Abstract
AIM of the study is to evaluate etiopathogenesis role played by predisposing conditions (Diabetes, Immunosupression), precipitating factors (trauma/surgery/ketoacidosis) and possible role of occupational hazard is discussed briefly. Clinical presentation and management of patients presenting with rhinoorbitocerebral mucormycosis is discussed. The prospective study of patient undergoing treatment of mucormycosis] without control Setting was done in ENT Deptt. NSCB Medical College, Jabalpur (tertiary referral centre of mid India). Subject were patients presenting with invasive fungal rhino sinusitis presenting with orbital involvement and cranial nerve palsies undergoing treatment. The detailed history, clinical examination including cranial nerve examination, blood test, CTscan and biopsy. Nasal endoscopy, CWL surgery and medical management with 6 month follow up. All six patients were diabetic when evaluated on presentation. Two patients had ketoacidosis. Four had history of surgery in recent past. Blood stained nasal discharge and dysaesthesia of face are early warning signs. They had necrotic lesion in nose and infraorbital area with 2, 3, 4, 5, 6 and 7 cranial nerve involvement. Skin necrosis/Mucosal necrosis, facial palsy and diplopia signify advanced disease. Altered sensorium, panopthalmitis & diabetes complicated with ketoacidosis signify bad prognosis. In present study two patients with advanced disease, altered sensorium and ketoacidosis succumbed within 72 hours in spite of anti fungal medicine. Of the four surviving patients, all responded well to treatment but had residual sixth and seventh nerve palsy. One patient defaulted in diabetes control & had recurrence after 6 months. Early diagnosis, aggressive surgical debridement and proper management of underlying metabolic abnormality along with amphotericin B can avert the bad prognosis of rhinoorbitocerebral mucormycosis.
Keywords: Rhino orbital, Mucormycosis, Cranial nerve paralysis, Diabetes melitis
Introduction
Mucormycosis is a term used to refer to any fungal infections of the order Mucorales, which belongs to class Zygomycetes. Rhinocerebreal mucormycosis is a rare but fatal infection of nasal cavity and sinuses. The incidence of mucormycosis is approximately 1.7 cases per 1,000,000 inhabitants per year [1]. Mucormycosis rarely affects otherwise healthy people [2]. It is disease of patients with pre-existing debilitating disease (diabetes melitis) or is receiving immunosuppressive therapy.
Orbito-cerebral Manifestations
Rhino-orbito-cerebral mucormycosis is known to exist in two forms, the well-known acute form and the less well-recognized chronic form. Acute rhinocerebral mucormycosis is an opportunistic but fulminant fungal infection of nose, sinuses, orbit and cranial structures. It aggressively spread to orbits and cranium within days [3]. In advanced disease chemosis, ptosis, proptosis, opthalmoplegia and blindness and multiple cranial nerve palsy (function of the cranial nerves II, III, IV, V and VI may be lost or impaired [4, 5]. A meticulous history, detailed workup, confirmation of diagnosis by histopathology and culture helps to make diagnosis. Aggressive management of these patients can reverse the adverse outcome. Prognosis is directly related to length of time before diagnosis and treatment. Invasive fungal disease complicating diabetes is usually referred late to ENT surgeon.
Materials and Methods
Six patients of uncontrolled diabetes mellitus with fungal invasive disease who had multiple cranial nerve involvement were studied prospectively from April 2006 to May 2008. Evaluation at presentation included a detailed history, ENT, ophthalmic, and neurological examination to assess the extent of disease, nasal endoscopy/CWL with biopsy. Diagnosis was made on histopathological examination. CT scan of PNS and brain were obtained to assess the extent of disease. Treatment with systemic amphotericin B was started as soon as the diagnosis of mucormycosis was established. Treatment was also instituted to stabilize the underlying metabolic derangement and surgical debridement were indicated.
Result of Study (Observation)
Six patients suffering from diabetes mellitus with biopsy proven mucormycosis involving 2nd, 3rd, 4th, 5th, 6th and 7th cranial nerves were studied. All patients had uncontrolled diabetes with 2 patients having ketoacidosis. Age ranged from 42 to 65 years (mean age 52 years). Male female ratio was 5:1. All were labourer by occupation (two farmer and one dairy worker). Duration of illness ranged from 10 days to 3 month.
Chief complaint was facial swelling, blood stained nasal discharge and crusting. All six patients had h/o prolonged antibiotic treatment with incomplete response. Four out of six had history of surgery/trauma (One had I & D, one cataract surgery and one was treated for head injury one month back, one tooth extraction). Facial dysesthesia was present in all on involved side.
Sign there was infra orbital anaesthesia on involved cheek. Infra orbital necrosis was present in 4 patient with palatal ulcer in two patients. All patient incidentally had left side lesion [unexplained in 3 rest 3 had h % minor surgery on side]. On anterior rhinoscopy all patients had black blood stained debris in region of inferior and middle turbinate along with necrosis on endoscopy. Vision was altered in all 6 with no vision in 2 and only perception of light in 4. These patient improved to finger counting during treatment. Eye movement were not demonstrated initial examination signifying altered 3, 4 and 6 nerve function. All had peri orbital oedema and ptosis, 7 cranial nerve palsy of lower motor type was present in all, two patient were irritable and disoriented and succumbed to disease within 48 hour of treatment.
Investigation All patient had raised blood sugar 240 mg/dl-and above 2 patient had ketosis. Urine sugar was positive in all. All were HIV and HBs antigen negative (Fig. 1).
Fig. 1.
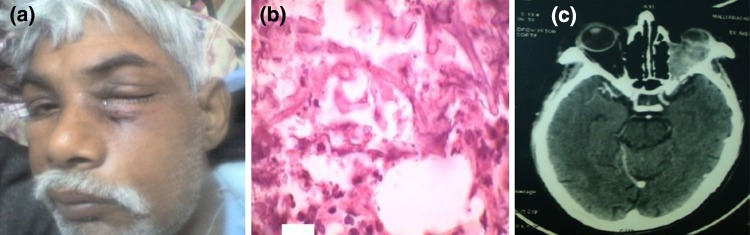
a Clinical photograph showing infra orbital necrosis. b Microscopic photograph showing hyphae in H and E stain. c CTscan showing periorbital involvement
CT Scan
Mucosal thickening of nose and paranasal sinus was present in all six patients and Bony destruction was present in 3 patients. One patient had supra ventricular hypodense focal lesion with edematous parenchyma. Nasal endoscopy and biopsy was done in all 6 patients. In 4 cases Cald Well Luc surgery and debridment was done. Histopathology demonstrated aseptate fungal hyphae in all patient. That formed the inclusion criteria for following study fungal culture was positive in only 3 patients in which culture specimen was taken from maxillary antrum mucosa.
Amphotericin B was given IV for 6 wks. Nasal and Antral lavage was also done with amphotericin. Four patients undergoing surgery responded well. There was improvement of vision, 3rd and 4th and, 5th cranial, nerve function recovered, Vision improvement started on 3rd day. All four patients had residual 6th and 7th nerve palsy at the end of 6 weeks of treatment. Two had fulminating disease and early mortality. Follow up at 6 months: out of 4 surviving patient there was persisting 6 and 7 nerve palsy. One had recurrent disease who had defaulted in diabetes control (Table 1).
Table 1.
Rhinoorbitocerebral mucormycosis master chart
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | ||
|---|---|---|---|---|---|---|---|
| 1 | Facial swelling/dysesthesia | + | + | + | + | + | + |
| 2 | Infra orbital necrosis | + | + | + | + | ||
| 3 | Hard palate perforation | + | + | ||||
| 4 | Nasal blockage/crusting | + | + | + | + | + | + |
| 5 | Blood stained discharge | + | + | + | + | + | + |
| 6 | 2nd, 3rd, 4th, 5th, 6th, 7th nerve palsy | + | + | + | + | + | + |
| 7 | Histopathology | Aseptate hyphae | Aseptate hyphae | Aseptate hyphae | Aseptate hyphae | Aseptate hyphae | Aseptate hyphae |
| 8 | Culture | +ve for fungus | +ve for fungus | +ve for fungus | |||
| 9 | CT scan(mucosal thickening) | + | + | + | + | + | + |
| 10 | CT scan (bony destruction) | + | + | + | |||
| 11 | Nasal endoscopy and biopsy | + | + | + | + | + | + |
| 12 | CWL and debridment | + | + | + | + | ||
| 1 | Diabetis | + | + | + | + | + | + |
| 2 | Ketoacidosis | + | + | ||||
| 3 | Duration of illness (days) | 90 | 17 | 21 | 60 | 10 | 28 |
| 4 | H/O surgery | + tooth extraction | + (I&D) | cataract | |||
| 5 | H/O trauma | + | H/of head injury |
Discussion
Mucormycosis is a rare fulminating opportunistic fungal infection caused by a fungus of the order mucorales [6, 7]. Mucormycosis infection in humans is usually acquired through airborne fungal spores, contamination of traumatized tissue, ingestion and direct inoculation [8]. For optimal growth in humans, mucorales fungi require the host to have decreased levels of neutrophils, since they play a key role in defense against the fungi in neutropenic individuals such as in chemotherapy patients or malignancy, pathogens proliferate in the host tissue can initiate aggressive and fulminating infection [9]. Depending on the immunological status of the host, the disease may manifest in six different ways depending on the affected site: rhinocerebral, pulmonary, cutaneous, gastrointestinal, central nervous system or miscellaneous. For example, patients with diabetes mellitus usually have the rhinocerebral and pulmonary forms of disease. Patients who are malnourished usually have the gastrointestinal forms of disease [10].
All six patients of our had uncontrolled diabetes which is a well-known predisposing factor for mucormycosis. Diabetes mellitus is most common and is associated with 40 % of mucormycosis cases overall and 70 % of patients with rhino cerebral mucormycosis [9]. High fatality with diabetes is due to the angioinvasive character of the Mucor, thereby causing thrombosis of blood vessels and tissue necrosis [11]. In the diabetic ketoacidotic patient, there is a high incidence of mucormycosis caused by Rhizopus oryzae, also known as Rhizopus arrhizus, because they produce the enzyme ketoreductase, which allows them to utilize the patient’s ketone bodies. It is also likely that the hyperglycemia stimulates fungal growth, and the diabetic reduction in chemotaxis and phagocytic efficiency permit these otherwise innocuous organisms to proliferate [12].
Sinonasal infection is most common manifestation of mucormycosis. In a study done by Ferry et al. [13] and by Yohai et al. [14] on mucormycosis cases, they reported sinus involvement in 69 and 79 % respectively. 70 % of the patient who developed rhinocerebral mucormycosis are in ketoacidosis with least resistance to infection (McNulty 1982) [15].
Rhino cerebral mucormycosis usually begins in the nasal mucosa, turbinate or palate and extends to the paranasal sinuses, spreading via the angular, lacrimal, and ethmoid vessels as well as by direct extension from the sinuses into the retro-orbital region [16]. The rhino orbital cerebral form is aggressive and begin with infection of nose in diabetes patient with Early symptoms of Non specific engorgement of turbinate, Nasal obstruction, Blood stained nasal discharge, black turbinate, facial dysesthesis. In advanced disease: chemosis, ptosis, proptosis, ophthalmoplegia and blindness and multiple cranial nerve palsy (function of the cranial nerves II, III, IV and VI may be lost or impaired [4, 5]. Typical clinical presentation includes facial pain, presence of an irregular black eschar on the palatal or nasal mucosa and drainage of pus from the eye and nose [17]. All these findings are consistent with all six of our cases and are suggestive of rhino cerebral mucormycosis.
Thrombosis of the internal maxillary artery or sphenoplatine artery caused by mucormycotic infection as a result of immunocompromised state due to chronic uncontrolled diabetes.
Radiology
Suspicion of mucormycosis requires a CT scan of the maxilla, orbits and brain. Radiographically, rhinocerebral mucormycosis has been associated with nodular thickening of sinus mucosa, sinus opacification without fluid levels, and spotty destruction of the bony walls of paranasal sinuses In particular, evidence of intracranial brain abscesses and orbital extensions is critical [12]. Magnetic resonance imaging of the head is useful in determining the extent of disease involvement, so that surgical margin can be planned [18]. It has been suggested that any diabetic patient in a ketoacidotic state who presents with clinical and radiographic findings of rhino sinusitis should be suspected as having mucormycosis until proven otherwise [19].
Histopathology and Microbiology
Early diagnosis and treatment are of extreme importance for successful eradication of infection and for patient survival. Serological assays for Mucor antigens have been developed. However, these assays remain investigational. Confirmation of the diagnosis is best obtained with a tissue specimen from the junction of necrotic and non necrotic tissue. The Grocott-Gomori methenamine silver stain is the most effective for identifying fungi, staining with methenamine silver or a PAS stain/Calcofluor white, in addition to H and E, will often show the organism in vessel walls or nerve bundles [5]. Spores are black or brown and smooth in appearance [20] but microscopically spores are more prominent in aspergillosis than in mucormycosis [21]. Invasion of the tissue by fungal non septate hyphae and right angle branching is present in mucormycosis specimens speciation requires culture of fungus and the advice of a mycologist with a special interest in the Mucorales. Because initial cultures of diseased tissue may be negative, histopathological examination is essential for early confirmation diagnosis [17, 22].
Medical management alone is not effective because of poor drug delivery to the infection due to extensive vascular thrombosis [23]. Systemic antifungal therapy includes the use of high dose amphotericin-B and is associated with an overall survival rate of 72 %. It is usually given in dextrose 5 % in water intravenously at a dose of 1.0–1.5 mg/kg daily since its usage is associated with renal toxicity and it requires careful monitoring of serum urea nitrogen, blood urea nitrogen potassium, creatinine as well as creatinine clearance as an essential part of the therapy. Recently, studies have shown that liposomal amphotericin B and fluconazole, caspofungin. Hyperbaric oxygen therapy (believed to improve neutrophilic killing by higher oxygen delivery, low dose of heparin, anti inflammatory medicine can be used with good success [24–26]. Mucormycosis is a severe tissue-loss and life-threatening disease. Aggressive control of the underlying disease and aggressive debridement are needed. Rehabilitation or closure of the existing oronasal fistula can be done surgically or by construction of a obturator with a removable prosthesis to support speech and feeding [12].
Mucormycosis is a rapidly progressive disease with a fulminant course and fatal outcome unless diagnosed early and treated rapidly. Until 1950 mucormycosis was universally fatal with amphotericin B, which crosses blood brain barrier survival improved. The prognosis is directly related to the severity of the underlying disease, the extent of the disease when treatment begins and the aggressiveness of the treatment. Survival of patient with no underlying disease is 60 %. However it is only 10 % in patients with other more significant underlying disease (Blitzer 1980). Ericson and colleagues reported survival of 80 % where medical and surgical treatment were given [27]. Strauss and colleague reported 40 % survival [28]. Death rate remains high if direct CNS invasion is found at initial examination [29].
Facial palsy with fungal rhinosinusitis is a well known entity which is reported randomly. Bell’s palsy is known in diabetic but diabetics with fungal rhinosinusitis with facial nerve palsy show poor recovery of nerve function. Although isolated cranial nerve palsy common in diabetes simultaneous multiple cranial neuropathy are rare and if present mucormycosis septic cavernous sinus thrombosis and diabetic polyneuropathy should be suspected. 3rd 4th, 5th and 6th cranial Nerve palsy can be initial presenting sign (You Mi Song) [4]. Ferry et al. [13] reported 16 patients in them rhinological symptoms where most common were present in 11 out of 16, Ocular in 6 and facial in 5.
Prognosis is dependent on multiple factors and early initiation of treatment is an important element. A multi-disciplinary approach consisting of dental specialists, ENT surgeons, ophthalmologists and neurologist is critical in successful management of a patient with mucormycosis. Hence the general approach is to treat early, aggressively and with all modalities available.
Conclusion
The following significant points were observed patients are usually treated long before ENT opinion is sought. Poor response to prolong antibiotic treatment in diabetic should raise the suspicion of fungal disease. Blood stained nasal discharge is usually a warning sign. Cranial nerve palsy with eye involvement in diabetics was the usual alerting sign. Thorough history, supported by detailed examination confirm by biopsy supplemented by CT along with surgical and medical management are required. Bell’s palsy is known to occur in diabetics however multiple cranial nerve palsy should raise suspicion of mucormycosis.
References
- 1.Bouza E, Munoz P, Guinea J. Mucormycosis: an emerging disease. Clin Microbiol Infect. 2006;12:7–23. doi: 10.1111/j.1469-0691.2006.01604.x. [DOI] [Google Scholar]
- 2.Singh J, Prasdnna NM. Phycomycosis in an apparently normal host. J Otolaryngol. 1977;6:37–42. [PubMed] [Google Scholar]
- 3. Haward W, Smith MD, John A, Kirchner et al (1985) Cerebral mucormycosis. Otolaryngol Clin N Am 68:715–726
- 4.You Mi Song MD, Sun Yang Shim MD. Bilateral opthalmic artery occlusion in rhinoorbital cerebral mucormycosis. Korean J Opthalmol. 2008;22:66–69. doi: 10.3341/kjo.2008.22.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Singh NP, Garg S, Kumar S, Gulati S (2006) Multiple cranial nerve palsy associated with type 2 DM. Singap Med J 47(8):712–5 [PubMed]
- 6.Shafer, Hine, Levy (eds) (2006) Shafer’s textbook of oral pathology, 5th edn. Rajendran, Sivapathasundharam Elsevier, Reed Elsevier India Private Limited, pp 510–511
- 7.Parfrey NA. Improved diagnosis and prognosis of mucormycosis: a clinicopathological study of 33 cases. Medicine (Baltimore) 1986;65:113–123. doi: 10.1097/00005792-198603000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Sugar AM. Mucormycosis. Clin Infect Dis. 1992;14:S126–S129. doi: 10.1093/clinids/14.Supplement_1.S126. [DOI] [PubMed] [Google Scholar]
- 9.Pak J, Tucci VT, Vincent AL, Sandin RL, Greene JN. Mucormycosis in immunochallenged patients. J Emerg Trauma Shock. 2008;1:106–113. doi: 10.4103/0974-2700.42203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Topazian RG, Goldberg MH. Oral and maxillofacial infections. 4. Philadelphia: WB Saunders Company; 2002. pp. 253–254. [Google Scholar]
- 11.West BC, Oberle AD, Chung KJ. Mucormycosis caused by Rhizopus microsporus: cellulitis in the leg of a diabetic patient cured by amputation. J Clin Microbiol. 1995;33:3341–3344. doi: 10.1128/jcm.33.12.3341-3344.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marx RE, Stern D. Oral and maxillofacial pathology: a rationale for diagnosis and treatment. 1. Chicago: Quintessence Publishing Co Inc.; 2006. pp. 104–106. [Google Scholar]
- 13.Ferry AP, Abedi S. Diagnosis and management of rhino-orbital cerebral mucormycosis (phycosis): a report of 16 personally observed cases. Ophthalmology. 1983;90:1096–1104. doi: 10.1016/S0161-6420(83)80052-9. [DOI] [PubMed] [Google Scholar]
- 14.Yohai RA, Bullock JD, Aziz AA, Markert RJ. Survival factors in rhino-orbital-cerebral mucormycosis. Surv Ophthalmol. 1994;39:3–22. doi: 10.1016/S0039-6257(05)80041-4. [DOI] [PubMed] [Google Scholar]
- 15.Spellberg B, Edwards J, Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005;18(3):556–569. doi: 10.1128/CMR.18.3.556-569.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salisbury PL, Caloss R, Jr, Cruz JM, Powell BL, Cole R, Kohut RI. Mucormycosis of the mandible after dental extractions in a patient with acute myelogenous leukemia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:340–344. doi: 10.1016/S1079-2104(97)90240-7. [DOI] [PubMed] [Google Scholar]
- 17.Tugsel Z, Sezer B, Akalin T. Facial swelling and palatal ulceration in a diabetic patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:630–636. doi: 10.1016/j.tripleo.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 18.Neville BW, Damm DD, Alle CM, Bouquot JE. Oral and maxillofacial pathology. 2. Philadelphia: Saunders Company Ltd.; 2005. [Google Scholar]
- 19.Van der Westhuijzen AJ, Grotepass FW, Wyma G, Padayachee A. A rapidly fatal palatal ulcer: rhinocerebral mucormycosis. Oral Surg Oral Med Oral Pathol. 1989;68:32–36. doi: 10.1016/0030-4220(89)90111-4. [DOI] [PubMed] [Google Scholar]
- 20. Pelczar MJ, Chan EC, Krieg NR (1993) Microbiology, 5 th edn. Tata McGraw Hill publishing company Ltd
- 21.Eversole LR. Clinical outline of oral pathology diagnosis and treatment. 3. London: BC Decker Inc.; 2002. [Google Scholar]
- 22.Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000;13:236–301. doi: 10.1128/CMR.13.2.236-301.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith JL, Stevens DA. Survival in cerebro-rhino-orbital zygomycosis and cavernous sinus thrombosis with combined therapy. South Med J. 1986;79:501–504. doi: 10.1097/00007611-198604000-00028. [DOI] [PubMed] [Google Scholar]
- 24.Cagatay AA, Oncü SS, Calangu SS, Yildirmak TT, Ozsüt HH, Eraksoy HH. Rhinocerebral mucormycosis treated with 32 gram liposomal amphotericin B and incomplete surgery: a case report. BMC Infect Dis. 2001;1:22. doi: 10.1186/1471-2334-1-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koçak R, Tetiker T, Koçak M, Baþlamiþli F, Zorludemir S, Gönlüþen G. Fluconazole in the treatment of three cases of mucormycosis. Eur J Clin Microbiol Infect Dis. 1995;14:559–561. doi: 10.1007/BF02113443. [DOI] [PubMed] [Google Scholar]
- 26.Couch L, Theilen F, Mader JT. Rhinocerebral mucormycosis with cerebral extension successfully treated with adjunctive hyperbaric oxygen therapy. Arch Otolaryngol Head Neck Surg. 1988;114:791–794. doi: 10.1001/archotol.1988.01860190095032. [DOI] [PubMed] [Google Scholar]
- 27.Ericsson M, Anniko M, Gustafsson H, et al. A case of chronic progressive [rhinocerebral mucormycosis treated with liposomal amphotericin B and surgery. Clin Infect Dis. 1993;16(585):586. doi: 10.1093/clind/16.4.585. [DOI] [PubMed] [Google Scholar]
- 28. Strauss MD, Kennedy RJ, Adam RD (1996) Therapy with amphothericin B lipid complex. Arch Intern Med 156:337–340 [DOI] [PubMed]
- 29.Choi HY, Jew JN, Jackson IT (1992) Rhinocerebral mucormycosis combined with brain abscess. Eur J Plast Surg 15(3):146–150


