Abstract
The nasopalatine duct cyst is the most common non-odontogenic developmental cysts. Nasopalatine duct cyst also termed as incisive canal cyst, arises from embryologic remnants of nasopalatine duct. Most of these cysts develop in the midline of anterior maxilla near the incisive foramen. This article reports a case and review of literature with respect to epidemiology, etiology, clinical presentation, radiographic and pathological findings, treatment and recurrence rates.
Keywords: Nasopalatine duct cyst, Non-odontogenic cyst, Incisive canal cyst, Median palatine cyst
Introduction
The nasopalatine ducts communicates with the nasal cavity in the anterior region of the maxilla. It is located on the palatal aspect in midline of maxilla; above the retroincisor palatal papilla. During fetal development the ducts gradually narrow until 1 or 2 central clefts are finally formed on the midline of the upper maxilla. The nasopalatine neurovascular bundle is located within the duct, and emerges from its intrabony trajectory through the nasopalatine foramen. There can be as many as six different foramina, though there are usually only two, with independent neurovascular bundles (right and left) the vascular and neural elements can emerge separately; in this sense, foramina containing exclusively vascular elements are known as Scarpa’s Foramina (Figs. 1, 2) [1].
Fig. 1.

Radiograph showing well-defined round radiolucent area between the roots of maxillary central incisors
Fig. 2.

Surgical picture showing the cystic area in the anterior part of the palate
The nasopalatine duct cyst (NPDC) was first described by Meyer in 1914 [2]. It is also know by other names such as anterior midline cyst, maxillary midline cyst, anterior middle palatine cyst, and incisive duct cyst were regarded as fissural cyst in the past [3]. At present according to the classification of the World Health Organization (WHO) it is regarded as developmental, epithelial, non-odontogenic cysts of the maxilla along with nasolabial cysts. It is considered to be the most common of the non-odontogenic cysts, occurring in about 1% of the population. The majority of cases occur between 4th and 6th decade of life. It is slightly more common in males than in females. These cysts are usually asymptomatic. On occasion, they may present as soft tissue mass (Figs. 3, 4, 5) [1].
Fig. 3.
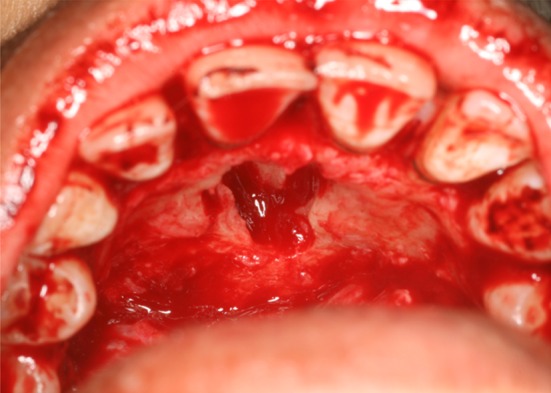
Post-surgical photograph showing cystic cavity
Fig. 4.

Photomicrograph of H&E stained section showing well-defined cystic lumen lined by pseudostratified ciliated columnar epithelium along with mucous glands in the CT wall (04 × 10). Inset showing photomicrographic high-power view of pseudostratified ciliated columnar epithelium (40 × 10)
Fig. 5.
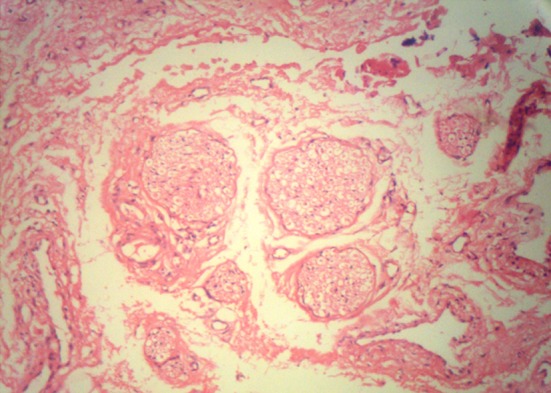
Photomicrograph of H&E stained section showing neurovascular elements in the deeper areas of CT (10 × 10)
Case Report
The case presented here is that of a 36 year old woman with a swelling in the anterior part of the palate for past 6 months. The swelling gradually increased to the present size. Extra orally no abnormality was detected.
Intra oral examination revealed a well defined swelling approximately 20 mm × 30 mm located posterior to the palatine papilla. On palpation the swelling was fluctuant and non tender. Occlusal radiograph showed well circumscribed oval shaped radiolucency in the midline of anterior maxilla between the roots of central incisors. No evidence of resorption of the tooth roots. On the basis of clinical and radiographic evidence a provisional diagnosis of Nasopalatine duct cyst was made. The specimen was excised under local anesthesia adapting the usual palatal approach and sent for histopathological examination fixed in 10% formalin.
Histopathological Examination
Microscopic examination revealed fibrous wall lined by pseudostratified ciliated columnar epithelium and partly by stratified squamous epithelium. Few nerve bundles, blood vessels and mucous cells were seen in the cyst wall.
Discussion
The NPDC is the most common developmental, non-neoplastic, non-odontogenic cysts of the oral cavity, occurring in about 1% of population [1]. They are believed to develop from remnants of paired embryonic nasopalatine ducts [3]. NPDC is one of the many pathologic processes that may occur within the jaw bones, but is unique in that it develops in only a single location, which is the midline of the anterior maxilla [4]. It can arise at any age, but is seen most often in patients between 30 and 60 years of age [2, 5] though there have been reports of NPDCS in pediatric patients up to 8 years of age [1]. It is slightly more common in males than in females; the ratio being 3:1 which could be because women typically seek dental help sooner than men [2]. Due to a lack of representative studies, it is not fully clear whether NPDCS are more common in Caucasians, Negroes or Asians [6].
Nasopalatine ducts ordinarily undergoes progressive degeneration however, the persistence of the epithelial remnants may later become the source of epithelia that gives rise to NPDC, from either spontaneous proliferation [7] or proliferation following trauma(e.g. removable dentures), bacterial infection or mucous retention [6]. Genetic factors have also been suggested [1, 5]. The mucous glands present among the proliferating epithelium can contribute to secondary cyst formation by secreting mucin within the enclosed structure [8]. The etiology is not clear, though in addition to the hypothesis of spontaneous proliferation from embryonic tissue remains. However few authors consider an unknown etiology or spontaneous proliferation to be the most plausible explanation, based on studies reporting cystic degeneration phenomena in the incisal duct and on the midline of the palate in human fetuses, in which the above mentioned circumstances are unable to have occurred [1].
There have even been exceptional reports such as the casual diagnosis of NPDC 9 months after rapid surgical palatal expansion or NPDC associated to the presence of two bilateral mesiodens [1]. NPDC can form within the incisive canal which is located in the palatine bone and behind the alveolar process of the maxillary central incisors, or in the soft tissue of the palate that overlies the foramen, called the cyst of the incisive papilla [5].
These cysts are usually asymptomatic and discovered on routine radiographs. The most common presenting symptoms are swelling of the anterior palate, drainage and pain. Rarely a large cyst may produce a “through-and-through” fluctuant expansion involving the anterior palate and labial mucosa. If the cyst is near the surface the swelling will be fluctuant with a bluish hue. Deeper cysts are covered by normal mucosa, unless it is ulcerated. Burning sensation and numbness may be experienced due to pressure on the nasopalatine nerve. Occasionally they cause intermittent discharge with a salty taste. Displacement of teeth is a rare finding [1].
Radiographically it appears as a round or ovoid radiolucency between the roots of the central incisors. Due to superimposition of the nasal spine, a heart shaped appearance may be seen. Most of the lesions have a well defined sclerotic border [1, 5]. In some individuals, a prominent incisive canal can appear as a radiolucent area and mimic NPDC. Most authors agree that 6 mm should be considered the upper limit for normal incisive canal radiolucencies larger than this should be considered potentially pathologic and merit further investigation [1].
The differential diagnosis should be established with the following conditions:
Odontogenic cysts (e.g., lateral radicular cyst, lateral periodontal cyst, odontogenic keratocyst).
Odontogenic tumors (e.g., ameloblastoma, odontogenic myxoma).
Non-odontogenic tumors (e.g., central giant tumor, brown tumor of hyperparathyroidism, central hemangioma) [1].
A through differential diagnosis must be established in order to avoid unnecessary treatments such as endodontic procedures in vital permanent upper central incisors [5]. A correct tentative diagnosis should be based on positive dental vitality testing and negative percussion findings of the permanent upper central incisors provided these teeth do not have pulp or periodontal problems. Radiological exploration is essential for diagnosing NPDCs, and in addition o panoramic X-rays, other complimentary techniques are advised, such as periapical and occlusal radiographs and computed tomography. The latter technique offers maximum guarantees in establishing a tentative diagnosis, since it generates a great detail of the structures (normally intact) adjacent to the lesion [1].
Histopathological examination reveals a cavity lined by epithelium and surrounded by connective tissue wall. A reported 71.8% of NPDCs have squamous, columnar, cuboidal or some combination of these epithelial types; respiratory epithelium is seen in 9.8% [5]. The type of epithelia that line the nasopalatine duct is highly variable, depending upon the relative proximity of the nasal and oral cavities. The most superior part of the duct is characterized by a respiratory type of epithelial lining and moving downwards the lining changes to cuboidal epithelium. In the most inferior portion closest to the oral cavity, squamous epithelium is the usual type [1].
The cyst wall may contain a chronic inflammatory reaction consisting of lymphocytes and plasma cells. Also helpful in the diagnosis of NPDC are the presence of neurovascular bundles, mucous glands and adipose tissue [1].
The hypekeratotic feature noted in Odontogenic Keratocyst can also be found in NPDC and is associated with a poorer prognosis, since the relapse rate is higher (close to 30%) [9]. Squamous cell carcinomas originating in maxillary bone are mainly due to the metaplasia experienced by the epitheial wall of a cyst or of the epithelial remains that participate in odontogenesis therefore there are cases in which NPDC gives rise to squamous cell carcinoma in the anterior zone of the upper maxilla [10].
The treatment of choice is surgical excision of the cyst, although some authors propose marsupalization of large cysts. The neurovascular bundle is a delicate and highly vascularized structure giving rise to profuse bleeding if inadvertently sectioned during surgery. Electrocoagulation is required in such cases. In squamous cell carcinoma radical en block resection of the anterior region of upper maxilla is required [1].
Conclusion
NPDC occurs in approximately 1% of the population. Presentation may be asymptomatic or include swelling, pain and drainage from the hard palate. A well circumscribed, round, ovoid or heart shaped radiolucency is seen on radiograph. Histopathological findings reveal squamous or respiratory cell types, or a combination of these, infiltrated by inflammatory cells. Enucleation is the preferred treatment with low recurrence rate.
References
- 1.Francoli JS, Marques NA, Aytis LB, Escoda CG. Nasopalatine duct: report of 22 cases and review of literature. Med Oral Patol Oral Cir Bucal. 2008;13(7):E438–E443. [PubMed] [Google Scholar]
- 2.Vasconcelos R, De Aguair MF, Castrow De, Araujo VC, Mesquita R. Retrospective analysis of 31 cases of nasopalatine duct cyst. Oral Dis. 1999;5(1):325–328. doi: 10.1111/j.1601-0825.1999.tb00098.x. [DOI] [PubMed] [Google Scholar]
- 3.Robertson H, Palacios E. Nasopalatine duct cyst. Ear Nose Throat J. 2004;83(5):313. [PubMed] [Google Scholar]
- 4.Kly N, Sheehy EC, Mc Donald F. Nasopalatine duct cyst: a case report. Int J Paediatr Dent. 2001;11(2):135–137. doi: 10.1046/j.1365-263x.2001.00248.x. [DOI] [PubMed] [Google Scholar]
- 5.Gnanasekhar JD, Walvekar SV, Al-kandari AM, Al-Duwairi Y. Misdiagnosis and mismanagement of nasopalatine duct cyst and its corrective therapy. A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(1):465–470. doi: 10.1016/S1079-2104(05)80372-5. [DOI] [PubMed] [Google Scholar]
- 6.Swanson KS, Kaugars GE, Gunsolley JC. Nasopalatine duct cyst: an analysis of 334 cases. J Oral Maxillofac Surg. 1991;49(3):268–271. doi: 10.1016/0278-2391(91)90217-A. [DOI] [PubMed] [Google Scholar]
- 7.Mermer Rw, Rider CA, Cleveland DB. Nasopalatine duct cyst: a rare sequelae of surgical rapid palatal expansion. Oral Surg Oral Med Oral Pathol Oral Radiol Endodon. 1995;80(6):620. doi: 10.1016/S1079-2104(05)80238-0. [DOI] [PubMed] [Google Scholar]
- 8.Regezi JA, Sciubba JJ, Jordan RCK. Oral pathology: clinical pathology correlations. St. Louis: Saunders; 2003. pp. 256–257. [Google Scholar]
- 9.Yih WY, Krump JL. Odontogenic keratocyst in the nasopalatine duct associated with mural cartilaginous metaplasia. J Oral Maxillofac Surg. 2005;63(9):1382–1384. doi: 10.1016/j.joms.2005.05.305. [DOI] [PubMed] [Google Scholar]
- 10.Takagi R, Ohashi Y, Suzuki M. Squamous cell carcinoma in the maxilla probably originating from Nasopalatine duct cyst: report of case. J Oral Maxillofac Surg. 1996;54(1):112–115. doi: 10.1016/S0278-2391(96)90318-3. [DOI] [PubMed] [Google Scholar]


