Abstract
Objective: Tele-assessment techniques can provide healthcare professionals with easily accessible information regarding patients' clinical progress. Recently, kinematic analysis systems have been used to assess rehabilitative outcomes in stroke patients. Kinematic systems, however, are not compatible with tele-assessment. The objective of our study was to develop a tele-assessment system for acquiring kinematic data of forward reaching movements in stroke patients, with an emphasis on cost-effectiveness, portability, and ease of use. Materials and Methods: We selected four healthy control participants and eight hemiplegic stroke patients for our study. The stroke patients were classified as Brunnstrom stage III, stage IV, or stage V. Our tele-assessment system used two three-axes accelerometers, a potentiometer, a multifunctional data acquisition card, and two computers. A standardized kinematic system was applied simultaneously to validate the measurements recorded by our tele-assessment system during five repetitions of forward reaching movements. Results: The correlation coefficients of the reaching displacement, velocity, and acceleration measurements obtained using our tele-assessment system and the standardized kinematic system were 0.956, 0.896, and 0.727, respectively. Differences in the maximum reaching distance and the maximum reaching velocity of forward reaching movements were observed among the study groups. There were no significant differences in the time required to complete the testing session among the study groups. Conclusions: Our tele-assessment system is valid for the evaluation of upper-extremity reaching ability in stroke patients. Further research is needed to investigate the feasibility of the use of the tele-assessment system in patients' homes.
Key words: tele-assessment, stroke, upper extremity function
Introduction
In hospital-based stroke rehabilitation programs, patients receive therapy in both inpatient and outpatient settings. Early supported discharge programs are designed to accelerate the transition from the hospital to the home by establishing skills that will be needed by recovering patients in their home environment. In a 5-year follow-up study, stroke patients who participated in early supported discharge programs reported better perceived health status than those receiving conventional rehabilitation.1 The use of telerehabilitation can increase the accessibility of early supported discharge rehabilitation programs, with therapists providing daily therapy in the patients' homes without being present.
Home-based telerehabilitation interventions have shown promising results in improving the health of stroke patients and in supporting the caregivers.2 Several systems for remote rehabilitation service have been developed to assist in patients' training.3–7 Nonetheless, systems for remote assessment are scant. If patients' accessibility to rehabilitation facilities is limited because of transportation-related problems, traditional clinical assessment, such as the Fugl–Meyer assessment,8 the Functional Independence Measure,9 and the Action Research Arm Test,10 cannot be performed. Tele-assessment techniques enable professionals to remotely collect real-time data regarding patients' progress.
Various tele-assessment systems have been developed. Videoconferencing has been shown to be a feasible and reliable method to evaluate patients with neurological symptoms.11,12 Park et al.13 developed a system that provided physical and audiovisual interaction between the clinician and the patient; the system included a clinician-operated master device and a patient-operated slave device. A similar tele-assessment system was developed that used advanced control modules to achieve bilateral interactions.14 However, the clinical application of these tele-assessment systems is limited by the costly, heavy equipment required and the lack of an objective kinematic analysis component.
Kinematic analysis has been used to evaluate treatment outcomes in stroke patients.15–19 Kinematic assessment has demonstrated reliability for evaluating spatiotemporal control of the upper limbs, such as forward reaching. However, electromagnetic-15 and video-based16–19 kinematic systems are complex and bulky, rendering them largely incompatible with tele-assessment in patients' homes. Convenient, easily used inertia-based motion detectors have been developed for the evaluation of upper limb functions, but the interpretation of the test results requires specialized training.20
The objective of our study was to develop a tele-assessment system for evaluating reaching movements in stroke patients, with an emphasis on cost-effectiveness, portability, and ease of use. In this article, the structure of our tele-assessment system and the process of validating the system are presented. Reaching movement parameters obtained by our tele-assessment system were compared with those obtained by a conventional kinematic assessment system. In addition, data obtained by our tele-assessment system from participants with different levels of upper arm impairment were analyzed to test the discrimination ability of the impairment level of our system.
Materials and Methods
Participants
Our study was approved by the Institutional Review Board of National Taiwan University Hospital (approval number 200810043R). Informed consent was obtained from each participant before his or her participation in the experiments. We recruited four healthy adults 24–35 years of age (mean age, 28 years) for the healthy control group. The inclusion criteria for stroke patient selection were as follows: (1) unilateral ischemic stroke; (2) Brunnstrom stage III–V for the arms, a commonly used clinical scale for classifying limb function in hemiplegic patients21; (3) the ability to execute forward reaching movements without support; and (4) the ability to understand three-step commands. Patients with an unstable medical condition, a pacemaker, or shoulder pain associated with forward reaching were excluded from our study. Based on these criteria, 8 stroke patients 38–87 years of age (mean age, 62.9 years) were selected for our study, of whom 2 were Brunnstrom stage III, 2 were stage IV, and 4 were stage V. All of the participants were right-handed. One stroke patient was right-sided hemiparetic, and all of the other stroke patients were left-sided hemiparetic. The onset to assessment intervals for the stroke patients ranged from 2 to 126 months, with a mean of 57.5 months (Table 1).
Table 1.
Demographic Data and Clinical Characteristics of the Study Participants
| PARTICIPANT NUMBER | AGE (YEARS) | SEX | HANDEDNESS | HEMIPARESIS | BRUNNSTROM STAGEa | POSTSTROKE (MONTHS) |
|---|---|---|---|---|---|---|
| 1 | 75 | Female | Right | Right | III | 126 |
| 2 | 56 | Female | Right | Right | III | 6 |
| 3 | 65 | Male | Right | Right | IV | 102 |
| 4 | 38 | Male | Right | Right | IV | 4 |
| 5 | 87 | Female | Right | Left | V | 84 |
| 6 | 67 | Female | Right | Right | V | 100 |
| 7 | 62 | Male | Right | Right | V | 36 |
| 8 | 53 | Female | Right | Right | V | 2 |
| 9 | 24 | Female | Right | Healthy | — | |
| 10 | 25 | Female | Right | Healthy | — | |
| 11 | 35 | Male | Right | Healthy | — | |
| 12 | 27 | Male | Right | Healthy | — |
Participants 9–12 were healthy control participants.
Tele-Assessment System Design
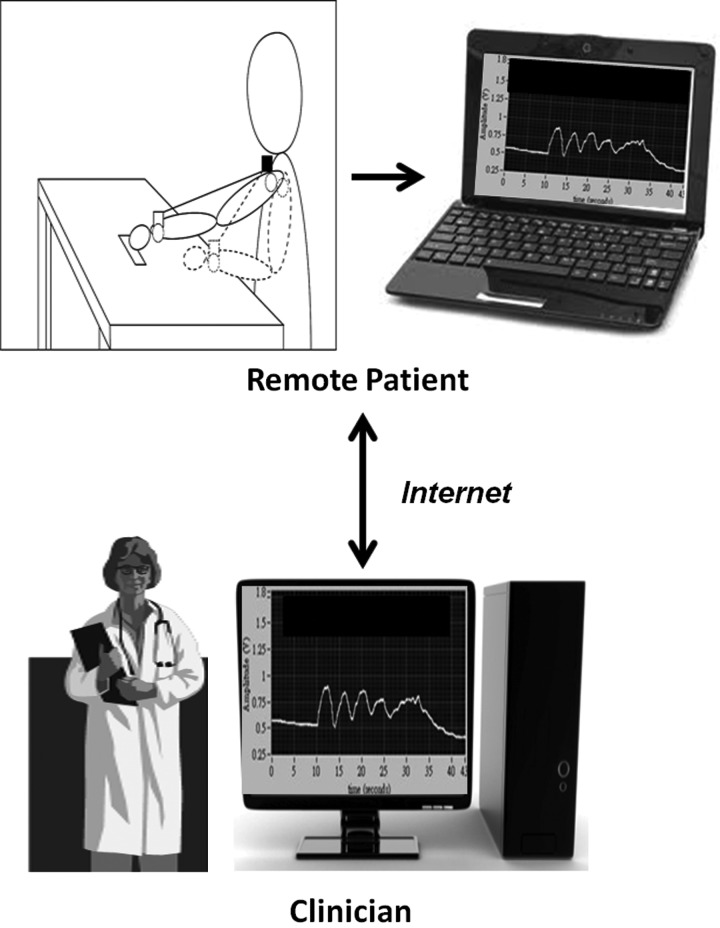
Our tele-assessment system consisted of a potentiometer, two accelerometers, a low-cost National Instruments (Austin, TX) USB-6221 multifunctional data acquisition module, and two computers. The assessment data were acquired using LabVIEW software (National Instruments), with the participant's computer functioning as the server and the clinician's computer as the client. The potentiometer was used for gathering the distance, speed, and acceleration data of the reaching movement, with the accelerometers monitoring the compensatory movements during forward reaching. The USB-6221 multifunctional data acquisition module used 16-bit resolution, a 250,000/s sampling rate, and 16 analog input channels for sensor data acquisition by the LabVIEW server, and the real-time analysis of the kinematic data were performed on the client computer. The participant's reaching pattern was displayed in real time on the monitor of the clinicians' computer (Fig. 1).
Fig. 1.
Illustration of the tele-assessment system showing the remote acquisition of forward reaching data in the patient's home and the transmission of the data from the patient's remote computer to the clinician's computer via the Internet.
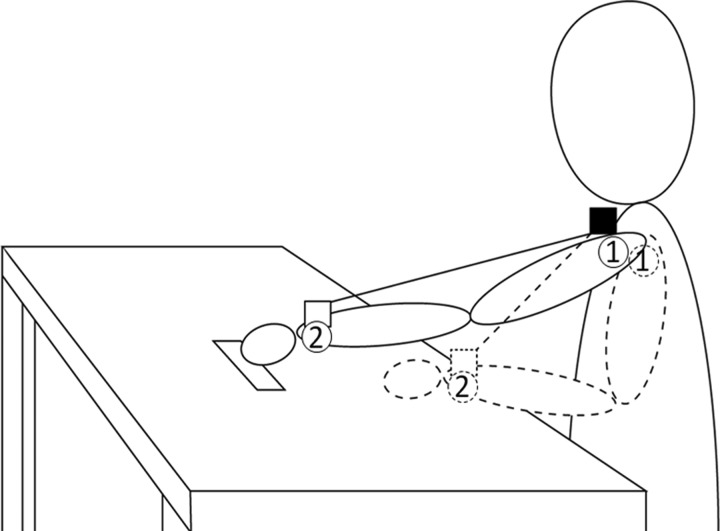
Sensor Location
The tele-assessment sensors were positioned as shown in Figure 2. To measure the acceleration of the movement, one of the accelerometers was placed over the left acromion, and the other was placed over the forearm at the intersection of the plane of the middle finger and the plane bisecting the radial and ulnar styloid processes. The displacement and motion speed were measured using a potentiometer. The potentiometer was placed over the midpoint of the proximal clavicle by attachment to a vest worn by the participant, and the movable end of the potentiometer was attached to the radial styloid process.
Fig. 2.
Diagram of the forward reaching measurements. The open circles (numbered 1 and 2) represent the accelerometers. The open square represents the stationary end of the potentiometer, and the solid square represents the movable end of the potentiometer. The positions of the participant's arm and the moveable potentiometer before the reaching movement are represented in stippled lines.
System Validation
We used the FASTRAK® (Polhemus, Colchester, VT) system to validate the kinematic assessment of our tele-assessment system. The two FASTRAK receivers were juxtaposed with the two accelerometers of our tele-assessment system, and the characteristics of the reaching movements were recorded simultaneously by both systems. The displacement, velocity, and acceleration data that were acquired using both systems were analyzed using Matlab 2011 (MathWorks, Natick, MA).
Experimental Procedures
The participants were asked to remove all metal items to avoid potential signal interference. The testing was performed while the participants were seated with their forearms placed on a table. Before testing was initiated, the examiner marked the longest distance on the table that the participant could reach during practice forward reaching motions. Two testing sessions were performed. During each testing session, the participant reached forward to his or her respective maximum distance for five continuous repetitions.
Statistical Analysis
The criterion-related validity was determined by calculating the Spearman correlation coefficient (r) for comparisons of the reaching data obtained using our tele-assessment system and those obtained using the FASTRAK system. An analysis of variance was used to determine whether any significant differences occurred among the four study groups in the maximum reaching distance, the maximum reaching velocity, and the time required to complete the testing session. The data were analyzed using Statistical Packages for Social Sciences version 16.0 computer software (SPSS, Inc., Chicago, IL). A value of p<0.05 was considered to represent a statistically significant difference.
Results
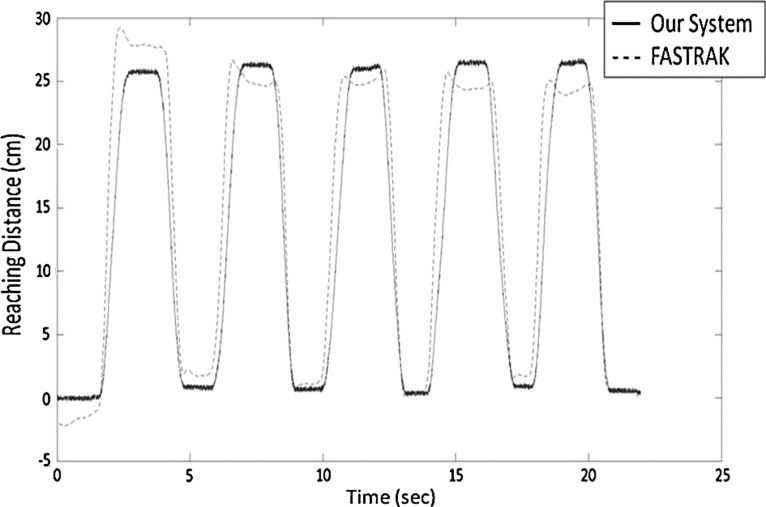
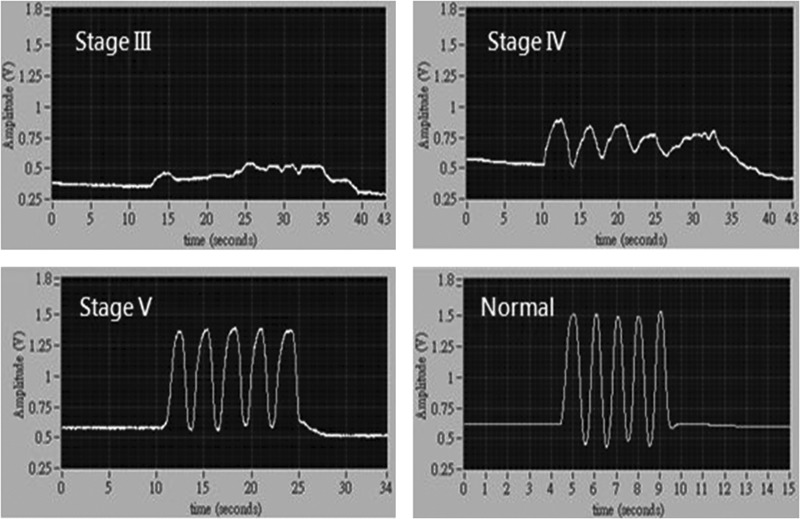
The correlation coefficients for the displacement, velocity, and acceleration measurements were 0.956, 0.896, and 0.727, respectively. The displacement waveforms of the potentiometer of our system and that of the FASTRAK system are superimposed in Figure 3. The reaching patterns of the study participants are shown in Figure 4. The average maximum reaching distance, maximum reaching velocity, and the average time required to complete the testing sessions are shown in Figure 5. The analysis of variance results showed that there were significant differences in the maximum reaching distance (Fig. 5A), maximum reaching velocity (Fig. 5B), and time required to complete the testing sessions (Fig. 5C) between groups (p<0.05).
Fig. 3.
Five repetitions of the forward reaching movements of a healthy control were recorded simultaneously using our tele-assessment system and the FASTRAK system, and the reaching distance waveforms were superimposed to demonstrate the validity of our tele-assessment system.
Fig. 4.
The patterns of the forward reaching movements of Brunnstrom stage III–IV stroke patients and control participants. The signal was generated from the amplitude values recorded by the potentiometer as the distance between the moveable and fixed ends changed during the forward reaching movements. The smoothness of the reaching pattern was obviously different for each group.
Fig. 5.
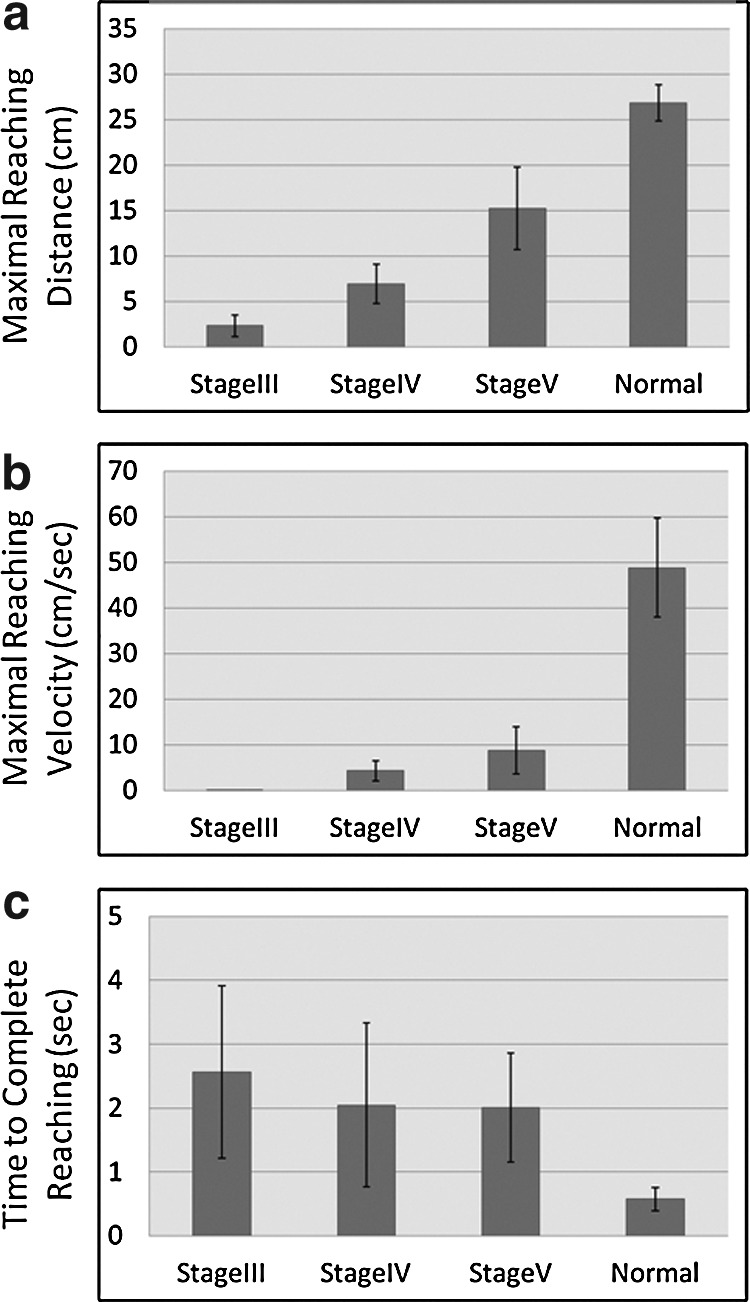
Reaching movement characteristics of each study group: (a) the maximum reaching distance, (b) the maximum reaching velocity, and (c) the time required to complete the testing sessions are represented. Data are mean±standard deviation values.
Discussion
The purpose of our study was to construct a tele-assessment system for evaluating forward reaching movements in stroke patients. Some tele-assessment systems have been developed for measuring range of motion and muscle strength.13,14 However, sensor-embedded tele-assessment systems for the measurement of functional tasks, such as forward reaching, require further investigation. Thus, we used this approach for developing the present tele-assessment system. Results acquired from kinematic analysis systems are useful for evaluation of movement deficiencies.16 Current kinematic systems, however, require well-trained specialists and are available in a clinical setting only. Compared with three-dimensional kinematic analysis systems, our tele-assessment system is more user-friendly.
We used the FASTRAK system to examine the validity of assessments performed using our tele-assessment system because it is considered by many clinicians to be the gold standard for rehabilitative assessment.22 The movement displacement, velocity, and acceleration data that were recorded using our tele-assessment system highly correlated with that obtained using the FASTRAK system, demonstrating that the accuracy of the assessment data collected using our tele-assessment system is comparable to that of the FASTRAK system. The differences observed in the displacement and velocity data between our tele-assessment system and those of the FASTRAK system may have resulted from the use of different measurement criteria between the two systems. Our tele-assessment system measures the displacement as the distance between the clavicle and the radial styloid process, whereas the FASTRAK system measures the length of the displacement in the x–y plane only.
The forward reaching ability of the various impairment severity of the participants appeared to be distinguishable based on the measurements recorded using our tele-assessment system. The reaching pattern figures, the maximal reaching distance, and the maximal reaching velocity gathered from the healthy participants and the stroke patients in each Brunnstrom stages were different. The result was similar to previous studies.23,24
With a weight of 900 g, our tele-assessment system is highly portable and is much smaller than the equipment required by the FASTRAK systems. Compared with other inertial sensor systems, our tele-assessment system is more easily operated, and the training course for operators is relatively short. A patient's assessment can be completed in approximately 15 min using our system. Moreover, it is much easier to determine the position at which the measurement device should be fixed, and the analysis process for our tele-assessment system is also relatively straightforward.
Our system is limited to single-dimension measurements of forward reaching arm movements. Future investigations could increase the dimensional capacity of the system through the use of inertial sensors, such as gyroscopes and magnetometers. Our tele-assessment system can be used in patients' homes, and clinicians can acquire patients' data remotely in real time. Further research is, however, needed to investigate potential confounding factors that may be associated with home use.
Acknowledgments
We wish to thank the study participants and the National Science Council of the Republic of China for the research grants (NSC 98-2221-E-002-097 and NSC 99-2221-E-002-028-MY2) that made this study possible.
Disclosure Statement
No competing financial interests exist.
References
- 1.Ytterberg C. Thorsén A-M. Liljedahl M, et al. Changes in perceived health between one and five years after stroke: A randomized controlled trial of early supported discharge with continued rehabilitation at home versus conventional rehabilitation. J Neurol Sci. 2010;294:86–88. doi: 10.1016/j.jns.2010.03.027. [DOI] [PubMed] [Google Scholar]
- 2.Johansson T. Wild C. Telerehabilitation in stroke care—A systematic review. J Telemed Telecare. 2011;17:1–6. doi: 10.1258/jtt.2010.100105. [DOI] [PubMed] [Google Scholar]
- 3.Piron L. Turolla A. Agostini M, et al. Exercises for paretic upper limb after stroke: A combined virtual-reality and telemedicine approach. J Rehabil Med. 2009;41:1016–1102. doi: 10.2340/16501977-0459. [DOI] [PubMed] [Google Scholar]
- 4.Piron L. Tonin P. Trivello E, et al. Motor tele-rehabilitation in post-stroke patients. Med Inform Internet Med. 2004;29:119–125. doi: 10.1080/14639230410001723428. [DOI] [PubMed] [Google Scholar]
- 5.Holden MK. Dyar TA. Dayan-Cimadoro L. Telerehabilitation using a virtual environment improves upper extremity function in patients with stroke. IEEE Trans Neural Syst Rehabil Eng. 2007;15:36–42. doi: 10.1109/TNSRE.2007.891388. [DOI] [PubMed] [Google Scholar]
- 6.Durfee W. Carey J. Nuckley D. Deng J. Design and implementation of a home stroke telerehabilitation system. Conf Proc IEEE Eng Med Biol Soc. 2009:2422–2425. doi: 10.1109/IEMBS.2009.5334951. [DOI] [PubMed] [Google Scholar]
- 7.Huijgen BC. Vollenbroek-Hutten MM. Zampolini M, et al. Feasibility of a home-based telerehabilitation system compared to usual care: Arm/hand function in patients with stroke, traumatic brain injury and multiple sclerosis. J Telemed Telecare. 2008;14:249–256. doi: 10.1258/jtt.2008.080104. [DOI] [PubMed] [Google Scholar]
- 8.Gladstone DJ. Danells CJ. Black SE. The Fugl-Meyer assessment of motor recovery after stroke: A critical review of its measurement properties. Neurorehabil Neural Repair. 2002;16:232–240. doi: 10.1177/154596802401105171. [DOI] [PubMed] [Google Scholar]
- 9.Linacre JM. Heinemann AW. Wright BD, et al. The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil. 1994;75:127–132. [PubMed] [Google Scholar]
- 10.Van der Lee JH. De Groot V. Beckerman H, et al. The intra- and interrater reliability of the action research arm test: A practical test of upper extremity function in patients with stroke. Arch Phys Med Rehabil. 2001;82:14–19. doi: 10.1053/apmr.2001.18668. [DOI] [PubMed] [Google Scholar]
- 11.Craig J. Patterson V. Russell C. Wootton R. Interactive videoconsultation is a feasible method for neurological in-patient assessment. Eur J Neurol. 2000;7:699–702. doi: 10.1046/j.1468-1331.2000.00133.x. [DOI] [PubMed] [Google Scholar]
- 12.Handschu R. Littmann R. Reulbach U, et al. Telemedicine in emergency evaluation of acute stroke: Interrater agreement in remote video examination with a novel multimedia system. Stroke. 2003;34:2842–2846. doi: 10.1161/01.STR.0000102043.70312.E9. [DOI] [PubMed] [Google Scholar]
- 13.Park HS. Peng Q. Zhang LQ. A portable telerehabilitation system for remote evaluations of impaired elbows in neurological disorders. IEEE Trans Neural Syst Rehabil Eng. 2008;16:245–254. doi: 10.1109/TNSRE.2008.920067. [DOI] [PubMed] [Google Scholar]
- 14.Oboe R. Daud OA. Masiero S, et al. Development of a haptic teleoperation system for remote motor and functional evaluation of hand in patients with neurological impairments. 2010 11th IEEE International Workshop on Advanced Motion Control. 2010:518–523. [Google Scholar]
- 15.Micera S. Carpaneto J. Posteraro F, et al. Characterization of upper arm synergies during reaching tasks in able-bodied and hemiparetic subjects. Clin Biomech (Bristol, Avon) 2005;20:939–946. doi: 10.1016/j.clinbiomech.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Caimmi M. Carda S. Giovanzana C, et al. Using kinematic analysis to evaluate constraint-induced movement therapy in chronic stroke patients. Neurorehabil Neural Repair. 2008;22:31–39. doi: 10.1177/1545968307302923. [DOI] [PubMed] [Google Scholar]
- 17.Platz T. Bock S. Prass K. Reduced skilfulness of arm motor behaviour among motor stroke patients with good clinical recovery: Does it indicate reduced automaticity? Can it be improved by unilateral or bilateral training? A kinematic motion analysis study. Neuropsychologia. 2001;39:687–698. doi: 10.1016/s0028-3932(01)00005-7. [DOI] [PubMed] [Google Scholar]
- 18.Wagner JM. Rhodes JA. Patten C. Reproducibility and minimal detectable change of three-dimensional kinematic analysis of reaching tasks in people with hemiparesis after stroke. Phys Ther. 2008;88:652–663. doi: 10.2522/ptj.20070255. [DOI] [PubMed] [Google Scholar]
- 19.Wu CY. Chuang LL. Lin KC, et al. Randomized trial of distributed constraint-induced therapy versus bilateral arm training for the rehabilitation of upper-limb motor control and function after stroke. Neurorehabil Neural Repair. 2011;25:130–139. doi: 10.1177/1545968310380686. [DOI] [PubMed] [Google Scholar]
- 20.Thies SB. Tresadern PA. Kenney LP, et al. Movement variability in stroke patients and controls performing two upper limb functional tasks: A new assessment methodology. J Neuroeng Rehabil. 2009;6:2. doi: 10.1186/1743-0003-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brunnstrom S. Movement therapy in hemiplegia: A neurophysiological approach. New York: Harper & Row; 1970. [Google Scholar]
- 22.Straker L. Campbell A. Coleman J, et al. In vivo laboratory validation of the physiometer: A measurement system for long-term recording of posture and movements in the workplace. Ergonomics. 2010;53:672–684. doi: 10.1080/00140131003671975. [DOI] [PubMed] [Google Scholar]
- 23.Trombly CA. Observations of improvement of reaching in five subjects with left hemiparesis. J Neurol Neurosurg Psychiatry. 1993;56:40–45. doi: 10.1136/jnnp.56.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kamper DG. McKenna-Cole AN. Kahn LE. Reinkensmeyer DJ. Alterations in reaching after stroke and their relation to movement direction and impairment severity. Arch Phys Med Rehabil. 2002;83:702–707. doi: 10.1053/apmr.2002.32446. [DOI] [PubMed] [Google Scholar]