Abstract
A 56-year-old male patient was admitted with an evolved inferior wall myocardial infarction (IWMI). Electrocardiogram (ECG) showed presence of ST elevation and T wave inversion in the inferior leads. ECG taken on the next day surprisingly showed features suggestive of acute high lateral wall myocardial infarction (LWMI), without features suggestive of re-infarction which was finally diagnosed to be an artefact due to lead reversal. Lead reversal between left arm and left leg can mimic as high LWMI in a case with IWMI and we should aware of this situation before misdiagnosing it as re-infarction.
Keywords: Lead reversal, Inferior wall MI, Lateral wall MI, Re-infarction
1. Introduction
Improper placement of recording electrodes on the skin can generate misleading patterns on the electrocardiogram (ECG).1 Most clinicians can recognize the most common lead reversal between right arm/left arm lead switch that imitates a non-sinus atrial rhythm with a high anterolateral myocardial infarction pattern, although many other errors are possible.2 Less common lead placement errors are often difficult to detect and demand a high index of suspicion.3
2. Case report
A 56-year-old male patient was admitted with an evolved inferior wall myocardial infarction (IWMI). Electrocardiogram (ECG) showed presence of ST elevation and T wave inversion in the inferior leads (Fig. 1). He was treated conservatively without thrombolysis. Echocardiography revealed presence of regional wall motion in the basal & mid inferior wall. He was admitted in the intensive coronary care unit (ICCU) for observation. ECG which was done on the next day, surprisingly showed features suggestive of acute high lateral wall myocardial infarction (LWMI) (Fig. 2), though the patient was comfortable without having any chest pain and was planned for being treated with fibrinolytic therapy in suspicion of a re-infraction. Echocardiography was repeated which showed features similar to the previous one. We then searched for lead reversal and found that the ECG changes were due to lead reversal between left arm and left leg. Coronary angiogram (CAG) was done later which also showed the obstructive lesion in the right coronary artery (RCA) (Fig. 3).
Fig. 1.
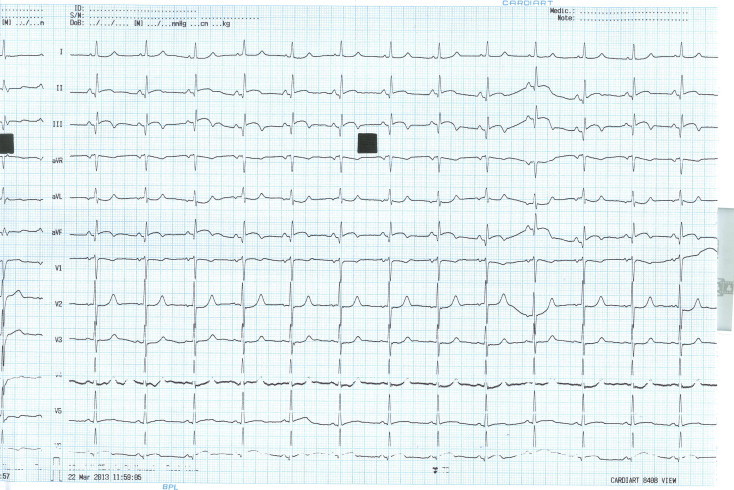
12 leads ECG showing features of evolved IWMI.
Fig. 2.
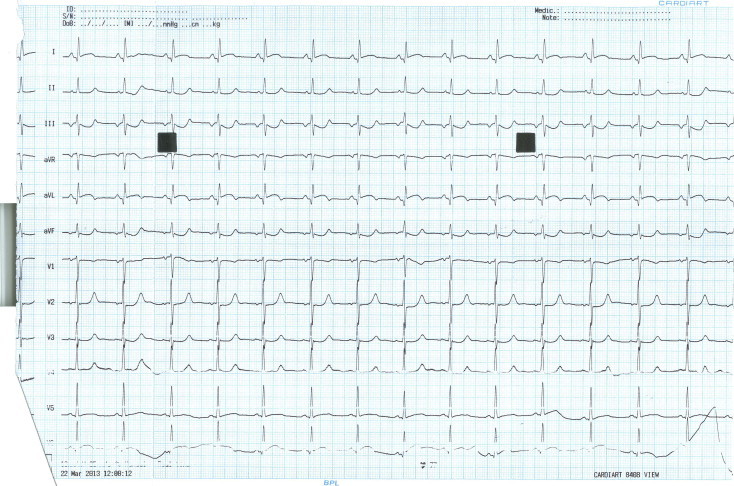
12 leads ECG showed ST elevation in lead I & aVL with ST depression in inferior leads after left arm–left leg lead reversal.
Fig. 3.
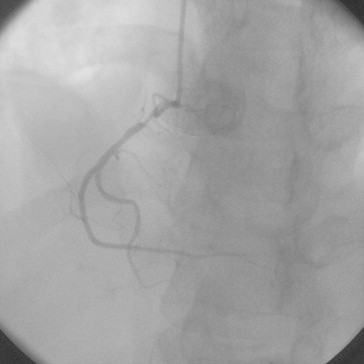
Coronary angiogram revealed the presence of 80% stenosis in the proximal RCA.
So, lead reversal between left arm and left leg can mimic as high LWMI in a case with IWMI and we should be aware of this situation before diagnosing it as re-infarction.
3. Discussion
The electrocardiographic error of left arm/left leg lead reversal is difficult to identify. Lead I amplitude greater than II as a terminal positive component may diagnose 90% of such errors.2 Exchanging the right arm and left leg leads creates what seems to be an inferior wall myocardial infarction and a non-sinus atrial rhythm in normal patients.1
But, in a case of IWMI, left arm/left leg lead reversal can mimic as an ECG of an acute lateral wall MI. This type of lead reversal may create confusion during treatment of acute coronary syndrome and can be misinterpreted as re-infarction while patients might be having no features suggestive of it. So, clinical judgement and high index of suspicion is most important in this scenario and we should keep in mind the changes in lead reversal in acute coronary syndrome situation. We must rule out the possibility of lead reversal before taking any further steps which might adversely affect the management.
Conflicts of interest
All authors have none to declare.
References
- 1.Peberdy M.A., Ornato J.P. Recognition of electrocardiographic lead misplacements. Am J Emerg Med. 1993;11:403–405. doi: 10.1016/0735-6757(93)90177-d. [DOI] [PubMed] [Google Scholar]
- 2.Heden B. Electrocardiographic lead reversal. Am J Cardiol. 2001;87:126–127. doi: 10.1016/s0002-9149(00)01465-x. [DOI] [PubMed] [Google Scholar]
- 3.Booker K.J., Holm K., Drew B.J., Ide B. Lead wire reversal during 12-lead EKG monitoring. Prog Cardiovasc Nurs. 2001;16:35–36. doi: 10.1111/j.0889-7204.2001.0990803.x. [DOI] [PubMed] [Google Scholar]


