Abstract
BACKGROUND
In the Genetic Epidemiology Network of Salt Sensitivity (GenSalt) study, we observed that blood pressure (BP) responses to dietary sodium and potassium interventions and the cold pressor test (CPT) varied greatly among individuals. We conducted a replication study to confirm our previous findings among 695 study participants.
METHODS
The dietary intervention included a 7-day low sodium (51.3 mmol/day), a 7-day high sodium (307.8 mmol/day), and a 7-day high sodium with potassium supplementation (307.8 mmol sodium and 60 mmol potassium/day). BP measurements were obtained during the baseline and each intervention phase. During the CPT, BP was measured before and at 0, 1, 2, and 4 minutes after the participants immersed their right hand in ice water for 1 minute.
RESULTS
Systolic and diastolic BP responses (mean ± SD (range), mm Hg) were 8.1±8.4 (−39.1 to 18.2) and −3.5±5.1 (−25.1 to 11.1) to low sodium, 9.1±8.4 (−13.3 to 33.1) and 4.0±5.4 (−16.0 to 20.7) to high sodium, and −4.6±5.8 (−31.8 to 11.6) and −1.9±4.3 (−16.9 to 14.2) to potassium supplementation, respectively (all P < 0.0001 for comparison with each former phase). The mean maximum systolic and diastolic BP responses to the CPT were 16.5±10.5 (−15.3 to 63.3) and 7.6±6.1 (−8.7 to 39.3), respectively (all P < 0.0001).
CONCLUSIONS
Our study indicates that there are large variations in BP responses to dietary sodium and potassium interventions and to the CPT among individuals.
Keywords: blood pressure, cold pressor test, dietary potassium, hypertension, salt sensitivity, sodium.
High dietary sodium and low potassium intake have been related to increased blood pressure (BP) in animal experiments, observational epidemiologic studies, and randomized controlled clinical trials.1–3 However, BP responses to dietary sodium and potassium intake vary considerably among individuals.2,4–6 The increased BP response to sodium, also known as salt sensitivity, has been associated with an increased risk of hypertension, cardiovascular disease, and premature death.7,8 The cold pressor test (CPT), which measures BP response to the stimulus of external cold, has been used for the evaluation of cardiovascular reactivity to stress in normotensive and hypertensive subjects. Cardiovascular hyper-reactivity to stress has been related to the development of hypertension and cardiovascular disease.9–11 In addition, increased BP response to the CPT has been associated with greater BP responses to changes in dietary sodium and potassium intake.12 Previous studies have indicated that both genetic and environmental factors may contribute to BP responses to dietary sodium and potassium intake and to the CPT.13–17
The Genetic Epidemiology Network of Salt Sensitivity (GenSalt) study aimed to investigate genetic factors related to BP responses to dietary sodium and potassium interventions, as well as the CPT.18 The study participant recruitment, dietary intervention, and data collection were conducted between October 2003 and July 2005. The study used a family-based feeding study design, and each family was ascertained through a proband with untreated prehypertension or stage 1 hypertension. Families of those with hypertension are most likely enriched in genetic variants for hypertension and tend to be more sensitive to dietary sodium and potassium interventions and the CPT. This design should potentially maximize the study power for identifying genetic variants for BP responses to dietary sodium and potassium intake and the CPT. A total of 1,906 study participants from 633 families took part in a 21-day dietary intervention including a 7-day low-sodium feeding, a 7-day high-sodium feeding, and a 7-day high-sodium feeding with potassium supplementation.
The GenSalt study observed that BP responses to dietary sodium and potassium interventions and the CPT varied greatly among individuals.19 The GenSalt study also indicated that the heritabilities for BP responses to dietary sodium and potassium interventions and to the CPT were moderate, ranging 0.24–0.42.14 Novel genetic variants have been identified that are associated with BP responses among the GenSalt study population.20–28 To replicate and validate significant findings of the GenSalt study, we recruited an independent sample from rural north China and conducted the same measurements and interventions as the GenSalt study. Here we present the detailed design and methods of the GenSalt replication study, as well as the baseline characteristics and blood pressure responses to the dietary sodium and potassium interventions and the CPT.
METHODS
Study participants
In the GenSalt replication study, the participant recruitment and dietary intervention were conducted from April 2010 to November 2010. Four field sites in Hebei, Shanxi, Shandong, and Jiangsu provinces in rural north China were selected. These field sites are similar with those of the GenSalt study in regards to ethnicity and environmental exposures, including lifestyle, nutritional factors, and habitual dietary intake of high salt and low potassium.18 The residents in these regions are of Han nationality, the ethnic majority in China.19 To provide a comparable replication sample for the GenSalt study, we applied the same family-based study design in the replication study.18 A community-based BP screening was conducted among persons aged 18–60 years in the study villages to identify potential probands and their families. Probands with mean systolic BP (SBP) of 130–160mm Hg and/or diastolic BP (DBP) of 85–100mm Hg, their siblings, and offspring were recruited for the dietary intervention. For families with eligible offspring, spouses of the probands were also invited to participate because their genetic relatedness with the offspring can provide additional information for genetic analyses. Individuals who had stage 2 hypertension, secondary hypertension, a history of clinical cardiovascular disease, diabetes, or chronic kidney disease or a urine albumin concentration ≥20mg/dl, who used antihypertensive medications, or who were pregnant, heavy alcohol users, or currently on a low-sodium diet were excluded from the dietary intervention. A total of 695 study participants from 308 families were enrolled in this study. Of these families, 300 include only siblings, and 8 include both siblings and offspring. The family sizes range 2–6 with an average of 2.3. Institutional review boards at all participating institutes approved the study, and written informed consent was obtained from each participant. The GenSalt replication study is an extension of the GenSalt study (Clinical Trials.gov Identifier: NCT00721721).
Dietary intervention
After a 3-day baseline observation, the study participants received a 7-day low-salt diet (3 grams of salt or 51.3 mmol of sodium per day) followed by a 7-day high-salt diet (18 grams of salt or 307.8 mmol of sodium per day). During the first 2 intervention phases, dietary potassium intake remained unchanged. In the final 7-day intervention phase, the participants maintained a high-salt diet (18 grams of salt or 307.8 mmol of sodium per day) and took a 60 mmol potassium supplement. During dietary interventions, total energy intake was varied according to each participant’s baseline energy intake. All foods were cooked without salt, and prepackaged salt was added to the individual study participant’s meal when it was served by the study staff. To ensure study participants’ compliance with the intervention program, they were required to have their breakfast, lunch, and dinner at the study kitchen under supervision of the study staff during the entire study period. The study participants were instructed to avoid consuming any foods and beverages that were not provided by the study. In addition, 3 timed urinary specimens (one 24-hour and 2 overnight) were collected at baseline and in each intervention phase (days 5, 6, and 7) to monitor participants’ compliance with the dietary sodium intervention. Timed overnight urinary excretions of sodium and potassium were converted to 24-hour values based on formulas developed from a random subsample of 238 GenSalt participants who had collected overnight and 24-hour measures on the same days at baseline and in each phase of the intervention.19
Phenotype measurements
A standard questionnaire was administered by trained staff at the baseline examination to collect information on demographic characteristics, personal and family medical history, and lifestyle risk factors. Body weight, height, and waist circumference were measured twice in light indoor clothing without shoes during the baseline examination. Waist circumference was measured 1cm above the participant’s navel during light breathing.
BP measurements.
Three BP measurements were obtained each morning of the 3-day baseline examination and on days 5, 6, and 7 of each intervention period by trained and certified observers using a random-zero sphygmomanometer according to a standard protocol. BP was measured with the participant in the sitting position after 5 minutes of rest. In addition, participants were advised to avoid alcohol, cigarette smoking, coffee, tea, and exercise for at least 30 minutes before their measurement. All BP observers were blinded to the dietary intervention. All the sphygmomanometers were centrally calibrated in the field coordinating center at Fuwai Hospital, Chinese Academy of Medical Sciences, Beijing, China.
All BP observers participated in a special training session on the use of a standardized protocol for measurement of BP. Satisfactory performance during a written test on knowledge of preparing study participants for BP measurement, selecting correct cuff size, and using standard techniques for BP measurement during a standardized videotape examination and during concordant measurements of BP with an instructor was required for certification as a GenSalt replication study BP observer.
Cold pressor test.
The CPT was conducted during the baseline examination. After the participant had remained seated for 20 minutes, 3 BP measurements were obtained using a standard mercury sphygmomanometer before the ice water immersion. Then the participant immersed their left hand in the ice water bath (3–5 °C) to just above the wrist for 1 minute. BP measurements at 0, 1, 2, and 4 minutes were obtained on the right arm using a standard mercury sphygmomanometer after the left hand had been removed from the ice water bath.
Laboratory measurements.
Overnight fasting blood samples were drawn by venipuncture at the baseline examination. All blood samples were analyzed in the central clinical laboratory in Beijing. Total cholesterol, high-density lipoprotein cholesterol, and triglycerides were analyzed enzymatically using commercially available reagents. Low-density lipoprotein cholesterol levels were calculated using the Friedewald equation for participants who had triglyceride levels <400mg/dl: low-density lipoprotein cholesterol = total cholesterol – high-density lipoprotein cholesterol – triglyceride/5. Plasma glucose was measured using a modified hexokinase by the modified kinetic Jaffe reaction method.
Statistical analysis
Means or percentages of baseline characteristics were calculated for the overall sample and different types of family members. The BP levels at baseline and during dietary interventions were calculated as the mean of 9 measurements from 3 clinical visits during the 3-day baseline observation or on days 5, 6, and 7 of each intervention phase. Mean arterial pressure = DBP + (SBP – DBP)/3. BP responses were defined as follows: BP response to low sodium from baseline = BP on low-sodium diet – BP at baseline; BP response to high sodium from low sodium = BP on high-sodium diet – BP on low-sodium diet; and BP response to potassium supplementation plus high sodium from high sodium = BP on high-sodium diet with potassium supplementation – BP on high-sodium diet.
The pre-CPT BP level was calculated as the mean of 3 BP measurements before the ice water immersion. BP responses at 0, 1, 2, and 4 minutes after the hand removal from ice water bath were calculated as the BP differences between BP levels at 0, 1, 2, and 4 minutes and the pre-CPT BP level, respectively. Individual maximum response was defined as the largest value among BP responses at 0, 1, 2, and 4 minutes. The area under the curve above baseline was calculated as the difference between the area under the response curve and the area below baseline. The area under the curve above baseline of BP response to the CPT summarizes the magnitude of BP increase (from pre-CPT to 0 minute) and its recovery from peak to baseline (0 to 4 minutes) during the CPT. The t test was used to examine the significance of these BP responses. Baseline characteristics and these variables of BP responses were also analyzed according to different types of family members as was done for the GenSalt study.18 All statistical analyses were conducted using SAS statistical software version 9.2 (SAS Institute, Cary, NC).
RESULTS
Baseline characteristics of study participants are presented in Table 1. The average age of the study participants was 48.0 years, and 56.0% were male. Compared with other family members, probands were older and had greater body mass index, waist circumference, BP levels, and plasma glucose and serum lipids, as well as higher prevalence of current cigarette smoking and alcohol drinking. All study participants were farmers and engaged in heavy physical labor.
Table 1.
Baseline characteristics of the GenSalt replication study participants.
| Characteristic | All | Probands | Siblings/ Spouse | Offspring |
|---|---|---|---|---|
| No. | 695 | 313 | 365/1 | 16 |
| Age, y | 48.0±9.1 | 49.5±8.2 | 47.7±8.4 | 24.7±7.1 |
| Male, % | 56.0 | 58.2 | 54.9 | 37.5 |
| High school graduated, % | 14.2 | 15.3 | 13.9 | 0 |
| Current cigarette smoking, % | 30.9 | 32.3 | 30.3 | 18.8 |
| Current alcohol drinking, % | 26.0 | 30.0 | 22.7 | 25.0 |
| Physical activity, MET | 21.0±12.0 | 20.4±11.5 | 21.5±12.5 | 20.0±10.0 |
| Body weight, kg | 66.5±11.6 | 69.0±11.7 | 64.8±11.1 | 57.4±9.6 |
| Body mass index, kg/m2 | 25.3±3.6 | 26.0±3.6 | 24.8±3.5 | 22.3±2.7 |
| Waist circumference, cm | 86.2±10.7 | 88.6±10.9 | 84.5±10.0 | 74.8±9.5 |
| Heart rate, beats/min | 71.9±6.9 | 71.5±7.1 | 72.1±6.7 | 76.2±5.6 |
| Plasma glucose, mg/dl | 98.2±25.7 | 101.2±28.7 | 96.1±23.0 | 85.3±8.2 |
| Serum total cholesterol, mg/dl | 175.3±38.1 | 179.4±37.0 | 173.1±38.8 | 146.7±25.1 |
| Serum HDL cholesterol, mg/dl | 48.1±13.8 | 47.8±13.7 | 48.3±14.2 | 50.1±7.0 |
| Serum LDL cholesterol, mg/dl | 97.2±30.7 | 99.5±30.0 | 96.2±31.4 | 76.5±17.6 |
| Serum triglyceride, mg/dl | 162.4±138.2 | 176.6±160.7 | 152.9±116.7 | 100.7±63.9 |
Continuous variables are indicated as mean ± SD.
Abbreviations: HDL, high density lipoprotein; LDL, low density lipoprotein; MET, metabolic equivalent.
Among the enrolled participants, 684 (98.4%), 666 (95.8%), 659 (94.8%), and 654 (94.1%) completed the baseline examination, low-sodium intervention, high-sodium intervention, and potassium-supplementation intervention, respectively. The 24-hour urinary excretions of sodium and potassium during the interventions indicated excellent compliance with the study diet (Table 2).
Table 2.
Blood pressure levels and urinary excretion of sodium and potassium during baseline and dietary interventions
| All | Probands | Siblings/Spouse | Offspring | |
|---|---|---|---|---|
| Baseline | ||||
| SBP, mm Hg | 124.5±14.5 | 131.6±12.2 | 118.9±13.6 | 115.4±12.4 |
| DBP, mm Hg | 80.4±9.3 | 83.7±8.6 | 77.8±9.1 | 74.4±8.4 |
| MAP, mm Hg | 95.1±10.3 | 99.6±8.8 | 91.5±10.0 | 88.0±8.9 |
| Sodium, mmol/24 h | 220.4±59.3 | 223.0±58.5 | 218.2±59.4 | 218.1±72.1 |
| Potassium, mmol/24 h | 39.1±12.9 | 38.8±13.1 | 39.5±12.9 | 32.9±8.2 |
| Low-sodium intervention | ||||
| SBP, mm Hg | 116.5±11.9 | 121.3±11.5 | 112.5±10.8 | 113.1±10.7 |
| DBP, mm Hg | 77.0±8.4 | 79.4±8.1 | 75.1±8.1 | 73.1±9.9 |
| MAP, mm Hg | 90.1±8.9 | 93.4±8.3 | 87.5±8.4 | 86.4±9.4 |
| Sodium, mmol/24 h | 62.8±27.8 | 62.3±25.8 | 63.3±29.3 | 60.7±29.2 |
| Potassium, mmol/24 h | 33.9±12.7 | 33.6±12.1 | 34.4±13.2 | 28.9±10.3 |
| High-sodium intervention | ||||
| SBP, mm Hg | 125.5±14.9 | 131.7±13.8 | 120.6±13.9 | 115.9±12.7 |
| DBP, mm Hg | 80.9±9.7 | 84.1±8.8 | 78.6±9.5 | 73.3±10.6 |
| MAP, mm Hg | 95.8±10.8 | 99.9±9.6 | 92.6±10.4 | 87.5±10.8 |
| Sodium, mmol/24 h | 236.7±43.7 | 240.1±42.3 | 234.7±44.7 | 216.4±42.1 |
| Potassium, mmol/24 h | 41.4±13.2 | 41.3±12.4 | 41.8±13.9 | 33.8±9.0 |
| Potassium supplementation plus high sodium | ||||
| SBP, mm Hg | 120.9±13.6 | 126.7±13.1 | 116.2±12.1 | 114.2±11.0 |
| DBP, mm Hg | 79.1±8.9 | 82.0±8.3 | 76.9±8.6 | 72.5±9.5 |
| MAP, mm Hg | 93.0±9.8 | 96.9±9.0 | 90.0±9.2 | 86.4±9.5 |
| Sodium, mmol/24 h | 240.0±41.0 | 243.1±41.2 | 237.7±40.5 | 231.0±45.1 |
| Potassium, mmol/24 h | 76.5±16.2 | 77.1±15.9 | 76.4±16.4 | 66.2±14.6 |
Values are mean ± SD.
Abbreviations: DBP, diastolic blood pressure; MAP, mean arterial pressure; SBP, systolic blood pressure.
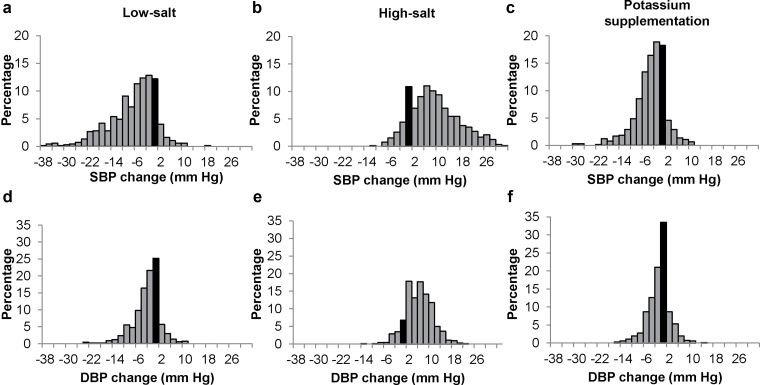
Mean SBP, DBP, and mean arterial pressure levels at baseline and during dietary interventions are presented in Table 2. In general, BP levels decreased from baseline during the low-sodium intervention and increased from the low-sodium intervention to the high-sodium intervention. BP levels were reduced during potassium supplementation compared with the high-sodium intervention (all P < 0.0001) (Table 3). Among all types of study participants, probands had the greatest SBP, DBP, and mean arterial pressure responses to dietary interventions. Distributions of SBP and DBP responses to dietary interventions are shown in Figure 1. Both SBP and DBP levels decreased during low-sodium and potassium-supplementation interventions but increased during the high-sodium intervention among the majority of study participants. For example, SBP decreased (responses <0mm Hg) in 86.4% and 82.5% participants during low-sodium and potassium-supplementation interventions, respectively, and increased (responses >0mm Hg) in 85.7% of participants during the high-sodium intervention.
Table 3.
Blood pressure responses to dietary sodium and potassium interventions
| All | Probands | Siblings/ spouse | Offspring | ||
|---|---|---|---|---|---|
| Mean ± SD | Range | ||||
| Responses to low sodium from baseline, mm Hg | |||||
| SBP | −8.1±8.4* | −39.1 to 18.2 | −10.3±8.8 | −6.5±7.4 | −2.3±9.0 |
| DBP | −3.5±5.1* | −25.1 to 11.1 | −4.3±5.2 | −2.9±4.8 | −1.3±6.9 |
| MAP | −5.0±5.6* | −28.4 to 12.9 | −6.3±5.8 | −4.1±5.1 | −1.6±6.9 |
| Responses to high sodium from low sodium, mm Hg | |||||
| SBP | 9.1±8.4* | −13.3 to 33.1 | 10.4±8.5 | 8.2±8.1 | 2.8±7.2 |
| DBP | 4.0±5.4* | −16.0 to 20.7 | 4.7±5.0 | 3.6±5.5 | 0.2±5.5 |
| MAP | 5.7±5.9* | −10.4 to 24.8 | 6.6±5.7 | 5.1±6.0 | 1.1±5.5 |
| Responses to potassium supplementation plus high sodium from high sodium, mm Hg | |||||
| SBP | −4.6±5.8* | −31.8 to 11.6 | −5.1±5.4 | −4.4±6.2 | −1.7±5.9 |
| DBP | −1.9±4.3* | −16.9 to 14.2 | −2.1±3.9 | −1.7±4.7 | −0.8±4.1 |
| MAP | −2.8±4.3* | −18.5 to 11.0 | −3.1±3.8 | −2.6±4.7 | −1.1±4.0 |
Values are mean ± SD.
Abbreviations: DBP, diastolic blood pressure; MAP, mean arterial pressure; SBP, systolic blood pressure.
*P < 0.0001 for comparison with zero blood pressure change.
Figure 1.
Distribution of systolic blood pressure (SBP) (upper panel, a–c) and diastolic blood pressure (DBP) (lower panel, d–f) responses to low-salt intervention (left panel), high-salt intervention (middle panel), and potassium supplementation (right panel). Black bars indicate individuals with zero blood pressure (BP) response. BP response to low salt = BP on low-salt diet – BP at baseline; BP response to high salt = BP on high-salt diet – BP on low-salt diet; and BP response to potassium supplementation = BP on high-salt diet with potassium supplementation – BP on high-salt diet.
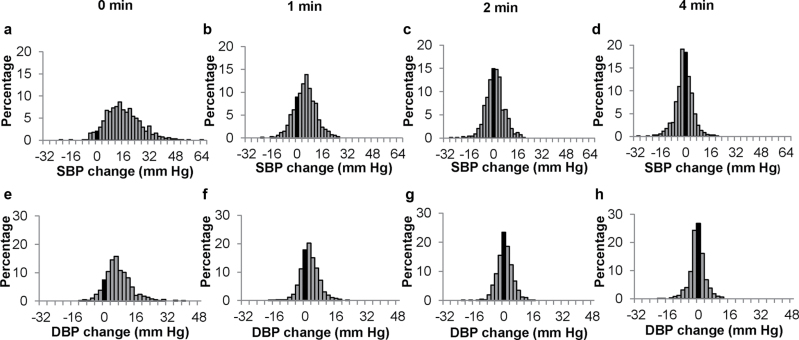
A total of 684 (98.4%) participants completed the CPT. Figure 2 shows the distributions of SBP and DBP responses at different time points during the CPT. The majority of participants (81.0%) achieved maximum responses at 0 minutes. The average BP returned to pre-CPT level 4 minutes after the end of ice-water immersion. Compared with other family members, probands had greater maximum BP responses to the CPT (Table 4).
Figure 2.
Distribution of systolic blood pressure (SBP) (upper panel, a–d) and diastolic blood pressure (DBP) (lower panel, e–h) responses to the cold pressor test (CPT) at 0, 1, 2, and 4 minutes after the end of ice-water immersion. Black bars indicate individuals with zero blood pressure (BP) response. BP response at 0 minutes = BP at 0 minutes – pre-CPT BP; BP response at 1 minute = BP at 1 minute – pre-CPT BP; BP response at 2 minutes = BP at 2 minutes – pre-CPT BP; and BP response at 4 minutes = BP at 4 minutes – pre-CPT BP.
Table 4.
Blood pressure responses to cold pressor test
| All | Probands | Siblings/ spouse | Offspring | ||
|---|---|---|---|---|---|
| Mean ± SD | Range | ||||
| SBP responses to cold pressor test from pretest, mm Hg | |||||
| 0 min | 16.2±10.9* | −22.0 to 63.3 | 17.0±10.9 | 15.6±10.8 | 13.9±10.8 |
| 1 min | 5.1±6.9* | −21.3 to 26.0 | 5.4±7.0 | 5.0±6.8 | 2.7±7.8 |
| 2 min | 1.0±6.1* | −28.0 to 19.3 | 1.1±6.3 | 0.9±5.9 | −1.1±7.2 |
| 4 min | −0.9±5.5* | −29.3 to 20.7 | −0.8±6.0 | −0.8±4.9 | −5.0±6.6 |
| Maximum | 16.5±10.5* | −15.3 to 63.3 | 17.3±10.6 | 15.9±10.5 | 15.3±9.0 |
| AUC | 21.8±26.0* | −87.0 to 107.0 | 23.2±26.5 | 21.1±25.5 | 10.0±25.2 |
| DBP responses to cold pressor test from pretest, mm Hg | |||||
| 0 min | 7.1±6.7* | −12.7 to 39.3 | 7.2±7.0 | 6.9±6.2 | 7.1±9.5 |
| 1 min | 2.4±4.8* | −18.7 to 22.7 | 2.4±4.9 | 2.4±4.6 | 1.1±6.9 |
| 2 min | 0.6±4.2** | −21.3 to 16.0 | 0.4±4.2 | 0.8±4.1 | −1.4±6.4 |
| 4 min | −0.5±3.9** | −19.3 to 12.0 | −0.6±4.0 | −0.3±3.7 | −2.5±5.6 |
| Maximum | 7.6±6.1* | −8.7 to 39.3 | 7.9±6.5 | 7.4±5.8 | 8.1±7.9 |
| AUC | 9.8±17.4* | −65.0 to 68.0 | 9.7±17.5 | 10.1±16.8 | 3.5±27.2 |
Values are mean ± SD. Blood pressure responses were calculated as blood pressure at time 0, 1, 2, and 4 minutes after ice water immersion – mean blood pressure at pretest.
Abbreviations: AUC, area-under-the-curve; DBP, diastolic blood pressure; SBP, systolic blood pressure.
*P <0.0001 for comparison with zero blood pressure change; **P <0.001 for comparison with zero blood pressure change.
Compared with the original GenSalt study participants, the replication study participants were older, had greater BMI and waist circumference, and had higher BP levels and hypertension prevalence because the replication study recruited a higher proportion of probands and siblings and a lower proportion of offspring (Supplementary Table S1). We also compared the BP responses to dietary interventions and the CPT between the replication study participants and the original GenSalt study participants. Most of the BP response variables were not significantly different between the original GenSalt study and the replication study after adjusting for multiple covariables. However, the replication study participants had significantly higher BP responses to high sodium from low sodium (Supplementary Table S2).
DISCUSSION
Hypertension is a global public health challenge because of its high prevalence and related risk of CVD and premature death.29,30 Hypertension is a complex disease and influenced by both genetic and environmental factors as well as their interactions. Recently, large-scale genome-wide association studies have achieved significant progress in revealing the genetic structure of BP traits.31–34 They identified multiple novel genomic loci associated with BP levels and hypertension. However, the effect sizes of those loci were small (<1mm Hg) and explained a very limited proportion of BP variation. Thus, the extensive and complicated interactions between genetic and environmental factors, which were not examined in most genome-wide association studies, may play an important role in BP regulation. High dietary sodium intake, low potassium intake, and cardiovascular hyper-reactivity to stress are related to elevated BP levels. It has been documented that genetic factors influence BP responses to dietary sodium and potassium intake and the CPT among individuals.13,14,16,17 Therefore, identifying genetic variants determining BP responses to these environmental factors should be able to greatly enhance our knowledge of the genetic architecture of BP regulation.
The GenSalt replication study provided further evidence to support several observations derived from the GenSalt study. First, BP responses to dietary sodium and potassium intake vary among individuals and are normally distributed. Second, salt sensitivity and potassium sensitivity are quite common in the human population. Most of the participants experienced a decrease in BP during the low-sodium and potassium-supplementation interventions and an increase during the high-sodium intervention. Third, BP responses to the CPT vary among the population. Finally, compared with other family members, probands showed greater BP responses to dietary sodium and potassium interventions and the CPT. Previous findings from the GenSalt study have indicated that older age and higher baseline BP levels were associated with greater BP responses to these interventions.19 The fact that probands were older and had higher baseline BP may partially explain the greater BP responses observed in probands.
The findings from the community-based GenSalt study can readily apply to the Chinese general population and other East Asian populations. In addition, biologic pathways for BP regulation should be similar across populations with different racial/ethnic backgrounds. This study warrants further replication studies in various populations.
The GenSalt study has conducted extensive genetic research, including genome-wide linkage studies, biological pathway–based candidate gene studies, and genome-wide association studies.20–23,27,28,35–37 For example, the GenSalt study identified the angiotensin II receptor type 1 gene as a significant predictor of BP responses to potassium intake by a genome-wide linkage and positional candidate gene analysis.21 In addition, the GenSalt study also found that polymorphisms of the epithelial sodium channel subunit γ and angiotensin-converting enzyme 2 were associated with BP responses to sodium interventions and the CPT, respectively.22,28 In spite of careful conduction and strict quality control procedures implemented in the GenSalt study, it is necessary to replicate and validate genetic findings of the study in independent samples. The same or comparable phenotype in replication samples is an important criterion for claiming replication.38,39 This study will provide valued and unique phenotypes to replicate the novel findings from the GenSalt study.
In summary, the GenSalt replication study confirmed the large variations of BP responses to dietary sodium and potassium interventions and the CPT among individuals. By using the identical protocol in an independent study sample, this study provides a unique opportunity to replicate the novel findings of genetic variants associated with BP responses to dietary sodium and potassium intake and the CPT from the GenSalt study.
SUPPLEMENTARY MATERIAL
Supplementary materials are available at American Journal of Hypertension (http://ajh.oxfordjournals.org).
DISCLOSURE
The authors declared no conflict of interest.
Supplementary Material
ACKNOWLEDGMENTS
The GenSalt replication study is supported by research grants (R01HL087263 and R01HL090682) from the National Heart, Lung, and Blood Institute , National Institutes of Health, Bethesda, MD. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Upsher-Smith Laboratories, Maple Grove, Minnesota, has provided Klor-Con M20 potassium tablets for the GenSalt replication study.
REFERENCES
- 1. Jones DW. Dietary sodium and blood pressure. Hypertension 2004; 43:932–935 [DOI] [PubMed] [Google Scholar]
- 2. Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann D, Klag MJ. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA 1997; 277:1624–1632 [DOI] [PubMed] [Google Scholar]
- 3. Adrogue HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med 2007; 356:1966–1978 [DOI] [PubMed] [Google Scholar]
- 4. Kawasaki T, Delea CS, Bartter FC, Smith H. The effect of high-sodium and low-sodium intakes on blood pressure and other related variables in human subjects with idiopathic hypertension. Am J Med 1978; 64:193–198 [DOI] [PubMed] [Google Scholar]
- 5. Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension 1996; 27:481–490 [DOI] [PubMed] [Google Scholar]
- 6. Franco V, Oparil S. Salt sensitivity, a determinant of blood pressure, cardiovascular disease and survival. J Am Coll Nutr 2006; 25:247S–255S [DOI] [PubMed] [Google Scholar]
- 7. Morimoto A, Uzu T, Fujii T, Nishimura M, Kuroda S, Nakamura S, Inenaga T, Kimura G. Sodium sensitivity and cardiovascular events in patients with essential hypertension. Lancet 1997; 350:1734–1737 [DOI] [PubMed] [Google Scholar]
- 8. Weinberger MH, Fineberg NS, Fineberg SE, Weinberger M. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension 2001; 37:429–432 [DOI] [PubMed] [Google Scholar]
- 9. Krantz DS, Manuck SB. Acute psychophysiologic reactivity and risk of cardiovascular disease: a review and methodologic critique. Psychol Bull 1984; 96:435–464 [PubMed] [Google Scholar]
- 10. Manuck SB. Cardiovascular reactivity in cardiovascular disease: “once more unto the breach.” Int J Behav Med 1994; 1:4–31 [DOI] [PubMed] [Google Scholar]
- 11. Treiber FA, Kamarck T, Schneiderman N, Sheffield D, Kapuku G, Taylor T. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosom Med 2003; 65:46–62 [DOI] [PubMed] [Google Scholar]
- 12. Chen J, Gu D, Jaquish CE, Chen CS, Rao DC, Liu D, Hixson JE, Hamm LL, Gu CC, Whelton PK, He J. Association between blood pressure responses to the cold pressor test and dietary sodium intervention in a Chinese population. Arch Intern Med 2008; 168:1740–1746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Svetkey LP, McKeown SP, Wilson AF. Heritability of salt sensitivity in black Americans. Hypertension 1996; 28:854–858 [DOI] [PubMed] [Google Scholar]
- 14. Gu D, Rice T, Wang S, Yang W, Gu C, Chen CS, Hixson JE, Jaquish CE, Yao ZJ, Liu DP, Rao DC, He J. Heritability of blood pressure responses to dietary sodium and potassium intake in a Chinese population. Hypertension 2007; 50:116–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kelly TN, He J. Genomic epidemiology of blood pressure salt sensitivity. J Hypertens 2012; 30:861–873 [DOI] [PubMed] [Google Scholar]
- 16. Mei H, Gu D, Rice TK, Hixson JE, Chen J, Jaquish CE, Zhao Q, Chen CS, Chen JC, Gu CC, Kelly TN, He J. Heritability of blood pressure responses to cold pressor test in a Chinese population. Am J Hypertens 2009; 22:1096–1100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Busjahn A, Faulhaber HD, Viken RJ, Rose RJ, Luft FC. Genetic influences on blood pressure with the cold-pressor test: a twin study. J Hypertens 1996; 14:1195–1199 [DOI] [PubMed] [Google Scholar]
- 18. GenSalt Collaborative Research Group GenSalt: rationale, design, methods and baseline characteristics of study participants. J Hum Hypertens 2007; 21:639–646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. He J, Gu D, Chen J, Jaquish CE, Rao DC, Hixson JE, Chen JC, Duan X, Huang JF, Chen CS, Kelly TN, Bazzano LA, Whelton PK. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J Hypertens 2009; 27:48–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhao Q, Gu D, Kelly TN, Hixson JE, Rao DC, Jaquish CE, Chen J, Huang J, Chen CS, Gu CC, Whelton PK, He J. Association of genetic variants in the apelin-APJ system and ACE2 with blood pressure responses to potassium supplementation: the GenSalt study. Am J Hypertens 2010; 23:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kelly TN, Hixson JE, Rao DC, Mei H, Rice TK, Jaquish CE, Shimmin LC, Schwander K, Chen CS, Liu D, Chen J, Bormans C, Shukla P, Farhana N, Stuart C, Whelton PK, He J, Gu D. Genome-wide linkage and positional candidate gene study of blood pressure response to dietary potassium intervention: the genetic epidemiology network of salt sensitivity study. Circ Cardiovasc Genet 2010; 3:539–547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zhao Q, Gu D, Hixson JE, Liu DP, Rao DC, Jaquish CE, Kelly TN, Lu F, Ma J, Mu J, Shimmin LC, Chen J, Mei H, Hamm LL, He J. Common variants in epithelial sodium channel genes contribute to salt sensitivity of blood pressure: the GenSalt study. Circ Cardiovasc Genet 2011; 4:375–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhao Q, Hixson JE, Rao DC, Gu D, Jaquish CE, Rice T, Shimmin LC, Chen J, Cao J, Kelly TN, Hamm LL, He J. Genetic variants in the apelin system and blood pressure responses to dietary sodium interventions: a family-based association study. J Hypertens 2010; 28:756–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Defago MD, Gu D, Hixson JE, Shimmin LC, Rice TK, Gu CC, Jaquish CE, Liu DP, He J, Kelly TN. Common genetic variants in the endothelial system predict blood pressure response to sodium intake: the GenSalt Study. Am J Hypertens 2013; 26:643–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gu D, Zhao Q, Kelly TN, Hixson JE, Rao DC, Cao J, Chen J, Li J, Ji X, Hu D, Wang X, Liu DP, He J. The role of the kallikrein-kinin system genes in the salt sensitivity of blood pressure: the GenSalt Study. Am J Epidemiol 2012; 176:S72–S80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mei H, Gu D, Hixson JE, Rice TK, Chen J, Shimmin LC, Schwander K, Kelly TN, Liu DP, Chen S, Huang JF, Jaquish CE, Rao DC, He J. Genome-wide linkage and positional association study of blood pressure response to dietary sodium intervention: the GenSalt Study. Am J Epidemiol 2012; 176:S81–S90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang L, Hou L, Li H, Chen J, Kelly TN, Jaquish CE, Rao DC, Hixson JE, Hu D, Chen CS, Gu C, Chen S, Lu X, Whelton PK, He J, Lu F, Huang J, Liu DP, Gu D. Genetic variants in the renin-angiotensin system and blood pressure reactions to the cold pressor test. J Hypertens 2010; 28:2422–2428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Huang J, Chen S, Lu X, Zhao Q, Rao DC, Jaquish CE, Hixson JE, Chen J, Wang L, Cao J, Li J, Li H, He J, Liu DP, Gu D. Polymorphisms of ACE2 are associated with blood pressure response to cold pressor test: the GenSalt study. Am J Hypertens 2012; 25:937–942 [DOI] [PubMed] [Google Scholar]
- 29. Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371:1513–1518 [DOI] [PubMed] [Google Scholar]
- 30. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet 2005; 365:217–223 [DOI] [PubMed] [Google Scholar]
- 31. Newton-Cheh C, Johnson T, Gateva V, Tobin MD, Bochud M, Coin L, Najjar SS, Zhao JH, Heath SC, Eyheramendy S, Papadakis K, Voight BF, Scott LJ, Zhang F, Farrall M, Tanaka T, Wallace C, Chambers JC, Khaw KT, Nilsson P, van der Harst P, Polidoro S, Grobbee DE, Onland-Moret NC, Bots ML, Wain LV, Elliott KS, Teumer A, Luan J, Lucas G, Kuusisto J, Burton PR, Hadley D, McArdle WL, Brown M, Dominiczak A, Newhouse SJ, Samani NJ, Webster J, Zeggini E, Beckmann JS, Bergmann S, Lim N, Song K, Vollenweider P, Waeber G, Waterworth DM, Yuan X, Groop L, Orho-Melander M, Allione A, Di Gregorio A, Guarrera S, Panico S, Ricceri F, Romanazzi V, Sacerdote C, Vineis P, Barroso I, Sandhu MS, Luben RN, Crawford GJ, Jousilahti P, Perola M, Boehnke M, Bonnycastle LL, Collins FS, Jackson AU, Mohlke KL, Stringham HM, Valle TT, Willer CJ, Bergman RN, Morken MA, Doring A, Gieger C, Illig T, Meitinger T, Org E, Pfeufer A, Wichmann HE, Kathiresan S, Marrugat J, O’Donnell CJ, Schwartz SM, Siscovick DS, Subirana I, Freimer NB, Hartikainen AL, McCarthy MI, O’Reilly PF, Peltonen L, Pouta A, de Jong PE, Snieder H, van Gilst WH, Clarke R, Goel A, Hamsten A, Peden JF, Seedorf U, Syvanen AC, Tognoni G, Lakatta EG, Sanna S, Scheet P, Schlessinger D, Scuteri A, Dorr M, Ernst F, Felix SB, Homuth G, Lorbeer R, Reffelmann T, Rettig R, Volker U, Galan P, Gut IG, Hercberg S, Lathrop GM, Zelenika D, Deloukas P, Soranzo N, Williams FM, Zhai G, Salomaa V, Laakso M, Elosua R, Forouhi NG, Volzke H, Uiterwaal CS, van der Schouw YT, Numans ME, Matullo G, Navis G, Berglund G, Bingham SA, Kooner JS, Connell JM, Bandinelli S, Ferrucci L, Watkins H, Spector TD, Tuomilehto J, Altshuler D, Strachan DP, Laan M, Meneton P, Wareham NJ, Uda M, Jarvelin MR, Mooser V, Melander O, Loos RJ, Elliott P, Abecasis GR, Caulfield M, Munroe PB. Genome-wide association study identifies eight loci associated with blood pressure. Nat Genet 2009; 41:666–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Levy D, Ehret GB, Rice K, Verwoert GC, Launer LJ, Dehghan A, Glazer NL, Morrison AC, Johnson AD, Aspelund T, Aulchenko Y, Lumley T, Kottgen A, Vasan RS, Rivadeneira F, Eiriksdottir G, Guo X, Arking DE, Mitchell GF, Mattace-Raso FU, Smith AV, Taylor K, Scharpf RB, Hwang SJ, Sijbrands EJ, Bis J, Harris TB, Ganesh SK, O’Donnell CJ, Hofman A, Rotter JI, Coresh J, Benjamin EJ, Uitterlinden AG, Heiss G, Fox CS, Witteman JC, Boerwinkle E, Wang TJ, Gudnason V, Larson MG, Chakravarti A, Psaty BM, van Duijn CM. Genome-wide association study of blood pressure and hypertension. Nat Genet 2009; 41:677–687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kato N, Takeuchi F, Tabara Y, Kelly TN, Go MJ, Sim X, Tay WT, Chen CH, Zhang Y, Yamamoto K, Katsuya T, Yokota M, Kim YJ, Ong RT, Nabika T, Gu D, Chang LC, Kokubo Y, Huang W, Ohnaka K, Yamori Y, Nakashima E, Jaquish CE, Lee JY, Seielstad M, Isono M, Hixson JE, Chen YT, Miki T, Zhou X, Sugiyama T, Jeon JP, Liu JJ, Takayanagi R, Kim SS, Aung T, Sung YJ, Zhang X, Wong TY, Han BG, Kobayashi S, Ogihara T, Zhu D, Iwai N, Wu JY, Teo YY, Tai ES, Cho YS, He J. Meta-analysis of genome-wide association studies identifies common variants associated with blood pressure variation in east Asians. Nat Genet 2011; 43:531–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ehret GB, Munroe PB, Rice KM, Bochud M, Johnson AD, Chasman DI, Smith AV, Tobin MD, Verwoert GC, Hwang SJ, Pihur V, Vollenweider P, O’Reilly PF, Amin N, Bragg-Gresham JL, Teumer A, Glazer NL, Launer L, Zhao JH, Aulchenko Y, Heath S, Sober S, Parsa A, Luan J, Arora P, Dehghan A, Zhang F, Lucas G, Hicks AA, Jackson AU, Peden JF, Tanaka T, Wild SH, Rudan I, Igl W, Milaneschi Y, Parker AN, Fava C, Chambers JC, Fox ER, Kumari M, Go MJ, van der Harst P, Kao WH, Sjogren M, Vinay DG, Alexander M, Tabara Y, Shaw-Hawkins S, Whincup PH, Liu Y, Shi G, Kuusisto J, Tayo B, Seielstad M, Sim X, Nguyen KD, Lehtimaki T, Matullo G, Wu Y, Gaunt TR, Onland-Moret NC, Cooper MN, Platou CG, Org E, Hardy R, Dahgam S, Palmen J, Vitart V, Braund PS, Kuznetsova T, Uiterwaal CS, Adeyemo A, Palmas W, Campbell H, Ludwig B, Tomaszewski M, Tzoulaki I, Palmer ND, Aspelund T, Garcia M, Chang YP, O’Connell JR, Steinle NI, Grobbee DE, Arking DE, Kardia SL, Morrison AC, Hernandez D, Najjar S, McArdle WL, Hadley D, Brown MJ, Connell JM, Hingorani AD, Day IN, Lawlor DA, Beilby JP, Lawrence RW, Clarke R, Hopewell JC, Ongen H, Dreisbach AW, Li Y, Young JH, Bis JC, Kahonen M, Viikari J, Adair LS, Lee NR, Chen MH, Olden M, Pattaro C, Bolton JA, Kottgen A, Bergmann S, Mooser V, Chaturvedi N, Frayling TM, Islam M, Jafar TH, Erdmann J, Kulkarni SR, Bornstein SR, Grassler J, Groop L, Voight BF, Kettunen J, Howard P, Taylor A, Guarrera S, Ricceri F, Emilsson V, Plump A, Barroso I, Khaw KT, Weder AB, Hunt SC, Sun YV, Bergman RN, Collins FS, Bonnycastle LL, Scott LJ, Stringham HM, Peltonen L, Perola M, Vartiainen E, Brand SM, Staessen JA, Wang TJ, Burton PR, Artigas MS, Dong Y, Snieder H, Wang X, Zhu H, Lohman KK, Rudock ME, Heckbert SR, Smith NL, Wiggins KL, Doumatey A, Shriner D, Veldre G, Viigimaa M, Kinra S, Prabhakaran D, Tripathy V, Langefeld CD, Rosengren A, Thelle DS, Corsi AM, Singleton A, Forrester T, Hilton G, McKenzie CA, Salako T, Iwai N, Kita Y, Ogihara T, Ohkubo T, Okamura T, Ueshima H, Umemura S, Eyheramendy S, Meitinger T, Wichmann HE, Cho YS, Kim HL, Lee JY, Scott J, Sehmi JS, Zhang W, Hedblad B, Nilsson P, Smith GD, Wong A, Narisu N, Stancakova A, Raffel LJ, Yao J, Kathiresan S, O’Donnell CJ, Schwartz SM, Ikram MA, Longstreth WT, Jr, Mosley TH, Seshadri S, Shrine NR, Wain LV, Morken MA, Swift AJ, Laitinen J, Prokopenko I, Zitting P, Cooper JA, Humphries SE, Danesh J, Rasheed A, Goel A, Hamsten A, Watkins H, Bakker SJ, van Gilst WH, Janipalli CS, Mani KR, Yajnik CS, Hofman A, Mattace-Raso FU, Oostra BA, Demirkan A, Isaacs A, Rivadeneira F, Lakatta EG, Orru M, Scuteri A, Ala-Korpela M, Kangas AJ, Lyytikainen LP, Soininen P, Tukiainen T, Wurtz P, Ong RT, Dorr M, Kroemer HK, Volker U, Volzke H, Galan P, Hercberg S, Lathrop M, Zelenika D, Deloukas P, Mangino M, Spector TD, Zhai G, Meschia JF, Nalls MA, Sharma P, Terzic J, Kumar MV, Denniff M, Zukowska-Szczechowska E, Wagenknecht LE, Fowkes FG, Charchar FJ, Schwarz PE, Hayward C, Guo X, Rotimi C, Bots ML, Brand E, Samani NJ, Polasek O, Talmud PJ, Nyberg F, Kuh D, Laan M, Hveem K, Palmer LJ, van der Schouw YT, Casas JP, Mohlke KL, Vineis P, Raitakari O, Ganesh SK, Wong TY, Tai ES, Cooper RS, Laakso M, Rao DC, Harris TB, Morris RW, Dominiczak AF, Kivimaki M, Marmot MG, Miki T, Saleheen D, Chandak GR, Coresh J, Navis G, Salomaa V, Han BG, Zhu X, Kooner JS, Melander O, Ridker PM, Bandinelli S, Gyllensten UB, Wright AF, Wilson JF, Ferrucci L, Farrall M, Tuomilehto J, Pramstaller PP, Elosua R, Soranzo N, Sijbrands EJ, Altshuler D, Loos RJ, Shuldiner AR, Gieger C, Meneton P, Uitterlinden AG, Wareham NJ, Gudnason V, Rotter JI, Rettig R, Uda M, Strachan DP, Witteman JC, Hartikainen AL, Beckmann JS, Boerwinkle E, Vasan RS, Boehnke M, Larson MG, Jarvelin MR, Psaty BM, Abecasis GR, Chakravarti A, Elliott P, van Duijn CM, Newton-Cheh C, Levy D, Caulfield MJ, Johnson T. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature 2011; 478:103–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. He J, Gu D, Kelly TN, Hixson JE, Rao DC, Jaquish CE, Chen J, Zhao Q, Gu C, Huang J, Shimmin LC, Chen JC, Mu J, Ji X, Liu DP, Whelton PK. Genetic variants in the renin-angiotensin-aldosterone system and blood pressure responses to potassium intake. J Hypertens 2011; 29:1719–1730 [DOI] [PubMed] [Google Scholar]
- 36. Gu D, Kelly TN, Hixson JE, Chen J, Liu D, Chen JC, Rao DC, Mu J, Ma J, Jaquish CE, Rice TK, Gu C, Hamm LL, Whelton PK, He J. Genetic variants in the renin-angiotensin-aldosterone system and salt sensitivity of blood pressure. J Hypertens 2010; 28:1210–1220 [PMC free article] [PubMed] [Google Scholar]
- 37. Kelly TN, Rice TK, Gu D, Hixson JE, Chen J, Liu D, Jaquish CE, Bazzano LA, Hu D, Ma J, Gu CC, Huang J, Hamm LL, He J. Novel genetic variants in the alpha-adducin and guanine nucleotide binding protein beta-polypeptide 3 genes and salt sensitivity of blood pressure. Am J Hypertens 2009; 22:985–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chanock SJ, Manolio T, Boehnke M, Boerwinkle E, Hunter DJ, Thomas G, Hirschhorn JN, Abecasis G, Altshuler D, Bailey-Wilson JE, Brooks LD, Cardon LR, Daly M, Donnelly P, Fraumeni JF, Jr, Freimer NB, Gerhard DS, Gunter C, Guttmacher AE, Guyer MS, Harris EL, Hoh J, Hoover R, Kong CA, Merikangas KR, Morton CC, Palmer LJ, Phimister EG, Rice JP, Roberts J, Rotimi C, Tucker MA, Vogan KJ, Wacholder S, Wijsman EM, Winn DM, Collins FS. Replicating genotype-phenotype associations. Nature 2007; 447:655–660 [DOI] [PubMed] [Google Scholar]
- 39. McCarthy MI, Abecasis GR, Cardon LR, Goldstein DB, Little J, Ioannidis JP, Hirschhorn JN. Genome-wide association studies for complex traits: consensus, uncertainty and challenges. Nat Rev Genet 2008; 9:356–369 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.