Creating positive working relationships with patients, safeguarding their personal information, engaging in collaborative healthcare decisionmaking with them, and helping them to stick with agreed-upon treatment plans are activities central to good clinical practice. These four aspects of patient care --the therapeutic alliance, confidentiality, informed consent, and treatment adherence -- are important in reaching clinical goals (Jonsen, Winslade, & Siegler, 1998). They are also critical to the ethical aspirations of the health professionals who seek to provide care that is based on trust, is truly respectful and compassionate, and brings benefit (Drane, 1988; American Medical Association, 2005; Roberts & Dyer, 2004; Koocher & Spiegel, 1998).
Despite their vital role, these four clinical ethics practices may be very challenging to fulfill in every day interactions with patients (Perkins, Hudson, Gray, & Stewart, 1998; Roberts, Geppert, & Bailey, 2002). Establishing a therapeutic relationship with a person who is ill, distressed, and frightened can be difficult (McCarty & Roberts, 1996). Sufficiently protecting an individual’s personal information, particularly for an embarrassing and highly sensitive health condition, can be hard to achieve in many clinical settings (Siegler, 1982; Bogenschutz & Geppert, 2003; Wettstein, 1994). Informed consent, similarly, is a complex task that entails engaging in a thorough ongoing dialogue with a patient about his or her health concerns, about the need for intervention, the proposed treatment and alternative approaches, and about expected outcomes and possible adverse consequences (Sugarman et al., 1999; Lidz, Meisel, Osterweis, Holden, Marx, & Munetz, 1983). It also involves verifying that the patient has the ability to make this decision and does so freely and in accordance with his or her personal beliefs and values (Roberts, 2002). Finally, treatment adherence may be the greatest challenge of all since the illness process itself may interfere with ability to follow-through on clinical recommendations and ill individuals may have fewer resources and supports (Siegler, 1982; Bebbington, 1995; Connors, Carroll, DiClemente, Longabaugh, & Donovan, 1997).
When providers and patients come from different backgrounds, obstacles to establishing a therapeutic alliance, safeguarding confidentiality, engaging in informed consent processes, and assuring treatment adherence may be heightened (Agard, Finkelstein, & Wallach, 1998; Perkins, Geppert, Gonzales, Cortez, & Hazuda, 2002; Okasha, Arboleda-Florez, & Sartorius, 2000). Differences in language and communication styles, in cultural values and attitudes, and in expectations of the provider-patient relationship together create greater complexity and opportunities for misunderstanding and missteps in the clinical care process (Carrese & Rhodes, 1995; Hollifield, Geppert, Johnson, & Fryer, 2003; Lefley, 2002). These issues have been studied previously, and diverse projects have documented that women and behavioral health care providers may be more attentive to these and related clinical ethics issues than their male and physical health care provider counterparts (Hojat, Gonnella, & Xu, 1995; Price, Price, Williams, & Hoffenberg, 1998; Roberts, Geppert, Warner, Green Hammond, & Lamberton, 2005; Roberts et al., 2001).
Continuing education efforts, particularly in the areas of clinical skills, professionalism, and cultural competence, have been identified as a possible approach to overcoming barriers in patient care (Sulmasy & Marx, 1997; Lefley, 2002). To our knowledge, however, no systematic work has been published on whether multidisciplinary health care providers perceive additional training on these clinical ethics practices specifically as helpful in preparing them for their work with patients from different backgrounds. We examine this question in this large survey of multidisciplinary providers in Alaska and New Mexico, where the cultural, racial and ethnic, religious, and educational backgrounds of providers and patients are often dissimilar (Roberts, Battaglia, Smithpeter, & Epstein, 1999; Roberts et al., 2001).
METHOD
As part of a National Institute on Drug Abuse-funded project, our multidisciplinary research team developed a 21-page survey to explore numerous issues confronting rural and urban healthcare practitioners in Alaska and New Mexico. This survey was developed based on extensive qualitative work and thorough review of the extant literature and consisted of 10 parts. Of particular interest in this brief report, are a set of items included in the section addressing training needs. Specifically, we asked providers to indicate to what extent additional training in each of four clinical ethical domains (how to assure confidentiality, how to establish a therapeutic alliance, how to engage in informed consent processes, and how to attain treatment adherence) would help them provide more effective care when working with clients/patients from an ethnic/cultural background different than their own. These items were rated on an 11-point scale ranging from not helpful at all (0) to very helpful (10).
Potential participants were identified by obtaining lists of licensed physicians, psychiatrists, physician assistants, nurse practitioners, registered nurses, psychologists, social workers, and mental health counselors in Alaska and New Mexico. For each of the professions in which the number of providers were large enough, 125 urban and 125 rural providers in each state were randomly selected to receive a survey. For professions with fewer than 250 licensees, all providers were selected; for rural groups of licensees that had fewer than 125, the complementary urban group was sampled to reach the desired goal of 250 providers per profession per state. Through this selection process, 3,695 licensees (1,722 in Alaska, 1,973 in New Mexico) were selected to be approached about participating in this study.
After receiving approval from the Institutional Review Boards at the University of Alaska Anchorage and the University of New Mexico Health Sciences Center, participants were contacted using survey procedures outlined by Dillman (1999). Each participant received a preletter, a summary of informed consent related information, up to two mailings of the survey, and up to two reminder letters. Participants were compensated $50 for returning completed surveys.
Participants were categorized as either physical healthcare providers (i.e., physicians, physician assistants, licensed nurse practitioners, and registered nurses) or behavioral healthcare providers (i.e., psychiatrists, psychologists, social workers, and mental health counselors). Due to small cell sizes, ethnic heritage was collapsed into two groups, namely, majority (i.e., white) participants and minority (i.e., African American, Alaska Native, American Indian, Asian American, Hispanic, or other minority) participants. Analyses included a 2 (Discipline) × 2 (Gender) × 2 (Ethnicity) × 4 (Ethical Domain) mixed model MANOVA, with Ethical Domain serving as a repeated measure and ratings of the four clinical domains as dependent variables.
RESULTS
Response rate
Of the 3,695 participants, 222 had undeliverable addresses and 488 were ineligible due to working less than half-time or having moved out of Alaska or New Mexico. Completed, usable surveys were returned by 1,555 participants (730 from Alaska and 825 from New Mexico), yielding an overall response rate of 52.2% (50.6% in Alaska and 53.7% in New Mexico).
Perceived helpfulness of additional training
Results of a 2 (Gender) × 2 (Ethnicity) × 2 (Discipline) × 4 (Ethics Domain) mixed model MANOVA, with the last variable serving as a repeated measure, revealed significant main effects for Ethics Domain, F(3, 4527) = 244.16, p < 0.001; Gender, F(1, 1509)=9.90, p < 0.005; and Ethnicity, F(1,1509) = 5.32, p < 0.05. Significant interactions between Ethics Domain and Discipline, F(3,4527) = 7.48, p < 0.001 and Ethics Domain and Ethnicity, F(3,4527)=3.33, p < 0.05, were also found. No other main effect or interactions were statistically significant.
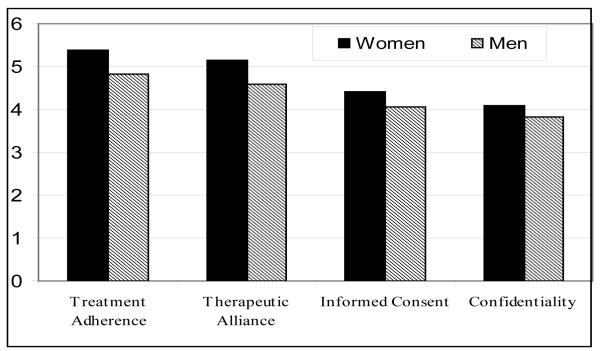
For the Ethics Domain main effect (Table 1, Figure 1), post hoc analysis revealed that providers saw additional training in all four ethics domains as having significantly different helpfulness from each other at the p< 0.001 level (maximum Cohen’s d = 0.41). Additional training in treatment adherence was rated highest in helpfulness (M=5.19), followed by therapeutic alliance (M=4.98), informed consent (M=4.30), and confidentiality (M=4.00). Thus, providers overall rated additional training in each of the four domains as moderately helpful in providing improved care effectiveness for patients/clients who derive from ethnic/cultural backgrounds different from them. For the Ethics Domain × Discipline interaction, post hoc analyses revealed that behavioral healthcare providers reported higher interest in training for confidentiality (p < 0.001, d=0.12), but did not differ from physical healthcare providers on the other three ethics practice domains.
Table 1.
Participant Characteristics
| Variable | Alaska | New Mexico | Total | |||
| Number | Percent | Number | Percent | Number | Percent | |
|
| ||||||
| Total of Respondents | 730 | 46.9% | 825 | 52.6% | 1521 | 100% |
| Gender | ||||||
| Men | 229 | 31.4% | 278 | 33.4% | 507 | 32.6% |
| Women | 501 | 68.6% | 547 | 66.6% | 1048 | 67.4% |
| Cultural Heritage | ||||||
| Hispanic | 17 | 2.3% | 129 | 15.3% | 146 | 9.4% |
| Asian or Pacific Islander | 6 | 0.8% | 13 | 1.6% | 19 | 1.2% |
| AK Native/Native American | 43 | 5.9% | 33 | 4.1% | 76 | 4.9% |
| Black or African American | 12 | 1.6% | 7 | 0.8% | 19 | 1.2% |
| White | 625 | 85.6% | 624 | 76.0% | 1249 | 80.3% |
| Other or Refused | 27 | 3.7% | 19 | 2.2% | 46 | 3.0% |
| Practice Community | ||||||
| Rural | 305 | 41.8% | 347 | 43.4% | 693 | 45.6% |
| Urban | 425 | 58.2% | 478 | 56.6% | 828 | 54.4% |
| Type of Care Provider | ||||||
| Physical healthcare | ||||||
| Physician (non-psychiatry) | 78 | 10.7% | 74 | 8.8% | 152 | 9.8% |
| Registered Nurse | 113 | 15.5% | 108 | 12.9% | 221 | 14.2% |
| Nurse Practitioner | 120 | 16.4% | 131 | 15.9% | 251 | 16.1% |
| Physician Assistant | 108 | 14.8% | 124 | 15.0% | 232 | 14.9% |
| Behavioral healthcare | ||||||
| Psychiatrist | 29 | 4.0% | 71 | 8.0% | 100 | 6.4% |
| Psychologist | 63 | 8.6% | 100 | 12.3% | 163 | 10.5% |
| Counselor | 115 | 15.8% | 111 | 14.0% | 226 | 14.5% |
| Social Worker | 104 | 14.2% | 106 | 13.3% | 210 | 13.5% |
| Mean | SD | Mean | SD | Mean | SD | |
|
|
||||||
| Years of Age | 48.8 | 9.2 | 49.0 | 9.8 | 48.9 | 9.5 |
| Years of Experience | 12.4 | 9.3 | 12.5 | 9.6 | 12.5 | 9.4 |
Figure 1. Perceived helpfulness of additional training for ethical domains when caring for patients/clients who derive from backgrounds different than the provider, by gender.
Ratings are based on an 11-point scale ranging from not helpful at all (0) to very helpful (10).
For the Gender main effect, female participants saw training on all four ethical domains as more helpful than male participants (p< 0.05 – p< 0.001; d’s = 0.20, 0.21, 0.13 & 0.10, respectively by domains as shown in Table 1). A comparison of the order of the domains by gender nevertheless revealed the same sequence, with both genders rating treatment adherence highest, followed by therapeutic alliance, informed consent, and confidentiality.
For the Ethnicity main effect, minority providers saw additional training in all four domains as more helpful than majority providers. Clarifying this main effect, the Ethics Domain × Ethnicity interaction revealed significant differences between majority and minority providers in perceived helpfulness of additional training on informed consent and confidentiality (p < 0.05 – p < 0.001; d’s = 0.14 and 0.21, respectively), but not on therapeutic alliance or treatment adherence (d’s = 0.10 and 0.08, respectively).
DISCUSSION
In this study of 1,555 multidisciplinary providers in Alaska and New Mexico, we found evidence to suggest that clinicians view additional training as moderately helpful in preparing them for the complex and challenging clinical ethics tasks of assuring treatment adherence, establishing therapeutic alliance, safeguarding confidentiality, and engaging in informed consent processes, in that order of helpfulness. Women providers overall were more receptive to additional training, consistent with findings of other ethics education studies (Shapiro & Miller, 1994), but even women endorsed additional training as only modestly helpful. Behavioral health providers and minority providers saw slightly greater value in additional training on the topic of confidentiality than did physical healthcare providers and majority providers. Minority providers were also more interested than majority providers in additional training around issues of informed consent. These ratings of the only modest utility of additional ethics training are humbling results for clinical disciplines that have placed great hope in the lifelong learning and continuing education approach to competence, accreditation, and certification processes for health professionals (Stobo & Blank, 1995; Long, 2000; Halpern, Lee, Boulter, & Phillips, 2001).
Taken together with the existing ethics education literature, our work suggests that efforts to develop ethics educational methods may be worthwhile but that the targeted learner groups may be somewhat skeptical about their helpfulness. In light of this pattern, it may be that targeting topics for certain professional learner groups, such as approaching key ethical issues for behavioral health providers, will help foster greater receptiveness toward educational activities. Notably in that context, across all participants, significant differences were noted with regard to the perceived helpfulness of training in the four ethical domains explored in this study, with the need for additional training about treatment adherence and therapeutic alliance being rated significantly higher than the need for training about informed consent and confidentiality. It may be that the former two topics are covered less often in existing ethics training programs or it may be that the participants experience more challenges within these two domains. Or, it may be that providers realize that treatment adherence and therapeutic alliance are more difficult to obtain and that they are less potentially under the control of the providers themselves than informed consent and confidentiality. Regardless of the reason for the higher ratings for treatment adherence and therapeutic alliance, it speaks to the fact that ethics training needs to go beyond the basics (e.g., confidentiality, informed consent) and must address other, more complex ethical issues that arise in clinical practice. On the other hand, this study may also serve as a caution that more training may not be the most appropriate strategy in real-world practice and that other approaches to improving practitioners’ skills should be identified and tested for their outcomes.
In interpreting our findings, three points remain unanswered. First, it is uncertain why the providers view additional training on these clinical ethics topics as only modestly helpful when studies of earlier career professionals across multiple disciplines, express far greater enthusiasm for ethics education (Jacobson, Tolle, Stocking, & Siegle, 1989; Mitchell, 1993; Angelos, DaRosa, Derossis, & Kim, 1999; Roberts, Warner, Green Hammond, Geppert, & Heinrich, 2005). Using the same survey instrument, we found that providers identified little value in other ethics education topics, so we do not believe that their modest enthusiasm pertains to the specific focus on dissimilarities in the backgrounds of providers and patients. Instead, it appears to be about the perceived utility of ethics education itself. Second, our study does not address the question of whether educational approaches actually improve providers’ skills in establishing a therapeutic alliance, safeguarding confidentiality, engaging in informed consent processes, or assuring treatment adherence, irrespective of what the learner groups perceive beforehand. Carefully designed ethics education studies are rare, but do suggest that they enhance skills and result in more positive attitudes toward ethics practices (Sulmasy, Terry, Faden, & Levine, 1994; Sulmasy & Marx, 1997). Third, how educational approaches compare to other strategies for changing practices (e.g., quality improvement activities, implementation of clinical practice protocols in clinical settings) remains an essentially unexplored area.
Three potential limitations of our work need to be acknowledged. First, our findings are based on self-report, and do not measure the effects of educational interventions on clinical ethics skills in the care of patients who come from different backgrounds than their providers. Second, almost half of those asked to participate in the project declined, although the rate of response of providers we obtained would be judged good for a time-consuming survey of up to an hour in an era when response rates to surveys overall has been declining for at least two decades (Tourangeau, 2004). Further, given that we do not have data available to compare respondents and non-respondents on demographics or any other variables, the potential for selection bias exists. Third, we only asked about interesting in training related to working with clients/patients from different ethnic/cultural backgrounds; we did ask about interest in training related to working with clients/patients from same ethnic/cultural backgrounds. Thus, despite the fact that we explicitly stated in the wording of the items that we were assessing their interest in gaining additional training to enhance their work with individuals from different ethnic/cultural backgrounds, the possibility remains that, at least for some individuals, we were actually assessing interest in these trainings in general and not specifically related to ethnic/culturally different clients.
Limitations notwithstanding,, this is a large, first-of-its-kind study with many participants and a rigorous sampling frame. For these reasons, we believe that these results merit attention and can serve as the basis for future education-oriented studies. Such work must help clarify whether practicing clinicians who shoulder responsibility for the care of patients -- many of whom will derive from different backgrounds than themselves -- can identify strategies other than traditional training paradigms for enhancing their clinical ethics skills and the extent to which diverse approaches have a positive impact. Such future work may want to include other methodologies to capture more nuanced information about the desire for and relevance of cross-cultural ethics training. For example, clinical case vignettes that vary the ethnic/cultural background of the patient/client may be useful in discerning different training needs based on similarity between provider and patient/client ethnic/cultural background; qualitative approaches such as key informant interviews or focus groups may provide deeper insights into participants’ reasons for interest or lack of interest in specific training topics vis-à-vis ethnic/cultural background of patient/client; and actual observation of providers’ service provision through actual observation or case file reviews may identify discrepancies between providers self-reported and actual training needs as related to working with patients/clients of different ethnic/cultural backgrounds from their own.
Table 2.
Perceived helpfulness of additional training for ethical domains when caring for patients/clients who derive from backgrounds different than the provider
| Ethical Care Standard |
Women Providers (n=1048) |
Men Providers (n=507) |
d | p |
Physical Health Providers (n=849) |
Behavioral Health Providers (n=694) |
d | p |
Majority Providers (n=849) |
Minority Providers (n=694) |
d | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment adherence | Mean | 5.37 | 4.81 | .20 | .001 | 5.22 | 5.15 | .02 | ns | 5.16 | 5.38 | .07 | ns |
| SD | 2.90 | 2.71 | 2.87 | 2.84 | 2.82 | 2.94 | |||||||
| Therapeutic alliance | Mean | 5.16 | 4.60 | .21 | .001 | 4.92 | 5.05 | .05 | ns | 4.93 | 5.20 | .10 | ns |
| SD | 2.74 | 2.60 | 2.70 | 2.71 | 2.66 | 2.84 | |||||||
| Informed consent | Mean | 4.42 | 4.05 | .14 | .01 | 4.34 | 4.26 | .05 | ns | 4.23 | 4.63 | .14 | .05 |
| SD | 2.89 | 2.64 | 2.82 | 2.81 | 2.74 | 3.04 | |||||||
| Confidentiality | Mean | 4.10 | 3.81 | .11 | .05 | 3.86 | 4.19 | .12 | .0 1 |
3.89 | 4.50 | .23 | .00 1 |
| SD | 2.91 | 2.69 | 2.82 | 2.86 | 2.76 | 3.08 |
Means and standard deviations are based on an 11-point scale, ranging from not helpful at all (0) to very helpful (10). ns=not statistically significant at .05 level.
In comparing across the ethical care standards within each group (i.e., column) the maximum Cohen’s d for women vs men providers was 0.44 vs 0.38, respectively, for physical vs behavioral health providers was 0.49 vs 0.34, respectively, for majority vs minority providers was 0.46 vs 0.30, respectively.
In comparing across the ethical care standards within each group (i.e., column), all means are reliably different at p<0.05 by Scheffe’s test.
Biography
Laura Weiss Roberts received her M.D. from the University of Chicago Pritzker School of Medicine. She is Charles E. Kubly Professor and Chairman of the Department of Psychiatry and Behavioral Medicine at the Medical College of Wisconsin. Dr. Roberts’ research interests include clinical psychiatry, ethical aspects of research and clinical care involving vulnerable populations, and ethics and professionalism education.
Mark E. Johnson received his Ph.D. in Counseling Psychology from the University of California at Santa Barbara. He is a Professor of Psychology and Co-Director of Behavioral Health Research and Services at the University of Alaska Anchorage. Dr. Johnson’s current research interests include HIV prevention, drug abuse, rural healthcare issues, and healthcare disparities.
Christiane Brems received her Ph.D. in Clinical Psychology from Oklahoma State University. She is a Professor of Psychology and Co-Director of Behavioral Health Research and Services at the University of Alaska Anchorage. Dr. Brems’s current research interests include rural mental healthcare, issues of the coexistence of mental health and substance use disorders, and disease prevention.
Teddy D. Warner received his Ph.D. in Social Psychology from the University of Kansas. He is a Research Associate Professor in the Department of Family and Community Medicine, University of New Mexico School of Medicine. Dr. Warner’s research interests include the empirical study of ethical issues surrounding research and health care provision, as well as the study of trauma assessment and treatment.
Contributor Information
LAURAWEISS ROBERTS, Address: Department of Psychiatry and Behavioral Medicine, Medical College of Wisconsin, 8701 Watertown Plank Road, Milwaukee, WI 53226, USA. [RobertsL@mcw.edu].
MARK E. JOHNSON, Address: University of Alaska Anchorage, P.O. Box 241626, Anchorage, AK 99524, USA.
CHRISTIANE BREMS, Address: University of Alaska Anchorage, P.O. Box 241626, Anchorage, AK 99524, USA..
TEDDY D. WARNER, Address: University of New Mexico School of Medicine, MSC 09 5040, 1 University of New Mexico, Albuquerque, NM 87131–0001, USA.
REFERENCES
- Agard E, Finkelstein D, Wallach E. Cultural diversity and informed consent. Journal of Clinical Ethics. 1998;9(2):173–176. [PubMed] [Google Scholar]
- American Medical Association Council on Ethical and Judicial Affairs . Code of medical ethics: Current opinions with annotations, 2004-2005. American Medical Association; Chicago, IL: 2005. [Google Scholar]
- Angelos P, DaRosa DA, Derossis AM, Kim B. Medical ethics curriculum for surgical residents: Results of a pilot project. Surgery. 1999;126(4):701–707. [PubMed] [Google Scholar]
- Bebbington PE. The content and context of compliance. International Clinical Psychopharmacology. 1995;9(Suppl 5):41–50. doi: 10.1097/00004850-199501005-00008. [DOI] [PubMed] [Google Scholar]
- Bogenschutz MP, Geppert CM. Women with addictive disorders: Ethical issues. In: Loue S, Sajatovic M, editors. The Encyclopedia of Women’s Health. Kluwer Academic/Plenum Publishers; New York: 2004. pp. 66–67. [Google Scholar]
- Carrese JA, Rhodes LA. Western bioethics on the Navajo reservation. Benefit or harm? Journal of the American Medical Association. 1995;274(10):826–829. [PubMed] [Google Scholar]
- Connors GJ, Carroll KM, DiClemente CC, Longabaugh R, Donovan DM. The therapeutic alliance and its relationship to alcoholism treatment participation and outcome. Journal of Consulting and Clinical Psychology. 1997;65(4):588–598. doi: 10.1037//0022-006x.65.4.588. [DOI] [PubMed] [Google Scholar]
- Dillman DA. Mail and internet surveys: The tailored design method. 2nd Ed Wiley; New York: 1999. [Google Scholar]
- Drane JF. Becoming a good doctor: The place of virtue and character in medical ethics. Sheed & Ward; Kansas City, MO: 1988. [Google Scholar]
- Halpern R, Lee MY, Boulter PR, Phillips RR. A synthesis of nine major reports on physicians’ competencies for the emerging practice environment. Academic Medicine. 2001;76(6):606–615. doi: 10.1097/00001888-200106000-00009. [DOI] [PubMed] [Google Scholar]
- Hojat M, Gonnella JS, Xu G. Gender comparisons of young physicians’ perceptions of their medical education, professional life, and practice: A follow-up study of Jefferson Medical College graduates. Academic Medicine. 1995;70(4):305–312. doi: 10.1097/00001888-199504000-00014. [DOI] [PubMed] [Google Scholar]
- Hollifield M, Geppert CM, Johnson Y, Fryer C. A Vietnamese man with selective mutism: The relevance of multiple interacting ‘cultures’ in clinical psychiatry. Transcultural Psychiatry. 2003;40(3):329–341. doi: 10.1177/13634615030403002. [DOI] [PubMed] [Google Scholar]
- Jacobson JA, Tolle SW, Stocking C, Siegle M. Internal medicine residents’ preferences regarding medical ethics education. Academic Medicine. 1989;64(12):760–764. doi: 10.1097/00001888-198912000-00015. [DOI] [PubMed] [Google Scholar]
- Jonsen AR, Winslade WJ, Siegler M. Clinical ethics. McGraw-Hill, Inc; New York: 1997. [Google Scholar]
- Koocher GP, Keith-Spiegel P. Ethics in psychology: Professional standards and cases. 2nd ed Oxford University Press; New York: 1998. [Google Scholar]
- Lefley HP. Ethical issues in mental health services for culturally diverse communities. In: Backlar P, Cutler DL, editors. Ethics in community mental health care. Kluwer Academic/Plenum Publishers; New York: 2002. pp. 3–22. [Google Scholar]
- Lidz CW, Meisel A, Osterweis M, Holden JL, Marx JH, Munetz MR. Barriers to informed consent. Annals of Internal Medicine. 1983;99:539–543. doi: 10.7326/0003-4819-99-4-539. [DOI] [PubMed] [Google Scholar]
- Long DM. Competency-based residency training: The next advance in graduate medical education. Academic Medicine. 2000;75(12):1178–1183. doi: 10.1097/00001888-200012000-00009. [DOI] [PubMed] [Google Scholar]
- McCarty T, Roberts LW. The difficult patient. In: Rubin RH, Voss C, Derksen DJ, Gateley A, Quenzer RW, editors. Medicine: A primary care approach. Saunders; Philadelphia: 1996. [Google Scholar]
- Mitchell JJ. Residents’ desire for more clinical ethics education. Academic Medicine. 1993;68(8):614–615. [PubMed] [Google Scholar]
- Okasha A, Arboleda-Florez J, Sartorius N, editors. American Psychiatric Press, Inc; Washington, DC: 2000. [Google Scholar]
- Perkins DV, Hudson BL, Gray DM, Stewart M. Decisions and justifications by community mental health providers about hypothetical ethical dilemmas. Psychiatric Services. 1998;49(10):1317–1322. doi: 10.1176/ps.49.10.1317. [DOI] [PubMed] [Google Scholar]
- Perkins HS, Geppert CM, Gonzales A, Cortez JD, Hazuda HP. Cross-cultural similarities and differences in attitudes about advance care planning. Journal of General Internal Medicine. 2002;17(1):48–57. doi: 10.1046/j.1525-1497.2002.01032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price J, Price D, Williams G, Hoffenberg R. Changes in medical student attitudes as they progress through a medical course. Journal of Medical Ethics. 1998;24(2):110–117. doi: 10.1136/jme.24.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts LW, Informed consent and the capacity for voluntarism American Journal of Psychiatry. 2002;159:705–712. doi: 10.1176/appi.ajp.159.5.705. [DOI] [PubMed] [Google Scholar]
- Roberts LW, Battaglia J, Smithpeter M, Epstein RS. An office on Main Street. Health care dilemmas in small communities. The Hastings Center Report. 1999;29(4):28–37. [PubMed] [Google Scholar]
- Roberts LW, Dyer AR. Concise guide to ethics in mental health care. American Psychiatric Publishing, Inc; Arlington, VA: 2004. [Google Scholar]
- Roberts LW, Geppert CM, Bailey R. Ethics in psychiatric practice: Informed consent, the therapeutic relationship, and confidentiality. Journal of Psychiatric Practice. 2002;8(5):290–305. doi: 10.1097/00131746-200209000-00005. [DOI] [PubMed] [Google Scholar]
- Roberts LW, Geppert CM, Warner TD, Green Hammond K, Lamberton LP. Bioethics principles, informed consent, and ethical care for special populations: Curricular needs expressed by men and women physicians-in-training. Psychosomatics. 2005;46(5):440–450. doi: 10.1176/appi.psy.46.5.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts LW, Warner TD, Brody JL, Battaglia J, Brehms C, Johnson ME, et al. Stigma, ethics, and the frontier: Challenges in caring for people with serious illnesses in Alaska and New Mexico. Arctic Research in the United States. 2001;15:2–13. [Google Scholar]
- Roberts LW, Warner TD, Green Hammond K, Geppert CM, Heinrich T. Becoming a good doctor: Perceived need for ethics training focused on practical and professional development topics. Academic Psychiatry. 2005;29(3):301–309. doi: 10.1176/appi.ap.29.3.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro J, Miller R. How medical students think about ethical issues. Academic Medicine. 1994;69(7):591–593. doi: 10.1097/00001888-199407000-00018. [DOI] [PubMed] [Google Scholar]
- Siegler M. Sounding boards. Confidentiality in medicine: A decrepit concept. New England Journal of Medicine. 1982;307(24):1518–1521. doi: 10.1056/NEJM198212093072411. [DOI] [PubMed] [Google Scholar]
- Stobo J, Blank L. ABIM’s project professionalism: Staying ahead of the wave. American Journal of Medicine. 1995;97:1–3. [Google Scholar]
- Sugarman J, McCrory DC, Powell D, Krasny A, Adams B, Ball E, et al. Empirical research on informed consent: An annotated bibliography. Hastings Center Report. 1999;29(1):S1–S42. [PubMed] [Google Scholar]
- Sulmasy DP, Marx ES. Ethics education for medical house officers: Long-term improvements in knowledge and confidence. Journal of Medical Ethics. 1997;23(2):88–92. doi: 10.1136/jme.23.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulmasy DP, Terry PB, Faden RR, Levine DM. Long-term effects of ethics education on the quality of care for patients who have do-not-resuscitate orders. Journal of General Internal Medicine. 1994;9(11):622–626. doi: 10.1007/BF02600306. [DOI] [PubMed] [Google Scholar]
- Tourangeau R. Survey research and societal change. Annual Review of Psychology. 2004;55:775–801. doi: 10.1146/annurev.psych.55.090902.142040. [DOI] [PubMed] [Google Scholar]
- Wettstein RM, Confidentiality . In: Review of psychiatry: Volume 13. Oldham JM, Riba MB, editors. American Psychiatric Press, Inc; Washington, DC: 1994. pp. 343–364. [Google Scholar]