Abstract
Purpose
Imaging by fluorodeoxyglucose positron-emission tomography (pet) has emerged as a valuable tool in the management of locally advanced cervical cancer (lacc), both for assessment of lymph node status and determination of response to chemoradiotherapy. The aim of the present study was to survey Canadian radiation oncologists to determine access to pet imaging for lacc patients and to assess current patterns of practice.
Methods
Radiation oncology centres across Canada were contacted to identify radiation oncologists who treat patients with lacc. The focus of the survey was patients treated with radical chemoradiotherapy with curative intent. An anonymous online tool was used to distribute a 23-item questionnaire asking about access to pet imaging, opinions on indications for pet imaging, and practice patterns relating to the use of pet in this patient population. Questionnaire responses were tabulated and analyzed.
Results
The response rate was 65% (35 of 54 questionnaire recipients). Most respondents (80%) have access to pet for lacc patients, usually restricted to study protocols. Of the respondents,48% considered that access to pet was timely. Frequency of routine orders for pet before and after treatment (to assess response) was 63% and 15% respectively. With better access, 91% of respondents would routinely order pet before treatment, and 61% would routinely order it for posttreatment assessment. For initial staging, 85% of respondents considered pet to be a standard of care, and nearly half (45%) believed it should be a standard of care to assess treatment response. Because of access limitations, nearly 70% of respondents (23 of 34) do not order pet as often as they feel it is clinically indicated, and 74% agree that better access to pet would lead to improved care for lacc patients in Canada.
Conclusions
Canadian radiation oncologists support the routine use of pet imaging in the initial workup of patients with lacc. Access to pet imaging limits routine use for these patients in clinically indicated situations. There is strong support for developing guidelines for pet use in this patient population.
Keywords: Cervical cancer, pet, access, practice patterns
1. INTRODUCTION
Imaging by fluorodeoxyglucose positron-emission tomography (pet) has emerged as a valuable tool in the clinical management of cervical cancer. For patients with locally advanced cervical cancer (lacc), pet imaging performed as part of the pre-treatment staging workup is highly sensitive and specific for detecting lymph node metastases, and is thereby strongly prognostic for survival1. Imaging by pet may significantly alter the initial management approach for cervical cancer patients. If, for example, positive para-aortic nodes are discovered, the radiation field may be extended to encompass pet-positive disease. In the 2011 U.S. National Comprehensive Cancer Network guidelines, pet combined with computed tomography (pet-ct) is recommended for the initial assessment of lacc2.
Positron-emission tomography may also be indicated for situations other than initial staging. A recent single-centre prospective cohort study investigated the use of pet to assess treatment response and found that the results of pet imaging 3 months post-therapy were highly predictive of survival3. Other authors have evaluated pet as an aid to brachytherapy planning4. The role of pet imaging in routine follow-up, detection of recurrence, and salvage therapy guidance for cervical cancer patients remains investigational5–7.
In Canada, the use of pet for lacc patients has not been well characterized, but is thought to be highly variable. Potential reasons for that variability include lack of access or poor access to pet in many cancer centres, long wait times for pet where the technique is available, and a lack of consensus among radiation oncologists about its appropriate use. The purpose of the present study was to use a survey of Canadian radiation oncologists who treat cervical cancer to determine their access to pet, their opinions about the indications for pet, and their current practice patterns.
2. METHODS
All radiation oncology centres across Canada were contacted to determine if their centre treats lacc patients. Participating centres identified radiation oncologists who treat cervical cancer and provided contact information. Those physicians were then sent a secure e-mail message explaining the survey objectives and providing a link to the online survey. Paper versions of the survey were mailed to participants at their request. Respondents were able to edit their answers until the study closed. Only one survey could be completed per e-mail address.
The survey was designed based on the Total Design Method of mail surveys, and questions were aimed at meeting the study objectives8. The survey comprised 23 multiple-choice, multiple-answer, and open-ended questions, and required about 10 minutes to complete. Unless otherwise specified, all questions pertained to patients with lacc treated with concurrent chemoradiotherapy.
A link to the survey was sent February 2, 2011. Reminders were sent February 16 and February 23 to physicians who had not yet responded. The survey closed March 2, 2011. Data were collected anonymously. Within the survey, individual respondents were asked for consent to the use of their responses, and all respondents consented. The data were tabulated and analyzed using frequency distributions.
3. RESULTS
The overall response rate was 65% (35 of 54 invitees). One respondent did not complete the survey in full. Responses were obtained from 9 of 10 Canadian provinces, representing 22 separate radiation treatment centres (Table i). With respect to indications for pet use, practitioners without access to pet were asked how they would use pet if access were available. The responses of practitioners with and without pet access were pooled to report on perceived indications for pet in cervical cancer.
TABLE I.
Survey response, by province
| Province | Respondents (n) | Treatment centres (n) |
|---|---|---|
| British Columbia | 4 | 3 |
| Alberta | 5 | 2 |
| Saskatchewan | 3 | 1 |
| Manitoba | 1 | 1 |
| Ontario | 13 | 8 |
| Quebec | 6 | 4 |
| New Brunswick | 1 | 1 |
| Prince Edward Island | 0 | 0 |
| Nova Scotia | 1 | 1 |
| Newfoundland and Labrador | 1 | 1 |
| TOTAL | 35 | 22 |
Table ii outlines access to pet among respondents. The technique was available to 80% of the surveyed radiation oncologists (28 of 35) for use in cervical cancer patients. Most had access to pet in their own hospital or within their city, but 18.5% (5 of 27) had to send patients to another city. Wait times for pet imaging averaged 1–4 weeks. Respondents with access to pet were split about whether they considered that access to be timely. Both ct and magnetic resonance imaging were used for anatomic correlation with pet by 56% of respondents (15 of 27); 33% (9 of 27) used ct alone; and 11% used magnetic resonance imaging alone.
TABLE II.
Access to positron-emission tomography (pet)
| Question |
Respondents
|
|
|---|---|---|
| (n) | (%) | |
| Do you have access to pet for locally advanced cervical cancer patients? | ||
| Yes | 28 | 80 |
| No | 7 | 20 |
| pet imaging for our patients is performed ... | ||
| In our hospital | 19 | 70 |
| In another hospital in the city | 3 | 11 |
| In another city | 5 | 19 |
| What is the average wait time for pet for cervical cancer patients at your centre? | ||
| <1 Week | 2 | 7 |
| <2 Weeks | 12 | 44 |
| 2–4 Weeks | 10 | 37 |
| >4 Weeks | 3 | 11 |
| Do you consider access to pet timely? | ||
| Yes | 13 | 48 |
| No | 14 | 52 |
For respondents with access to pet, 63% (17 of 27) routinely order it for newly diagnosed patients, and 15% (4 of 27) routinely order it for post-treatment assessment (Table iii). Post-treatment pet is typically ordered after 6–12 weeks and, less commonly, after 3 months. Only 7% of respondents reported ordering pet for the initial workup of early-stage disease (<1B2 by International Federation of Gynecology and Obstetrics criteria). Positron-emission tomography was not routinely used to assess response during treatment, nor for routine follow-up. No respondents were using pet for cervical cancer brachytherapy planning in Canada.
TABLE III.
Current use of positron-emission tomography (pet) for locally advanced cervical cancer
| Question |
Respondents
|
|
|---|---|---|
| (n) | (%) | |
| Do you routinely order pet in newly diagnosed patients? | ||
| For all new patients who will be treated with radical radiotherapy | 12 | 45 |
| For patients with early stage disease (<1B2) to decide treatment | 2 | 7 |
| For radiotherapy planning | 6 | 22 |
| To evaluate distant or suspicious disease | 16 | 59 |
| No | 10 | 37 |
| Do you routinely order pet during radiation treatment? | ||
| Yes | 1 | 4 |
| No | 26 | 96 |
| Do you routinely order pet after completion of radiotherapy? | ||
| Routinely for all patients to assess disease response | 4 | 15 |
| To evaluate patients with prior radiographic suspicion of extrapelvic disease | 9 | 33 |
| For prognostic purposes | 2 | 7 |
| No | 15 | 56 |
| Do you order pet as part of routine follow-up? | ||
| Yes | 0 | 0 |
| No | 27 | 100 |
| Do you use pet for brachytherapy planning? | ||
| Yes | 0 | 0 |
| No | 27 | 100 |
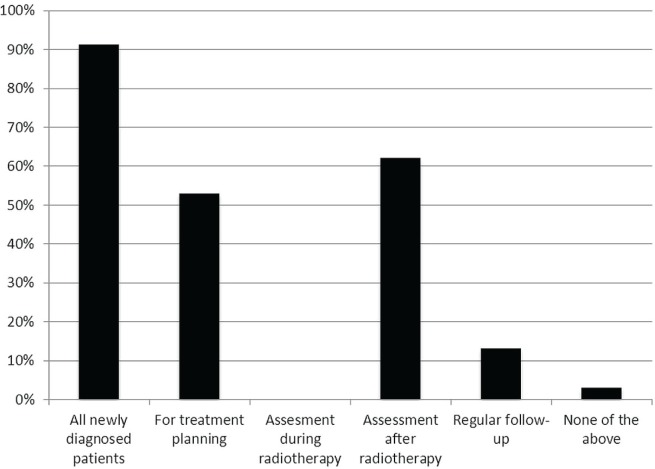
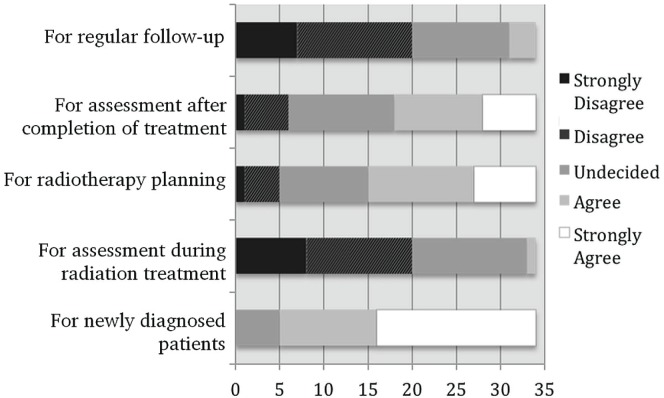
Given better access to pet, 91% of respondents (31 of 34) indicated that they would routinely order pet as part of the initial workup of newly diagnosed patients, and 62% (21 of 34), for routine post-therapy assessment (Figure 1). With better access, 12% (4 of 34) would use pet for routine follow-up. Although 85% of respondents (29 of 35) felt that pet should be considered the standard of care for newly diagnosed lacc patients, just 47% (16 of 34) felt that pet is the standard for post-therapy assessment (Figure 2).
FIGURE 1.
Indications for the use of positron-emission tomography (pet) in locally advanced cervical cancer. Graph shows responses to the question “Given better access to pet for locally advanced cervical cancer patients, I would routinely order it in the following situations.”
FIGURE 2.
Positron-emission tomography (pet) as the standard of care for lacc. Graph shows responses to the statement “pet imaging should be considered standard of care for locally advanced cervical cancer.”
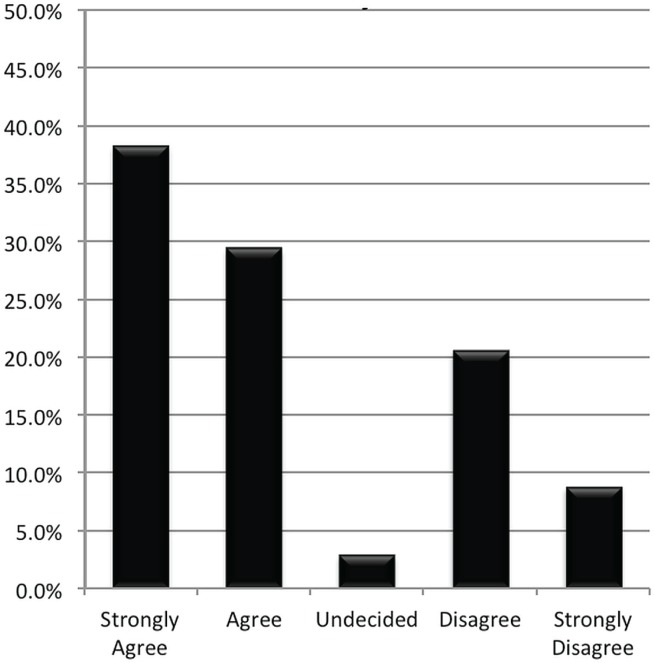
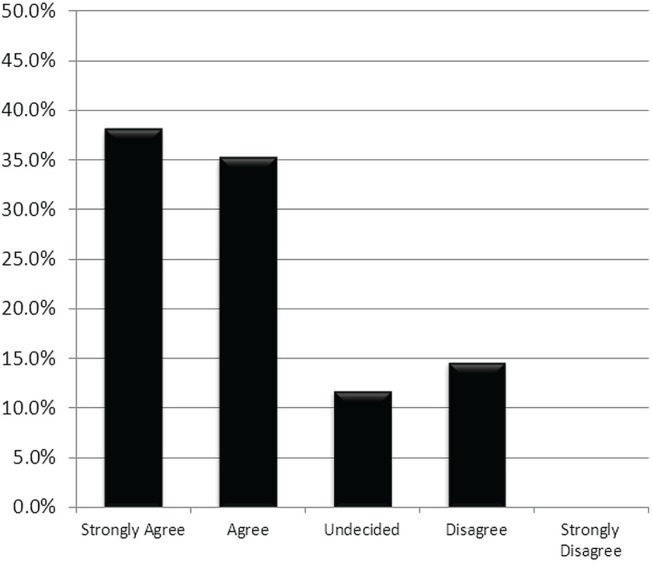
When radiation oncologists were asked whether, because of poor access, they ordered pet less often than they felt was clinically indicated, 68% (23 of 34) agreed (Figure 3). Even more of the respondents (74%, 25 of 34) felt that better access to pet would lead to better care for their patients with cervical cancer (Figure 4). Almost all (85%) supported the development of Canadian guidelines for the use of pet in cervical cancer.
FIGURE 3.
Does limited access to positron-emission tomography (pet) prevent its use in clinically indicated situations? Graph shows responses to the statement “Because of poor access, I do not order pet or pet–ct [computed tomography] scans in patients with cervical cancer as often as clinically indicated.”
FIGURE 4.
Would better access to positron-emission tomography (pet) lead to improved patient care? Graph shows responses to the statement “Better access to pet or pet–ct [computed tomography] would lead to improved patient care for my patients with cervical cancer.”
4. DISCUSSION
Positron-emission tomography is a useful tool in the management of patients with lacc. Its ability to detect pelvic and para-aortic nodes at the time of diagnosis is well established, with sensitivity and specificity exceeding 90% for pet-ct5. When compared with historical series using lymph node dissection, pet-ct demonstrated similar rates of node positivity, stage-for-stage9. Nodal status, though not part of International Federation of Gynecology and Obstetrics staging, is a strong predictor of clinical outcome in cervical cancer patients. Lymph node status determined by pet-ct can stratify patients into distinct disease-specific survival groups, independent of clinical stage9.
Initial treatment strategies can be adapted based on information provided by a staging pet-ct. Radiation plans can be modified to include pet-positive para-aortic nodes. Although extended fields have fallen out of favour in the era of combined chemoradiotherapy, modern radiotherapy techniques such as intensity-modulated radiotherapy can produce acceptable treatment plans and may facilitate a more aggressive treatment approach in these patients10.
Combined pet-ct can be extremely helpful in assessing lacc patients for response to treatment. In addition to initial stage and lymph node status, posttreatment response based on pet-ct strongly predicts for disease recurrence3. Schwarz et al. prospectively evaluated pet-ct imaging 3 months after therapy in advanced cervical cancer patients. Those authors observed 2-year cause-specific survival rates of 96% in patients with a complete metabolic response, 43% in those with persistent in-field fluorodeoxyglucose uptake, and 14% in those with evidence of new sites of disease.
Evidence is lacking for the routine use of pet-ct for follow-up in cervical cancer patients, in whom the technique has been shown to detect asymptomatic recurrences11. However, early detection of asymptomatic recurrences has not been demonstrated to improve outcomes.
Our survey assessed the practice patterns and opinions of Canadian radiation oncologists concerning the use of pet imaging for lacc. The most common use of pet in lacc is as part of the initial staging workup. Routine use for post-treatment evaluation is much less common, but given improved access, most respondents would incorporate such evaluation into their practice. Perhaps not surprisingly, most physicians would, given better access, incorporate pet into routine staging and post-treatment evaluation. But even with better access, Canadian radiation oncologists do not favour routine use of pet for response assessment during treatment or for regular follow-up. Overall, these clinical preferences for the use of pet are supported by the available evidence.
Despite 80% of responding radiation oncologists having some access to pet for lacc, the degree of access is highly variable. In the country’s most populous province, Ontario, access to pet for lacc patients is restricted to those enrolled in a clinical trial comparing treatment delivery based on pretreatment pet-ct or ct alone. In the post-treatment setting, pet is not available. Multiple survey respondents described having to send patients to another province for pet imaging—an approach that requires highly motivated patients because of the additional time and expense incurred. In our two major centres in Alberta, patients will routinely undergo pretreatment imaging at one centre and post-treatment imaging at the other.
An American survey of gynecologic oncologists conducted in 2009 found that pet-ct was accessible to75% of gynecologic oncologists12, with 63% ordering pet-ct for initial assessment of advanced-stage patients and fewer than 20% routinely ordering post-treatment pet-ct. Those results are very similar to the present findings. In contrast, only 15% of American respondents identified access limitations as a barrier to using pet-ct, compared with our finding that improved access would probably significantly increase pet-ct use for the lacc population in Canada.
Our nearly 70% survey response rate was satisfactory, but the study population is still inherently small. Despite our best efforts to contact every radiation oncology centre in the country, not all centres responded. Although we were able to characterize the accessibility of pet to Canadian radiation oncologists for the management of cervical cancer, comments on the proportion of patients who have access to pet were beyond the scope of the study. Most patients with early-stage disease are managed by gynecologic oncologists, and therefore the use of pet in the early-stage cervical cancer population was not fully assessed in our study.
5. CONCLUSIONS
Canadian radiation oncologists support the routine use of pet imaging in the initial workup of patients with lacc. Given better access, most radiation oncologists would routinely order both pre-treatment and post-treatment pet imaging. The opinions of survey respondents about the indications for pet in lacc generally agree with the existing clinical evidence. Access to pet imaging currently limits its routine use for lacc patients in clinically indicated situations. There is strong support for the development of guidelines for pet use in this patient population.
6. CONFLICT OF INTEREST DISCLOSURES
No financial conflicts of interest were identified.
7. REFERENCES
- 1.Narayan K, Fisher RJ, Bernshaw D, Shakher R, Hicks RJ. Patterns of failure and prognostic factor analyses in locally advanced cervical cancer patients staged by positron emission tomography and treated with curative intent. Int J Gynecol Cancer. 2009;19:912–18. doi: 10.1111/IGC.0b013e3181a58d3f. [DOI] [PubMed] [Google Scholar]
- 2.Koh WJ, Greer BE, Abu-Rustum NR, et al. Cervical cancer. J Natl Compr Canc Netw. 2013;11:320–43. doi: 10.6004/jnccn.2013.0043. [DOI] [PubMed] [Google Scholar]
- 3.Schwarz JK, Siegel BA, Dehdashti F, Grigsby PW. Association of posttherapy positron emission tomography with tumor response and survival in cervical carcinoma. JAMA. 2007;298:2289–95. doi: 10.1001/jama.298.19.2289. [DOI] [PubMed] [Google Scholar]
- 4.Lin LL, Mutic S, Low DA, et al. Adaptive brachytherapy treatment planning for cervical cancer using fdg-pet. Int J Radiat Oncol Biol Phys. 2007;67:91–6. doi: 10.1016/j.ijrobp.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 5.Grigsby PW. pet/ct imaging to guide cervical cancer therapy. Future Oncol. 2009;5:953–8. doi: 10.2217/fon.09.70. [DOI] [PubMed] [Google Scholar]
- 6.Haie–Meder C, Mazeron R, Magne N. Clinical evidence on pet-ct for radiation therapy planning in cervix and endometrial cancers. Radiother Oncol. 2010;96:351–5. doi: 10.1016/j.radonc.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 7.Magne N, Chargari C, Vicenzi L, et al. New trends in the evaluation and treatment of cervix cancer: the role of fdg-pet. Cancer Treat Rev. 2008;34:671–81. doi: 10.1016/j.ctrv.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Dilman D. Mail and Telephone Surveys: The Total Design Method. New York, NY: John Wiley and Sons; 1978. [Google Scholar]
- 9.Kidd EA, Siegel BA, Dehdashti F, et al. Lymph node staging by positron tomography in cervical cancer: relationship to prognosis. J Clin Oncol. 2010;28:2108–13. doi: 10.1200/JCO.2009.25.4151. [DOI] [PubMed] [Google Scholar]
- 10.Esthappan J, Chaudhari S, Santanam L, et al. Prospective clinical trial of positron emission tomography/computed tomography image-guided intensity-modulated radiation therapy for cervical carcinoma with positive para-aortic lymph nodes. Int J Radiat Oncol Biol Phys. 2008;72:1134–9. doi: 10.1016/j.ijrobp.2008.02.063. [DOI] [PubMed] [Google Scholar]
- 11.Brooks RA, Rader JS, Dehdashti F, et al. Surveillance fdg-pet detection of asymptomatic recurrences in patients with cervical cancer. Gynecol Oncol. 2009;112:104–9. doi: 10.1016/j.ygyno.2008.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kizer NT, Zighelboim I, Case AS, Dewdney SB, Thaker PH, Massad LS. The role of pet/ct in the management of patients with cervical cancer: practice patterns of the members of the Society of Gynecologic Oncologists. Gynecol Oncol. 2009;114:310–14. doi: 10.1016/j.ygyno.2009.04.018. [DOI] [PubMed] [Google Scholar]