Abstract
Purpose
We used a superficial parotid lobe–sparing delineation approach for dose optimization with better protection for the parotid glands in intensity-modulated radiotherapy (imrt) for nasopharyngeal carcinoma (npc) patients.
Methods
Compared with traditional contouring of the entire parotid glands as organs at risk (oars) in imrt for npc, we used a superficial parotid lobe–sparing delineation approach of contouring the superficial parotid lobes as oars. Changes in dose to the parotid glands, the targets, and other oars were evaluated.
Results
The mean dose to the parotid glands overall decreased by more than 4 Gy in the test plans. Impressively, the mean dose to the superficial parotid lobes in the test plans was not more than 30 Gy, regardless of clinical stage. In T1–3 npc patients, the dose distributions for targets were not significantly different in the control plans and the test plans. However, for some T4 patients, the dose distributions for targets and brainstem in the test plans could not meet clinical requirements.
Conclusions
The superficial parotid lobe–sparing delineation approach can significantly lower the mean dose to the entire parotid and to the superficial parotid lobe in T1–3 npc patients, which would be expected to result in less xerostomia and better quality of life for those patients.
Keywords: Intensity-modulated radiotherapy, nasopharyngeal carcinoma, superficial parotid lobes
1. INTRODUCTION
Nasopharyngeal carcinoma (npc) is one of the most commonly diagnosed head-and-neck malignancies in Southeast Asia, and radiotherapy is the main treatment. During radiotherapy treatment, the salivary glands on both sides usually receive a high dose of radiation. As a result, patients experience long-term xerostomia: dry mouth, sore throat, altered taste, dental decay, changes in voice quality, and impaired chewing and swallowing1–5. Yeh et al.6 reported that 87.8% of npc patients (745 of 849) had xerostomia after conventional radiotherapy. In recent years, intensity-modulated radiotherapy (imrt) has relieved this problem to some extent. Kam et al.7 compared the incidence of severe xerostomia in 56 early-stage npc patients, of whom 28 received conventional radiotherapy, and 28 received parotid-sparing imrt. One year after treatment, the authors found that, compared with patients in the conventional radiotherapy group, those in the imrt group had a significantly lower incidence of observer-rated severe xerostomia (39.3% vs. 82.1%, p = 0.01) and a higher parotid salivary flow. Hsiung et al.8 also reported that imrt could significantly preserve parotid gland function for npc patients.
The parotid is the largest salivary gland in humans, producing about 60%–65% of stimulated saliva. Damage to this gland plays an important role in the generation of xerostomia. The parotid is highly sensitive to radiation: in the first week of conventional radiotherapy, salivary flow decreases by 50%–60%; after 7 weeks of conventional radiotherapy, salivary flow diminishes to approximately 20% of that before treatment9. Consensus is that a mean dose to the parotid of less than 26–30 Gy can preserve its function substantially10,11; however, Zhao et al.12 reported that the mean dose to the parotid in npc patients receiving imrt was about 36.5 Gy. A parotid dose limitation of less than 26–30 Gy is hard to achieve in imrt plans for npc because of parapharyngeal extension of targets and because of the location of the deep lobe of the parotid.
Usually, the entire parotid is contoured as an organ at risk (oar) in imrt dose optimization for npc patients. For the present study, we developed a superficial parotid lobe–sparing delineation approach in imrt planning for npc patients. In the control plans, we contoured both parotids in full as oars in the traditional way, with a prescribed dose of 36 Gy. In the test plans, we contoured only the superficial parotid lobes as oars, with a prescribed dose of 26 Gy. We then evaluated the dose changes to the parotid glands, the targets, and the other oars.
2. METHODS
2.1. Patients
From August 2010 to January 2011, our study, conducted at the Nasopharyngeal Carcinoma Department of Sun Yat-sen University Cancer Center, enrolled 31 newly diagnosed patients with pathology-proven npc. All patients had a World Health Organization performance status of 0–1 and received 9-field step-and-shoot imrt. Table i shows the characteristics of the study patients.
TABLE I.
Clinical characteristics of the nasopharyngeal carcinoma patients
| Characteristic | Value [n (%)] |
|---|---|
| Patients | 31 |
| Sex | |
| Men | 21 (67.8) |
| Women | 10 (32.2) |
| Age (years) | |
| ≤40 | 16 (51.6) |
| >40 | 15 (48.4) |
| T stage | |
| T1 | 7 (22.6) |
| T2 | 6 (19.4) |
| T3 | 13 (41.9) |
| T4 | 5 (16.1) |
| N stage | |
| N0 | 7 (22.6) |
| N1 | 8 (25.8) |
| N2 | 12 (38.7) |
| N3 | 4 (12.9) |
| Clinic stagea | |
| i | 2 (6.5) |
| ii | 6 (19.4) |
| iii | 14 (45.1) |
| ivb | 9 (29.0) |
| Histology | |
| who type i | 0 (0) |
| who type ii | 0 (0) |
| who type iii | 31 (100) |
Union for International Cancer Control 2002 TNM staging system.
Nonmetastatic patients only (stages iva and ivb). who = World Health Organization.
2.2. Delineation of Superficial and Deep Lobes of Parotid Glands
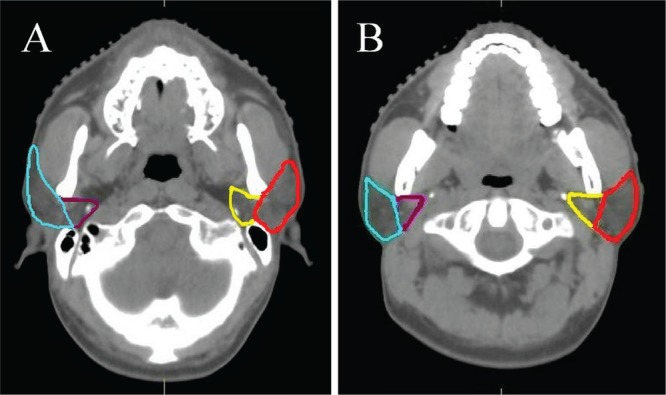
In addition to each entire parotid gland, the superficial and deep lobes of the parotids were outlined on every computed tomography slice. The parotid gland is usually divided into a superficial lobe and a deep lobe by the posterior border of the mandible or the facial nerve that threads through it. The superficial lobe covers the front part of masseter muscle’s posterior border anteriorly. Its trailing edge is adjacent to the front edge of mastoid and the anterior border of the upper side of the sternocleidomastoid muscle. The deep lobe is located in the retromandibular fossa and beneath the mandibular ramus13. For the present study, we drew the borders of the superficial and deep lobes of the parotids using the facial nerve process and anatomy (Figure 1).
FIGURE 1.
Delineation of the superficial and deep lobes of the parotid gland. (A) At the skull base, the boundary is the line from the stylomastoid foramen to the posterior border of the mandible. (B) When the stylomastoid foramen disappears, the boundary becomes the line from the anterior border of the sternocleidomastoid muscle to the anterior border of the mandible.
2.3. IMRT Planning
All patients were immobilized with thermoplastic head–neck–shoulder masks in the supine position. Computed tomography slices for treatment planning (3-mm thickness) were made from the upper edge of the frontal sinuses to 2 cm below the clavicular head.
Contours for targets and oars were delineated in a Monaco treatment planning system (version 3.0: Elekta, Stockholm, Sweden):
The nasopharyngeal gross tumour volume (gtvnx) and cervical gross tumour volume (gtvnd) included the gross extent of the tumour found by physical examination and imaging studies.
The clinical target volume 1 (ctv1) consisted of the high-risk region, including the gtv plus a 5- to 10-mm margin and the entire nasopharyngeal mucosa plus 5 mm into the submucosal area.
The clinical target volume 2 (ctv2) consisted of potentially involved regions, including the ctv1 plus a 5- to 10-mm margin and the high-risk lymphatic drainage area, which needs prophylactic irradiation.
Planning target volumes (ptvs) were derived by expanding the ctvs by 3 mm three-dimensionally so as to preclude set-up variability.
The oars included the spinal cord, brainstem, optic nerves, optic chiasm, parotid glands, lens, pituitary gland, temporal lobes, mid-ears, larynx, temporomandibular joints, and mandible.
All patients underwent imrt in 30 fractions, 1 fraction daily, 5 days per week. A mono-isocentric technique was used for 9 coplanar and equally-divided fields with the isocentre set in the gtvnx. The prescribed radiation dose was
ptvnx (ptv of gtvnx): 68 Gy or 70 Gy for T1 patients, 70 Gy for T2–4 patients
gtvnd: 64 Gy for positive lymph nodes
ptv1 (ptv of ctv1): 60 Gy
ptv2 (ptv of ctv2): 54 Gy
All targets were treated simultaneously. The prescribed doses to oars other than the parotid glands were restricted according to the Radiation Therapy Oncology Group 0225 protocol14.
2.4. Evaluation of Treatment Plan
For ptv homogeneity, the prescription dose encompassed at least 95% of the ptv. The ptvnx volume receiving more than 110% of the prescription dose did not exceed 10%, and the ptvnx volume receiving less than 93% of the prescription dose did not exceed 1%. The volume outside the ptvs receiving more than 110% of the prescribed dose to the ptvnx did not exceed 1% or 1 cm3.
2.5. Re-planning Using the Superficial Parotid Lobe–Sparing Delineation Approach
In the control imrt plans, V36 (the percentage volume receiving 36 Gy or more) in the entire parotid was prescribed to be less than 40%. All treatment plans were then re-planned according to the new superficial parotid lobe–sparing delineation requirement: V26 (the percentage volume receiving 26 Gy or more) in the superficial parotid lobe was prescribed to be less than 30%, without any change in the prescriptions for the targets and other oars compared with the control imrt plans. The same physicist created all the plans.
2.6. Statistics
The Wilcoxon matched-pairs signed–rank sum test was applied to compare mean dose; percentage volume of target regions, the parotid glands, and other oars receiving a specific dose; maximum dose in target regions; and homogeneity and conformity indices. All tests were two-sided. The level of significance was set at 5% (p < 0.05). The statistical analysis was performed using the SPSS software application (version 16.0: SPSS, Chicago, IL, USA).
3. RESULTS
3.1. Evaluation of Dose to the Parotid Glands
The mean volumes of the left and right parotid glands were 29.1 cm3 and 28.7 cm3 respectively. The mean volumes of deep lobes of the left and right parotid glands were 6.2 cm3 and 6.0 cm3 respectively. The deep lobes accounted for 21.3% and 20.9% of the entire left and right parotid glands respectively. Compared with the control plans, the study plans resulted in significantly lower mean doses to both entire parotid glands and in a significantly lower percentage volume receiving 30 Gy or more (p < 0.05, Table ii). In the test plans, the mean dose to the left and right superficial parotid lobes decreased by 4.4 Gy and 4.0 Gy respectively. Depending on T stage, N stage, and clinical stage, the decrease in the dose to the superficial parotid lobes ranged from 2.3 Gy to 5.7 Gy (Table iii).
TABLE II.
Dose and change in dose to the parotids in the control and test plans
| Variable |
Dose
|
Change in dose (control – test) | |
|---|---|---|---|
| Control | Test | ||
| Dose to left parotid | |||
| Overall (Gy) | |||
| Mean | 38.5±5.5 | 34.9±5.0 | 3.6±4.8 |
| Range | 30.8 to 56.3 | 26.4 to 42.9 | −3.9 to 22.5 |
| Superficial lobe (Gy) | |||
| Mean | 33.5±5.1 | 29.1±4.0 | 4.4±5.1 |
| Range | 27.9 to 58.9 | 21.4 to 40.1 | −4.4 to 24.4 |
| V30 (%) | |||
| Mean | 59.3±15.2 | 50.4±13.2 | 8.9±1.4 |
| Range | 37.5 to 100 | 22.4 to 78.1 | −28.5 to 55.1 |
| V60 (%) | |||
| Mean | 11.4±9.0 | 9.9±8.4 | 1.0±5.0 |
| Range | 0.4 to 30.9 | 0.06 to 28.0 | −8.38 to 14.4 |
| Dose to right parotid | |||
| Overall (Gy) | |||
| Mean | 38.5±5.6 | 34.5±5.2 | 3.5±4.3 |
| Range | 28.7 to 51.5 | 23.9 to 43.9 | −2.7 to 18.6 |
| Superficial lobe (Gy) | |||
| Mean | 33.7±5.0 | 29.7±4.2 | 4.0±4.8 |
| Range | 27.0 to 49.4 | 20.9 to 39.7 | −3.7 to 18.6 |
| V30 (%) | |||
| Mean | 59.1±16.3 | 49.1±14.9 | 10.0±14.5 |
| Range | 34.0 to 100 | 16.1 to 74.5 | −22.3 to 52.6 |
| V60 (%) | |||
| Mean | 9.3±7.8 | 8.3±8.3 | 1.0±5.0 |
| Range | −0.1 to 30.4 | 0.0 to 31.8 | −8.4 to 14.4 |
V30 = percentage of the volume that received 30 Gy or more; V60 = percentage of the volume that received 60 Gy or more.
TABLE III.
Change in dose to the superficial parotid lobes in patients with nasopharyngeal carcinoma at different T, N, and clinical stages, using superficial parotid lobe–sparing technology
| Variable | Patients (n) | Superficial lobe | Dose in test plan (Gy) | Dose reduction (Gy) |
|---|---|---|---|---|
| T stage | ||||
| T1 | 7 | Left | 27.4 | 4.8 |
| Right | 28.5 | 4.6 | ||
| T2 | 6 | Left | 29.7 | 1.6 |
| Right | 28.8 | 1.5 | ||
| T3 | 13 | Left | 29.2 | 3.9 |
| Right | 30.4 | 3.2 | ||
| T4 | 5 | Left | 30.3 | 8.5 |
| Right | 30.6 | 8.2 | ||
| N stage | ||||
| N0 | 7 | Left | 29.2 | 3.8 |
| Right | 31.2 | 3.6 | ||
| N1 | 8 | Left | 30.4 | 2.4 |
| Right | 29.5 | 2.3 | ||
| N2 | 12 | Left | 28.6 | 5.7 |
| Right | 29.5 | 5.6 | ||
| N3 | 4 | Left | 27.5 | 5.4 |
| Right | 28.3 | 3.1 | ||
| Clinical stage | ||||
| i | 2 | Left | 26.6 | 3.8 |
| Right | 30.0 | 3.6 | ||
| ii | 6 | Left | 30.7 | 2.4 |
| Right | 29.6 | 2.3 | ||
| iii | 14 | Left | 28.7 | 5.7 |
| Right | 29.7 | 5.6 | ||
| iva–ivb | 9 | Left | 29.0 | 5.4 |
| Right | 29.6 | 3.2 |
3.2. Evaluation of Dose to Targets
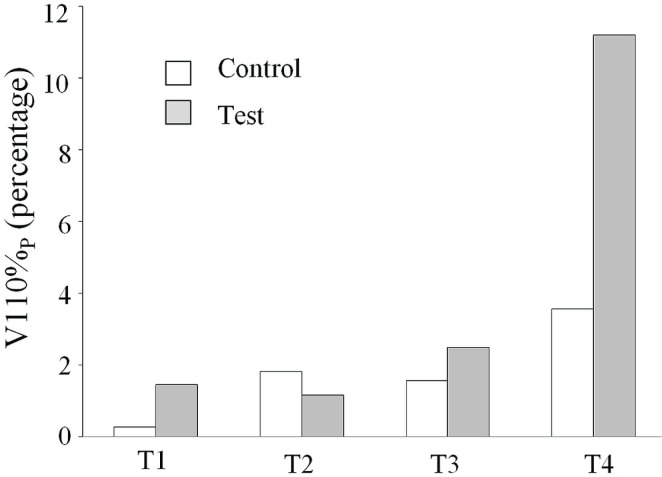
Dose distributions for targets were not significantly different between the control plans and the test plans (p > 0.05); however, for patients staged T4, the volume of the ptv that received 110% of the prescription dose (V110) increased from a mean of 3.55% to a mean of 11.19% (p = 0.08), with the measured V110 reaching 17.93% and 22.83% in two T4 patients (Figure 2). In the control plans, no patient had a V110 exceeding 10%.
FIGURE 2.
In the control and test plans for patients at various T stages, the planning target volume received 110% or more of the prescription dose (V110). Except in test plans for patients with T4 disease, the mean V110 was always less than 10%.
To evaluate any differences in the homogeneity and conformity of the ptv, we compared the homogeneity and conformity indices between the control and test plans15:
where rtog stands for “Radiation Therapy Oncology Group” and MD is the maximum dose, PD is the prescription dose, VPD is the volume receiving the prescription dose, and TV is the target volume.
No differences in the homogeneity and conformity indices were found between the control plans and the test plans (p > 0.05, Table iv).
TABLE IV.
Dose changes in target regions, using superficial parotid lobe–sparing technology
| Variable |
Plan
|
p Value | |
|---|---|---|---|
| Control | Test | ||
| ptvnx V110 (%) | |||
| Mean | 1.65±2.61 | 3.39±5.33 | 0.10 |
| Range | 0.00 to 8.78 | 0.00 to 22.83 | |
| ptvnx V100 (%) | |||
| Mean | 99.62±0.66 | 99.73±0.57 | 0.06 |
| Range | 97.80 to 100.00 | 97.89 to 100.00 | |
| ptvnx V95 (%) | |||
| Mean | 99.94±0.19 | 99.92±0.29 | 0.58 |
| Range | 99.21 to 100.00 | 99.10 to 100.00 | |
| V60 (%) | |||
| Mean | 99.91±0.20 | 99.86±0.39 | 0.64 |
| Range | 99.08 to 100.00 | 97.97 to 100.00 | |
| V54 (%) | |||
| Mean | 99.40±0.55 | 99.32±0.47 | 0.30 |
| Range | 97.88 to 99.97 | 98.34 to 99.95 | |
| Dmax | |||
| Mean | 77.95±1.88 | 78.84±2.56 | 0.07 |
| Range | 74.24 to 85.52 | 74.39 to 85.17 | |
| Dmean to ptvnx | |||
| Mean | 73.19±0.94 | 73.83±2.02 | 0.04 |
| Range | 70.87 to 74.81 | 71.32 to 78.25 | |
| Dmean to ptv1 | |||
| Mean | 69.77±1.57 | 70.15±1.67 | 0.01 |
| Range | 65.48 to 72.72 | 64.80 to 72.73 | |
| Dmean to ptv2 | |||
| Mean | 62.10±1.05 | 63.06±1.74 | 0.03 |
| Range | 59.80 to 64.91 | 60.15 to 69.90 | |
| Homogeneity index | |||
| Mean | 1.12±0.02 | 1.13±0.03 | 0.07 |
| Range | 1.09 to 1.18 | 1.09 to 1.22 | |
| Conformity index | |||
| Mean | 1.00±0.01 | 1.00±0.01 | 0.06 |
| Range | 0.98 to 1.00 | 0.98 to 1.00 | |
ptvnx, ptv1, ptv2 = planning target volume for the tumour, for the high-risk region, and for the potentially involved region; V110, V100, V95 = volume covered by more than 110%, 100%, or 95% of the prescribed dose; V60, V54 = percentage of the volume receiving 60 Gy or more, or 54 Gy or more; Dmax = maximum dose in target regions; Dmean = mean dose.
3.3. Evaluation of Dose to Other OARs
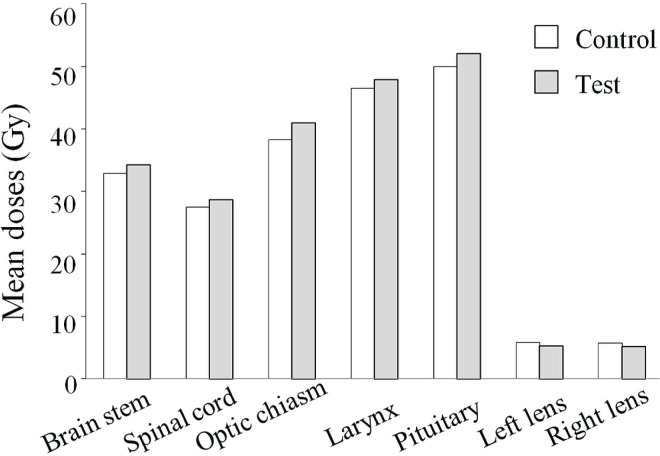
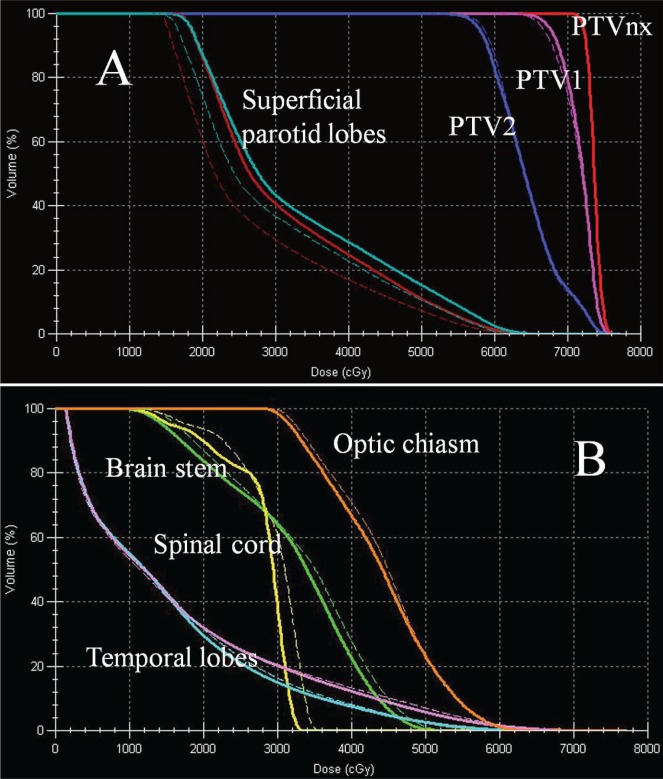
Bilaterally, the dose to the lenses dropped slightly in the test plan. Doses to other oars showed a small increase compared with doses in the control plans. In the test plans, the mean doses to the brainstem and spinal cord were 34.3 Gy and 28.7 Gy (increases of 1.4 Gy and 1.1 Gy respectively), the mean dose to the optic chiasm increased by 2.7 Gy to 41.0 Gy, the mean dose to the larynx increased by 1.4 Gy to 47.9 Gy, and the mean dose to the pituitary increased by 2.1 Gy to 52.1 Gy (Figure 3). For patients with T1–3 tumours, doses to all oars remained within acceptable limits. However, for patients with T4 tumours, the mean V60 (percentage volume receiving 60 Gy or more) for brainstem reached 3.2%. The mean doses to the optic chasm, pituitary, bilateral middle ears, optic nerves, and larynx exceeded the lower limit of acceptability, but remained below the upper limit. Figure 4 shows the changes in the dose–volume histogram for 1 patient.
FIGURE 3.
Changes in the dose to brainstem, spinal cord, optic chiasm, larynx, pituitary gland, and lenses between the control and test plans. Except for the lenses bilaterally, the mean dose to organs at risk increased slightly from the control to the test plans.
FIGURE 4.
Dose–volume histogram for changes in target and organs at risk for a patient with T3N1M0 nasopharyngeal carcinoma. Dotted lines represent test plans, solid lines represent control plans. (A) The mean doses to the left and right superficial parotid lobes decreased significantly, with no significant change in target regions. ptv = planning target volume. (B) Doses to some organs at risk, such as the brainstem and spinal cord, showed small increases, but were within the prescription.
4. DISCUSSION
Xerostomia is a common radiation-related complication in npc patients. Recently, imrt has greatly eased that problem by delivering tumouricidal doses to target regions and by reducing the dose to the parotid glands at the same time. Most data about the relationship between radiation dose and parotid gland function has come from research into head-and-neck cancers. For some patients with head-and-neck cancer, only the ipsilateral neck receives radiotherapy, and thus a low radiation dose to the contralateral parotid gland can be achieved.
Eisbruch et al.10 proposed that, given unstimulated and stimulated saliva flow rates respectively recovered to 76% and 114% of pre-radiotherapy values at 12 months as a criterion, a mean dose of less than 26 Gy to one entire parotid gland is the threshold dose. Patients whose parotid glands received more than 26 Gy experienced low unstimulated and stimulated saliva flow rates that could not recover over time. Blanco et al.16 also reported that, in conventional fractionation, a mean dose less than 25.8 Gy to one entire parotid gland could significantly lower the incidence of xerostomia; otherwise, saliva flow would be reduced to less than 25% of its pretreatment value. Münter et al.17 also reported that a mean dose of less than 26–30 Gy to the entire parotid could significantly preserve salivary gland function.
However, the foregoing criteria are difficult to meet in npc patients. Because of the special anatomic location and lymphatic drainage of the nasopharynx, both sides of the parapharynx and neck have to be included in radiation targets. As a result, the mean dose to the parotid usually exceeds 35 Gy. In 33 early-stage npc patients treated with imrt, Kwong et al.18 reported that the mean dose to the parotid gland was 38.8 Gy. In their study of 139 npc patients treated with imrt, Zhao et al.12 reported that the mean doses to the left and right parotid glands were 36.47 Gy and 36.72 Gy respectively. One year after radiotherapy, grades 0, 1, and 2 xerostomia were 10.6%, 64.9%, and 24.5% respectively. It is therefore urgent to lower the dose to the parotids in npc patients treated with imrt.
As already mentioned, the parotids as a whole are usually contoured as oars in dose optimization for imrt in npc patients. However, overlap of the targets and the deep lobes of the parotids make dose optimization with protection of the parotids difficult. In 20 npc patients with T3–4 disease, Chau et al.19 reported changes in their oar contouring of the parotid glands, splitting the organs into target-overlapping and non-target-overlapping subsegments. As a result, the mean dose to the parotids was reduced from 42 Gy to 38.6 Gy. At the same time, a significant improvement in target coverage and tumour control probability was able to be achieved.
In radiotherapy, the parotid can be considered a parallel organ. A V40 (percentage volume receiving 40 Gy or more) in the contralateral parotid gland of less than 33% has been reported to be satisfactory for complete salivary recovery after 24 months20, which suggests that if just part of the parotid were to be sufficiently protected, function could still be well preserved. The parotid gland is usually divided into superficial and deep lobes by the posterior border of the mandible or the facial nerve that threads through it. In the present study, we found that the superficial lobe of the parotid gland accounted for about 80% of the volume of the parotid gland as a whole, suggesting that a mean dose to the superficial parotid lobe of less than 26–30 Gy would preserve its function substantially.
In the test imrt plans, we used the superficial parotid lobes as the parotid oars during dose optimization. The results showed that, compared with the dose in the traditional plans, the mean dose to both entire parotid glands in the test plans declined by more than 4 Gy. Most importantly, the mean dose to the superficial parotid lobes in the test plans was 30 Gy or less regardless of clinical stage, and the V40 for the left and right parotids was 31.9% and 29.2% respectively. At the same time, we found that the dose distributions for the targets in T1–3 npc patients were not significantly different between the control plans and the test plans. The homogeneity and conformity indices also were not different between the control plans and the test plans. Hence, contouring the superficial lobes of the parotids as the parotid oars is feasible in imrt planning for T1–3 npc patients. However, in the test plans for T4 patients, we found that the percentage of the ptv receiving more than 110% of the prescription dose increased from 3.55% to 11.19% and that the mean V60 for the brain stem reached 3.2%. Those findings suggest that imrt plans that try to overprotect the parotids might be not suitable for npc patients with large local disease. In that situation, target coverage, rather than parotid protection, should be the first consideration.
5. CONCLUSIONS
A superficial parotid lobe–sparing delineation approach can significantly lower the mean dose to both entire parotid glands and to the superficial parotid lobes in T1–3 npc patients. This approach would be expected to result in less xerostomia and better quality of life for the patients so treated.
6. CONFLICT OF INTEREST DISCLOSURES
The authors declare that they have no competing interests.
7. REFERENCES
- 1.Abendstein H, Nordgren M, Boysen M, et al. Quality of life and head and neck cancer: a 5 year prospective study. Laryngoscope. 2005;115:2183–92. doi: 10.1097/01.MLG.0000181507.69620.14. [DOI] [PubMed] [Google Scholar]
- 2.Hammerlid E, Taft C. Health-related quality of life in long-term head and neck cancer survivors: a comparison with general population norms. Br J Cancer. 2001;84:149–56. doi: 10.1054/bjoc.2000.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hammerlid E, Silander E, Hörnestam L, Sullivan M. Health-related quality of life three years after diagnosis of head and neck cancer—a longitudinal study. Head Neck. 2001;23:113–25. doi: 10.1002/1097-0347(200102)23:2<113::AID-HED1006>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 4.Bjordal K, Ahlner–Elmqvist M, Hammerlid E, et al. A prospective study of quality of life in head and neck cancer patients. Part ii: longitudinal data. Laryngoscope. 2001;111:1440–52. doi: 10.1097/00005537-200108000-00022. [DOI] [PubMed] [Google Scholar]
- 5.de Graeff A, de Leeuw JR, Ros WJ, Hordijk GJ, Blijham GH, Winnubst JA. A prospective study on quality of life of patients with cancer of the oral cavity or oropharynx treated with surgery with or without radiotherapy. Oral Oncol. 1999;35:27–32. doi: 10.1016/S1368-8375(98)00049-9. [DOI] [PubMed] [Google Scholar]
- 6.Yeh SA, Tang Y, Lui CC, Huang YJ, Huang EY. Treatment outcomes and late complications of 849 patients with nasopharyngeal carcinoma treated with radiotherapy alone. Int J Radiat Oncol Biol Phys. 2005;62:672–9. doi: 10.1016/j.ijrobp.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Kam MK, Leung SF, Zee B, et al. Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol. 2007;25:4873–9. doi: 10.1200/JCO.2007.11.5501. [DOI] [PubMed] [Google Scholar]
- 8.Hsiung CY, Ting HM, Huang HY, Lee CH, Huang EY, Hsu HC. Parotid-sparing intensity-modulated radiotherapy (imrt) for nasopharyngeal carcinoma: preserved parotid function after imrt on quantitative salivary scintigraphy and comparison with historical data after conventional radiotherapy. Int J Radiat Oncol Biol Phys. 2006;66:454–61. doi: 10.1016/j.ijrobp.2006.04.033. [DOI] [PubMed] [Google Scholar]
- 9.Franzén L, Funegård U, Ericson T, Henriksson R. Parotid gland function during and following radiotherapy of malignancies in the head and neck. A consecutive study of salivary flow and patient discomfort. Eur J Cancer. 1992;28:457–62. doi: 10.1016/S0959-8049(05)80076-0. [DOI] [PubMed] [Google Scholar]
- 10.Eisbruch A, Ten Haken RK, Kim HM, Marsh LH, Ship JA. Dose, volume and function relationships in parotid salivary glands following conformal and intensity-modulated irradiation of head and neck cancer. Int J Radiat Oncol Biol Phys. 1999;45:577–87. doi: 10.1016/S0360-3016(99)00247-3. [DOI] [PubMed] [Google Scholar]
- 11.Chambers MS, Garden AS, Rosenthal D, et al. Intensitymodulated radiotherapy: is xerostomia still prevalent? Curr Oncol Rep. 2005;7:131–6. doi: 10.1007/s11912-005-0039-4. [DOI] [PubMed] [Google Scholar]
- 12.Zhao C, Lu TX, Han F, et al. Clinical study of 139 nasopharyngeal carcinoma patients for intensity modulated radiation therapy. Chin J Radiat Oncol. 2006;15:1–6. [Google Scholar]
- 13.Wang HJ, Zhao LH. Topographic Anatomy [Chinese] Beijing, China: People’s Medical Publishing House; 2005. pp. 12–13. [Google Scholar]
- 14.Radiation Therapy Oncology Group (rtog) A phase ii study of intensity modulated radiation therapy (imrt) +/chemotherapy for nasopharyngeal cancer [Web page] Philadelphia, PA: RTOG; 2011. [Available online at: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0225; cited August 28, 2011] [Google Scholar]
- 15.Shaw E, Kline R, Gillin M, et al. Radiation Therapy Oncology Group: radiosurgery quality assurance guidelines. Int J Radiat Oncol Biol Phys. 1993;27:1231–9. doi: 10.1016/0360-3016(93)90548-A. [DOI] [PubMed] [Google Scholar]
- 16.Blanco AI, Chao KS, El Naqa I, et al. Dose–volume modeling of salivary function in patients with head-and-neck cancer receiving radiotherapy. Int J Radiat Oncol Biol Phys. 2005;62:1055–69. doi: 10.1016/j.ijrobp.2004.12.076. [DOI] [PubMed] [Google Scholar]
- 17.Münter MW, Karger CP, Hoffner SG, et al. Evaluation of salivary gland function after treatment of head-and-neck tumors with intensity-modulated radiotherapy by quantitative pertechnetate scintigraphy. Int J Radiat Oncol Biol Phys. 2004;58:175–84. doi: 10.1016/S0360-3016(03)01437-8. [DOI] [PubMed] [Google Scholar]
- 18.Kwong DL, Pow EH, Sham JS, et al. Intensity-modulated radiotherapy for early-stage nasopharyngeal carcinoma: a prospective study on disease control and preservation of salivary function. Cancer. 2004;101:1584–93. doi: 10.1002/cncr.20552. [DOI] [PubMed] [Google Scholar]
- 19.Chau RMC, Leung SF, Kam MK, et al. A split-organ delineation approach for dose optimisation for intensity-modulated radiotherapy for advanced T-stage nasopharyngeal carcinoma. Clin Oncol (R Coll Radiol) 2008;20:134–41. doi: 10.1016/j.clon.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 20.Ortholan C, Chamorey E, Benezery K, et al. Modeling of salivary production recovery after radiotherapy using mixed models: determination of optimal dose constraint for imrt planning and construction of convenient tools to predict salivary function. Int J Radiat Oncol Biol Phys. 2009;73:178–86. doi: 10.1016/j.ijrobp.2008.03.068. [DOI] [PubMed] [Google Scholar]