularly in ICUs [2, 4-7]. In this study, only 9 cases (7.3%) were community acquired while 114 were nosocomial, of which 49.6% occurred in the ICU. A. baumannii is the most common nosocomial pathogen among gram-negative bacilli and is characterized by marked antimicrobial resistance in the ROK. According to the KONIS data, A. baumannii represented 17.7% (95/537) of clinical specimens from patients with nosocomial gram-negative bacilli infections in 2006. The percentage of such infections caused by A. baumannii increased over the subsequent 5 years to 27.1% (389/1435) in 2010-2011. The percentage of imipenem-resistant A. Baumannii isolates has increased dramatically from 43.6% (41/94) in 2006 to 84.8% (313/369) in 2010-2011 [1].
A. baumannii can cause outbreaks of nosocomial infections such as bloodstream infection, ventilator-associated pneumonia, urinary tract infection, and wound infection [12]. The sources of bacteremia have been found to be, in decreasing order of frequency, the respiratory tract, vascular catheters, the intra-abdominal region, the urinary tract, soft tissues, and wounds [8, 13, 14]. Pneumonia and vascular access infections were the most common sources of bacteremia in this study, together accounting for nearly 50% of the cases; this result is similar to the results of previous studies [8, 14]. When pneumonia was the source of bacteremia, 64.2% (18/28) of the cases occurred in the ICU. In comparison, when vascular catheter-related infections were the source of bacteremia, 63.6% (7/11) of the patients were infected in the community or a general ward. This difference was not statistically significant.
A. baumannii bacteremia is associated with a high mortality rate, ranging from 29% to 46.9% [2, 13-15]. A diverse spectrum of comorbidities has been investigated as potential risk factors for mortality in these patients, such as previous severity of organ failure, neutropenia, elevated APACHE II score, malignancy, inappropriate antimicrobial treatment, pneumonia as the source of bacteremia, and septic shock [10, 13-16]. Our research showed that the major portal of entry was respiratory infection, and higher 30-day mortality rates were recorded in the patients with nosocomial pneumonia (28.4% vs 57.1%). Although no association between route of infection and mortality was observed in the multivariate analysis, our results showed a significantly higher mortality rate in those who received mechanical ventilation and those with underlying malignancy.
The most serious issue in the treatment of A. baumannii infection is multidrug resistance (MDR) because the number of appropriately active agents is limited. Several studies have reported that antibiotic resistance has an adverse impact on mortality rate, duration of hospitalization, and healthcare costs in patients with A. baumannii bacteremia. One matched-control study showed that mortality rate increased from 13% to 34% in A. baumannii bacteremia when the pathogen possessed MDR and that duration of hospitalization and healthcare costs were additionally increased [12]. Moreover, according to a multicenter study conducted in Taiwan, the acquisition of carbapenem resistance led to higher mortality rates and increased durations of hospital stay [9]. In contrast, however, one study has reported that mortality did not differ between patients with CRAB and CSAB bacteremia. However, in that study, patients with CRAB bacteremia had less severe illness on admission than those with CSAB [15]. Our results showed that carbapenem resistance was present in 42.3% (52/123) of cases, and resistance was identified as a significant independent risk factor for mortality in the multivariate analysis.
Some limitations were inherent in the present study. Although cases were consecutively enrolled according to an accurate laboratory database minimizing selection bias, clinical information regarding risk factors was collected retrospectively. Therefore, our results can not be generalized to other populations of patients. However, the study was strengthened by the inclusion of a large number of patients with a range of comorbidities and by its well-defined 30-day mortality end point.
In conclusion, A. baumannii bacteremia mostly develops as a nosocomial infection and is associated with a high mortality rate. Underlying malignancy, the need for mechanical ventilation, and infection with carbapenem-resistant strains were risk factors associated with a higher mortality rate in the patients with A. baumannii bacteremia.
References
- 1.Jeon MH, Park WB, Kim SR, Chun HK, Han SH, Bang JH, Park ES, Jeong SY, Eom JS, Kim YK, Kim HB, Lee KY, Choi HJ, Kim HY, Kim KM, Sung JH, Uh Y, Chung HS, Kwon JW, Woo JH. Korean nosocomial infections surveillance system, intensive care unit module report: data summary from July 2010 through June 2011. Korean J Nosocomial Infect Control. 2012;17:28–39. [Google Scholar]
- 2.Blot S, Vandewoude K, Colardyn F. Nosocomial bacteremia involving Acinetobacter baumannii in critically ill patients: a matched cohort study. Intensive Care Med. 2003;29:471–475. doi: 10.1007/s00134-003-1648-8. [DOI] [PubMed] [Google Scholar]
- 3.Maragakis LL, Perl TM. Acinetobacter baumannii: epidemiology, antimicrobial resistance, and treatment options. Clin Infect Dis. 2008;46:1254–1263. doi: 10.1086/529198. [DOI] [PubMed] [Google Scholar]
- 4.Tseng YC, Wang JT, Wu FL, Chen YC, Chie WC, Chang SC. Prognosis of adult patients with bacteremia caused by extensively resistant Acinetobacter baumannii. Diagn Microbiol Infect Dis. 2007;59:181–190. doi: 10.1016/j.diagmicrobio.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Kim SY, Jung JY, Kang YA, Lim JE, Kim EY, Lee SK, Park SC, Chung KS, Park BH, Kim YS, Kim SK, Chang J, Park MS. Risk factors for occurrence and 30-day mortality for carbapenem-resistant Acinetobacter baumannii bacteremia in an intensive care unit. J Korean Med Sci. 2012;27:939–947. doi: 10.3346/jkms.2012.27.8.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cisneros JM, Reyes MJ, Pachón J, Becerril B, Caballero FJ, García-Garmendía JL, Ortiz C, Cobacho AR. Bacteremia due to Acinetobacter baumannii: epidemiology, clinical findings, and prognostic features. Clin Infect Dis. 1996;22:1026–1032. doi: 10.1093/clinids/22.6.1026. [DOI] [PubMed] [Google Scholar]
- 7.Wareham DW, Bean DC, Khanna P, Hennessy EM, Krahe D, Ely A, Millar M. Bloodstream infection due to Acinetobacter spp: epidemiology, risk factors and impact of multi-drug resistance. Eur J Clin Microbiol Infect Dis. 2008;27:607–612. doi: 10.1007/s10096-008-0473-y. [DOI] [PubMed] [Google Scholar]
- 8.Kim YJ, Kim SI, Hong KW, Kim YR, Park YJ, Kang MW. Risk factors for mortality in patients with carbapenem-resistant Acinetobacter baumannii bacteremia: impact of appropriate antimicrobial therapy. J Korean Med Sci. 2012;27:471–475. doi: 10.3346/jkms.2012.27.5.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheng WH, Liao CH, Lauderdale TL, Ko WC, Chen YS, Liu JW, Lau YJ, Wang LH, Liu KS, Tsai TY, Lin SY, Hsu MS, Hsu LY, Chang SC. A multicenter study of risk factors and outcome of hospitalized patients with infections due to carbapenem-resistant Acinetobacter baumannii. Int J Infect Dis. 2010;14:e764–e769. doi: 10.1016/j.ijid.2010.02.2254. [DOI] [PubMed] [Google Scholar]
- 10.Wikler MA. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; Approved Standard. 8th ed. Wayne, Pa: CLSI; 2008. [Google Scholar]
- 11.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128–140. doi: 10.1016/0196-6553(88)90053-3. [DOI] [PubMed] [Google Scholar]
- 12.Lee NY, Lee HC, Ko NY, Chang CM, Shih HI, Wu CJ, Ko WC. Clinical and economic impact of multidrug resistance in nosocomial Acinetobacter baumannii bacteremia. Infect Control Hosp Epidemiol. 2007;28:713–719. doi: 10.1086/517954. [DOI] [PubMed] [Google Scholar]
- 13.Lee YT, Kuo SC, Yang SP, Lin YT, Tseng FC, Chen TL, Fung CP. Impact of appropriate antimicrobial therapy on mortality associated with Acinetobacter baumannii bacteremia: relation to severity of infection. Clin Infect Dis. 2012;55:209–215. doi: 10.1093/cid/cis385. [DOI] [PubMed] [Google Scholar]
- 14.Choi JY, Park YS, Kim CO, Park YS, Yoon HJ, Shin SY, Kim YA, Song YG, Yong D, Lee K, Kim JM. Mortality risk factors of Acinetobacter baumannii bacteraemia. Intern Med J. 2005;35:599–603. doi: 10.1111/j.1445-5994.2005.00925.x. [DOI] [PubMed] [Google Scholar]
- 15.Routsi C, Pratikaki M, Platsouka E, Sotiropoulou C, Nanas S, Markaki V, Vrettou C, Paniara O, Giamarellou H, Roussos C. Carbapenem-resistant versus carbapenem-susceptible Acinetobacter baumannii bacteremia in a Greek intensive care unit: risk factors, clinical features and outcomes. Infection. 2010;38:173–180. doi: 10.1007/s15010-010-0008-1. [DOI] [PubMed] [Google Scholar]
- 16.Cisneros JM, Rodríguez-Baño J. Nosocomial bacteremia due to Acinetobacter baumannii: epidemiology, clinical features and treatment. Clin Microbiol Infect. 2002;8:687–693. doi: 10.1046/j.1469-0691.2002.00487.x. [DOI] [PubMed] [Google Scholar]


