Abstract
Background
Plants have widely been used and documented for their therapeutic potential in many parts of the world. There are, however, few reports on the use of plants for the treatment of diseases of equines. To this end, participatory epidemiology and rapid rural appraisal techniques were used to document the plants having pharmacotherapeutic significance against different ailments of equines in selected population of Punjab, Pakistan.
Methods
A survey was conducted to interview a total of 450 respondents (150 from each of the districts of Faisalabad, Lahore and Sargodha of Pakistan) to collect information about disease recognition of the equines and their treatment on a well − structured questionnaire. A total of 60 plants belonging to 40 families were documented. An inventory was developed depicting detailed information of plants used in treatment of different conditions of equines.
Results
The top ten species of plants used were: Allium cepa, Zingiber officinale, Vernonia anthelmintica, Capsicum annum, Brassica campestris, Trachyspermum ammi, Anethum graveolens, Picrorhiza kurroa, Azadirachta indica, and Citrullus colocynthis. Seeds were the most frequently used (n = 16/60) parts, followed by leaves (n = 12/60) and fruits (n = 11/60) of plants. Based on the combination of different parts of plants used in different ratios and variation in their dose or mode of preparation led to a large number of recipes/remedies against wounds, lameness, bronchitis, colic, anorexia, dermatitis, weakness, parasitism (internal & external), fever, heat stress, urine retention, swelling, toxemia, and indigestion.
Conclusions
This study generated lot of data on phytomedicinal approach for the treatment of ailments in the equines in some selected areas. It would, therefore, be imperative to expand similar studies in other parts of Pakistan and elsewhere. Moreover, use of the documented plants may be validated employing standard scientific procedures, which may have their application in the drug discovery/development by the pharmaceutical industry.
Keywords: Phytotherapy, Plants, Equines, Indigenous, Ethnobotanicals, Punjab, Pakistan
Background
Equines (horses, donkeys and mules) are playing key roles in providing an economical draught power to resource-poor countries like Pakistan. Equines suffer from a variety of health conditions that not only hamper optimum performance, but also cause huge losses due to mortality [1]. Parasitism has been reported as the major health issue of equines in Punjab, Pakistan followed by wound, bacterial infections, lameness, bronchitis, dermatitis, and colic [2]. In addition to allopathic/modern medicine, there is extensive use of traditional herbs for the treatment of different diseases in equines all over the world [3]. Ethnobotany has revealed that the indigenous knowledge of a community is a key player in the identification of medicinal plants which have been tested through generations in the human history [4]. Traditional medicine and bio-prospecting [5] may often lead to the development of a new herbal product based on their use by significant numbers of people over the extended periods of time [6]. The plant-based medicines have particularly been found promising as anti-parasitics, stomachics, and in treatment of various respiratory ailments [7]–[12]. So far, only a handful of investigations are reported on the use of plants for different ailments/conditions; however, inventories of plants for phyotherapy in the food animals are extensively reported. The present study was, therefore, carried out to document the plants being used in traditional veterinary practices for equines in some selected peri-urban areas of Punjab (Pakistan) where equines are frequently used for different purposes.
Methods
Study districts
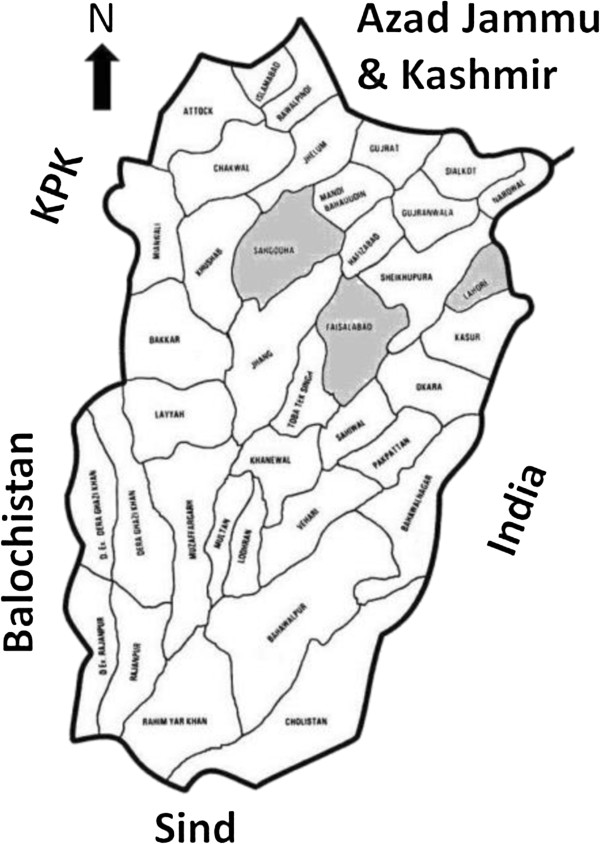
Three districts of the central Punjab; Faisalabad, Lahore and Sargodha were included in the present survey. District Lahore is the capital of Punjab (second largest city of Pakistan after Karachi), while district Faisalabad is the hub of textiles (third largest city) of the country. District Sargodha is comparatively smaller city and considered as an agricultural trade center with various industries. The equine population of the three districts has been estimated as 24628 horses, 174994 donkeys and 7849 mules [13]. The use of equines in the three selected industrial districts of Punjab is frequent because it is the cheapest source for carriage of industrial raw materials and products from and to the market [2]. Figure 1 shows physical map of Punjab province and the three study districts.
Figure 1.
Physical map of the Punjab province, Pakistan indicating districts Faisalabad, Sargodha and Lahore.
Selection of respondents
A small scaled rapid rural appraisal (RRA), an exploratory phase [14] was conducted in metropolitan Faisalabad, Punjab, Pakistan for the purpose of collecting an initial data from candidates who could participate in the second (surveillance) phase of the project.
Of the total 1000 registered farmers (who submitted their willingness to participate in the survey), 450 were selected as key respondents for this study. One hundred and fifty respondents represented each of the three districts of Faisalabad, Lahore and Sargodha. Selection of respondents within each district was done using proportional allocation and map grid methods in order to collect information from the selected districts. The selected respondents belonged to 9 sites each of districts Faisalabad and Sargodha, and 6 sites of Lahore (Table 1).
Table 1.
List of district wise sites for selection of respondents
| Districts/sites | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| Faisalabad |
Sidhupura |
Chak 79 |
Ahmad Nagar |
Pansera |
Chakera |
Naitheri wala |
Aziz Town |
Karad Wala |
Brooke Hospital for Animal Static Clinic (UAF) |
| Sargodha |
Noor colony |
Chak 87 |
Chak 88 South |
Chak 34 |
Fatima Jinnah Road |
Farooq Colony |
Makam-e-Hayat |
Chak 88 North |
Saido wanan |
| Lahore | Shahdra Town | Fazal Park | Raiwand | Badian | Sharakpur | Thokar Niaz Baig |
Participatory epidemiology and collection of data
A questionnaire containing a blend of open ended and closed (dichotomous and multiple choice) questions was prepared and refined through formal and informal testing [15]. For effective communication and data recording, a survey team was appointed; comprising of a veterinarian, professionals of The Brooke Hospital for Animals, and a community leader from the local village. Interviews, focused group discussions, and field visits were conducted with the respondents. The information about disease recognition of the equines and their treatments was collected using the well-structured questionnaire, open-ended interviews and guided-dialogue techniques. Focused group discussions were arranged to cross-check/verify the information provided by the respondents to reach more accurate results. The respondents were asked to tell how they acquired the knowledge of phytotherapy related to the disease/condition recognition of equines. In addition, the direct observation approach was also followed as described by Etkins [16]. Thus, local names of plants, dose, parts of plant used, methods of preparation, and mode of administration were recorded. The farmers were asked to show the plant species described for the treatment of diseases/conditions for their taxonomic identification by the botanists at the Department of Botany, University of Agriculture, Faisalabad, Pakistan and the voucher specimens were preserved for record. The information collected was maintained in Microsoft Excel for further analyses and interpretation.
Results
Respondents
Equine owners/traditional veterinary healers were well familiar with the signs and symptoms of the diseases/conditions of equines in the study area and a majority of the botanical ingredients used in treatment were of indigenous origin. Therefore, farmers had these remedies available at their door step or at the most in the nearby grocery shops. The respondents were not trained by any authority about usage of plants for treatment of their animals. In fact, their knowledge was based on folk beliefs and previous practices based on hit and trial methods.
Diversity of plants used
A total of 60 plants were documented (Table 2) for their use in different diseases/conditions of equines. Documented plants represented 40 families. Fabaceae was the largest represented family including five plants, followed by other families (Table 2). Composition, dosage, mode of preparation and administration, and frequency of usage of Traditional Veterinary Practices (TVPs) has been presented in Table 3. Plants and diversity of their usage in different diseases have been presented in Table 4. Thirty one species were used for the treatment of multiple diseases/conditions. Piyaz (Onion; Allium cepa), Adrak (Ginger; Zingiber officinale), Kali zeeri (Iron weed; Vernonia anthelmintica), Mirch (Chilli; Capsicum annum), Sarsoon (Rapeseed plany; Brassica campestris), Ajwain (Carom seeds; Trachyspermum ammi), Ajwain (Dill; Anethum graveolens), Kutka (Picrorhiza kurroa), Neem (Azadirachta indica), and Kor tumma (Bitter gourd; Citrullus colocynthis) were the top ten most frequently used plants as part of prescriptions in different diseases/conditions of equines.
Table 2.
An inventory of floral diversity documented by local respondents (n=450) from three districts (Faisalabad, Sargodha and Lahore) of Punjab, Pakistan for the treatment of equine disease
|
Sr. |
Botanical name/ |
Local name | Family | Part (s) used | Usage diversity |
No. of |
Part of |
|---|---|---|---|---|---|---|---|
| No. | English name | prescriptions | remedies | ||||
| 1. |
Acacia nilotica (L.) Willd. ex Delile |
Desi kikar |
Fabaceae |
Branches |
Internal parasites, swelling |
2 |
2 |
| 2. |
Allium cepa L. var. aggregatum G. Don |
Piyaz |
Liliaceae |
Bulb |
Anorexia, bad habits, bronchitis, colic, diarrhea, fever, heat stress, indigestion, pain, quidding, weakness |
11 |
33 |
| 3. |
Allium sativum L. |
Lehsan |
Liliaceae |
Bulb |
Bronchitis, fever, indigestion |
3 |
3 |
| 4. |
Aloe vera (L.) Burm. f. |
Kawar gandal |
Aloaceae |
Leaves |
Anorexia, bronchitis |
2 |
2 |
| 5. |
Amomum subulatum Roxb. |
Ilaichi |
Zingiberaceae |
Fruit |
Fever |
1 |
1 |
| 6. |
Anethum graveolens L. |
Soye |
Umbelliferae |
Seeds |
Anorexia, bronchitis, colic, fever, indigestion, lameness, toxemia, weakness |
8 |
10 |
| 7. |
Azadirachta indica A. Juss. |
Neem |
Meliaceae |
Leaves |
Dermatitis, external parasites, lameness, wound |
5 |
13 |
| 8. |
Bambusa bambos L. |
Bans |
Bambusaceae |
Leaves |
Bronchitis |
1 |
1 |
| 9. |
Brassica campestris L. ssp. napus Duthie and Fuller |
Surson |
Brassicaseae |
Seeds, seed oil |
Colic, dermatitis, diarrhea, external parasites, lameness, retention of urine, swelling, weakness, wound |
8 |
47 |
| 10. |
Calotropis procera (Ait.) W.T.Ait. |
Aak |
Asclepiadaceae |
Buds |
Weakness |
1 |
1 |
| 11. |
Capsicum annum L. |
Subz mirch |
Solanaceae |
Fruit |
Anorexia, bronchitis, fever, indigestion, lameness, quidding, retention of urine, toxemia, weakness |
9 |
19 |
| 12. |
Cascuta reflexa Roxb. |
Akas bail |
Cuscutaceae |
Whole plant |
Lameness |
1 |
1 |
| 13. |
Cicer arietinum L. |
Kalay chaney |
Fabaceae |
Seeds |
Dermatitis, lameness, wound |
3 |
4 |
| 14. |
Citrullus colocynthis (L.) Schrad. |
Kor tumma |
Cucurbitaceae |
Fruit |
Anorexia, fever, indigestion, weakness |
4 |
9 |
| 15. |
Citrus limon (L.) Burm. |
Nimbu |
Rutaceae |
Fruit |
Lameness, wound |
2 |
2 |
| 16. |
Cocos nucifera L. |
Giri |
Arecaceae |
Oil |
Lameness |
1 |
1 |
| 17. |
Curcuma longa L. |
Haldi |
Zingiberaceae |
Rhizome |
External parasite, lameness, wound |
3 |
8 |
| 18. |
Eruca sativa Mill. |
Tara mera |
Cruciferae |
Seed, seed oil |
Dermatitis, external parasite, wound |
3 |
5 |
| 19. |
Eugenia caryophyllata Thunb. |
Loung |
Myrtaceae |
Fruit |
Anorexia, lameness, pain |
3 |
4 |
| 20. |
Euphorbia caducifolia Haines. |
Danda thor |
Euphorbiaceae |
Branches |
Colic |
1 |
1 |
| 21. |
Ficus religiosa L. |
Pipal |
Moraceae |
Bark |
Swelling |
1 |
1 |
| 22. |
Foeniculum vulgare P. Mill. |
Sounf |
Apiaceae |
Seeds |
Indigestion, weakness |
2 |
2 |
| 23. |
Geranium wallichianum D. Don Ex Sweet |
Ratan jot |
Geraniaceae |
Seeds |
Lameness, wound |
2 |
4 |
| 24. |
Glycyrrhiza glabra L. |
Mullathi |
Fabaceae |
Roots |
Bronchitis |
1 |
7 |
| 25. |
Grewia asiatica L. |
Falsa |
Tiliaceae |
Fruit |
Lameness |
1 |
1 |
| 26. |
Halorrhena pubescens Wall. ExG. Don. |
Kuro |
Apocynaceae |
Bark |
Heat stress |
1 |
1 |
| 27. |
Hordeum vulgare L. |
Jow |
Poaceae |
Seeds |
Heat stress |
1 |
1 |
| 28. |
Lagenaria siceraria Molina |
Kuddo |
Cucurbitaceae |
Leaves |
Internal parasite |
1 |
1 |
| 29. |
Lawsonia inermis L. |
Mehndi |
Lythraceae |
Leaves |
Wound |
1 |
7 |
| 30. |
Lens culinaris Medik. |
Masoor |
Fabaceae |
Seeds |
Wound |
1 |
1 |
| 31. |
Lepidium sativum L. |
Halion |
Apiaceae |
Seeds |
Internal parasites, weakness |
2 |
2 |
| 32. |
Linum usitatissimum L. |
Alsi |
Linaceae |
Seeds |
Internal parasites |
1 |
1 |
| 33. |
Mallotus philippinensis (Lamk.) Meull. Arg. |
Kamela |
Euphorbiaceae |
Fruit |
Anorexia, internal parasites |
2 |
4 |
| 34. |
Mangifera indica L. |
Aam |
Anacardiaceae |
Fruit |
Lameness |
1 |
1 |
| 35. |
Medicago sativa L. |
Lusan |
Papilionaceae |
Leaves |
Lameness |
1 |
1 |
| 36. |
Mentha longifolia (L.) Huds. |
Podina |
Lamiaceae |
Leaves |
Anorexia |
1 |
1 |
| 37. |
Myristica fragrans HOUTT. |
Jaful |
Myristicaceae |
Fruit |
Lameness, pain, tetanus |
3 |
5 |
| 38. |
Nicotiana tabacum L. |
Tambaku |
Solanaceae |
Leaves |
Colic, pain |
2 |
3 |
| 39. |
Nigella sativa L. |
Kalonji |
Ranunculaceae |
Seeds |
Anorexia, bronchitis |
2 |
2 |
| 40. |
Olea europaea L. |
Zaytoon |
Oleaceae |
Fruit |
Lameness |
1 |
1 |
| 41. |
Oryza sativa L. |
Chawal |
Poaceae |
Whole plant |
Internal parasites |
1 |
1 |
| 42. |
Peganum harmala L. |
Hurmil |
Zygophyllaceae |
Fruit |
Anorexia, lameness, pain, swelling |
4 |
4 |
| 43. |
Pennisetum glaucum L. |
Bajra |
Poaceae |
Whole |
Lameness |
1 |
1 |
| 44. |
Picrorhiza kurroa Royle ex. Benth. |
Kourdh |
Scrofulariaceae |
Rhizome |
Anorexia, fever, indigestion, lameness, tetanus, weakness |
6 |
11 |
| 45. |
Piper betle L. |
Paan |
Piperaceae |
Leaves |
Anorexia |
1 |
1 |
| 46. |
Piper nigrum L. |
Kali mirch |
Piperaceae |
Pepper corn |
Anorexia, bronchitis, toxemia |
3 |
5 |
| 47. |
Prunus dulcis Mill. |
Badam |
Rosaceae |
Seed |
Diarrhea |
1 |
1 |
| 48. |
Ricinus communis L. |
Arind |
Euphorbiaceae |
Flower oil |
Internal parasites |
1 |
1 |
| 49. |
Rosa damascena Mill. |
Gulab |
Rosaceae |
Flowers |
Bronchitis |
1 |
4 |
| 50. |
Sesamum indicum L. |
Til |
Pedaliaceae |
Seeds, seed oil |
Colic, dermatitis, lameness, pain |
4 |
7 |
| 51. |
Trachyspermum ammi (L.) Sprague ex Turrill. |
Ajwain |
Apiaceae |
Seeds |
Anorexia, bronchitis, colic, fever, heat stress, indigestion, lameness, retention of urine |
8 |
19 |
| 52. |
Trifolium alexandrinum L. |
Barseem |
Papilionaceae |
Whole plant |
Wound |
1 |
1 |
| 53. |
Trigonella foenum-graecum L. |
Methray |
Fabaceae |
Seeds |
Toxemia |
1 |
1 |
| 54. |
Triticum aestivum L. |
Gundum |
Poaceae |
Flour, grain |
External parasites, lameness, weakness, wound |
4 |
5 |
| 55. |
Vernonia anthelmintica (L.) Willd. |
Kali zeeri |
Asteraceae |
Seeds |
Anorexia, bronchitis, colic, diarrhea, heat stress, indigestion, lameness, toxemia, + Weakness+ Wound |
10 |
23 |
| 56. |
Withania coagulans Dunal |
Paneer |
Solanaceae |
Leaves |
Anorexia, fever, indigestion, weakness |
4 |
4 |
| 57. |
Withania somnifera L. Dunal |
Aksan |
Solanaceae |
Leaves |
Wound |
1 |
1 |
| 58. |
Zea mays L. |
Makai |
Gramineae |
Flour |
Anorexia, haematuria, weakness, wound |
4 |
5 |
| 59. |
Zingiber officinale Roscoe |
Adrak |
Zingiberaceae |
Rhizome |
Anorexia, bronchitis, colic, fever, heat stress, indigestion, lameness, pain, tetanus, weakness |
10 |
26 |
| 60. | Ziziphus jujuba L. Lam., non P. Mill. | Beri | Rhamnaceae | Leaves | Wound | 1 | 1 |
Table 3.
List of traditional veterinary practices based on plant materials for the treatment of different diseases/conditions of equines reported by the local respondents (n=450) in the study area
|
S. |
Phytotherapeutic material used |
Dose and administration |
Usage |
|---|---|---|---|
|
No. |
|
|
|
| Anorexia | |||
| 1 |
Zingiber officinale (rhizome) + Capsicum annum (fruit) + Allium cepa (bulb) + Common salt |
50 g + 125 g + 250 g + 125 g; MGB/PO (Mix, Grind, and make a Bolus to administer Per Oss) |
2 |
| 2 |
Allium cepa (bulb) + Citrullus colocynthis (fruit) + Capsicum annum (fruit) + Zingiber officinale (rhizome) + Jaggery |
125 g + 50 g + 125 g + 50 g + 100 g; MGB/PO |
1 |
| 3 |
Allium cepa (bulb) + Zingiber officinale (rhizome) + Black salt |
250 g + 100 g + 100 g; MGB/PO - 2-3 days |
1 |
| 4 |
Capsicum annum (fruit) + Allium cepa (bulb) + Vernonia anthelmintica (seeds) + Eugenia caryophyllata (fruit) + Zingiber officinale (rhizome) + Common salt |
500 g + 250 g + 250 g + 100 g + 250 g + 250 g; MGB/PO |
1 |
| 5 |
Capsicum annum (fruit) + Allium cepa (bulb) + Zingiber officinale (rhizome) + Trachyspermum ammi (seeds) + Nigella sativa (seeds) + Black salt + Common salt + Picrorhiza kurroa (rhizome) + Citrullus colocynthis (fruit) + Peganum harmala (fruit) |
125 g + 125 g + 50 g + 25 g + 50 g + 50 g + 50 g + 50 g + 50 g; MGB/PO – divide into 02 doses for 02 days |
1 |
| 6 |
Common salt + Allium cepa (bulb) + Capsicum annum (fruit) |
125 g + 250 g + 125 g; MGB/PO |
1 |
| 7 |
Common salt + Black salt + Allium cepa (bulb) + Piper nigrum (pepper corn) + Vernonia anthelmintica (seeds) + Trachyspermum ammi (seeds) |
50 g + 50 g + 50 g + 25 g + 25 g + 25 g; MGB/PO |
1 |
| 8 |
Zea mays (flour) + Brown sugar |
250 g + 250 g; MGB/PO |
1 |
| 9 |
Zea mays (flour) + Brown sugar + Water |
250 g + 250 g + 5 L; Mix and give PO |
1 |
| 10 |
Jaggery + Allium cepa (bulb) |
250 g + 500 g; MGB/PO |
1 |
| 11 |
Mallotus philippinensis (fruit) + Yogurt |
10 g + 125 g; MGB/PO |
1 |
| 12 |
Mentha longifolia (leaves) + Capsicum annum (fruit) + Common salt + Allium cepa (bulb) |
125 g + 50 g + 50 g + 125 g; MGB/PO |
1 |
| 13 |
Picrorhiza kurroa (rhizome) + Citrullus colocynthis (fruit) + Aloe vera (leaves) + Allium cepa (bulb) |
125 g + 125 g + 50 g; MGB/PO |
1 |
| 14 |
Piper nigrum (pepper corn) + Black salt + Vernonia anthelmintica (seeds) + Capsicum annum (fruit) |
50 g + 25 g + 25 g + 25 g; MGB/PO |
1 |
| 15 |
Trachyspermum ammi (seeds) + Vernonia anthelmintica (seeds) + Jaggery |
25 g + 50 g + 125 g; MGB/PO |
1 |
| 16 |
Trachyspermum ammi (seeds) + Zingiber officinale (rhizome) + Piper nigrum (pepper corn) + Piper betle (leaves) + Jaggery |
50 g + 50 g + 50 g + 25 g + 250 g; MGB/PO |
1 |
| 17 |
Vernonia anthelmintica (seeds) + Anethum graveolens (seeds) + Black salt + Zingiber officinale (rhizome) + Withania coagulans (leaves) + Common salt + Picrorhiza kurroa (rhizome) + Citrullus colocynthis (fruit) + Jaggery + Allium cepa (bulb) + Capsicum annum (fruit) |
125 g + 125 g + 12 g + 50 g + 250 g + 50 g + 250 g + 500 g + 250 g + 250 g + 250 g; MGB/PO |
1 |
| 18 |
Zingiber officinale (rhizome) + Allium cepa (bulb) + Capsicum annum (fruit) + Vernonia anthelmintica (seeds) + Black salt |
125 g + 1 kg + 250 g + 50 g + 250 g; MGB/PO |
1 |
| |
Total entries |
|
19 |
| |
Bad habit (Mud eating) |
|
|
| 1 |
Jaggery + Allium cepa (bulb) |
250 g + 250 g; Boiled bulbs mixed with jiggery – given PO |
1 |
| |
Total entries |
|
1 |
| |
Bronchitis |
|
|
| 1 |
Glycyrrhiza glabra (roots) + Jaggery |
250 g + 250 g; MGB/PO – 2-3 days |
4 |
| 2 |
Jaggery + Allium cepa (bulb) |
250 g + 250 g; MGB/PO – 2-3 days |
4 |
|
3 |
Nuswar |
10 g nuswar pushed in nose with a pipe |
3 |
| 4 |
Glycyrrhiza glabra (roots) + Rosa damascena (flowers) + Piper nigrum (pepper corn) |
250 g + 375 g + 25 g; MGB/PO – 2-3 days |
2 |
| 5 |
Glycyrrhriza glabra (roots) + Zingiber officinale (rhizome) + Allium cepa (bulb) + Jaggery |
50 g + 50 g + 125 g + 125 g; MGB/PO |
2 |
| 7 |
Bumbusa bambos (leaves) |
500 g PO |
1 |
| 8 |
Glycyrrhiza glabra (roots) + Allium cepa (bulb) + Nigella sativa (seeds) + Ammonium chloride + Jaggery |
250 g + 2 kg + 250 g + 125 g + 2 kg; Mixed, ground and fried to make custard – 125 g daily for 5 days |
1 |
| 9 |
Glycyrrhriza glabra (roots) + Jaggery + Allium cepa (bulb) |
50 g + 250 g + 250 g; MGB/PO |
1 |
| 10 |
Glycyrrhiza glabra (roots) + Jaggery + Vernonia anthelmintica (seeds) + Anethum graveolens (seeds) + Allium cepa (bulb) |
25 g + 250 g + 25 g + 25 g + 250 g; MGB/PO |
1 |
| 11 |
Glycyrrhiza glabra (roots) + Rosa damascena (flowers) + Allium cepa (bulb) |
125 g + 250 g + 500 g; MGB/PO |
1 |
| 12 |
Glycyrrhiza glabra (roots) + Rosa damascena (flowers) + Ammonium chloride + Piper nigrum (pepper corn) + Allium cepa (bulb) + Jaggery + Water |
125 g + 125 g + 25 g + 25 g + 250 g + 125 g + 125 ml; Mixed, fried and made custard – given PO |
1 |
| 13 |
Glycyrrhiza glabra (roots) + Rosa damascena (flowers) + Zingiber officinale (rhizome) |
125 + 125 g + 125 g; MGB/PO |
1 |
| 14 |
Aloe vera (leaves) + Capsicum annum (fruit) + Zingiber officinale (rhizome) + Allium sativum (bulb) + Vernonia anthelmintica (seeds) |
125 g + 125 g + 50 g + 50 g + 50 g; MGB/PO |
1 |
| 15 |
Jaggery + Allium cepa (bulb) + Glycyrrhiza glabra (roots) + Zingiber officinale (rhizome) + Piper nigrum (pepper corn) |
250 g + 500 g + 100 g + 100 g + 50 g; MGB/PO |
1 |
| 16 |
Joshanda + Jaggery + Allium cepa (bulb) + Water |
1 kg + 1 kg + 2 kg + 2 L; Mixed, boiled in water till concentrated – given PO |
1 |
| 17 |
Rosa damascena (flowers) + Glycyrrhiza glabra (roots) + Ammonium chloride |
375 g + 50 g + 10 g; MGB/PO |
1 |
| 18 |
Trachyspermum ammi (seeds) + Jaggery + Common salt |
100 g + 200 g + 50 g; MGB/PO |
1 |
| 19 |
Trachyspermum ammi (seeds) + Vernonia anthelmintica (seeds) + Jaggery |
25 g + 25 g + 125 g; MGB/PO |
1 |
| |
Total entries |
|
28 |
| |
Colic |
|
|
| 1 |
Brassica campestris (seed oil) |
500 ml – PO |
2 |
| 2 |
Brassica campestris (seed oil) + Water |
250 ml + 250 ml – PO |
2 |
| 3 |
Nicotiana tabacum (leaves) + Jaggery |
50 g + 250 g; MGB/PO |
2 |
| 6 |
Allium cepa (bulb) |
500 g juice – PO |
1 |
| 7 |
Ammonium chloride + Brassica campestris (seed oil) + Common salt |
50 g + 125 ml + 50 g; Mix and give PO |
1 |
| 8 |
Ammonium chloride + Potassium bicarbonate |
50 g + 50 g; MGB/PO |
1 |
| 9 |
Euphorbia caducifolia (branches) + Water |
10 ml juice mixed in 250 ml water – PO |
1 |
| 11 |
Jaggery + Allium cepa (bulb) |
250 g + 250 g; MGB/PO |
1 |
| 12 |
Jaggery + Nicotiana tabacum (leaves) |
250 g + 50 g; Mix and give PO |
1 |
| 13 |
Sodium carbonate + Jaggery + 7up |
125 g + 250 g + 250 ml; Bolus followed by 7up |
1 |
| 14 |
Potassium nitrate + Potassium bicarbonate + Hukka water |
25 g + 25 g + 250 ml; Mix and give PO |
1 |
| 15 |
Trachyspermum ammi (seeds) + Soap + Common salt + Water |
125 g + 125 g + 250 g + 2 L; Decoction given PO |
1 |
| 16 |
Sesamum indicum (seeds) |
500 ml PO |
1 |
| 17 |
Trachyspermum ammi (seeds) + Anethum graveolens (seeds) + Jaggery + White salt |
50 g + 50 g + 250 g + 125 g; MGB/PO |
1 |
| 18 |
Trachyspermum ammi (seeds) + Vernonia anthelmintica (seeds) + Jaggery + Brassica campestris (seed oil) + Water |
50 g + 50 g + 250 g + 250 ml + 250 ml; Decoction PO |
1 |
| 19 |
Vernonia anthelmintica (seeds) + Zingiber officinale (rhizome) + Milk + Water |
50 g + 50 g + 250 ml + 250 ml; Grind and give PO |
1 |
| |
Total entries |
|
22 |
| |
Dermatitis |
|
|
| 1 |
Brassica campestris (seed oil) |
50-100 ml; Topical application |
5 |
| 2 |
Hukka water |
Topical application |
5 |
| 3 |
Eruca sativa (seed oil) |
100 ml; Topical application |
2 |
| 4 |
Eruca sativa (seed oil) + Sulfur |
250 ml + 50 g; Topical application |
2 |
| 6 |
Cicer arietinum (seeds) + Eruca sativa (seed oil) |
250 g + 250 ml; GMB/PO |
1 |
| 7 |
Azadirachta indica (leaves) + Alum + Common salt + Water |
250 g + 25 g + 50 g + 3 L; Decoction applied topically |
1 |
| 8 |
Brassica campestris (seed oil) + Eruca sativa (seed oil) |
50 ml + 50 ml; Topical application (massage) |
1 |
| 9 |
Brassica campestris (seed oil) + Jaggery |
50 ml + 50 g; Topical application |
1 |
| 10 |
Brassica campestris (seed oil) + Yogurt |
Topical application |
1 |
| 13 |
Eruca sativa (seeds) + Common salt |
Topical application |
1 |
| 14 |
Sesamum indicum (seed oil) |
50 ml; Topical application |
1 |
| |
Total entries |
|
21 |
| |
Diarrhea |
|
|
| 1 |
Allium cepa (bulb) + Common salt |
2 bulbs + 50 g; MGB/PO |
1 |
| 2 |
Citrullus colocynthus (fruit) + Vernonia anthelmintica (seeds) + Black salt + Common salt |
50 g + 50 g + 50 g + 50 g; MGB/PO |
1 |
| 3 |
Milk + Brassica campestris (seed oil) |
250 ml + 125 ml; Decoction given PO |
1 |
| 4 |
Prunus dulcis (seeds) + Jaggery |
7-10 seeds + 250 g; MGB/PO |
1 |
| 5 |
Vernonia anthelmintica (seeds) + Black salt + Citrillus colocynthus (fruit) |
50 g + 50 g + 50 g; MGB/PO |
1 |
| |
Total entries |
|
5 |
| |
External parasite |
|
|
| 3 |
Azadirachta indica (leaves) + Water |
250 g + 1 L; Topical application of decoction |
2 |
| 4 |
Brassica campestris (seed oil) + Sump oil |
125 ml + 125 ml; Topical application |
1 |
| 5 |
Brassica campestris (seed oil) + Kerosene oil |
250 ml + 125 ml; Topical application |
1 |
| 6 |
Curcuma longa (rhizome) |
Topical application of powder |
1 |
| 7 |
Eruca sativa (seeds) + Triticum aestivum (flour) |
50 g + 250 g; MGB/PO |
1 |
| 9 |
Brassica campestris (seeds) |
Topical application of ground seeds |
1 |
| |
Total entries |
|
11 |
| |
Eye problem |
|
|
| |
Total entries |
|
2 |
| |
Fever |
|
|
| 1 |
Vernonia anthelmintica (seeds) + Anethum graveolens (seeds) + Black salt + Zingiber officinale (rhizome) + Withania coagulans (leaves) + Common salt + Picrorhiza kurroa (rhizome) + Citrullus colocynthis (fruit) + Jaggery + Allium cepa (bulb) + Capsicum annum (fruit) |
125 g + 125 g + 12 g + 50 g + 250 g + 50 g + 250 g + 500 g + 250 g + 250 g + 250 g; GMB for 8 days and give in equal doses PO |
2 |
| 2 |
Allium cepa (bulb) + Capsicum annum (fruit) + Zingiber officinale (rhizome) + Jaggery + Allium sativum (bulb) |
125 g + 50 g + 25 g + 125 g + 25 g; GMB/PO |
1 |
| 3 |
Black salt + Trachyspermum ammi (seeds) |
125 g + 50 g PO |
1 |
| 4 |
Common salt + Trachyspermum ammi (seeds) + Water |
50 g + 50 g + 50 ml; MGB/PO |
1 |
| 7 |
Jaggery + Amomum subulatum (fruit) |
250 g + 50 g; MGB/PO |
1 |
| 9 |
Piper nigrum (pepper corn) + Trachyspermum ammi (seeds) + Water + Sugar |
500 g + 100 g + 500 ml + 1 kg; Mix, fry and make custard – 250 g daily for 5 days |
1 |
| |
Total entries |
|
10 |
| |
Haematuria |
|
|
| 1 |
Butter + Piper nigrum (pepper corn) |
125 g + 25 g; MGB/PO |
1 |
| 2 |
Zea mays (flour) + Brown sugar + Water |
500 g + 500 g + 2 L PO |
1 |
| 3 |
Potassium bicarbonate + Potassium nitrate |
50 g + 50 g PO |
1 |
| |
Total entries |
|
4 |
| |
Heat stress |
|
|
| 1 |
Trachyspermum ammi (seeds) + Common salt |
50 g + 125 g; Soak seeds overnight, grind and mix with salt – give PO |
2 |
| 2 |
Allium cepa (bulb) + Jaggery |
250 g + 250 g; Half boil bulbs, mix in jiggery and give PO |
1 |
| 3 |
Dalda ghee + Vernonia anthelmintica (seeds) |
125 g + 50 g; MGB/PO |
1 |
| 4 |
Trachyspermum ammi (seeds) + Jaggery |
250 g + 250 g PO |
1 |
| 5 |
Vernonia anthelmintica (seeds) + Sugar |
50 g + 125 g; MGB/PO |
1 |
| 6 |
Water |
As much as animal can drink |
1 |
| 7 |
Zingiber officinale (rhizome) + Halorrhena pubescens (bark) + Black salt + Common salt + Water |
50 g + 50 g + 25 g + 25 g + 1 L; Soak all in earthen utensil for 24 hrs; PO |
1 |
| 8 |
Hordeum vulgare (seeds) + Water |
2 kg + 4 L; Soak overnight; PO |
1 |
| |
Total entries |
|
9 |
| |
Indigestion |
|
|
| 1 |
Capsicum annum (fruit) + Allium cepa (bulb) + Vernonia anthelmintica (seeds) + Trachyspermum ammi (seeds) + Zingiber officinale (rhizome) + Jaggery + Citrullus colocynthis (fruit) + Black salt + Common salt |
50 g + 250 g + 50 g + 50 g + 50 g + 100 g + 100 g + 100 g + 100 g; MGB/PO |
1 |
| 2 |
Citrullus colocynthis (fruit) + Picrorhiza kurroa (rhizome) + Vernonia anthelmintica (seeds) + Black salt + Ammonium chloride |
100 g + 10 g + 10 g + 50 g + 3 balls; Mixed in hot water and given PO |
1 |
| 3 |
Jaggery + Trachyspermum ammi (seeds) + Zingiber officinale (rhizome) + Allium cepa (bulb) + Allium sativum (bulb) |
250 g + 50 g + 50 g + 250 g + 50 g; PO |
1 |
| 4 |
Vernonia anthelmintica (seeds) + Anethum graveolens (seeds) + Black salt + Zingiber officinale (rhizome) + Withania coagulans (leaves) + Common salt + Picrorhiza kurroa (rhizome) + Citrullus colocynthis (fruit) + Jaggery + Allium cepa (bulb) + Capsicum annum (fruit) |
125 g + 125 g + 12 g + 50 g + 250 g + 50 g + 250 g + 500 g + 250 g + 250 g + 250 g; MGB/PO, equally divided in 8 balls and given one daily |
1 |
| 5 |
Zingiber officinale (rhizome) + Trachyspermum ammi (seeds) + Foeniculum vulgare (seeds) + Black salt + Jaggery |
50 g + 50 g + 50 g + 50 g + 250 g; MGB/PO |
1 |
| |
Total entries |
|
5 |
| |
Internal parasites |
|
|
| 1 |
Mollotus philipinensis (fruit) + Jaggery |
50 g + 250 g PO |
6 |
| 2 |
Mallotus philippinensis (fruit) + Yogurt |
10 g + 125 g PO |
3 |
| 3 |
Acacia nilotica (branches) + Jaggery |
125 g + 125 g PO |
1 |
| 4 |
Jaggery + Azadirachta indica (leaves) |
250 g + 500 g; Jaggery 10 minutes before A. indica leaves PO |
1 |
| 5 |
Jaggery + Oryza sativa (whole plant) |
250 g + 1 kg; Give Jaggery on first day and O. sativa next day |
1 |
| 6 |
Jaggery + Yogurt + Mollotus philpinensis (fruit) |
125 g + 250 g + 50 g PO |
1 |
| 7 |
Lagenaria siceraria (leaves) |
250 g; Ground and given PO |
1 |
| 8 |
Linum usitatissimum (seeds) + Lepidium sativum (seeds) + Jaggery + Mallotus philippinensis (fruit) |
60 g + 60g + 250 g + 25 g; PO |
1 |
| 9 |
Mallotus philippinensis (fruit) + Milk whey |
10 g + 250 ml PO |
1 |
| 10 |
Nurru (stem) + Jaggery |
250 g + 250 g; Given jaggery first and then nurru |
1 |
| 11 |
Ricinus cummunis (flower oil) |
250 ml oil PO |
1 |
| 12 |
Ricinus cummunis (flower oil) |
250 ml PO |
1 |
| |
Total entries |
|
31 |
| |
Lameness |
|
|
| 1 |
Brassica campestris (seed oil) |
50-100 ml; Topical application |
8 |
| 2 |
Sesamum indicum (seed oil) |
50 ml; Topical application |
4 |
| 3 |
Copper sulfate + Jaggery |
10 g + 100 g PO |
3 |
| 5 |
Citrus limon (fruit) |
Half piece for massage on the affected site |
2 |
| 7 |
Brassica campestris (seed oil) + Kerosene oil |
50 ml + 50 ml; Topical application |
1 |
| 12 |
Azadirachta indica (leaves) + Common salt + Water |
250 g + 250 g + 6 Lit; Topical application of decoction |
1 |
| 13 |
Azadirachta indica (leaves) + Water |
100 g + 1 L; Topical application of decoction |
1 |
| 14 |
Azadirachta indica (leaves) + Water + Common salt + Alum |
250 g + 4 L + 1 kg + 250 g; Topical application of decoction |
1 |
| 15 |
Brassica campestris (seed oil) + Kerosene oil + Capsicum annum (fruit) |
50 ml + 50 ml + 25 g; Topical application |
1 |
| 16 |
Brassica campestris (seed oil) |
Topical application of semi-hot oil |
1 |
| 17 |
Cascuta reflexa (whole plant) + Ghee |
C. reflexa fried in oil; Topical application |
1 |
| 18 |
Cicer arietinum (seeds) |
50 g grains tied on affected area by putting in a cloth bag |
1 |
| 19 |
Cicer arietinum (seeds) + Jute bag |
250 g grains tied on affected area by putting in a jute bag |
1 |
| 21 |
Common salt + Triticum aestivum (flour) + Water |
Topical application of hot mixture |
1 |
| 22 |
Geranium wallichianum (seeds) + Brassica campestris (seed oil) |
50 g + 50 ml; Mix, fry and apply topically |
1 |
| 23 |
Geranium wallichianum (seeds) + Brassica campestris (seed oil) |
50 g + 50 ml; Mix, fry and apply topically |
1 |
| 24 |
Jaggery + Curcuma longa (rhizome) |
250 g + 50 g; MGB/PO |
1 |
| 27 |
Medicago sativa (leaves) + Common salt |
500 g + 100 g; Mix and apply on the affected area for 2-3 days |
1 |
| 28 |
Mangifera indica (fruit) |
Topical application on the lesion |
1 |
| 29 |
Myristica fragrans (fruit) + Geranium wallichianum (seeds) + Eugenia caryophyllata (fruit) + Sesamum indicum (seeds oil) + Brassica campestris (seed oil) |
50 g + 50 g + 50 g + 250 ml + 250 ml; Topical application |
1 |
| 30 |
Olea europaea (fruit) + Cocus nucifera (oil) + Fish + Sump oil |
250 ml + 250 ml + 250 ml + 250 ml; Topical application |
1 |
| 31 |
Pennisetum glaucum (whole) + Jaggery |
125 g + 125 g; MGB/PO |
1 |
| 32 |
Peganum harmala (fruit) + Alum + Jaggery |
Topical application |
1 |
| 34 |
Sesamum indicum (seeds) + Eugenia caryophyllata (fruit) + Myristica fragrans (fruit) |
125 ml + 10 g + 50 g; Topical hot application |
1 |
| 35 |
Trachyspermum ammi (seeds) + Anethum graveolens (seeds) + Vernonia anthelmintica (seeds) + Jaggery |
125 g + 125 g + 50 g + 500 g; MGB/PO |
1 |
| 36 |
Vernonia anthelmintica (seeds) + Anethum graveolens (seeds) |
250 g + 250 g; 50 g daily |
1 |
| 37 |
Water + Triticum aestivum (flour) + Common salt + Alum |
2 L + 500 g + 125 g + 25 g; Topical application of decoction |
1 |
| 38 |
Zingiber officinale (rhizome) + Picrorhiza kurroa (rhizome) + Vernonia anthelmintica (seeds) + Grewia asiatica (fruit) + Jaggery |
250 g + 250 g + 250 g + 250 g + 250 g; GMB/PO |
1 |
| 39 |
Ricinus cummunis (bark) + Sesamum indicum (seeds oil) |
250 g + 250 ml; Boiled bark in seed oil and applied on affected part for 2-3 days |
1 |
| |
Total entries |
|
58 |
| |
Pain associated with infection |
|
|
| 1 |
Sesamum indicum (seed oil) + Eugenia caryophyllata (fruit) + Myristica fragrans (fruit) |
125 ml + 25 g + 25 g; Mixed, fried and applied topically |
1 |
| 2 |
Sodium carbonate + Jaggery |
One spoon + 250 g; MGB/PO |
1 |
| 3 |
Nicotiana tabacum (leaves) + Jaggery |
50 g + 250 g; MGB/PO |
1 |
| 4 |
Zingiber officinale (rhizome) + Allium cepa (bulb) + Glycyrrhiza glabra (roots) + Capsicum annum (fruit) + Water |
1 kg + 3 kg + 1 kg + 1 kg + 1 litre; MGB/PO |
1 |
| 5 |
Alum + Peganum harmala (fruit) + Jaggery |
50 g + 125 g + 125 g; Mix, fry and give PO one spoon a day |
1 |
| |
Total entries |
|
5 |
| |
Quidding |
|
|
| 1 |
Capsicum annum (fruit) + Jaggery + Common salt + Allium cepa (bulb) |
50 g + 250 g + 50 g + 250 g; MGB/PO |
1 |
| |
Total entries |
|
1 |
| |
Retention of urine |
|
|
| 1 |
Capsicum annum (fruit) |
Applied Capsicum annum (fruit) L. on urethral opening |
2 |
| 2 |
Brassica campestris (seed oil) + Milk |
125 ml + 250 ml; PO |
1 |
| 3 |
Brassica campestris (seed oil) + Water |
250 ml + 250 ml; given decoction PO |
1 |
| 7 |
Trachyspermum ammi (seeds) |
125 g seeds soaked overnight in water and given PO |
1 |
| |
Total entries |
|
8 |
| |
Swelling |
|
|
| 1 |
Acacia nilotica (branches) + Ficus religiosa (bark) + Water + Brassica campestris (seed oil) |
250 g + 250 g + 2 L + 25 ml; Topical application of decoction |
1 |
| 2 |
Azadirachta indica (leaves) + Alum + Common salt + Water |
250 g + 50 g + 1 spoon + 2 L; Topical application of decoction |
1 |
| 3 |
Leather + Brassica campestris (seed oil) |
500 g + 500 ml; Heated leather in seed oil and applied on inflammation |
1 |
| 4 |
Peganum harmala (fruit) |
125 g PO |
1 |
| |
Total entries |
|
4 |
| |
Tetanus |
|
|
| 1 |
Egg + Zingiber officinale (rhizome) + Myristica fragrans (fruit) + Picrorhiza kurroa (rhizome) |
One + 25 g + One seed + 25 g; MGB/PO – 3 days |
1 |
| 2 |
Myristica fragrans (fruit) + Picrorhiza kurroa (rhizome) + Jaggery |
One fruit + 25 g + 10 g; MGB/PO and cuts on nose for bleeding |
1 |
| |
Total entries |
|
2 |
| |
Toxemia |
|
|
| 1 |
Capsicum annum (fruit) + Common salt |
250 g + 125 g; PO |
1 |
| 2 |
Capsicum annum (fruit) + Ghee + Water |
250 g + 250 g + 1000 ml; decoction PO |
1 |
| 3 |
Capsicum annum (fruit) + Ghee |
250 g + 250 g; Ground, fried and given PO |
1 |
| 4 |
Capsicum anuum (fruit) + Trigonella foenum-graecum (seeds) + Vernonia anthelmintica (seeds) + Anethum graveolens (seeds) + Water |
1000 g + 500 g + 250 g + 250 g + 10 litre; Boiled and made custard – 200 g daily |
1 |
| 5 |
Piper nigrum (pepper corn) + Ghee |
125 g + 125 g; Ground, mixed in warm ghee and given PO |
1 |
| 6 |
Vernonia anthelmintica (seeds) + Anethum graveolens (seeds) + Trigonella foenum-graecum (seeds) + Capsicum anuum (fruit) + Water |
250 g + 500 g + 500 g + 500 g + 5 litre; Decoction PO |
1 |
| |
Total entries |
|
6 |
| |
Weakness |
|
|
| 1 |
Vernonia anthelmintica (seeds) + Anethum graveolens (seeds) + Black salt + Zingiber officinale (rhizome) + Withania coagulans (leaves) + Common salt + Picrorhiza kurroa (rhizome) + Citrullus colocynthis (fruit) + Jaggery + Allium cepa (bulb) + Capsicum annum (fruit) |
125 g + 125 g + 12 g + 50 g + 250 g + 50 g + 250 g + 500 g + 250 g + 250 g + 250 g; MGB/PO – 4 boluses for 4 days |
1 |
| 2 |
Allium cepa (bulb) + Jaggery |
250 g + 250 g; MGB/PO |
1 |
| 3 |
Brassica campestris (seed oil) + Triticum aestivum (flour) |
125 ml + 25 g PO |
1 |
| 4 |
Calotropis procera (buds) + Brassica campestris (seed oil) |
100 g + 100 ml; Decoction PO |
1 |
|
5 |
Common salt + Capsicum annum (fruit) + Picrorhiza kurroa (rhizome) + Citrullus colocynthis (fruit) |
125 g + 125 g + 10 g 250 g; Decoction PO |
1 |
| 6 |
Zea mays (flour) + Brown sugar + Water |
250 g + 250 g + 10 L PO |
1 |
| 7 |
Lepidium sativum (seeds) + Jaggey + Water + Milk |
50 g + 50 g + 100 ml + 2000 ml; Made custard and given PO |
1 |
| 8 |
Vernonia anthelmintica (seeds) + Foeniculum vulgare (seeds) + Jaggery |
50 g + 50 g + 125 g; MGB/PO |
1 |
| |
Total entries |
|
13 |
| |
Wound |
|
|
| 1 |
Brassica campestris (seed oil) |
50-100 ml; Topical application |
25 |
| 3 |
Brassica campestris (seed oil) + Lawsonia inermis (leaves) |
50 ml + 50 g; Applied oil first and then leaves of L. inermis on wound |
5 |
| 4 |
Curcuma longa (rhizome) + Brassica campestris (seed oil) |
250 g + 250 ml; Topical application |
4 |
| 5 |
Lawsonia inermis (leaves) |
Topical application |
4 |
| 6 |
Lawsonia inermis (leaves) + Water |
50 g + 50 ml; Topical application |
4 |
| 7 |
Azadirachta indica (leaves) + Water |
250 g + 500 ml; Washed wounds with hot decoction |
3 |
| 8 |
Brassica campestris (seed oil) + Kerosene oil |
150 ml + 150 ml; Topical application |
3 |
| 9 |
Lawsonia inermis (leaves) + Brassica campestris (seed oil) |
250 g + 25 ml; Topical application |
2 |
| 10 |
Azadirachta indica (leaves) + Common salt + Water |
500 g + 250 g + 2 Litre; Washed wounds with decoction |
2 |
| 11 |
Brassica campestris (seed oil) + Carbon of cell |
Topical application |
2 |
| 12 |
Brassica campestris (seed oil) + Water |
50 ml + 500 ml; Washed wound with decoction and applied oil |
2 |
| 15 |
Dalda ghee + Curcuma longa (rhizome) |
25 g + 10 g; Applied mild hot ghee on wound and sprinkled C. longa powder |
2 |
| 16 |
Hot iron + Brassica campestris (seed oil) |
Topical application |
1 |
| 17 |
Azadirachta indica (leaves) + Brassica campestris (seed oil) |
125 g + 125 ml; Washed the wounds with decoction and poured oil on the wound |
1 |
| 18 |
Azadirachta indica (leaves) + Brassica campestris (seed oil) + Common salt |
500 g + 500 ml + 100 g; Boiled leaves in seed oil and salt and applied on wound for 2-3 days |
1 |
| 19 |
Azadirachta indica (leaves) + Brassica campestris (seed oil) + Alum |
500 g + 500 ml + 100 g; Boiled leaves in oil and alum, washed wounds with extract |
1 |
| 20 |
Azadirachta indica (leaves) + Curcuma longa (rhizome) + Alum + Milk fat |
250 g + leaves + 50 g + 25 g + 50 g; all ingredients were ground to powder, Then applied milk fat on wound then powder |
1 |
| 21 |
Azadirachta indica (leaves) + water + Dettol |
250 g + 2 litre + few drops; Mixed and washed the wound |
1 |
| 22 |
Withania somnifera (leaves) + Brassica campestris (seed oil) |
1 kg + 500 ml; Boiled leaves in oil and tied on wounds for 3 days |
1 |
| 23 |
Zea mays (flour) + Common salt + Water |
250 g + 250 g + 250 ml; Topical application |
1 |
| 24 |
Lens culinaris (seeds) + Brassica campestris (seed oil) |
250 g + 250 ml; Topical application of decoction |
1 |
| 25 |
Brassica campestris (seed oil) + Kerosene oil + Curcuma longa (rhizome) |
50 ml + 50 ml + 100 g; Topical application |
1 |
| 26 |
Brassica campestris (seed oil) + Soap |
125 ml; Washed wound with soap and applied oil |
1 |
| 27 |
Trifolium alexandrinum (whole) |
Put Trifolium alexandrinum in closed utensils for hours and after that tied on wound |
2 |
| 28 |
Capsicum anuum (fruit) |
50 g; Topical application of powder |
1 |
| 29 |
Cicer arietinum (seeds) |
50 g; wraped cloth and tied on wound, kept on pouring water on cloth |
1 |
| 33 |
Citrus limon (fruit) |
Cut into half and rubbed on wound |
1 |
| 31 |
Curcuma longa (rhizome) |
10 g; Topical application |
1 |
| 32 |
Eruca sativa (seeds) + Brassica campestris (seeds) |
Topical application |
1 |
| 33 |
Geranium wallichianum (seeds) + Brassica campestris (seed oil) |
50 g + 250 ml; Topical application |
1 |
| 34 |
Ghee + Curcuma longa (rhizome) |
25 g + 25 g; Mixed, fried and applied topically |
1 |
| 35 |
Lawsonia inermis (leaves) + Alum |
50 g + 50 g; Topical application |
1 |
| 36 |
Lawsonia inermis (leaves) + Alum + Brassica campestris (seed oil) |
125 g + 50 g + 50 ml; Topical application |
1 |
| 37 |
Lawsonia inermis (leaves) + Alum + Water |
250 g + 50 g + 200 ml; Heated the alum, ground and mixed with water and L. inermis; Topical application |
1 |
| 38 |
Leather + Brassica campestris (seed oil) |
Burnt leather to ash, mixed with brassica oil and applied on wound |
1 |
| 39 |
Vernonia anthelmintica (seeds) + Triticum aestivum (flour) |
125 g + 125 g PO |
1 |
| 40 | Ziziphus jujube (leaves) + Brassica campestris (seed oil) | 250 g + 250 ml; Boiled leaves in seed oil and tied on wounds for 2-3 days | 1 |
Table 4.
Frequency of plants used for the treatment of equine diseases/ conditions documented by local veterinary healers from three districts (Faisalabad, Sargodha and Lahore) of Punjab, Pakistan
| Conditions | Plants | Entries |
Prescriptions/ |
Plants as part of prescriptions for the same disease more than one time[1] |
|---|---|---|---|---|
| remedies | ||||
| Anorexia |
17 |
23 |
19 |
Allium (A.) cepa (12), Capsicum (Cp.) annum (9), Zingiber (Z.) officinale (8), Vernonia (V.) anthelmintica (6), Citrullus (Ct.) colocynthis (4), Trachyspermum (T.) ammi (4), Picrorhiza (Pr.) kurroa (3), Piper (P.) nigrum (3), Zea mays (2) |
| Bad habits |
1 |
5 |
2 |
- |
| Bronchitis |
12 |
33 |
21 |
Glycyrrhiza glabra (11), A. cepa (8), Rosa damascena (5), Z. officinale (4), P. nigrum (2), T. ammi (2), V. anthelmintica (2) |
| Colic |
9 |
24 |
21 |
Brassica (B.) campestris (4), T. ammi (3), A. cepa (2), Nicotiana tabacum (2), V. anthelmintica (2) |
| Dermatitis |
6 |
32 |
16 |
Eruca sativa (5), B. campestris (4) |
| Diarrhoea |
5 |
5 |
5 |
Ct. colocynthus (2), V. anthenthelmintica (2) |
| Ectoparasites |
5 |
23 |
11 |
B. campestris (2) |
| Eye problem |
- |
2 |
2 |
- |
| Fever |
11 |
12 |
9 |
T. ammi (3), A. cepa (2), Capsicum (Cp)annum (2), Z. officinale (2) |
| Haematuria |
2 |
4 |
4 |
- |
| Heat stress |
6 |
10 |
8 |
T. ammi (2), V. anthelmintica (2) |
| Indigestion |
11 |
6 |
6 |
Z. officinale (4), A. cepa (3), T. ammi (3), Cp. annum (2), Ct. colocynthis (2), Pr. kurroa (2), V. anthelmintica (2) |
| Endoparasites |
8 |
31 |
12 |
Molottus philpinensis (4), Ricinus cummunis (2) |
| Lameness |
21 |
58 |
40 |
B. campestris (7), Sesamum indicum (4), Azadirachta (Az.) indica (3), Geranium wallichianum (3), V. anthelmintica (3), Anethum (An.) graveolens (2), Cicer arietinum (2), Eugenia caryophllata (2), Myristica (M.) fragrans (2) |
| Pain |
9 |
5 |
5 |
- |
| Quidding |
2 |
3 |
3 |
- |
| Urine retention |
3 |
10 |
8 |
B. campestris (2) |
| Swelling |
5 |
11 |
7 |
B. campestris (2) |
| Tetanus |
3 |
2 |
2 |
M. fragrans (2), Pr. kurroa (2) |
| Toxemeia |
5 |
7 |
7 |
Cp. annum (5), An. graveolens (2), Trigonella foenum-graceum (2), V. anthelmintica (2) |
| Weakness |
14 |
23 |
13 |
A. cepa (2), B. campestris (2), Cp. annum (2), Ct. colocynthis (2), Pr. kurroa (2), V. anthelmintica (2) |
| Wound | 16 | 121 | 57 | B. campestris (20), Az. indica (7), Lawsonia inermis (6), Curcuma longa (5) |
[1]Plants were used in more than one prescription because of difference either in their dose, composition of the prescription, mode of preparation and administration, vehicles, etc.
Conditions reported against plant usage
Number and nature of TVPs documented for the treatment of different diseases/conditions have been summarized in the Table 2. It is evident from the data (Table 4) that maximum number of plant based remedies/prescriptions was documented for the treatment of wounds (n = 57) followed by lameness (n = 40), bronchitis and colic (n = 21), anorexia (n = 19), dermatitis (n = 16), weakness (n = 13), internal parasites (n = 12), external parasites (n = 11), fever (n = 09), heat stress and retention of urine (n = 08), swelling and toxemia (n = 07), indigestion (n = 06), diarrhoea and pain (n = 05), haematuria (n = 04), quidding (n = 03), bad habits, eye problem and tetanus (n = 02). Similar trend was seen for the number of TVPs used for different diseases/conditions being highest (n = 121) for wounds and the lowest for tetanus (n = 02). Maximum number of plants were used against lameness (n = 21) followed by anorexia (n = 17), wounds (n = 16), weakness (n = 14), bronchitis (n = 12), etc. as shown in the Table 4.
Approaches adapted in plant usage
Seeds were the most frequently used (n = 16/60) part of plants as such or as their oils followed by leaves (n = 12/60) and fruit (n = 11/60). The other parts of plants used were: whole plant, rhizome, bark, branches, bulb, buds, flour, pepper corn, roots, etc (Table 2). Prescriptions for treatment/control of different conditions of equines were based on single or multiple plants. Most of the recipes were prepared by mixing and grinding the ingredients. The powder was then made into physic balls as bolus to be given orally or decoctions were prepared for drenching the animals and/or used for topical application as washing, spraying, ointment, liniment, massage, etc. The prescriptions also differed in dose, method of preparation, and mode of administration of plants and/or materials other than plants; within and amongst the diseases/conditions. In some cases, frying, burning (to create smoke around animals), pouring, drinking, soaking before use, forced inhalation and steaming of ingredients were practiced.
Discussion
There are several recent evidences of plant based treatment and control strategies from Pakistan, especially for parasitism [11,12]. This has been supported by repellent activity of Moringa oleifera[17], an indication to be used against ecto-parasites. Plants from different geographical regions have produced variable results [18] as the synthesis of secondary plant products can be affected by environmental/growing conditions. Steroid saponins show pharmacologic actions like antifungal, antibacterial, anti-inflammatory and hypocholesteremic influences (Wang et al., [19]). So, plants producing saponins and organosulfur compounds like those of genus Allium can be used in the conditions described above.
Large number of qualified veterinarians also advocates the use of phytotherapy, other than preventive medication, but these practices are less organized in the form of scientific reports and are usually transferred orally as these have been developed by farmers, rather than by scientists in sophisticated laboratories. This situation is typical of a rural underdeveloped culture like that of pastoralists of Africa [20] and other parts of world having dependence on phytotherapy for their animals. Inadequate access to modern health care facilities due to cost-ineffectiveness, inherited beliefs, empirical evidence of efficacy, cultural acceptability and availability of botanicals at the farmers’ doorstep are the main factors [21] that lead to dependence of livestock farmers on the phytotherapy. The indigenous knowledge and skills can contribute towards development of phytotherapy in less developed areas of the world [22,23]. Plants are considered to possess relatively higher bioactive secondary compounds, thus hold promise for drug discovery. Most of the plant-derived chemicals are secondary metabolites, of which at least 12,000 have been isolated; a number estimated to be less than 10% of the total [24]. Nok et al.[25,26] and Nok and Williams [27] have discussed the active principles as well as the mechanisms of action of some plant extracts that are used in phytotherapy.
Fruitful efforts have also been made previously to document TVPs in some parts of Punjab, Pakistan focusing livestock but not including equines [28]–[32]. Equine industry has the ready and largely uninformed access to herbal products. Therefore, at least to the extent of equines, herbals are more than traditional veterinary medicine. The researchers have, therefore, focused on documentation and validation of usage of plants based on the claims of traditional healers [33]–[37].
Results of the present study have revealed that equine owners and/or traditional veterinary healers have great wealth of indigenous knowledge based on their practices and experience, which is evident from the number of plants (n = 60) used for treatment of different diseases/conditions of equines in Faisalabad, Sargodha and Lahore. Use of plants in multiple disorders indicates diversity of their pharmacological and toxicological impacts [38]. Plants have more than one mode of actions; therefore, provide broad spectrum activities in different diseases [39] due to diversity of phyto − chemicals. Twenty − four plants including Anethum graveolens, Bambusa bambos, Cascuta reflexa, Citrus limon, Cocus nucifera, Ficus religiosa, Geranium wallichianum, Grewia asiatica, Halorrhena pubescens, Lagenaria siceraria, Lepidium sativum, Mangifera indica, Medicago sativa, Myristica fragrans, Nigella sativa, Oryza sativa, Peganum harmala, Pennisetum glaucum, Picrorhiza kurroa, Piper betle, Prunus dulcis, Trifolium alexandrinum, Withania somnifera and Zea mays were found to be used for different indications in equines. As far as could be ascertained, there is no published literature on the use of plants for the treatment of ailments in equines. There are thousands (≈250,000) of species of plants naturally available [40], with a low proportionate exploited for medicinal purposes. Further, 5–5% of the higher plants have been investigated for their active constituents against a wide range of infectious and non-infectious diseases of humans and animals (Pieters and Vlietinck [41]). Plants are primary source of natural products used by traditional healers in 80% of the developing societies [42]. There was about 40% repetition in the ethno-botanical preparations (EBPs) documented in the present study and those documented by others for other species of animals [28]–[32]). It has been reported previously that different parts of the same plant (leaves, fruits, flowers, seeds, seed kernels, latex, stem, grains, bulbs, tuber, roots, basal rosette, bark, thallus, shoots, wood, buds, aerial parts, branches, etc.) and variety of solvents used for their extraction diversify their usage ([43]–[46]). Variation in the doses and mode of preparation of remedies within and among different conditions has also been reported elsewhere [11,28,30,32,47]. The aspect of non-standardized doses in phytotherapy have been criticized, because of toxicity constraints, under dosing, and cost; however, cost can be reduced by proper standardization of doses [48,49]. The common adage that natural is synonymous with safe, has led to significant and widespread disease [50], and it is critical that those involved in equine husbandry and health care are aware of the potential dangers of herbal medicine. Therefore, researches on the standardization of doses regarding efficacy vs safety should be carried out.
Conclusions
The current research suggests that EBPs have a crucial role in animal health and production in the study area. The current study revealed a diverse range of plants which is in practice to treat the prevalent ailments in equine population of Punjab. The pitfalls of TVPs found in this study were related with the improper diagnosis of diseases (some cases), non-standardization of dosages, mode of preparation and administration, and lack of understanding regarding importance of value addition (e.g., validation) to the existing practices, adverse/overdosing effects and documentation of indigenous knowledge. For example, traditional healers were not aware of the minimum essentials of parasite biology and strategic worm control practices. Fundamental issues in phytotherapy; however, are the dose, efficacy and safety left to an educated guess or is completely ignored. However, a handsome volume of the indigenous knowledge has been documented for the first time in the region in relation to the treatment of equines which provides a baseline for future scientific investigations in phytochemistry. The promising candidates of plant origin can be isolated through modern chemistry protocols and authenticated for their medical value after in vivo and in vitro experimentations.
Competing interests
We declare that none of the authors have competing interests.
Authors’ contributions
ZI: designed the project for the Ph.D. research of KG who was actively involved in the field surveys and compilation of the data. MS provided the transport and consultation services for approaching the equines of the study area. MSS provided comments and suggestions during drafting and reporting of the data and wrote the draft of manuscript. Q was involved in writing and reviewing of manuscript. All authors approve the final submission of the manuscript.
Contributor Information
Khurram Goraya, Email: khurramgoraya@hotmail.com.
Zafar Iqbal, Email: zafaruaf1@gmail.com.
Muhammad Sohail Sajid, Email: drsohailuaf@hotmail.com.
Ghulam Muhammad, Email: profdrgm_pk@yahoo.com.
Qurat ul Ain, Email: ainizafar24@gmail.com.
Muhammad Saleem, Email: rvaseditor@gmail.com.
Acknowledgements
The financial support of the Higher Education Commission, Islamabad for completion of this study is acknowledged. Authors would like to thank all the local veterinary healers of the study districts who participated for making this surveillance a success. Professional collaboration of The Brookes Hospital for Animals at the Faculty of Veterinary Sciences is highly appreciable for making field visits possible.
References
- Urquhart GM, Armour J, Duncan JL, Dunn AM, Jennings FW. Veterinary Parasitology. 2. UK: Blackwell Science; 2007. [Google Scholar]
- Goraya K, Iqbal Z, Sajid MS, Muhammad G. Frequency distribution of equine diseases in three metropolises of the upper Punjab, Pakistan. Int J Agric Biol. 2013;00:000–000. [Google Scholar]
- Lans C, Turner N, Brauer G, Lourenco G, Georges K. Ethnoveterinary medicines used for horses in Trinidad and in British Columbia, Canada. J Ethnobiol Ethnomed. 2006;2:31. doi: 10.1186/1746-4269-2-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox PA. Will tribal knowledge survive the millennium? Science. 2000;287:44–45. doi: 10.1126/science.287.5450.44. [DOI] [PubMed] [Google Scholar]
- Ole−Miaron JO. Ethnoveterinary practices of the Loitokitock Maasai: impact on the environment. Vet J. 1997;17:159–167. [Google Scholar]
- Lans C. Creole remedies: case studies of ethnoveterinary medicine in Trinidad and Tobago. PhD Thesis. Netherlands: Wageningen University; 2001. [Google Scholar]
- Akhtar MS, Iqbal Z, Khan MN, Lateef M. Anthelmintic activity of medicinal plants with particular reference to their use in animals in the Indo-Pakistan subcontinent. Small Rumin Res. 2000;38:99–107. doi: 10.1016/S0921-4488(00)00163-2. [DOI] [Google Scholar]
- Iqbal Z, Lateef M, Jabbar A, Muhammad G, Khan MN. Anthelmintic activity of Calotropis procera (Ait.) Ait. F. flowers in sheep. J Ethnopharmacol. 2005;102:256–261. doi: 10.1016/j.jep.2005.06.022. [DOI] [PubMed] [Google Scholar]
- Iqbal Z, Sarwar M, Jabbar A, Ahmad S, Nisa M, Sajid MS, Khan MN, Mufti KA, Yaseen M. Direct and indirect anthelmintic effects of condensed tannins in sheep. Vet Parasitol. 2007;144:125–131. doi: 10.1016/j.vetpar.2006.09.035. [DOI] [PubMed] [Google Scholar]
- Lateef M, Iqbal Z, Sajid MS, Abbas RZ, Sindhu ZUD, Akhtar M, Khan MN, Awais MM, Iqbal A, Ain QU. An account of botanical anthelmintics and methods used for their evaluation. Rev Vet Anim Sci. 2013;1:7–14. [Google Scholar]
- Sindhu ZUD, Iqbal Z, Khan MN, Jonsson NN, Siddique M. Documentation of ethno − veterinary practices used for treatment of different ailments in selected a hilly area of Pakistan. Int J Agric Biol. 2010;12:353–358. [Google Scholar]
- Sindhu ZUD, Shafiq-Ullah, Abbas RZ, Iqbal Z, Hameed M. Inventory of ethno-veterinary practices used for the control of parasitic infections in district Jhang, Pakistan. Int J Agric Biol. 2012;14:922–928. [Google Scholar]
- Anonymous. Pakistan livestock census. Pakistan, Islamabad: Agricultural Census Organization, Ministry of Economic Affairs and Statistics; 2006. [Google Scholar]
- Dunn T. Rapid rural appraisal: a description of the methodology and its application in teaching and research at Charles Stuart University. Wagga Wagga Australia: Rural Society; 1992–1994. [Google Scholar]
- Thrusfield M. Veterinary epidemiology. 3. Blackwell science; 2007. pp. 231–232. [Google Scholar]
- Etkins NL. Anthropological methods in ethnopharmacology. J Ethnopharmacol. 1993;38:93–104. doi: 10.1016/0378-8741(93)90004-O. [DOI] [PubMed] [Google Scholar]
- Ashfaq M, Ashfaq U. Evalauation of mosquitocidal activity of water extract of Moringa Oleifera seeds against Culex Quinuefasciatus (Diptera: Culicidae) in Pakistan. Pak Entomol. 2012;34:21–26. [Google Scholar]
- Waller PJ, Bernes G, Thamsborg SM, Sukura A, Richter SH, Ingebrigtsen K, Hoglund J. Plants as de-worming agents of livestock in the Nordic countries: historical perspective, popular beliefs and prospects for the future. Acta Vet Scand. 2001;42:31–44. doi: 10.1186/1751-0147-42-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P, Su Z, Yuan W, Deng G, Li S. Phytochemical constituents and pharmacological activities of Eryngium L. (Apiaceae) Pharmaceutical Crops. 2012;3:99–120. doi: 10.2174/2210290601203010099. [DOI] [Google Scholar]
- De Leeuw PN, McDermott JJ, Lebbie SHB. Monitoring of livestock health and production in sub − Saharan Africa. Prev Vet Med. 1995;25:195–212. doi: 10.1016/0167-5877(95)00547-1. [DOI] [Google Scholar]
- Bennet−Jenkins E, Bryant C. Novel sources of anthelmintics. Int J Parasitol. 1996;26:937–947. doi: 10.1016/S0020-7519(96)80068-3. [DOI] [PubMed] [Google Scholar]
- Brokensha DW, Warren DM, Werner O. Indigenous knowledge systems and development. Lanham, MD: University Press of America; 1980. [Google Scholar]
- IDS. Whose knowledge counts? IDS Bull. 1979;10:2. [Google Scholar]
- Schultes RE. The kingdom of plants: medicines from the earth, Thomson, WAR. New York, NY: McGraw−Hill Book Co; 1978. p. 208. [Google Scholar]
- Nok AJ, Esievo AN, Longet I, Arowosafe S, Onyenekwe PC, Gimba CE, Kagbu JA. Trypanocidal potentials of Azadirachta indica: in vivo activity of leaf extract against Trypanosoma brucei. J Clin Biochem Nutr. 1993;15:113–118. doi: 10.3164/jcbn.15.113. [DOI] [Google Scholar]
- Nok AJ, Esievo KAN, Armbrose A, Isaac AI, Emmanuel GC, Solomon MO, James KA. Trypanocidal activity of an organotin compound (tri-n-butyltin oxide) toward Trypanosoma brucei. J Clin Biochem Nutr. 1992;13:81–85. doi: 10.3164/jcbn.13.81. [DOI] [Google Scholar]
- Nok AJ, Williams S. Allium sativum induced death of African Trypanosomes. Parasitol Res. 1996;82:634–637. doi: 10.1007/s004360050177. [DOI] [PubMed] [Google Scholar]
- Dilshad SMR, Rehman N, Iqbal Z, Muhammad G, Iqbal A, Ahmed N. An inventory of the ethnoveterinary practices for reproductive disorders in cattle and buffaloes, Sargodha district of Pakistan. J Ethnopharmacol. 2008;117:393–402. doi: 10.1016/j.jep.2008.02.011. [DOI] [PubMed] [Google Scholar]
- Farooq Z, Iqbal Z, Mushtaq S, Muhammad G, Iqbal MZ, Arshad M. Ethnoveterinary practices for the treatment of parasitic diseases in livestock in Cholistan desert (Pakistan) J Ethnopharmacol. 2008;118:213–219. doi: 10.1016/j.jep.2008.03.015. [DOI] [PubMed] [Google Scholar]
- Jabbar A, Iqbal Z, Khan MN. In vitro anthelmintic activity of Trachyspermum ammi seeds. Phcog Mag. 2006b;2:126–129. [Google Scholar]
- Khan MK, Sajid MS, Khan MN, Iqbal Z, Iqbal MU. Bovine fasciolosis: prevalence, effects of treatment on productivity and cost benefit analysis in five districts of Punjab, Pakistan. Res Vet Sci. 2009;87:70–75. doi: 10.1016/j.rvsc.2008.12.013. [DOI] [PubMed] [Google Scholar]
- Muhammad G, Khan MZ, Hussain MH, Iqbal Z, Iqbal M, Athar M. Ethnoveterinary practices of owners of pneumatic-cart pulling camels in Faisalabad city (Pakistan) J Ethnopharmacol. 2005;97:241–246. doi: 10.1016/j.jep.2004.11.008. [DOI] [PubMed] [Google Scholar]
- Aqel MB. Relaxant effect of the volatile oil of rosmarinus officinalis on tracheal smooth muscle. J Ethnopharmacol. 1991;33:57–62. doi: 10.1016/0378-8741(91)90161-6. [DOI] [PubMed] [Google Scholar]
- Lanhers MC, Fleurentin J, Mortier F, Vinche A, Younos C. Anti-Inflammatory and analgesic effects of an aqueous extract of Harpagophytum procumbens. Planta Med. 1992;58:17–123. doi: 10.1055/s-2006-961411. [DOI] [PubMed] [Google Scholar]
- Pearson W. Ethnoveterinary medicine: the science of botanicals in equine health and disease. The Netherlands; 2003. pp. 31–40. (Proceedings of the 2nd European equine health and nutrition congress, lelystad). [Google Scholar]
- Sommer H, Felbinger U, Pütz R, Reutershan R, Schaefer J. The effects of an herb mixture on horses with respiratory disease. Tierarztl Umsch. 1986;41:846–848. [Google Scholar]
- Wagner I, Greim C, Laufer S, Heide L, Gleiter CH. Influence of willow bark extract cyclooxygenase activity and on tumor necrosis factor alpha or interleukin 1 beta release in vitro and ex vivo. Clin Pharmacol Ther. 2003;73:272–274. doi: 10.1067/mcp.2003.32. [DOI] [PubMed] [Google Scholar]
- Iwu M. Handbook of African medicinal plants. Boca Raton, FL: CRC Press; 1993. [Google Scholar]
- Reichling J, Saller R. Herbal remedies in veterinary phytotherapy. Schweiz Arch Tierheilkd. 2001;43:395–403. [PubMed] [Google Scholar]
- Borris RP. Natural products research: perspectives from a major pharmaceutical company. J Ethnopharmacol. 1996;51:29–38. doi: 10.1016/0378-8741(95)01347-4. [DOI] [PubMed] [Google Scholar]
- Pieters L, Vlietnick AJ. Bioguide isolation of pharmacologically active plant components, still a valuable strategy for the finding of new lead compounds. Journal of Ethnopharmacology. 2005;100:57–60. doi: 10.1016/j.jep.2005.05.029. [DOI] [PubMed] [Google Scholar]
- Farnsworth NR, Akerele O, Bingel AS, Soejarto DD, Guo Z. Medicinal plants in therapy. Bull World Health Organ. 1985;63:965–981. [PMC free article] [PubMed] [Google Scholar]
- Giday M, Asfaw Z, Elmqvist T, Woldu Z. An ethnobotanical study of medicinal plants used by the Zay people in Ethiopia. J Ethnopharmacol. 2003;85:43–52. doi: 10.1016/S0378-8741(02)00359-8. [DOI] [PubMed] [Google Scholar]
- Nfi AN, Mbanya JN, Ndi C, Kameni A, Vabi M, Pingpoh D, Yonkeu S, Moussa C. Ethnoveterinary medicine in the Northern Provinces of Cameroon. Vet Res Commun. 2001;25:71–76. doi: 10.1023/A:1026766219786. [DOI] [PubMed] [Google Scholar]
- Ole−Miaron JO. The Maasai ethnodiagnostic skill of livestock diseases: a lead to traditional bioprospecting. J Ethnopharmacol. 2003;84:79–83. doi: 10.1016/S0378-8741(02)00283-0. [DOI] [PubMed] [Google Scholar]
- Viegi L, Pieroni A, Guarrera PM, Vangelisti R. A review of plants used in folk veterinarymedicine in Italy as basis for a databank. J Ethnopharmacol. 2003;89:221–244. doi: 10.1016/j.jep.2003.08.003. [DOI] [PubMed] [Google Scholar]
- Deeba F, Muhammad G, Iqbal Z, Hussain I. Appraisal of ethno-veterinary practices used for different ailments in dairy animals in peri-urban areas of Faisalabad (Pakistan) Int J Agric Biol. 2009;11:535–541. [Google Scholar]
- Bakhiet AO, Adam SEI. Therapeutic utility, constitutents and toxicity of some medicinal plants. Vet Human Toxicol. 1995;37:255–258. [PubMed] [Google Scholar]
- Longuefosse JL, Nossin E. Medical ethnobotany survey in Martinique. J Ethnopharmacol. 1996;53:117–120. doi: 10.1016/0378-8741(96)01425-0. [DOI] [PubMed] [Google Scholar]
- Pearson W. Pyrrolizidine Alkaloids in higher plants: hepatic veno-occlusive disease associated with chronic consumption. JNFMF. 2000;3:87–96. [Google Scholar]