Abstract
Introduction
Acetabular bone defect reconstruction is an increasing problem for surgeons with patients undergoing complex primary or revision total hip replacement surgery. Impaction bone grafting is one technique that has favourable long-term clinical outcome results for patients who undergo this reconstruction method for acetabular bone defects. Creating initial mechanical stability of the impaction bone graft in this technique is known to be the key factor in achieving a favourable implant survival rate. Different sizes of bone chips were used in this technique to investigate if the size of bone chips used affected initial mechanical stability of a reconstructed acetabulum.
Methodology
Twenty acetabular models were created in total. Five control models were created with a cemented cup in a normal acetabulum. Then five models in three different groups of bone chip size were constructed. The three groups had an acetabular protrusion defect reconstructed using either; 2–4 mm3, 10 mm3 or 20 mm3 bone chip size for impaction grafting reconstruction. The models underwent compression loading up to 9500 N and displacement within the acetabular model was measured indicating the initial mechanical stability.
Results
This study reveals that, although not statistically significant, the largest (20 mm3) bone chip size grafted models have an inferior maximum stiffness compared to the medium (10 mm3) bone chip size.
Interpretations
Our study suggests that 10 mm3 size of bone chips provide better initial mechanical stability compared to smaller or larger bone chips. We dismissed the previously held opinion that the biggest practically possible graft is best for acetabular bone graft impaction.
Keywords: Impaction bone graft, Acetabular model, Bone chip size
1. Introduction
Charnley first introduced primary hip replacement surgery in 1961.1 Since this time the aim in all joint replacement surgery is to achieve a stable implant fixation with excellent short and long-term outcome for the patient, whilst attempting to restore normal hip biomechanics and anatomy which are key to longevity of implant success. Controversy exists as to the best method of surgically restoring normal anatomy in correcting severe bony acetabular defects that can be found at both complex primary and revision total hip replacement surgery.
Bone impaction grafting is a surgical reconstruction method that aims to reconstitute the bone defects. Slooff et al first reported impaction grafting as a technique in 1984 to achieve a stable implant by impacting morselized bone graft and subsequently allowing living bone stock to be restored.2 This technique offers a biological repair to bone defects present at the time of surgery with long-term favourable clinical results.3–5 Bone impaction grafting raises many important issues for consideration from a mechanical and biological viewpoint to optimize the surgical outcome for patients who are subjected to this surgical technique.
The initial stability of the implant has been found to be the most important factor influencing graft healing and incorporation6–8 and therefore the overall outcome of this reconstructive technique. In studies of impaction grafting, a larger bone chip size has been identified as producing higher stability than a smaller chip size8,9 and the ideal bone chip size on the acetabulum has been suggested to be between 8 and 10 mm.3,8,10,11 However, it is not known if using the largest possible particle of bone chips size to reconstruct an acetabular defect would have a detrimental effect on the initial mechanical stability of the implanted component. Therefore the aim of this study was to use a laboratory model to investigate the initial mechanical stability of an acetabular component following impaction grafting with three different size of bone chip.
2. Materials and methodology
An acetabular model was developed using a synthetic bone compromising an E-glass-filled epoxy cylinder (74 mm diameter, 3 mm wall thickness, ∼55 mm length) filled with an open cellular rigid polyurethane foam (Sawbones Europe AB, Malmo, Sweden12). According to the manufacturer's data, the open cellular rigid polyurethane foam had a density of 20 pcf, cell size of 0.5–1 mm, compressive strength of 5.4 MPa and compressive modulus of 137 MPa and resembled the appearance of cadaveric cancellous bone.13 The cylinder was machined centrally with a 53 mm bull nosed spherical slot drill, to a depth of 26 mm for the control group and 46 mm for the protrusio models to allow impaction graft reconstruction. A total of 20 specimens were used, five for the control group and five for each of the three impaction grafting groups.
The control group were implanted with a 47 mm Charnley cup flanged LPW (DePuy International Ltd, Leeds, England) using bone cement prepared in vacuum mixing system (CMW1 and SmartMix, vacuum mixing bowl, DePuy International Ltd. T/A DePuy CMW, Blackpool, FY4 4QQ, England) as per manufacturer recommendations. The cement was then pressurised for 2 min with a 55 mm cement pressuriser (DePuy).
The acetabular cup was inserted at 5 min and pressurised until the cement had set.
2.1. Study groups of impaction grafting of acetabular protrusio defect
In order to manufacture the synthetic bone chips, the same open cellular rigid polyurethane foam as, described above, was machined into 3 different chips sizes as shown in Fig. 1. The chips in the largest (20 × 20 × 20 mm chip size) and medium (10 × 10 × 10 mm chip size) were all of uniform cube shape. The bone chips in the smallest group varied from a minimum of 2 × 2 × 2 mm to a maximum of 4 × 4 × 4 mm in shape. There was less uniformity in the shape of these chips due to the difficulties in machining small chips from the cellular rigid polyurethane foam.
Fig. 1.
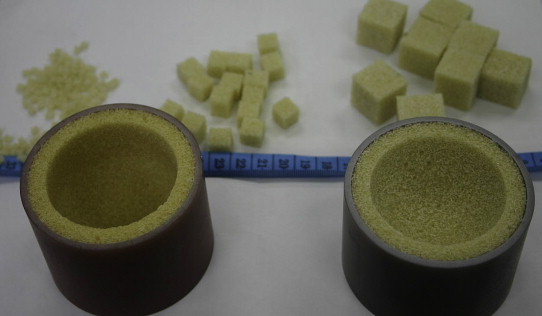
Two acetabular models with sawbone graft in background. The acetabular model on the right in the figure is from the control group with a 53 mm spherical central defect to 26 mm depth. The acetabular model on the left is taken prior to impaction grafting of the protrusio defect of depth 46 mm.
Five acetabular protrusio models for each graft chip size were reconstructed. Reconstruction was performed using serial acetabular packers (DePuy International Ltd, Leeds) and a hammer. The last impactor used in all models was 51 mm in diameter, to allow a 2 mm cement mantle. Impaction was stopped once the impaction head was flush with the acetabular rim leaving a stable impacted sawbone bed. Further hammer blows were unable to impact the graft to any extent.
The reconstructed acetabular models underwent cementation of an acetabular cup using the same method as the control group. All 20 models were then stored for 24 h in saline soaked gauze at 6°C to allow for complete cement polymerisation.13
All acetabular models were tested in a materials testing machine (Instron 3366 Materials Testing Machine – 10 kN, Instron, High, UK). The models were secured in an angled holder at 45° abduction and 0° anteversion as shown below in Fig. 2. The posterior lip of the LPW cup was positioned superiorly to standardise cup alignment within the loading set-up. A femoral head (22.225 mm) was mounted on a stem and attached to the moving crosshead of the Instron machine. The angled holder with a cup securely attached with headless pins was then loosely attached to the base plate of a testing machine. The angled holder was firmly attached to the base plate once the femoral head was centred within the acetabular cup prior to application of a compressive load.
Fig. 2.

Instron loading set-up with femoral head engagement in acetabulum.
The models were tested under compression up to a load of 9.5 kN at 20 ± 1 °C at a speed of 1 mm/min. The load and displacement were recorded and the maximum slope (N/mm) of resulting load-displacement curve was calculated.
3. Results
All 20 models tested up to the static load of 9.5 kN revealed no yield or visible damage.
Fig. 3, below reveals results of the load-displacement of the largest bone chip size grafted models group respectively under static loading. All force displacement graphs had an initial toe region before the femoral head had fully engaged with the acetabular cup, followed by a linear region. In all of the groups tested, some models were noted to have a change in gradient whilst be loaded.
Fig. 3.
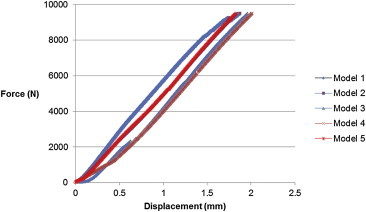
Largest graft models static loading graph (N/mm).
All groups had some models that experienced some change in stiffness during static loading as noted by a change in the gradient of the slope under static loading. This change of gradient was noted most commonly in the smallest and medium grafted models with at least three models in these groups undergoing a possible “settling of graft” effect. Only two models were noted to have an obvious change in gradient in the largest grafted group. Two models in the control group, however, were also noted to undergo a change in gradient on static loading which suggest that this effect may not be due to a graft settling effect on loading. One model in the smallest graft size group was only loaded to 8000 N due to a technical error with the materials testing machine.
3.1. Stiffness results from maximum slope
The maximum stiffness data is presented in the bar chart in Fig. 4. Both control group and medium graft impaction size were found to have superior stiffness on compression loading compared to the largest and smallest graft impaction models but this superior stiffness was not statistically significant.
Fig. 4.
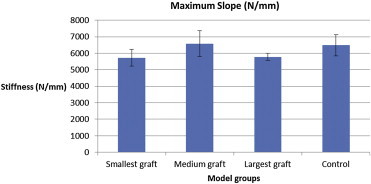
Maximum slope from static compressive extensive loading. The bar extensions represent the confidence intervals of 95% for each group.
Further statistical analysis of the stiffness of the four different model groups was performed with analysis of variance (ANOVA) tests. This enabled comparison between the four groups and a p-value of 0.060 was found with no significant difference between the groups.
4. Results summary
In total 20 specimens were successfully tested in four groups (control, smallest graft size (2–4 mm3), medium graft size (10 mm3) and largest graft size (20 mm3)). The results of the stiffness measurements show a trend to towards medium (10 mm3) graft size improving stiffness of the reconstructed acetabular model, however, no significant difference was found between any of the three graft size models and control group for the maximum slope measurements.
5. Discussion
5.1. Static compression
Initial cup stability is the key to longevity in acetabular reconstructions using impacted bone graft.14 This study revealed no yield on static compression loading up to 9500 N in any model reconstructed using impacted graft of three different sizes of bone chip. The bone chips were made out of Polyurethane Foam. This material has been shown on biomechanical testing and simulation to have similar microstructure and material properties to cancellous bone.15
The compression load of 9500 N is over three times higher than the level experienced clinically of 300% body weight on climbing stairs, equivalent of roughly 3000 N in a 100 kg patient.16 It is also significantly above the maximum load experienced through the hip joint which can be eight times body weight equivalent of roughly 8000 N in a 100 kg patient. This finding promotes this technique as having excellent initial stability in its use for reconstructing contained acetabular defects.
On static compression loading, the maximum stiffness was calculated to illustrate that medium bone chip size (10 mm3) had superior mean maximum stiffness of 6586 (N/mm) compared to smallest (2–4 mm3) and largest bone chip size (20 mm3), with a mean maximum stiffness of 5729 and 5778 (N/mm) respectively. The medium bone chip size even had a marginally superior mean maximum stiffness compared to the control group where no acetabular cavity was present requiring reconstruction. A p-value of 0.06 was found, highlighting a trend towards a difference between the smallest and medium bone chip size reconstructed acetabular models on maximal stiffness. Although this trend was noted no statistical difference was noted between the 3 different graft size groups and the control group with a confidence interval of 95%.
The mean maximum stiffness results from this study would suggest that although no statistical difference could be found between the different bone chip sizes that the medium (10 mm3) chip size had the best mean maximal stiffness supporting previous studies that have also found this to be the best bone chip size for acetabular reconstruction on mechanical testing.8–11 This study indicates that using the largest available bone chips does not necessarily produce the best results, which contradicts earlier findings previously reported when commenting on bone chip size for acetabular reconstruction.8,9 Arts and Bolder comment that the biggest practical bone size should be used for acetabular reconstruction. Our study revealed the largest chip size (20 mm3) to have an inferior mean maximal stiffness although not statistically different compared to the smaller chip size of medium (10 mm3). Possible reasons for these findings are that although it was possible practically to impact the largest chip bone size within the contained acetabular defect each new bone chip had to be added in individually due to their size. With the medium sized bone chips, it was possible to impact several new bone chips of the medium bone chip size simultaneously thus creating a more stable impacted bone chip construct with superior inter-digitation between the bone chips. The chips in the largest size group were each compacted on their own before a further chip could be added.
Ideally the acetabular models would have undergone cyclical testing, although our biomechanical department did not have these facilities available, as performed in similar mechanical stability bone impaction graft testing research.8,9,12,17–20 This would have allowed a comparison to be made between the initial mechanical stability results in this study and their findings, whilst also possibly demonstrating a statistically significant difference between the different bone chip size groups at a level of confidence interval of 95%.
It should be noted that the largest group (20 mm3) had very small standard deviations. This effect can also be seen on the load-displacement curves (Fig. 3) for the largest graft size models. No ‘settling’ effect was seen in this group and this may be due to the higher number of impactions that were required to construct these models. Another possible explanation for these consistent results under compressive loading could be due to the surgical technique that had to be performed when constructing these models that involved a one-by-one method due to size of the bone chips rather to the two other bone chip groups whereby several bone chips could be impacted at one time to create a stable construct.
The load-displacement graphs exhibited some initial ‘toe-region’ due to displacement necessary for the femoral head to become centred within the acetabular cup to allow force to be applied to the acetabular models. To allow comparison between the models this region was removed and not included in the analysis.
A change in the stiffness under static compressive loading – i.e. a change of gradient could have been due to the graft settling within the reconstruction. The control group had no reconstruction, however, and it also underwent a change in stiffness under compressive loading. This would suggest that the change in stiffness may have been due to movement/failure within the angled acetabular holding device rather than a graft settling effect. Future dial testing could be used to reveal if there was movement within the angled holder itself or if the change in gradient of stiffness is only due to movement within the acetabular model.
The study also aimed to address, research and reveal the ideal bone chip size to be used for acetabular defect reconstruction in the context of previous findings.9–11 Our study would suggest that 10 mm3 bone chip size should be used, supporting earlier findings.8 The results of this study reveal that, although not statistically significant, the largest (20 mm3) bone chip size grafted models have an inferior maximum stiffness compared to the medium (10 mm3) bone chip size. Our findings challenge the previously held opinion that the best initial stability would be gained by impacting the biggest surgically possible bone chip size into an acetabular defect although we should not forget that these findings were present in an in vitro model i.e. Sawbone and further in vitro and in vivo work is required prior to formal acceptance of the ideal bone chip size in clinical practice.
Author's contributions
CSH, main author, planning, design and investigator of published results.
PBB, planning, design and revision of manuscript.
RKW, planning, design, interpretation of the results and revision of manuscript.
ZJ, planning, design, interpretation of the results and revision of manuscript.
Conflicts of interest
All authors have none to declare.
Acknowledgements
Technical support: Phil Wood and staff, iMBE Laboratory Manager in Mechanical Engineering department, University of Leeds. Depuy Orthopaedics International: Donation of Acetabular cup and bone cement. Financial support: Leeds Teaching Hospitals Charitable Trust fund for research grant.
References
- 1.Charnley J. Arthroplasty of the Hip. A new operation. Lancet. 1961;1:1119–1132. doi: 10.1016/s0140-6736(61)92063-3. [DOI] [PubMed] [Google Scholar]
- 2.Slooff T.J.J.H., Huiskes R., Van Horn J., Lemmens A.J. Bone grafting in total hip replacement for acetabular protrusion. Acta Orthop Scand. 1984;55:593–596. doi: 10.3109/17453678408992402. [DOI] [PubMed] [Google Scholar]
- 3.Schreurs B.W., Busch V.J., Welton M.L., Verdonschot N., Slooff T.J., Gardeniers J.W. Acetabular reconstruction with impaction bone-grafting and a cemented cup in patients younger than fifty years old. J Bone Joint Surg Am. 2004;86A:2385–2392. doi: 10.2106/00004623-200411000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Schreurs B.W., Bolder S.B., Gardeniers J.W., Verdonschot N., Slooff T.J., Veth R.P. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented cup. A 15- to 20-year follow-up. J Bone Joint Surg Br. 2004;86B:492–497. [PubMed] [Google Scholar]
- 5.Lie S.A., Havelin L.I., Furnes O.N., Engesaeter L.B., Vollset S.E. Failure rates for 4762 revision total hip arthroplasties in the Norwegian Arthroplasty Register. J Bone Joint Surg Br. 2004;86B:504–509. [PubMed] [Google Scholar]
- 6.Karrholm J., Hultmark P., Carlsson L., Malchau H. Subsidence of a non-polished stem in revisions of the hip using impaction grafting. Evaluation with radiostereometry and dual-energy X-ray absorptiometry. J Bone Joint Surg Br. 1999;81B:135–142. doi: 10.1302/0301-620x.81b1.8922. [DOI] [PubMed] [Google Scholar]
- 7.Ling R.S. Femoral component revision using impacted morsellised cancellous graft. J Bone Joint Surg Br. 1997;79B:874–875. doi: 10.1302/0301-620x.79b5.8078. [DOI] [PubMed] [Google Scholar]
- 8.Arts J.J., Verndonschot N., Buma P., Scheurs B.W. Larger bone graft size and washing of bone grafts prior to impaction enhances the initial stability of cemented cups. Acta Orthop. 2006;77:227–233. doi: 10.1080/17453670610045957. [DOI] [PubMed] [Google Scholar]
- 9.Bolder S.B.T., Schruers B.W., Verdonschot N., Van Unen J.M., Gardeniers J.W.M., Slooff T.J.J.H. Particle size of bone graft and method of impaction affect initial stability of cemented cups. Human cadaveric and synthetic pelvic specimen studies. Acta Orthop Scand. 2003;74:652–657. doi: 10.1080/00016470310018144. [DOI] [PubMed] [Google Scholar]
- 10.Giesen E.B.W., Lamerigts N.M.P., Verdonschott N., Schreurs B.W., Huiskes R. Mechanical characteristics of impacted morsellised bone grafts used in revision of total hip arthroplasty. J Bone Joint Surg Br. 1999;81B:1052–1057. doi: 10.1302/0301-620x.81b6.8742. [DOI] [PubMed] [Google Scholar]
- 11.Ullmark G. Bigger size and defatting of bone chips will increase cup stability. Arch Orthop Trauma Surg. 2000;120:445–447. doi: 10.1007/s004029900122. [DOI] [PubMed] [Google Scholar]
- 12.ISO 5833 . ISO; Geneva: 2002. Implants for Surgery – Acrylic Resin Cements.http://www.sawbones.com/products/bio/testblocks/celluar.aspx [Google Scholar]
- 13.Bolder S.B.T., Verdonschot N., Schreurs B.W. Technical factors affecting cup stability in bone impaction grafting. Proc Inst Mech Eng H. 2007;221:81–86. doi: 10.1243/09544119JEIM245. [DOI] [PubMed] [Google Scholar]
- 14.Brewster N., Gillespie W., Howie C., Madabhushi S., Usmani A., Fairburn D. Mechanical considerations in impaction bone grafting. J Bone Joint Surg Br. 1999;81B:118–124. doi: 10.1302/0301-620x.81b1.8480. [DOI] [PubMed] [Google Scholar]
- 15.Shim V., Boheme J., Josten C., Anderson I. InTech; 2012. Use of Polyurethan Foam in Orthopaedic Biomechanical Experimentation and Stimulation; pp. 171–200. Chapter 9. [Google Scholar]
- 16.Bergmann G., Deuretzbacher G., Helle M. Hip contact forces and gait pattern from routine activities. J Biomech. 2001;34:859–871. doi: 10.1016/s0021-9290(01)00040-9. [DOI] [PubMed] [Google Scholar]
- 17.Bolder S.B.T., Verdonschot N., Schreurs B.W., Buma P. The initial stability of cemented acetabular cups can be augmented by mixing morselised bone grafts with tricalcium phosphate/hydroxyapatite particles in bone impaction grafting. J Arthroplasty. 2003;18:1056–1063. doi: 10.1016/s0883-5403(03)00408-x. [DOI] [PubMed] [Google Scholar]
- 18.Arts J.J., Gardeniers J.W., Welten M.C., Verdonschott N., Schruers B.W., Buma P. No negative effects of bone impaction grafting with bone and ceramic mixtures. Clin Orthop Rel Res. 2005;438:239–247. doi: 10.1097/01.blo.0000169081.61398.58. [DOI] [PubMed] [Google Scholar]
- 19.Arts J.J.C., Schreurs B.W., Buma P., Verdonschot N. Cemented cup stability during lever-out testing after acetabular bone impaction grafting with bone graft substitutes mixes containing morselized cancellous bone and tricalcium phosphate-hydroxyapatite granules. Proc Inst Mech Eng H. 2005;219:257–263. doi: 10.1243/095441105X34266. [DOI] [PubMed] [Google Scholar]
- 20.Bolder S.B.T., Verdonschot N., Schreurs B.W., Buma P. Acetabular defect reconstruction with impacted morselized bone grafts or TCP/HA particles. Biomaterials. 2002;23:659–666. doi: 10.1016/s0142-9612(01)00153-3. [DOI] [PubMed] [Google Scholar]


