Abstract
Background
Gestational exposure to famine has been associated with several chronic diseases in adulthood, but few studies in humans have related prenatal famine exposure to health-related quality of life. We used the circumstances of the Dutch Famine of 1944-1945 (during which official rations were =900 kcal/day for 24 weeks) to assess whether exposure to famine prior to conception or at specified stages of pregnancy was related to self-reported health-related quality of life and depressive symptoms in adulthood.
Methods
We studied 923 individuals including persons born in western Holland between January 1945 and March 1946, persons born in the same 3 institutions in 1943 and 1947 and same-sex siblings of persons in series 1 or 2. Between 2003 and 2005 (mean age 59 y), we assessed self-reported quality of life with the Short Form 36 questionnaire and derived mental and physical component scores. Depressive symptoms were assessed with the Center for Epidemiologic Studies Depression scale.
Results
Mean mental and physical component scores were 52.4 (SD = 9.4) and 48.9 (9.0), respectively. The mean depression score was 11.6 (7.4). Age-, sex- and schooling-adjusted estimates for mutually adjusted exposures were -2.48 for the mental component score with exposure before conception (95% confidence interval = -4.46 to 0.50) and 0.07 with exposure during pregnancy (-1.15 to 1.29). Adjusted estimates for the physical component score were 1.26 with exposure before conception (-0.67 to 3.19) and -0.73 with exposure during pregnancy (1.94 to 0.48). Adjusted estimates for the depression score were 2.07 with exposure before conception (0.60 to 3.54) and 0.96 with exposure during pregnancy (0.09 to 1.88). There was no evidence of heterogeneity of effects by specific periods of pregnancy exposed to famine.
Conclusions
A mother's exposure to famine prior to conception of her offspring was associated with lower self-reported measures of mental health and quality of life in her adult offspring.
Prenatal exposure to the Dutch Famine of 1944-1945 has been associated with increased prevalence of overweight,1 hypertension,2 and coronary heart disease.3 Maternal famine exposure around the time of conception has been related to prevalence of major affective disorders,4,5 antisocial personality disorders,6 schizophrenia,7-9 decreased intracranial volume,10 and congenital abnormalities of the central nervous system.11 Much of this research has focused on clinically diagnosed conditions, and little research has attempted to study the relation of less severe symptoms to this exposure.
One previous report suggested that “perceived health” was poorer among persons with gestational exposure to the Dutch famine.12 In that study, quality of life was assessed using a single question. Quality of life is a subjective evaluation that integrates demographic characteristics, medical conditions, and psychological constitution. The impact of prenatal famine exposure has not been studied using more comprehensive instruments to assess self-reported quality of life. We therefore evaluated the effect of famine exposure around the time of conception and during defined periods of gestation on self-reported quality of life and depressive symptoms with widely used instruments.
Methods
The Dutch famine occurred in a society with a well-developed administrative structure and adequate pre-famine nutrition. The famine was the result of a transport embargo on food supplies imposed by the German occupying forces in early October 1944. The severity and widespread nature of the famine have been fully documented.13,14 Nutrition in the Netherlands had generally been adequate up to October 1944.15 Official rations, which eventually consisted of little more than bread and potatoes, fell below 900 kcal per day by 26 November 1944, and were as low as 500 kcal per day by April 1945. The macronutrient composition of the ration remained relatively stable over this period, but the composition of non-ration foods changed, with a reduction in the intake of fat. The famine ceased with liberation in May 1945, after which Allied food supplies were rapidly distributed across the country. Dramatic effects of the famine have been documented on the course and outcome of pregnancy,16,17 as well as on fertility14 and follow-up studies have documented persistent consequences among the offspring.1-3, 18.
Study population
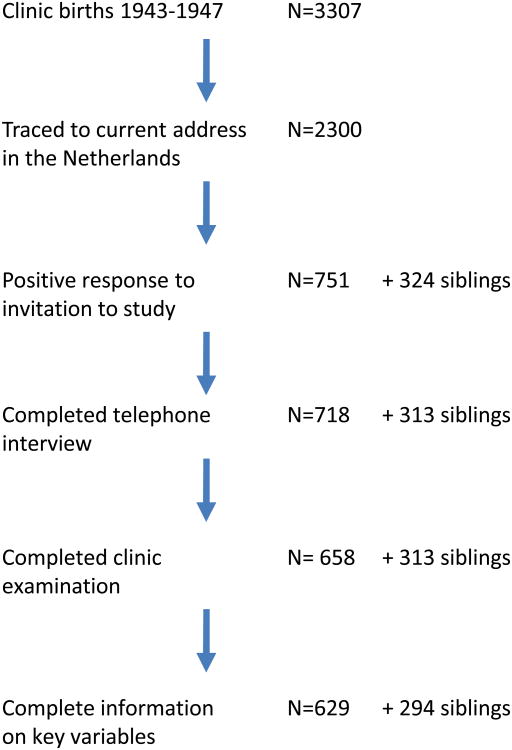
As described in more detail elsewhere,19 we identified 3307 live-born singleton births at three institutions in famine-exposed cities (the midwifery training schools in Amsterdam and Rotterdam and the university hospital in Leiden). We selected all 2417 births between 1 February 1945 and 31 March 1946 (infants whose mothers were exposed to the famine during or immediately preceding pregnancy) and a sample of 890 births in 1943 and 1947 as hospital time controls (infants whose mothers did not experience famine during this pregnancy). (See Figure for a flowchart) The sample of controls included an equal number of births for each month, allocated across the three institutions according to their size.
Names and addresses at birth for these 3307 infants were provided to the Population Register in the municipality of birth with a request for tracing to their current address. 308 (9%) were reported to have died in the Netherlands and 275 (8%) to have emigrated. The Population Registry in Rotterdam declined to trace 130 persons born out of wedlock, and for 294 subjects (9%) a current address could not be located. Address information was therefore obtained for 2300 persons (70% of the birth series).
A letter of invitation signed by the current director of the institution in which they were born was sent to these 2300 persons. We mailed one reminder letter to non-responders. Initially, our study design called for the recruitment of same-sex sibling pairs only, and the lack of an available sibling was a reason for ineligibility. We received some reply to 58% of the initial letters and to 44% of the reminder letters; 347 persons (20% of 1767 respondents) expressed willingness to participate, together with a sibling. None of the siblings was included in the hospital birth series. Among the 1415 who declined, 951 (67%) reported not having a same-sex sibling available for study. To increase the number of study subjects, we recontacted these 951 individuals, 381 of whom expressed willingness to participate. A higher positive response to our letters in women compared with men (36% vs. 29% overall) was consistent across all exposure categories.
We conducted telephone interviews (n=1031; 718 from the birth series and 313 siblings), followed by a clinical examination (n=971; 658 from the birth series and 313 siblings) at the Leiden University Medical Center in 2003-2005. All study protocols were approved by the Human Subjects Committees of all participating institutions. Study participants provided oral consent at the start of the telephone interview and written informed consent at the start of the clinical examination. The standardized telephone interview took approximately one hour. The clinical examination took approximately four hours. The study measures we report here were collected using self-administered paper-based questionnaires during the clinical visit.
Definitions of exposure to famine
We used the date of last menstrual period (LMP) as noted in the hospital records to define the start of gestation unless the LMP was missing or implausible (12%). In those cases we inferred the LMP date from relevant annotations on the birth record, or we estimated gestational age from birth weight and date of birth, using cut-points from tables of sex-, parity- and birth- weight-specific gestational ages from the combined birth records of the Amsterdam midwives school (1948-1957) and the University of Amsterdam Obstetrics Department (1931-1965).20 For each infant the most consistent and plausible estimate of gestation was selected and used together with date of birth to infer the LMP date.
We considered mothers with LMP between 1 February 1945 and 12 May 1945, who would have experienced an average of =900 kcal/d in the 10 weeks immediately preceding conception, to have preconceptional exposure. We characterized exposure to famine during gestation by determining the gestational ages (in weeks after the LMP) during which the mother was exposed to an official ration of =900 kcal/day between 26 November 1944, and 12 May 1945. We considered the mother exposed in gestational weeks 1-10, 11-20, 21-30, or 31-until delivery if these gestational time windows were entirely included in this period. Thus, pregnancies with LMPs between 26 November 1944, and 4 March 1945, were exposed in weeks 1-10; between 18 September 1944 and 24 December 1944 in weeks 11-20; between 10 July 1944, and 15 October 1944, in weeks 21-30; and between 2 May 1944 and 24 August 1944, in weeks 31 through delivery. By these definitions, a participant could have been exposed to famine during one or at most two adjacent 10-week periods. We considered individuals exposed in at least one of the 10-week periods to have been gestationally exposed.
Study outcomes
The Short-Form Health Survey
The Medical Outcomes Study 36-item Short-Form Health Survey is a widely evaluated generic patient-reported health outcome measure, developed in the United States in the 1980s.21,22 Numerous studies provide support for the underlying scale structure, reliability, psychometric quality, and validity in English. The survey has been translated and validated for the Dutch language.23 We used the standard version that utilizes a recall period of 4 weeks. The questionnaire is composed of 36 items, with 2-6 standardized response choices per item. It is organized into 8 scales: physical functioning, role limitations due to physical health problems, bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and general mental health. Scales were scored using standard procedures.24 Briefly, item responses were converted to a range of 0-100, with higher values representing better health. Scales were calculated by averaging the scores for the appropriate items unless fewer than 50% of the required items were available (=3% of the physical functioning scale and =1% of all other scales). We also derived two summary scores, namely a physical component score and a mental component score.24 By design, each summary score is standardized to a value of 50 for the general population of the United States, with a standard deviation of 10.
The Center for Epidemiologic Studies Depression instrument
We assessed depressive symptoms using the Center for Epidemiologic Studies Depression scale. This instrument has been widely used to assess depressive symptoms in the elderly. It has shown a good internal consistency and validity, and is relatively insensitive to physical disorders.25 The instrument has been translated into Dutch, and has been validated in Dutch elderly (55-85 years).25 There are20 questions with multiple-choice answers (score range 0-3) that are summed to arrive at a total score (theoretical range 0-60 points). Higher levels represent more depressive symptoms. We calculated a depression score for persons with one or two missing items (37% and 1% of respondents, respectively) by assigning the mean score of completed questions to the missing items. No scores were calculated for individuals with three or more missing items (0.3% of participants).
Statistical methods
We computed means and distributions, as appropriate. We assessed the differences in scores attributable to exposure to famine using linear regression models. All statistical analyses were conducted with STATA software version 8.0 (Stata Inc, College Station, TX). We combined the two populations of controls into a single group and controlled for clustering of responses within families using the xt set of routines. We controlled for age at assessment (with linear and quadratic terms to control for any non-linearity in the data), and completion of secondary school as a measure of social class. In models focusing on exposure to famine overall, we built models with preconceptional exposure, gestational exposure, or both. In models focusing on exposure in defined periods, terms for preconceptional exposure and the four 10-week periods were entered as a set, and the overall significance of the set was tested using a 5-degrees-of-freedom Wald Chi-square test. We examined additive interactions with sex. As none was significant using p=0.10 as a threshold, we ran pooled models with adjustment for sex. We report estimates and associated 95% confidence intervals (CIs).
Results
Complete data were available for 923 people; 411 had preconceptional or gestational exposure, 218 were born in the same hospitals outside the famine period, and 294 were sibling controls. Selected characteristics of these individuals are provided in Table 1.
Table 1. Selected characteristics in 2003-2005 of Dutch individuals born in one of three hospitals in 1943-1947 and their siblings.
| Famine-exposeda (n=411) | Time controlsb (n=218) | Sibling controls (n=294) | |
|---|---|---|---|
| Men (%) | 47 | 45 | 43 |
| Birth weight (g); mean (SD) | 3319 (519) | 3460 (487) | c |
| Crown to heel length (cm); mean (SD) | 50.4 (2.3) | 50.8 (2.2) | c |
| Age at assessment (years); mean (SD) | 58.8 (0.5) | 59.0 (1.8) | 57.2 (6.2) |
| Completed secondary school; % | 68 | 73 | 68 |
| Current smoker; % | 25 | 23 | 23 |
| Regular alcohol consumption; % | 84 | 83 | 80 |
| Body mass index (kg/m2); mean (SD) | 28.4 (4.9) | 27.2 (4.3) | 27.0 (4.2) |
Individuals exposed immediately before conception or for any 10-week period during gestation.
Born in the same institutions as exposed but not exposed to famine immediately prior to conception or during gestation
Not available for siblings
The mean mental component and physical component scores of the Short-Form Health Survey were 52.4 (SD = 9.4) and 48.9 (9.0), respectively. For the 8 domains of the Short-Form Health Survey, mean scores ranged from 67 (general health) to 85 (social functioning and role-emotional). The mean depression score was 11.6 (7.4). (Table 2).
Table 2.
Self-reported quality of life and depressive symptoms among Dutch adults assessed in 2003-2005, by exposure to the Dutch Famine before conception or during gestation.
| No famine exposure | Famine exposure | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Hospital controls | Sibling controls | Any exposure | Pre-conception | Weeks 1-10 | Weeks 11-20 | Weeks 21-30 | Weeks 31 to delivery | |
| (n=218) | (n=294) | (n=411) | (n=91) | (n=72) | (n=126) | (n=136) | (n=124) | |
|
|
||||||||
| Quality of Life (SF-36) | ||||||||
| Mental component score | 53.1 (9.7) | 52.9 (8.5) | 51.8 (9.8) | 50.4 (10.5) | 51.1 (9.1) | 52.3 (9.5) | 52.4 (10.2) | 52.6 (9.4) |
| Physical component score | 48.6 (9.0) | 49.7 (8.8) | 48.6 (9.2) | 50.2 (9.8) | 48.3 (9.7) | 48.3 (8.7) | 47.9 (9.0) | 48.0 (9.6) |
| Physical Functioning | 83.2 (18.5) | 84.8 (17.9) | 81.7 (21.1) | 85.2 (19.9) | 81.9 (20.4) | 82.7 (19.4) | 80.9 (22.2) | 78.3 (23.8) |
| Role-Physical | 79.6 (35.5) | 82.7 (33.4) | 77.9 (36.2) | 80.5 (35.7) | 72.9 (38.9) | 76.0 (36.8) | 78.3 (35.2) | 78.6 (35.7) |
| Bodily Pain | 78.1 (22.8) | 79.2 (23.1) | 78.1 (22.0) | 79.9 (23.9) | 76.7 (24.7) | 77.3 (22.2) | 76.5 (21.1) | 78.8 (20.5) |
| General Health | 66.6 (16.6) | 69.0 (16.4) | 65.9 (17.7) | 67.5 (17.3) | 65.3 (17.2) | 65.3 (16.3) | 64.6 (17.1) | 66.5 (19.6) |
| Vitality | 69.2 (18.7) | 69.9 (17.1) | 68.0 (18.3) | 66.3 (18.5) | 66.9 (18.1) | 68.3 (19.4) | 69.3 (19.0) | 68.5 (18.0) |
| Social Functioning | 86.1 (20.5) | 86.0 (18.6) | 84.7 (20.2) | 83.9 (21.4) | 86.5 (17.6) | 86.1 (18.4) | 83.7 (22.7) | 84.5 (19.5) |
| Role-Emotional | 88.5 (29.6) | 87.4 (28.0) | 82.2 (34.2) | 82.4 (34.9) | 78.7 (38.1) | 81.5 (35.4) | 83.8 (30.9) | 83.9 (32.5) |
| Mental Health | 77.6 (16.9) | 78.2 (15.3) | 76.1 (16.5) | 73.9 (16.9) | 74.3 (14.4) | 77.6 (15.6) | 76.9 (17.5) | 77.2 (16.6) |
| Depressive symptoms (CES-D) | 11.1 (7.8) | 10.5 (6.8) | 12.6 (7.4) | 13.2 (7.9) | 12.7 (7.2) | 12.7 (7.3) | 12.4 (7.3) | 11.6 (7.3) |
|
| ||||||||
Data are means (standard deviations). The mental and physical component scores are standardized to mean 50 and SD 10. The 8 domains are expressed as percentage of “perfect health.” The depression score has a theoretical range of 0-60 points. Any exposure includes individuals exposed immediately before conception or for any 10-week period during gestation. Individuals exposed during gestation may have been exposed in one or two specific periods.
Male sex and completion of secondary school were each associated with higher mental and physical component scores, and a lower depression score (Table 3). Body mass index was associated with lower mental and physical component scores and a higher depression score. Age-, sex- and schooling-adjusted estimates for mutually adjusted exposures were -2.48 for the mental component score with exposure before conception (95% confidence interval = -4.46 to 0.50) and 0.07 with exposure during pregnancy (-1.15 to 1.29). Adjusted estimates for the physical component score were 1.26 with exposure before conception (-0.67 to 3.19) and -0.73 with exposure during pregnancy (1.94 to 0.48). Adjusted estimates for the depression score were 2.07 with exposure before conception (0.60 to 3.54) and 0.96 with exposure during pregnancy (0.09 to 1.88). (Table 4). Further adjustment for body mass index did not alter these estimates (data not shown).
Table 3.
Association of measures of quality of life and depression with selected characteristics measured at follow-up, among 923 Dutch men and women assessed in 2003-2005.
| Mental component Score Coefficient (95% CI) | Physical component Score Coefficient (95% CI) | Depressive symptoms Score Coefficient (95% CI) | |
|---|---|---|---|
| Sex (male =1, female = 0) | 2.88 (1.51, 4.24) | 3.09 (1.90, 4.29) | -3.01 (-4.07 to -1.96) |
| Schooling (higher schooling = 1, else = 0) | 1.47 (0.15, 2.78) | 1.88 (0.64, 3.12) | -2.02 (-3.00 to -1.05) |
| BMI (per kg/m2) | -0.09 (-0.23, 0.04) | -0.41 (-0.53, -0.28) | 0.15 (0.05 to 0.24) |
Estimates are linear regression coefficients and associated 95% CIs. Models are adjusted for age, age squared, and familial clustering. The mental and physical component scores are standardized to mean 50 and SD 10. The depressive symptoms score has a theoretical range of 0-60 points, and this population has a mean of 11.6 and a SD of 7.4.
Table 4.
Association of measures of quality of life and depression with exposure to the Dutch famine immediately preceding or during gestation, among 923 Dutch men and women assessed in 2003-2005.
| Exposure immediately before conception Coefficient (95% CI) | Exposure during gestation Coefficient (95% CI) | ||
|---|---|---|---|
| Mental component score | Model 1 | -2.49 (-4.46 to -0.52) | |
| Model 2 | 0.22 (-0.99 to 1.44) | ||
| Model 3 | -2.48 (-4.46 to -0.50) | -0.07 (-1.15 to 1.29) | |
| Physical component score | Model 1 | 1.40 (-0.52 to 3.31) | |
| Model 2 | -0.82 (-2.03 to 0.38) | ||
| Model 3 | 1.26 (-0.67 to 3.19) | -0.73 (1.94 to 0.48) | |
| Depressive symptoms | Model 1 | 1.92 (0.45 to 3.39) | |
| Model 2 | 0.87 (-0.02 to 1.76) | ||
| Model 3 | 2.07 (0.60 to 3.54) | 0.96 (0.09 to 1.88) | |
Estimates are linear regression coefficients and associated 95% CIs. Comparison group is combined hospital and sibling controls. Models are adjusted for age, age squared, sex, schooling attainment and familial clustering.
The mental and physical component scores are standardized to mean 50 and SD 10. The depressive symptoms score has a theoretical range of 0-60 points, and this population has a mean of 11.6 and a SD of 7.4.
Models considering specific 10-week period of gestational exposure are presented in Table 5. For the physical component score, all the coefficients were negative and within 1 point of null, while for the depression score, all four 10-week periods had positive coefficients, ranging from 0.29 (95% CI = -1.06 to 1.65) for exposure in weeks 31 through delivery to 1.27 (-0.06 to 2.60) for exposure in weeks 21-30. For the mental component score and the depression score, the magnitude of the period-specific coefficients was smaller than that observed for preconceptional exposure.
Table 5.
Association of measures of quality of life and depression with timing of exposure to the Dutch famine immediately preceding or during gestation, among 923 Dutch men and women assessed in 2003-2005.
| Period of famine exposure | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| Weeks 1-10 before conception Coefficient (95% CI) | Weeks 1-10 of gestation Coefficient (95% CI) | Weeks 11-20 of gestation Coefficient (95% CI) | Weeks 21-30 of gestation Coefficient (95% CI) | Weeks 31 to delivery Coefficient (95% CI) | P (Wald test) | |
|
|
||||||
| Mental component score | -2.45 (-4.52 to -0.39) | -0.54 (-2.87 to 1.78) | 0.12 (-1.76 to 2.00) | -0.73 (-2.53 to 1.07) | 0.31 (-1.51 to 2.14) | 0.22 |
| Physical component score | 1.22 (-0.80 to 3.23) | -0.80 (-3.05 to 1.46) | -0.07 (-1.92 to 1.72) | -0.93 (-2.69 to 0.83) | -0.80 (-2.58 to 0.98) | 0.45 |
| Depressive symptoms | 2.20 (0.67 to 3.73) | 0.54 (-1.19 to 2.26) | 0.74 (-0.64 to 2.12) | 1.27 (-0.06 to 2.60) | 0.29 (-1.06 to 1.65) | 0.015 |
|
| ||||||
Estimates are linear regression coefficients and associated 95% CIs. Comparison group is combined hospital and sibling controls.
Models are adjusted for age, age squared, schooling attainment, familial clustering and exposure in adjacent 10-week periods. Wald test (5 df) for set of 5 periods
Sensitivity analyses
In models in which each of the eight domains of the quality-of-life survey was entered as a dependent variable, not one suggested associations with famine exposure (eTable 1A; http://links.lww.com). Logistic regression models in which each dependent variable was dichotomized close to its median were consistent with the linear regression models (eTable 1B; http://links.lww.com), as were models in which each source of controls (hospital births or siblings) was considered separately (eTables 2A and 2B; http://links.lww.com). Birth weight was not associated with any of the scores (eTable 3A; http://links.lww.com), and adjustment for birth weight did not alter the estimates of the association between famine exposure and these measures (eTable 3B; http://links.lww.com). Our estimates were robust to various approaches to adjustment for clustering within families (population-averages general estimating equations, and use of the Huber-White estimator to correct standard errors) (data not shown).
Discussion
Preconceptional exposure to the Dutch famine was associated with a 2.48 point lower score on the mental component score of a quality-of-life survey, and with a 2.07 point higher depression score—both of which are indicative of poorer mental health-related quality of life. Prenatal exposure to famine was also associated with a 0.96-point increased depression score. We did not observe any large or consistent associations with the physical component of the quality-of-life survey. These differences are relatively large—the 2.48 point decrease in the mental component score represents 0.25 SD of this measure, while the 2.07 increase in the depression score represents 0.28 SD of this measure.
Quality of life, as measured by our instrument and other generic health-related instruments, has to our knowledge not been explored in previous Dutch famine studies. One previous study reported that persons exposed to the Dutch famine in early gestation (but not in mid- or late gestation) more often rated their health as poor.12 That study used one generic question (translated as “How do you rate your health?”), which does not differentiate between mental and physical health or cover other relevant aspects in any detail. Our results extend those findings in two ways. We identify preconception exposure as being critical, and we single out mental health as the domain selectively affected.
Many of the persons who met our a priori definition of preconceptional famine exposure were also exposed (though not for as long as ten weeks) to the height of the famine around the time of conception or in early gestation. Indeed, a series of studies has shown schizophrenia to be related to periconceptional or early gestational famine exposure, using a definition of exposure that overlaps substantially with preconceptional famine as defined here.9 More recently we have shown that this same period of exposure is associated with relative hypomethylation of the IGF2-gene.26 Our present observations add to the body of evidence that maternal nutritional status at the point of conception may be critical to the development of the fetus in multiple domains.
A strength of the current study is the population-based design. Individuals were recruited from institutional birth records on the basis of their place and date of birth, irrespective of their health status. Another strength is the study size that allows for assessment of famine effects specific for gestational periods and results in reasonably precise estimates. The timing of exposure was based on the gestational age relative to the last menstrual period, which may have an advantage over timing based on the birth date because the exposure classification is not biased by variation in pregnancy duration. Lastly, the instruments we administered are well-recognized sensitive measures of quality of life and depressive symptoms that have been shown to be valid in Dutch populations.23, 25 We did not obtain a measure of lifetime prevalence of psychiatric illness and cannot assess whether this measure was differentially distributed by famine exposure category.
A limitation of our study is the indirect quantification of food intake based on the official rations, rather than on personal data. However, the severity and general distribution of the food reduction have been documented extensively. Fertility was reduced by 50%, and women who were pregnant during the famine failed to gain any weight during the pregnancy.17 The nutritional deficits caused by the famine were accompanied by other social and psychological stressors, and the famine remains a salient event in Dutch culture.
Another limitation of the study is the limited participation. We cannot exclude the possibility that selection bias has resulted in a differential response between exposed individuals and the reference population. However, loss to follow-up did not differ by exposure status, and a non-response analysis showed that those who were enrolled were similar to non-responders in terms of birth weight, birth length, placental weight, maternal age at delivery, and birth order.19 Socioeconomic status was slightly lower for non-responders. Except for age, demographic and background variables were similar between the exposed and reference groups. The quality-of-life and depression scores in our reference population were similar to those previously reported for the general population of the Netherlands.23, 25 Thus selection bias is an unlikely explanation for the null results. We conclude that famine exposure prior to conception is associated with poorer self-reported mental health and a higher level of depressive symptoms.
Supplementary Material
Figure 1.
Flow chart of study sample selection, follow-up, contact and examination.
Acknowledgments
Funding: Supported by the NHLBI/NIH (R01 HL-067914: PI: LHL).
Footnotes
SDC Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com).
References
- 1.Stein AD, Kahn HS, Rundle A, Zybert PA, van der Pal-de Bruin K, Lumey LH. Anthropometric measures in middle age after exposure to famine during gestation: evidence from the Dutch famine. Am J Clin Nutr. 2007;85:869–76. doi: 10.1093/ajcn/85.3.869. [DOI] [PubMed] [Google Scholar]
- 2.Stein AD, Zybert PA, van der Pal-de Bruin K, Lumey LH. Exposure to famine during gestation, size at birth, and blood pressure at age 59 y: evidence from the Dutch Famine. Eur J Epidemiol. 2006;21:759–65. doi: 10.1007/s10654-006-9065-2. [DOI] [PubMed] [Google Scholar]
- 3.Painter RC, de Rooij SR, Bossuyt PM, Simmers TA, Osmond C, Barker DJ, Bleker OP, Roseboom TJ. Early onset of coronary artery disease after prenatal exposure to the Dutch famine. Am J Clin Nutr. 2006 Aug;84(2):322–7. doi: 10.1093/ajcn/84.1.322. [DOI] [PubMed] [Google Scholar]
- 4.Brown AS, Susser ES, Lin SP, Neugebauer R, Gorman JM. Increased risk of affective disorders in males after second trimester prenatal exposure to the Dutch hunger winter of 1944-45. Br J Psychiatry. 1995;166:601–06. doi: 10.1192/bjp.166.5.601. [DOI] [PubMed] [Google Scholar]
- 5.Brown AS, van Os J, Driessens C, Hoek HW, Susser ES. Further evidence of relation between prenatal famine and major affective disorder. Am J Psychiatry. 2000;157:190–95. doi: 10.1176/appi.ajp.157.2.190. [DOI] [PubMed] [Google Scholar]
- 6.Neugebauer R, Hoek HW, Susser E. Prenatal exposure to wartime famine and development of antisocial personality disorder in early adulthood. JAMA. 1999;282:455–62. doi: 10.1001/jama.282.5.455. [DOI] [PubMed] [Google Scholar]
- 7.Hoek HW, Brown AS, Susser E. The Dutch famine and schizophrenia spectrum disorders. Soc Psychiatry Psychiatr Epidemiol. 1998;33:373–79. doi: 10.1007/s001270050068. [DOI] [PubMed] [Google Scholar]
- 8.Susser E, Neugebauer R, Hoek HW, Brown AS, Lin S, Labovitz D, et al. Schizophrenia after prenatal famine. Further evidence Arch Gen Psychiatry. 1996;53:25–31. doi: 10.1001/archpsyc.1996.01830010027005. [DOI] [PubMed] [Google Scholar]
- 9.Hoek HW, Susser E, Buck KA, Lumey LH, Lin SP, Gorman JM. Schizoid personality disorder after prenatal exposure to famine. Am J Psychiatry. 1996;153:1637–39. doi: 10.1176/ajp.153.12.1637. [DOI] [PubMed] [Google Scholar]
- 10.Hulshoff Pol HE, Hoek HW, Susser E, Brown AS, Dingemans A, Schnack HG, et al. Prenatal exposure to famine and brain morphology in schizophrenia. Am J Psychiatry. 2000;157:1170–72. doi: 10.1176/appi.ajp.157.7.1170. [DOI] [PubMed] [Google Scholar]
- 11.Brown AS, Susser ES. Sex differences in prevalence of congenital neural defects after periconceptional famine exposure. Epidemiology. 1997;8:55–58. doi: 10.1097/00001648-199701000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Roseboom TJ, van der Meulen JH, Ravelli AC, Osmond C, Barker DJ, Bleker OP. Perceived health of adults after prenatal exposure to the Dutch famine. Paediatr Perinat Epidemiol. 2003;17:391–97. doi: 10.1046/j.1365-3016.2003.00516.x. [DOI] [PubMed] [Google Scholar]
- 13.Burger GC, Drummond JC, Sanstead HR. The Hague. The Netherlands: Staatsuitgeverij; 1948. Malnutrition and starvation in western Netherlands, September 1944 -July 1945. Parts I and II. [Google Scholar]
- 14.Lumey LH, Van Poppel FW. The Dutch famine of 1944-45: mortality and morbidity in past and present generations. Soc Hist Med. 1994;7:229–46. doi: 10.1093/shm/7.2.229. [DOI] [PubMed] [Google Scholar]
- 15.Trienekens G. The food supply in The Netherlands during the Second World War. In: Smith DF, Phillips J, editors. Food Science Policy and Regulation in the Twentieth Century International and Comparative Perspectives. London: Routledge; 2000. pp. 117–33. [Google Scholar]
- 16.Smith CA. The effect of wartime starvation in Holland upon pregnancy and its product. Am J Obstet Gynecol. 1947;53:599–608. doi: 10.1016/0002-9378(47)90277-9. [DOI] [PubMed] [Google Scholar]
- 17.Stein AD, Ravelli AC, Lumey LH. Famine, third-trimester pregnancy weight gain, and intrauterine growth: the Dutch Famine Birth Cohort Study. Hum Biol. 1995;67:135–50. [PubMed] [Google Scholar]
- 18.Roseboom T, de Rooij S, Painter R. The Dutch famine and its long-term consequences for adult health. Early Hum Dev. 2006;82:485–91. doi: 10.1016/j.earlhumdev.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 19.Lumey LH, Stein AD, Kahn HS, van der Pal-de Bruin KM, Blauw GJ, Zybert PA, Susser ES. Cohort profile: The Dutch Hunger Winter Families Study. Int J Epidemiol. 2007;36:1196–1204. doi: 10.1093/ije/dym126. [DOI] [PubMed] [Google Scholar]
- 20.Kloosterman GJ. On intrauterine growth. Int J Gynaecol Obstet. 1970;8:895–912. [Google Scholar]
- 21.Ware JE, Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33:264–279. [PubMed] [Google Scholar]
- 22.Garratt A, Schmidt L, Mackintosh A, Fitzpatrick R. Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ. 2002;324:1417. doi: 10.1136/bmj.324.7351.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51:1055–68. doi: 10.1016/s0895-4356(98)00097-3. [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Kosinski M, Keller SK. A User's Manual. Boston, MA: The Health Institute; 1994. SF-36® Physical and Mental Health Summary Scales. [Google Scholar]
- 25.Beekman AT, Deeg DJ, Van Limbeek J, Braam AW, De Vries MZ, van Tilburg W. Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): results from a community-based sample of older subjects in The Netherlands. Psychol Med. 1997;27:231–35. doi: 10.1017/s0033291796003510. [DOI] [PubMed] [Google Scholar]
- 26.Heijmans BT, Tobi EW, Stein AD, Putter H, Blauw G-J, Susser ES, Slagboom PE, Lumey LH. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc Nat Acad Sci. 2008;105:17046–17049. doi: 10.1073/pnas.0806560105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.