Abstract
Culture shapes how individuals perceive and respond to others with mental illness. Prior studies have suggested that Asians and Asian Americans typically endorse greater stigma of mental illness compared to Westerners (White Europeans and Americans). However, whether these differences in stigma arise from cultural variations in automatic affective reactions or deliberative concerns of the appropriateness of one’s reactions to mental illness remains unknown. Here we compared implicit and explicit attitudes toward mental illness among Asian and Caucasian Americans. Asian Americans showed stronger negative implicit attitudes toward mental illness relative to Caucasian Americans, suggesting that cultural variation in stigma of mental illness can be observed even when concerns regarding the validity and appropriateness of one’s attitudes toward mental illness are minimized. Asian Americans also explicitly endorsed greater desire for social distance from mental illness relative to Caucasian Americans. These findings suggest that cultural variations in mental illness stigma may arise from cultural differences in automatic reactions to mental illness, though cultural variations in deliberative processing may further shape differences in these immediate reactions to mental illness.
Keywords: stigma, culture, mental illness, attitudes, implicit processes, social cognition
Though mental illness is stigmatized across societies, cultural variations in this stigma also exist (Abdullah & Brown, 2011). In particular, members of Asian cultures typically express greater stigma relative to their Western cultural counterparts, endorsing greater perceptions of mental illness and people with mental illness as shameful, threatening, abnormal, and morally deficient (Furnham & Chan, 2004; Yang, 2007), and desiring greater social distance from mental illness (Rao, Feinglass, & Corrigan, 2007).
From the perspective of dual-process models of attitudes and stigma (Gawronski & Bodenhausen, 2007; Reeder & Pryor, 2008; Strack & Deutsch, 2004), cultural variations in observed stigma may arise from cultural variability in two mechanisms involved in evaluating mental illness. The first mechanism concerns spontaneously activated affective reactions of positivity or negativity, or favor or disfavor toward mental illness, which are automatically activated irrespective of concerns of appropriateness or validity (Gawronski & Bodenhausen, 2007; Strack & Deutsch, 2004). As culturally-shared lay theories and meanings of mental illness may vary between cultures, automatic reactions elicited toward mental illness may also vary. The second mechanism consists of deliberative processes involved in validating activated knowledge for appropriateness and consistency (Gawronski & Bodenhausen, 2007; Strack & Deutsch, 2004). While negative reactions may be automatically activated against stigmatized groups, perceived social norms regarding the acceptability of experiencing and expressing these biases may influence how they are controlled and reported. As cultures vary in perceived social norms regarding how one should feel toward and talk about stigmatized groups, the expression of automatic affective reactions may vary across cultures as these reactions are validated and judged for appropriateness using culturally-discrepant sets of standards and available knowledge.
While the stigma of mental illness has been assessed at automatic levels of processing (Rusch, Corrigan, Todd, & Bodenhausen, 2010; Teachman, Wilson, & Komarovskaya, 2006), cultural comparisons of mental illness stigma have almost exclusively depended on self-report measures, such as responses on questionnaires, surveys, vignettes, and interviews. Whether observed cultural differences in stigma are due to between-culture variations in automatic affective reactions to mental illness or exclusively dependent on variations in relatively controlled processes, such as normative concerns, remains unclear. Given that lay assumptions, meanings, and social consequences associated with mental illness may vary across Asian and Western cultures, we predict that cultural variations in automatic evaluations of mental illness will be observed even when the influence of controlled processes and normative concerns on evaluations is minimized.
Method
Participants
Forty Caucasian American (CA) undergraduate students (20 females; M age = 18.90, SD = 0.78) and 40 Asian American (AA) students (25 females; 20 Chinese, 19 Korean, 1 multiracial Chinese-Korean; M age = 18.75, SD = 1.17) participated for course credit. Among the AA participants, 24 were born in the United States, and 16 were born in either China or Korea. The AA participants were fluent English speakers, and all instructions and materials were presented in English. All participants gave informed consent prior to participation.
Materials and Measures
Participants first completed a practice categorization task that involved categorizing only physical illness (PI) words (e.g., cancer, smallpox) and mental illness (MI) words (e.g., depression, schizophrenia) into their respective categories. In the PI block, participants were told to press the space bar only when they saw a word that reflected a physical illness and make no responses to words that reflected mental illnesses. The MI block consisted of the same procedure, but with MI words as targets (pressing space bar) and PI words as distracters (making no response). Each block consisted of 30 trials. This practice task served two functions: (1) It allowed participants to get accustomed to the response style they would be using later in the Go/No-Go Association Task, and (2) it allowed tests for baseline cultural differences in the mere identification and categorization of mental and physical illnesses.
The Go/No-Go Association Task (GNAT; Nosek & Banaji, 2001) was utilized to measure implicit attitudes toward mental illness (MI). The GNAT is conceptually similar to the widely used Implicit Association Test (IAT; Greenwald, Nosek, & Banaji, 2003). While the IAT measures implicit biases toward one category relative to another opposing category, the GNAT functions as a single-category implicit attitude measure, reflecting biases toward a specific category in a manner that is less dependent upon the level of bias toward another category.
The GNAT requires the participants to categorize words into corresponding superordinate categories by making or inhibiting a response. All words were presented in English. In the “MI+good” block, participants were instructed to press the space bar in response to words representing mental illness or positively valenced words (e.g., good, wonderful), while inhibiting responses to physical illness words and negatively valenced words (e.g., awful, unpleasant). Likewise, in the “MI+bad” block, participants responded to words representing mental illness or negative words, while inhibiting responses to distracters (physical illness words and positive words). To assess whether cultural differences in implicit biases are specific to mental illness or broadly reflects more general cultural variations in biases toward illness, participants also completed a physical illness (PI) GNAT task, which was similar to the MI GNAT, but utilized physical illness words as targets and mental illness words as distracters across the two blocks. The MI and PI words used in the GNAT were the same as the words used in the MI and PI baseline practice tasks.
Each of the four GNAT blocks (MI+good, MI+bad, PI+good, PI+bad) were presented in a randomized order. Each block consisted of 16 practice trials followed by 40 critical trials. Practice trials had a response deadline of 1,000 ms and the critical trials of each GNAT block had a response deadline of 700 ms. A relatively short response window was employed to elicit greater automaticity from participants’ responses and to limit the influence of deliberation. Error feedback was provided during the first 100 ms of a 150 ms interstimulus interval with an “O” or an “X” to indicate correct and incorrect responses, respectively.
The GNAT data were scored according to the improved IAT scoring algorithm (Greenwald et al., 2003), which has also been used for scoring GNAT data measuring response latency (Raganath, Smith, & Nosek, 2008). A GNAT D score, which serves as a measure of implicit bias, was calculated for mental and physical illness by computing the difference in mean RT between the GNAT blocks for each concept (e.g., MI+bad minus MI+good) and dividing this value by the standard deviation of the RT across the two blocks. The GNAT D scores were calculated so that negative values represent negative implicit biases, while positive values represent positive implicit biases.
The Social Distance Scale (SDS; Link, Cullen, Frank, & Wozniak, 1987) was also administered as a measure of explicit attitudes toward mental illness. The SDS is a five-item scale that assesses the participant’s willingness to engage in interactions of increasing intimacy with a person with a mental illness (e.g., “Live next door to someone with a mental illness,” “Have a person with a mental illness marry into the family”). Each item was rated on a 4-point scale anchored from definitely willing to definitely unwilling. For each participant, responses for items were averaged, with higher scores reflecting greater overall unwillingness to engage in social contact/relationships with people with mental illness.
Results
There were no significant differences between the CA and AA group in reaction times and error rates for the MI and PI baseline practice tasks (all ps > 0.10), suggesting no differences between the cultural groups in which words they considered to be a physical or mental illness or their familiarity/understanding of the words.
Comparison of GNAT D for mental illness between the two groups revealed that the AA group (M = −0.08, SD = 0.23) exhibited significantly stronger biases toward mental illness relative to the CA group (M = 0.08, SD = 0.45), t(78) = 2.06, p = 0.04, d = 0.45. The two groups did not significantly differ in their implicit biases toward physical illness (CA: M = −0.03, SD = 0.41; AA: M = 0.01, SD = 0.34) (p > 0.10) (Figure 1).
Figure 1.
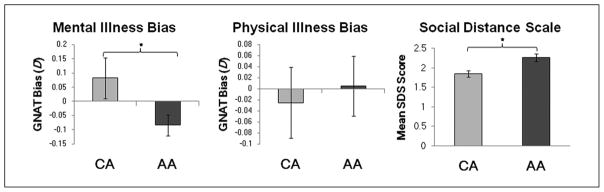
Implicit Attitude Biases Toward Mental and Physical Illnesses and Explicitly Endorsed Social Distance From People With Mental Illness Among Caucasian American and Asian American Participants
Note: Positive D scores represent positive biases toward the target category. Greater SDS scores represent greater desire for social distance from a person with mental illness (maximum score of 4). Asterisks indicate significance at p < 0.05 level.
To determine whether each group’s implicit attitudes were significantly biased, one-sample t tests against zero were conducted on each group’s GNAT D scores for physical and mental illness. For both groups, implicit biases toward physical illness did not significantly differ from zero (all ps > 0.10). Conversely, implicit biases toward mental illness were significantly lower than zero for only the AA group, t(39) = −2.25, p = 0.03, but not the CA group (p > 0.10).
Replicating prior cultural comparisons, on the SDS (CA: a = .82; AA: a = .85), AAs (M = 2.27, SD = 0.61) endorsed significantly greater desire for social distance than CAs (M = 1.86, SD = 0.52) from people with mental illness, t(78) = −3.28, p = 0.001, d = 0.72 (Figure 1). The SDS was not correlated with MI GNAT D scores for the overall sample, r(78) = −0.09, p > 0.10, nor within groups [CA: r(38) = −0.15, p > 0.10; AA: r(38) = 0.21, p > 0.10].
Discussion
Here we demonstrate for the first time that Asian Americans show stronger implicit mental illness stigma compared to Caucasian Americans. Importantly, cultural variations in implicit stigma appear to be unique for mental illness, rather than for stigma of illnesses more generally. Our findings suggest that cultural variations in mental illness stigma may arise from cultural variations in automatic affective reactions to mental illness. Cultural differences in deliberate concerns about the appropriateness of one’s immediate reactions to mental illness may not be necessary to produce cultural variations in mental illness stigma, though these concerns may modify how automatic reactions toward mental illness are expressed. Cultural variations in automatic affective reactions toward mental illness suggest that cultural differences in the meanings or assumptions associated with mental illness may underlie cultural variations in stigma.
In East Asian cultures, shame from mental illness undermines one’s perceived ability to fulfill social obligations and accrue social capital or “face,” which are central cultural values, leading to emotions of anxiety and dread linked to mental illness (Yang, 2007). Those of Asian cultural backgrounds are also more likely to associate danger and mistrust with mental illness (Abdullah & Brown, 2011; Furnham & Chan, 2004) and as a result may experience more spontaneous affective reactions associated with anxiety, fear, or threat when encountering representations of mental illness. Future studies comparing cultural variations in implicit stigmatizing attitudes would benefit from examining the relationship between specific cultural lay beliefs about mental illness and the automatic affective reactions elicited toward mental illness.
Acknowledgments
We thank G. Bebko, G. Bodenhausen, D. Bridge, V. Mathur, and J. Richeson for helpful discussion. We also thank C. Alvia-Ramos and Z. Chen for their help with data collection.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by NSF BCS-0720312 and NSF BCS-0722326 grants to J.Y.C., and Institute of Education Science Grant R305B080027 to Northwestern University.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms: An integrative review. Clinical Psychology Review. 2011;31:934–948. doi: 10.1016/j.cpr.2011.05.003. [DOI] [PubMed] [Google Scholar]
- Furnham A, Chan E. Lay theories of schizophrenia: A cross-cultural comparison of British and Hong Kong Chinese attitudes, attributions and beliefs. Social Psychiatry and Psychiatric Epidemiology. 2004;39:543–552. doi: 10.1007/s00127-004-0787-8. [DOI] [PubMed] [Google Scholar]
- Gawronski B, Bodenhausen GV. Unraveling the processes underlying evaluation: Attitudes from the perspective of the APE Model. Social Cognition. 2007;25:687–717. [Google Scholar]
- Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology. 2003;85:197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Frank J, Wozniak JF. Social rejection of former mental patients: Why labels matter. American Journal of Sociology. 1987;92:1461–1500. [Google Scholar]
- Nosek BA, Banaji MR. The Go/No-Go Association Task. Social Cognition. 2001;19:625–664. [Google Scholar]
- Raganath KA, Smith CT, Nosek BA. Distinguishing automatic and controlled components of attitudes from direct and indirect measurement methods. Journal of Experimental Social Psychology. 2008;44:386–396. doi: 10.1016/j.jesp.2006.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao D, Feinglass J, Corrigan P. Racial and ethnic disparities in mental illness stigma. Journal of Nervous and Mental Disease. 2007;195:1020–1023. doi: 10.1097/NMD.0b013e31815c046e. [DOI] [PubMed] [Google Scholar]
- Reeder GD, Pryor JB. Dual psychological processes underlying public stigma and the implications for reducing stigma. Mens Sana Monographs. 2008;6:175–186. doi: 10.4103/0973-1229.36546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusch N, Corrigan PW, Todd AR, Bodenhausen GV. Implicit self-stigma in people with mental illness. Journal of Nervous and Mental Disease. 2010;198:150–153. doi: 10.1097/NMD.0b013e3181cc43b5. [DOI] [PubMed] [Google Scholar]
- Strack F, Deutsch R. Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review. 2004;8:220–247. doi: 10.1207/s15327957pspr0803_1. [DOI] [PubMed] [Google Scholar]
- Teachman BA, Wilson JG, Komarovskaya I. Implicit and explicit stigma of mental illness in diagnosed and healthy samples. Journal of Social and Clinical Psychology. 2006;25:75–95. [Google Scholar]
- Yang LH. Applications of mental illness stigma theory to Chinese societies: Synthesis and new directions. Singapore Medical Journal. 2007;48:977–985. [PubMed] [Google Scholar]


