Abstract
Background
Vast majority of spine fractures in thoracolumbar region are unstable and often associated with neurological deficit. With the advancement of technology, these fractures are now more often managed operatively. The present study aimed at evaluating the role of open reduction & internal fixation using pedicle screws and short segment fixation in patients with Thoracic and Lumbar spine fractures.
Design
In this prospective study, 25 patients in age group of 15–65 years (mean age 28.25 years) with thoracolumbar fractures with associated neurological deficit or compression fractures with loss of more than 50% vertebral height or angulations more than 20° with or without neurological deficit were included. The results were evaluated based on restoration and maintenance of vertebral body height, spinal lordosis/kyphosis and evaluation of the neurological recovery which was done at regular intervals using Frankel's grading.
Results
The mean follow-up period was 20.3 months. The average preoperative kyphotic angle as measured by Cobbs method was 20° which improved to 7.8° following instrumentation. The average preoperative vertebral height was 58.65% which improved to 78.55% postoperatively. Preoperatively, only 20% of patients had useful paraplegia (Frankel grade D and E) while 80% had useless paraplegia (Frankel's grade C and below). Following surgery, 60% patients had useful paraplegia while 40% had useless paraplegia.
Conclusion
Short segment trans-pedicle posterior fixation is helpful for not only stabilization of the fractures and restoration of anatomy, but also maintaining the same over a period with good functional outcome.
Keywords: Thoracolumbar fracture, Posterior short segment fixation, Trans-pedicle screw
1. Introduction
Fractures and dislocations of the spine are serious injuries that commonly occur in young people. The treatment of unstable fractures and fracture-dislocations of the thoracic and lumbar spine has long been controversial. Reports about high complication rates after thoracolumbar stabilization compared to successful treatment of thoracolumbar fractures with bracing and early mobilization as well as reports of spinal remodelling had led to a renaissance of conservative treatment. Contrary to these opinions, there are many authors who favour immediate stabilization of the injured spine and a direct decompression of the spinal cord because it allows better nursing care and early mobilization and evidently shortens the time of stay in the hospital.1 Furthermore, there is strong experimental and clinical evidence that early operative reduction, decompression of the spinal cord and stabilization of the injured spine, is an effective method of ensuring the optimal environment for neurological recovery.2−4
For the last 2–3 decades, with the advent of newer techniques, aids and better surgical skill, operative management in the form of decompression and internal fixation has become main mode of treatment in spinal injuries as it reduces hospital stay, provides lasting stability, achieves proper reduction of fracture and many times improves the neurological status of the patients.
The main goals of surgical treatment are to achieve reduction, stability, and early painless mobilization and to provide a reasonable chance of neurological recovery. Anterior stabilization has the advantage that it is more effective for restoration of neurological function and does not need laminectomy, which leads to progression of deformity and neurological injury.5 Posterior spinal fixation system has the advantage of using less extensive approach with less blood loss and complications without compromising the quality of stabilization.5 Short internal fixation of the spine spares healthy mobile segments in fusion and thus preserves mobility.6
The aims of this study were to evaluate the role of open reduction & internal fixation in the management of Thoracic and Lumbar Fractures by short segment fixation and assess postoperative results by performing objective evaluation of patients.
2. Materials and methods
This prospective study of twenty-five patients with thoracolumbar spinal trauma was conducted at our institute between March 2005 and June 2007.
All the patients, with thoracolumbar spinal trauma with associated neurological deficit were included. Patients of compression fractures with loss of more than 50% vertebral height with or without neurological deficit or fractures with angulation of more than 20° were included in the study.
Initial resuscitation of the patient was done in the emergency department. Patients were carefully examined regarding head injury signs and other associated injuries. After properly resuscitating the patient and giving them analgesics, detailed neurological examination was done. Sensory examination was done with pin pricks, cotton wisp and tuning fork, from head to toe to include all dermatomes. Perianal area was examined for any possible sensory sparing. Neurological grading was done using Frankel's scale. Complete motor system examination was performed to know the involvement of myotomes. Reflexes were examined meticulously. Anal tone, anal wink and bulbocavernosus reflexes were elicited to know about the type of cord lesion.
Anteroposterior and lateral radiographs of involved spine were taken in the presence of a doctor and the exact level of the injury was ascertained. The fracture was classified according to Dennis Classification. But unlike Dennis classification, which is based on CT scan, we in addition to X-rays employed MRI scan of the patient to have a better idea of the injuries to the spinal cord.
Postural turning every 2 h, passive mobilization of all joints and chest physiotherapy were started. Air mattress was used for the patients to prevent bed sores. Adequate hydration and nutrition of the patient was taken care of. Night splints were used to prevent deformities. Regular bowel care with laxatives and enema was done. Need for surgery was explained to the patient and his/her relatives and informed consent was taken for surgery. After pre-anaesthetic check-up and obtaining clearance for anaesthesia, patient was posted for surgery.
2.1. Operative protocol
Intravenous antibiotic prophylaxis was routinely given to all the patients prior to surgery. After the administration of general anaesthesia the patient was placed in prone position. The spine was then exposed through a posterior midline incision. Laminotomy was carried out in all the patients. The facet joints and the transverse processes of the vertebrae were identified. The entry point for the pedicle was identified using these landmarks i.e. A horizontal line drawn from the middle of the transverse processes in the lumbar vertebrae or from the junction of upper one third and lower two third of the transverse process in lower dorsal vertebrae and a vertical line through the most prominent ridge on the corresponding superior facet. At the intersection of these two lines, cortical bone was nibbled. A “starter” was passed through this point via the pedicle into vertebral body. C-arm imaging was used for accurate placement of screw. The hole thus created was then tapped using an appropriate size cancellous bone tap and the pedicle screw was inserted. After placing the four screws, appropriate size rods were used with connecting rods. Distraction was done and locking nuts were tightened. The wound was thoroughly irrigated and closed over suction drains.
Patients were kept in postoperative recovery room for 24 h following surgery. Appropriate back-care, postural turning was started on the very first day. Detailed neurological examination was done postoperatively. Patient was shifted to the ward under doctor's supervision and appropriate plain radiographs were taken on the way to the ward. First postoperative dressing was done 48 h after surgery, drain was removed and suture line inspected. Adequate postoperative care was given. Sutures were removed around 12th day. Patients were made to sit with Taylor's brace on 10th–12th postoperative day except in cases with three column injury. Physical examination of the patient was done regularly to check for the presence of bed sores, upper respiratory tract infections or urinary tract infections. Where indicated urine samples were sent for culture and sensitivity and if positive the infection was managed accordingly. Regular physiotherapy and assisted mobilization was continued till the patient was discharged from the hospital. Another detailed neurological examination was done before discharge. Psycho-sociological guidance was given throughout the treatment and vocation guidance was given at the time of discharge depending on the patient's skill and ability.
After discharge from the hospital each patient was called for first follow-up at 4–6 weeks after operation and thereafter bimonthly follow-up was done. The patients were examined clinically, neurologically and radiologically at each follow-up and any complications of the procedure were noted [Figs. 1 and 2].
Fig. 1.
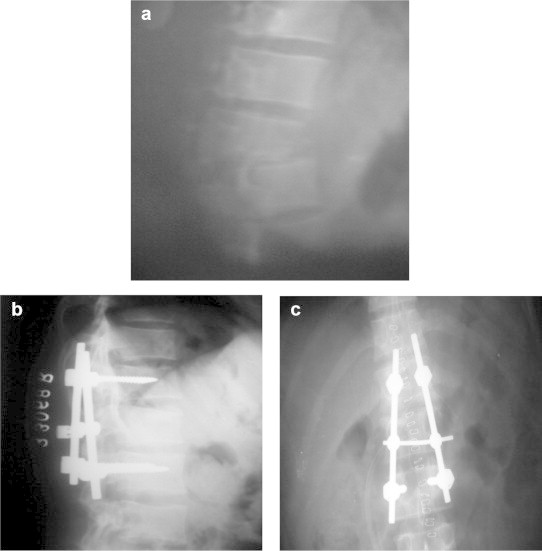
(a): Preoperative radiograph of a patient showing fracture dislocation. (b & c): Postoperative radiograph of the same patient showing reduction & fixation.
Fig. 2.
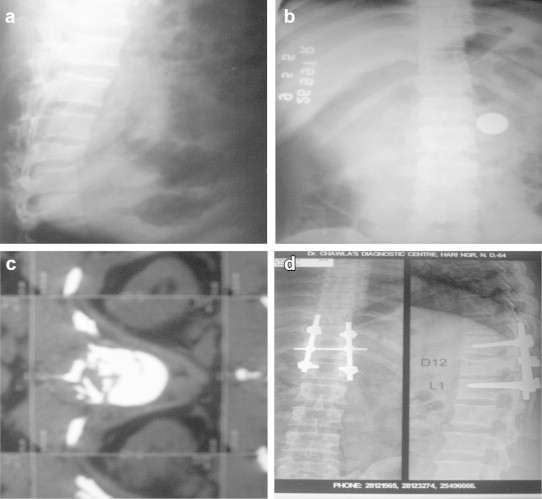
(a & b): Preoperative radiograph of another patient showing compressed fracture. (c): Preoperative MRI of the same patient showing bony fragments in the vertebral canal. (d) Postoperative radiograph showing reduction & stabilization (patient did not have any neurological recovery).
Results were assessed by following parameters
-
1.
Restoration and maintenance of vertebral body height.
-
2.
Restoration and maintenance of spinal lordosis/kyphosis.
-
3.
Evaluation of the neurological recovery at regular intervals by Frankel's grading.
-
4.
To look for any evidence of implant failure e.g. screws loosening, breakage/bending of plates etc.
-
5.
To look for any complications e.g. bed sores, urinary tract infection, respiratory tract infection or neurological deterioration.
3. Results
25 patients of unstable thoracolumbar fractures were operated by using posterior spinal fixation system during 2005–2007. Eighteen of the operated patients were males and remaining seven were females. Eighteen of the patients in the study were below 35 years of age [Table 1]. The most common modes of thoracolumbar fractures were fall from height (12 cases), road traffic accidents (8 cases) or weight falling on the back (5 cases). Seven patients had other associated injuries with bilateral fracture calcaneum being the commonest (3 cases). Out of twenty-five, 16 patients had a simple wedge compression fracture, 5 patients had burst fracture and 4 patients had fracture dislocation type of fracture. All fracture dislocation fractures were flexion rotation type.
Table 1.
Age & sex distribution of patients (n = 25).
| Age in years | Males | Females | Total |
|---|---|---|---|
| 16–25 | 10 | 1 | 11 |
| 26–35 | 5 | 2 | 7 |
| 36–45 | 3 | 2 | 5 |
| 46–55 | 1 | 1 | 2 |
| Total | 19 | 6 | 25 |
18 patients were operated upon within 48 h to 3 weeks of sustaining injury. Mean period of hospital stay was 34 days. Majority of patients (18 cases) sustained a fracture at D12–l1 level. One patient had fracture of D9, one had fracture of D10, two had Fracture of D11, two had fracture of L2 and one patient had fracture of L3 vertebra. The average preoperative kyphotic angle as measured by Cobbs method was 20° which improved to 7.8° following instrumentation. The average preoperative vertebral height was 58.65% which improved to 78.55% postoperatively. At final follow-up, there was a slight gain of Kyphotic angle and loss of vertebral height suggestive of insignificant increase of deformity compared to immediate postoperative period [Table 2].
Table 2.
Radiological assessment of fractures.
| Radiological parameters | Preoperative | Postoperative | At final follow-up |
|---|---|---|---|
| Average kyphotic angle | 20° | 7.8° | 8.9° |
| Average vertebral height | 58.65% | 78.55% | 76.05% |
Preoperatively, out of the twenty-five patients, 5 patients had useful paraplegia (Frankel grade D and E) and 20 patients had useless paraplegia (Frankel grade C, B and A). At the end of follow-up period of average 20.3 months (Ranging from 16 to 26 months) after surgery, 15 patients had useful paraplegia while 10 had useless paraplegia [Table 3 ]. On final follow-up, we observed that 4 patients in Frankel's grade A did not show any improvement while two patients in Grade E maintained their neurological status. Incomplete deficit improved by at least one Frankel grade in 19 patients. None of the patients in our study had deterioration in neurological status.
Table 3.
Comparison of preoperative and final neurological outcome.
| Frankle grade | Pre-operative | Final follow-up |
|---|---|---|
| A (complete paralysis) | 9 | 4 |
| B (sensory function only below injury level) | 7 | 3 |
| C (incomplete motor function below injury level) | 4 | 3 |
| D (fair to good motor function below injury level) | 3 | 9 |
| E (normal function) | 2 | 6 |
Complications noted in the series were misplaced screws (3 cases), bed sores (4 patients), Urinary tract infection (5 cases) and superficial wound infection (1 patient).
4. Discussion
18 of the patients in the study were below 35 years of age. The mean age in the study was 28.25 years which is similar to that of quoted by Gertzbein et al7 (29.1 years), Howards et al8 (30.3 years) and Tezeren9 (33.4 years).
The commonest mode of injury in our study was a fall from height (12 cases) followed by road traffic accidents (8 cases). Those who accounted for spinal injury due to fall from height were mostly the labourers working in under construction buildings. Whereas in Western studies (Roy-Camille et al,10 Howards et al8) road traffic accident accounted for the majority of cases. Difference may be due to the differing lifestyles in our country as compared with the west. The incidence of associated injuries in our study was 28% as compared to 55% as reported by Roy-Camille10 probably due to the difference in the mode of injury. Three patients in our study had bilateral fracture calcaneum due to fall from height. Knop et al11 in his series also reported that fall from height to be the commonest cause of injury in his series (68%).
Twenty patients were operated upon within three weeks of sustaining the fracture (mean injury operational interval in our series was 16 days). No patient could be operated upon within 48 h of injury as most of patient presented late to the hospital after being referred from the periphery and lack of resources available to them for prompt surgical attention. Most of the patients (18 cases) in our study had a fracture at D12–L1 level. Fractures at the thoracolumbar region were also the commonest in the study conducted by Roy-Camille al (1986).10 Kaye and Nance (1990) attributed it to Maximum mobility at this region.12 Similar observations were noted by Knop11 who in his series found 6 fractures at D12 level & 30 at L1 level. So together they constituted 64.28%.
The average kyphotic angle preoperatively was 20°. Following surgery the average kyphotic angle was reduced from 20° to 7.8°. At final follow-up the average kyphotic angle was 8.9°. In our study 10 cases had a postoperative angulation of <5° which we consider excellent. Our cases had loss of correction of angulation at follow-up with a mean of 1.1°. Ebelke et al13 reported loss of correction of angulation of 4° in patients in whom anterior grafting was done and 8° loss of angulation in those where anterior grafting was not undertaken. The reasons for this variation in the result are because Ebelke et al13 dealt with burst fractures only whereas we had fracture-dislocations as well in our study. We used fourth generation screw and did not have any implant breakage leading to loss of reduction.
Vertebral height was measured and recorded preoperatively, immediate postoperatively and at one month follow-up. Average preoperative vertebral height was 58.65%, whereas average immediate postoperative vertebral height 78.55%. At final follow-up, the average vertebral height was 76.05%. The results obtained by Bernucci et al14 (1994) and Roy-Camille10 (1986) of near anatomical restoration must be viewed with the fact that they were able to operate the patients with a mean injury operation interval of 15 h as compared to 16 days in our study. This proves that the short segment posterior fixation is useful not only in restoring the vertebral height but also in maintaining it.
All patients who underwent surgery were assessed neurologically preoperatively, and then at regular intervals postoperatively. The neurological function of each patient at each of these examinations was graded by Frankel's classification. Preoperatively, only 5 of our patients had useful paraplegia (Frankel grade D and E) while 20 had useless paraplegia (Frankel's grade C and below). Following surgery, 15 patients had useful paraplegia while 10 had useless paraplegia. At final follow-up, we observed that 4 patients in Frankel's grade A did not improve. Incomplete deficit improved by at least one Frankel grade in 19 patients. None of the patients in our study had deterioration in neurological status. Two patients in Grade E maintained their neurological status. These results correspond with those of Steffee et al15 (1986), An et al16 (1991), Ebelke et al13 (1991) and Temple et al17 (1994). Kim et.al18 also reported very good results with posterior short segment fixation for unstable dorsalo-lumber fractures.
We attribute our results to over cautious approach in patients with incomplete or no neurological deficit, meticulous haemostasis to avoid haematoma formation, minimal interference with neural tissue to prevent cord oedema and guarded mobilization with orthotic support.
Though 19 of our patients with incomplete deficit improved by at least one Frankel grade, but it were difficult to assess whether the neurological recovery was related to any of the treatment variables or whether it reflected the natural tendency of incomplete cord and cauda equina lesions to improve.
The average hospitalization time was 34 days, shortest being 15 days and longest stay of 53 days as compared to 23 days of Edwards and Levine19 (1986) and 17 days of Aebi et.al20 The main reason for the longer hospital stay was due to preoperative complications such as urinary tract infection, bed sores, respiratory infection and hypertension with resultant delay in pre-anaesthetic clearance.
5. Conclusion
The purpose of treating vertebral fractures are to achieve early neurological restoration, overcome damage spinal segments anatomically and accomplish firm and stable fixation.21 Our study demonstrates that stabilization of spine using posterior short segment transpedicular fixation is safe, technically easy and effective. The anatomical restoration is good. It allows early mobilization, better nursing care and shortens the hospital stay. The decompression of spinal cord provides optimal environment for neurological recovery.
Conflicts of interest
All authors have none to declare.
References
- 1.Wood K., Buttermann G., Mehbod A. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003 May;85-A:773–781. doi: 10.2106/00004623-200305000-00001. Erratum in: J Bone Joint Surg Am. 2004 Jun; 86-A(6): 1283. [DOI] [PubMed] [Google Scholar]
- 2.Gaebler C., Maier R., Kukla C., Vecsei V. Long-term results of pedicle stabilized thoracolumbar fractures in relation to the neurological deficit. Injury. 1997 Nov–Dec;28:661–666. doi: 10.1016/s0020-1383(97)00151-4. [DOI] [PubMed] [Google Scholar]
- 3.Bradford D.S., McBride G.G. Surgical management of thoracolumbar spine fractures with incomplete neurological deficits. Clin Orthop. 1987;218:201–216. [PubMed] [Google Scholar]
- 4.McAfee P.C., Yuan H.A., Fredickson B.A. The value of computed tomography in thoracolumbar fractures. J Bone Joint Surg Am. 1983;65A:461–473. [PubMed] [Google Scholar]
- 5.Chadha M., Bahadur R. Steffee variable screw placement system in the management of unstable thoracolumbar fractures: a Third World experience. Injury. 1998;29:737–742. doi: 10.1016/s0020-1383(98)00173-9. [DOI] [PubMed] [Google Scholar]
- 6.Borissov Adar, Borissov Konstatin. Posterior instrumentation for spinal injuries and non-traumatic disorders. Report on surgical practice. East Cent Afr J Surg. 2006;Vol. 11:75–80. [Google Scholar]
- 7.Gertzbein S.D., Court-Brown C.M., Jacobs R.R. Decompression and circumferential stabilization of unstable spine fractures. Spine. 1988;13:892–895. doi: 10.1097/00007632-198808000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Howards A.N., Vaccaro A., Cotler J.M. Low lumbar burst fractures comparision among body cast, Harrington rod, Luque rod and steffee plate. Spine. 1991;16:440–444. [PubMed] [Google Scholar]
- 9.Tezeren G., Kuru I. Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005;18:485–488. doi: 10.1097/01.bsd.0000149874.61397.38. [DOI] [PubMed] [Google Scholar]
- 10.Roy-Camille R., Saillant G., Berteaux D., Salgado V. Osteosynthesis of thoracolumbar spine with metal plates screwed through the vertebral pedicles. Reconstr Surg Traumatol. 1976;15:2. [PubMed] [Google Scholar]
- 11.Knop Christian, Fabian H.F., Bastian L., Blauth M. Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine. Jan 2001;26:88–99. doi: 10.1097/00007632-200101010-00016. [DOI] [PubMed] [Google Scholar]
- 12.Kaye J.J., Nance E.P. Thoracic and lumber spine trauma. Radiol Clin North Am. 1990;28:361–377. [PubMed] [Google Scholar]
- 13.Ebelke D.K., Asher M.A., Neff J.R., Krake D.P. Survivorship analysis of VSP instrumentation in the treatment of thoracolumbar and lumbar burst fractures. Spine. 1991;16:428–492. [PubMed] [Google Scholar]
- 14.Bernucci C., Maiello M., Silvestro C. Delayed worsening of the surgical correction of angular and axial deformity consequent to burst fractures of the thoracolumbar spine. Surg Neurol. 1994;42:23–25. doi: 10.1016/0090-3019(94)90245-3. [DOI] [PubMed] [Google Scholar]
- 15.Steffee A.D., Biscup R.S., Sitowski D.J. Segmental spine plates with pedicle screw fixation: a new internal fixation device for disorders of lumbar and thoracolumbar spine. Clin Orthop. 1986;203:45–53. [PubMed] [Google Scholar]
- 16.An H.S., Vaccaro A.R., Cotler J.M., Lin S. Burst fractures of lower lumber spine: Comparison between body cast, Harrington rod, Luque rod and Steffee plate. Spine. 1991;16:440–444. [PubMed] [Google Scholar]
- 17.Temple H.T., Kruse R.W., Dam B.E. Lumbar and lumbosacral fusion using Steffee instrumentation. Spine. 1994;19:537–541. doi: 10.1097/00007632-199403000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Kim K.S., Oh S.H., Huh J.S., Noh J.S., Chung B.S. Dorsal short-segment fixation for unstable thoracolumbar junction fractures. J Korean Neurosurg Soc. 2006;40:249–255. [Google Scholar]
- 19.Edwards C.C., Levine A.M. Early rod sleeve stabilization of the inured thoracic and lumbar spine. Orthop Clin North Am. 1986;17:121–145. [PubMed] [Google Scholar]
- 20.Aebi M., Elter C.H.R., Kehl T. The internal skeletal fixation system. Clin Orthop. 1988;227:30–44. [PubMed] [Google Scholar]
- 21.Lee Y.S., Sung J.K. Long-term follow-up results of short segment posterior screw fixation for thoracolumbar burst fractures. J Korean Neurosurg Soc. 2005;37:416–421. [Google Scholar]


