Abstract
Objective
To describe the theoretical basis, use, and satisfaction with Teen CHAT, an online educational intervention designed to improve physician-adolescent communication about healthy weight.
Methods
Routine health maintenance encounters between pediatricians and family practitioners and their overweight adolescent patients were audio recorded, and content was coded to summarize adherence with motivational interviewing techniques. An online educational intervention was developed using constructs from social cognitive theory and using personalized audio recordings. Physicians were randomized to the online intervention or not, and completed post-intervention surveys.
Results
Forty-six physicians were recruited, and 22 physicians were randomized to view the intervention website. The educational intervention took an average of 54 minutes to complete, and most physicians thought it was useful, that they would use newly acquired skills with their patients, and would recommend it to others. Fewer physicians thought it helped them address confidentiality issues with their adolescent patients.
Conclusion
The Teen CHAT online intervention shows potential for enhancing physician motivational interviewing skills in an acceptable and time-efficient manner.
Practice Implications
If found to be effective in enhancing motivational interviewing skills and changing adolescent weight-related behaviors, wide dissemination will be feasible and indicated.
Keywords: Motivational interviewing, obesity, overweight, adolescents, physician-patient communication, tailored intervention
1. Introduction
One of the major healthcare challenges in the 21st century is obesity, (1) and confronting this problem in the younger population is critical. (2) Almost one in five children are obese and one out of three are overweight, (3) yet effective interventions that can reach most overweight and obese adolescents do not exist. While surgical treatment of obesity has been successful, such an extreme intervention is limited to only the most at-risk adolescents; the effectiveness of medications is modest and side effects are prominent. Hence, the primary focus of treatment remains behavioral lifestyle interventions, (4) many taking place in the primary care office. Even modest interventions for children and adolescents can have significant long-term public health impacts. A recent analysis of health care costs estimated that even a one-percentage point reduction in the prevalence of adolescent obesity could translate into over $500 million in annual health care cost savings. (5)
Physicians must play a role in any broad behavioral interventions, after all, most adolescents report having a usual source of care, and between 50% and 80% of adolescents see a health care provider each year. (6) Patients expect physicians to address weight, and when the physicians do not, they assume weight is not a concern. Further, expert committee recommendations emphasize the role of primary care physicians in preventing, assessing, and treating child and adolescent obesity. (7) These recommendations include counseling about healthy eating and physical activity by targeting specific behaviors while using patient-centered communication.
Effective communication is patient-centered. When physicians use patient-centered communication, defined as showing empathy, having interpersonal sensitivity, forming partnerships, and mutually exchanging information, (8) patients might be more likely to change. (9) Motivational interviewing (MI) is one approach to patient-centered communication that addresses behavior change. MI may be used by health care providers to explore and resolve ambivalence regarding behavioral change. (10) When physicians use MI when speaking with patients, they seek to elicit patients’ own reasons for change, act as partners, are supportive, explore their patients’ concerns, and convey that patients are the drivers of their own change process. Our group noted that, even without specific MI-training, some physicians use MI techniques during adolescent clinical encounters, and that use of these techniques is associated with positive patient behaviors such as exercising more and with a decrease in self-reported weight one month after the clinical encounter. (9) Similar results were found with adults: patients of physicians who used MI techniques were more likely to lose weight whereas patients of physicians who did not gained weight. (11)
While MI techniques show promise, many physicians have not been taught this counseling approach. Although many regard the ability to communicate as an inborn talent, these skills can be learned, and practice experience alone does not improve physician communication. Rigorous evaluations of communications skills teaching, specifically those that have trained physicians to use MI techniques, have shown positive results when interventions incorporate adult learning principles, practice, and feedback in settings supervised by trained facilitators, (12–16) with effects noted up to two years after the training. (16) However, such workshops are often costly, time-intensive, and often do not allow physicians to learn at their own pace.
Given these limitations, we developed Teen CHAT, a personalized, online, training program to enhance MI behaviors in physician counseling for overweight and obese adolescents. We partly modeled the intervention after one we had previously developed for oncologists to address patient emotion (17) which doubled the times oncologists responded empathically to a patient expression of negative emotion and also was related to higher patient trust. (18) Here we describe the basic structure of the Teen CHAT study, the theoretical basis of the intervention, content development and format of the intervention, and describe physician use of and satisfaction with the intervention.
2. Methods
2.1 Overview
Teen CHAT is a two-arm clinical trial with participating physicians randomized to the Teen CHAT MI-based intervention or to no intervention. In the baseline phase, we audio recorded between three and five encounters between each physician and their overweight and obese adolescents who were in the clinic for annual well visits. We used these encounters to tailor the intervention. In the post-intervention phase, we are audio recording between four and six encounters per physician. The primary outcomes of Teen CHAT are to increase physician use of MI techniques. Secondary outcomes are to improve patients’ weight, physical activity, and nutrition three months after the encounter.
We recruited 46 physicians from general pediatrics and family practice groups. All physicians completed baseline surveys regarding discomfort discussing weight, nutrition, and physical activity with patients, self-efficacy for counseling about weight, outcome expectations for counseling, barriers to counseling, and concerns about reimbursement. Study staff reviewed all upcoming routine well-visit and chronic care appointments for patients 12–18 years old for each physician, and these patients were prescreened for BMI. Patients with a BMI ≥85th percentile were sent introductory letters from the treating physician describing the study with a phone number to call to immediately opt-out of participation. If the patient or parent did not decline participation, study staff called to screen for eligibility. After the patient and parent provided verbal assent/consent, study staff administered a baseline survey with the patient over the phone. On the day of the encounter, study staff obtained written consent/assent from parent and patient, respectively, and audio recorded the physician-patient encounter. Immediately after the recorded visit, physicians completed brief surveys about time constraints and content of the visit. Patients also completed a post-visit survey and follow-up face-to-face survey 3 months after the encounter.
Physicians were then randomized to either the control arm or to receive the online, tailored intervention described below. Following the intervention, staff will audio record a new set of four to six adolescent encounters per physician.
2. 2 The Teen CHAT Intervention
2.2.1 Theoretical Basis
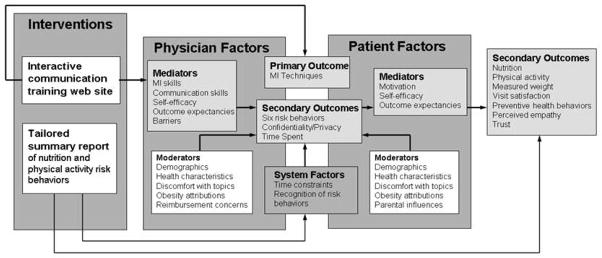
The Teen CHAT conceptual model is summarized in Figure 1. The primary intervention is an individually tailored interactive communication training web site to be used by physicians. We also created individually-tailored patient reports to be reviewed by physicians at the time of their patients’ appointments. The written report provides information regarding nutrition and physical activity risk behaviors and was designed to address system factors such as physician time constraints and to assist in recognition of risk behaviors. The six targeted risk behaviors were chosen because of evidence linking these behaviors with healthy weight in children and adolescents and included physical activity (minutes per day), screen time (hours per day), sleep (hours per day), breakfast consumption (days per week), fast food (meals per week), and sweetened drink consumption (servings per day). These summarized risk behaviors comprised secondary outcomes of the Teen CHAT study. Information on the patient report was collected via phone interview with the adolescent patient prior to the medical visit, and the report was printed and given to the physician at the time of the patient’s routine healthy maintenance visit. Additional information regarding potential moderators were also collected from patients and physicians.
Figure 1. Conceptual model.
(adapted from Walsh & McPhee (30))
The training web site was designed to improve primary care physicians’ communication with their overweight and obese adolescent patients regarding healthy nutrition and exercise with an emphasis on the primary outcome, enhancing MI skills. The intervention model emphasized constructs from social cognitive theory (19) and a physician-barrier model proposed by Cabana. (20) Specifically, the model identifies the following challenges: 1) physicians often lack the knowledge, skills, and self-efficacy to motivate adolescents to change behaviors; 2) physicians may have negative outcome expectations about the impact their counseling has on patients’ ability to change; 3) physicians may be overwhelmed by competing demands of other aspects of the adolescent preventive health visit and not have time to address nutrition and physical activity effectively; and 4) when physicians do not communicate well, patients may feel discouraged or may feel that they do not need to change. We then identified the following precepts to address these challenges: 1) physicians can learn how to counsel using MI techniques and can learn to avoid unhelpful communication behaviors; 2) physicians can feel more confident about their ability to communicate and believe that their counseling makes a difference; and 3) patients will be more likely to change when counseled by confident, skilled physicians.
2.2.2. Content development
Our interdisciplinary team with expertise in doctor-patient communication, multi-media education, health promotion and adolescent health developed the content of the intervention. The Teen CHAT online program was divided into four educational modules, each with specific educational objectives. These objectives included: 1) Understand how high quality counseling can lead to improved nutrition and physical activity in adolescents; 2) Apply MI techniques that will help motivate teen patients to make healthy changes; 3) Learn the “5 A’s” (Ask, Advise, Assess, Assist, and Arrange), a step-by-step approach to counseling about weight related topics and 4) Develop skills to enhance communication with adolescents.
Key concepts related to the four learning objectives were identified (see Table 1). Modules included written text that was professionally narrated, graphs, still photos, and brief interactive exercises. Content areas more focused on skill development, such as training in MI techniques, included exemplar video vignettes our team produced for this project using primary care physicians and actors portraying adolescent patients and their parents. These video examples included behaviors to incorporate (open questions, reflections, and praise) and behaviors to avoid (giving advice without permission, confronting, and showing disapproval). Most videos included “direct to camera” interviews with both physicians and patients reflecting on their experiences and reiterating key communication skills demonstrated during the encounter. Example scripts for two of these videos are included in text boxes 1 (“Avoid Judging”) and 2 (“Ask Permission”). The 5 A’s is a framework developed for smoking cessation counseling in the office setting, and is also useful for most areas of preventive counseling in primary care. (21, 22) The adolescent communication module covered: 1) Adolescents don’t like being treated like children; 2) adolescents expect physicians to be their doctor, not their parent, so do not judge—concentrate on the facts; 3) adolescents do not respect physician attempts to address them as a peer; and 4) adolescent patients are especially concerned about their privacy, and ensuring confidentiality is an important part of the earning patient trust. These concepts were illustrated using written information on the screen with narrative voice-over and video examples.
Table 1.
Modules in the Teen CHAT online educational intervention
| Welcome |
| Introduction |
| Why Teen CHAT? |
| Objectives |
| Why Counsel? |
| Introduction |
| Nutrition and Physical Activity Matter |
| Good counseling works |
| Motivational interviewing |
| Introduction |
| What is Motivational Interviewing? |
| Ask Open-Ended Questions |
| Practice Reflective Listening |
| Praise Positive Behaviors |
| Your Goals for Using MI |
| Behaviors to Avoid |
| Your Goals for Behaviors to Avoid |
| Summary |
| The 5 A’s |
| Explanation |
| An Example |
| Your Examples |
| Teen Communication |
| Introduction |
| Explanation |
| An Example |
| Summary |
| Take-Home Messages |
| What Other Doctors Are Doing |
| What Teens are Doing |
| Additional Resources |
The basic framework of the intervention was then reviewed by four primary care pediatricians who were otherwise not part of the study, nor members of any of the participating practices. These pediatricians provided reflections on the content and suggestions for revisions that were integrated into the final intervention.
One central and distinguishing feature of this intervention was that the program was tailored to each individual physician using audio clips from their baseline encounters along with other baseline data. Feedback regarding a provider’s own performance of certain skills has been shown to be a crucial element associated with provider’s improved use of those skills. (23) For each physician, we included up to 23 audio clips from the individual physicians’ recorded encounters with their own patients. These audio clips were used to illustrate both the positive behaviors we promoted and the behaviors we asked physicians to avoid and included examples of the physician using closed and/or open-ended questions, praise, reflective statements, and each component of the 5 A’s, among others.
To obtain these audio clips, first we coded the baseline encounters for the MI techniques using the Motivational Interviewing Treatment Integrity (MITI) Code (24) and 5 A’s with a codebook adapted from our other study with primary care physicians and overweight adult patients. (22) The MITI Code has been previously validated for convergent and discriminant validity. (25) Data generated from coding indicated the extent to which each physician exhibited each of the positive and negative behaviors during the recorded encounters. Specific instances of each behavior were marked in the audio recordings, with exemplar instances noted. These data, along with exemplar audio clips from the recordings were imported into the intervention program. We developed an algorithm to select content from a library of messages, thus tailoring communication feedback to each physician based on the frequency of each behavior. These messages and the matching exemplar audio clips were delivered to the providers along with standardized content in each section of the intervention. Two coders rated the audio clips with all reliabilities receiving moderate to near perfect agreement (Cohen’s Kappa range .66–1.0 for 5 As and .52–1.0 for MITI). Additionally, individually tailored graphs and tables were presented showing how the behavior of each provider and his/her patients compared to that of other physicians in the study.
Because the main limitation of formal MI training for physicians is time, the intervention was designed to take no more than 60 minutes to complete, although physicians could spend additional time by repeating sections or taking more time to consider and respond to interactive components. Participants were able to sign in at their convenience, and were able to complete the intervention in one sitting or over multiple sessions. After completion of the intervention, their access was maintained, allowing them to come back to the training as often as they liked.
2.2.3. Format
The program was hosted on a secure web server and was accessed by physicians through an ordinary web browser. The principal investigator (PI) emailed physicians asking when they would have a 3-week window in which they could view the intervention. She made a face-to-face appointment with each physician to introduce the intervention. Prior to the appointment, she emailed physicians the web address and a personalized sign-up code that physicians used to create a unique user name and password. During the appointment, the PI introduced the program but did not address physicians’ personal communication behaviors. She asked physicians to set a goal for when they would view the intervention and elicited barriers that might get in the way of reaching that goal. She used MI techniques to help motivate physicians to overcome barriers and view the program.
When physicians logged in, they were greeted with a welcome video from one of the investigators. A navigation system allowed physicians to move quickly between different sections, but the PI encouraged physicians to first complete the entire program from start to finish. A video vignette began the introduction section, and similar videos of doctor/teen interactions were used throughout the program. Table 2 (available online) is the script for the video about avoiding judging, and Table 3 (available online) is the script for the video illustrating the importance of asking permission.
Table 2.
Avoid judging
| Physician and teenage boy are in an exam room |
| Physician: Last visit we talked about improving your food choices. So, let’s talk about that some more. What did you have for lunch yesterday? |
| Teen Patient: French fries and, um, ice cream. |
| Physician: Are you serious? French fries and ice cream? What were you thinking? |
| Video cuts to patient alone: |
| Patient (direct to camera): The doctor sounds just like my parents. He asked a question. I answered it. Next time, I’ll just keep my mouth shut. |
| Video cuts back to physician and teenage boy are in an exam room |
| Physician: Last visit we talked about improving your food choices. So, let’s talk about that some more. What did you have for lunch yesterday? |
| Patient: French fries and, um, ice cream. |
| Physician: Hmmm. French fries and ice cream. |
| Patient: Okay, I know that’s not so good for me. But I just didn’t like the other stuff on the menu. |
| Physician: I hear you. It can be hard finding decent food at a cafeteria. If you want to eat healthier and still enjoy your lunch, what do you think you can do? |
| Patient: Well, I guess I could look at the menu a day ahead and plan a little better. Or, I could bring my lunch sometimes. |
| Physician: I think that’s great. |
| Video cuts to physician alone: |
| Physician (direct to camera): When I responded without judgment, empathized with my patient’s situation, and listened, I got what I needed – a conversation and input from my patient. |
Table 3.
Ask permission
| Physician and teenage girl are in an exam room |
| Physician: I’ve been looking at your chart and I noticed that your weight’s creeping up. What do you think about that? |
| Patient: Yeah. I guess I could do something about it. |
| Physician: Why don’t you try swimming? Many of my patients like that. |
| Patient: Yeah, ok. |
| Video cuts to patient alone |
| Patient (direct to camera): Swimming? I don’t even know how to swim! Get real! |
| Video cuts back to physician and teenage girl in the exam room |
| Physician: I’ve been looking at your growth chart here and I noticed that your weight’s been creeping up. What do you think about that? |
| Patient: Yeah. I guess I could do something about it. |
| Physician: What sorts of things might you try? |
| Patient: I don’t know. I haven’t thought much about it. |
| Physician: I have some ideas that have helped other patients. Would it be okay if I shared them with you? |
| Patient: Sure. Now that I think about it, I am on the computer a lot. Pretty much from when I get home ‘til I go to sleep. And I know that’s not so great. |
| Physician: You spend a lot of time in front of the computer. |
| Video cuts to physician alone |
| Physician (direct to camera): Asking permission to share ideas and get feedback about them really helped me to zero in on what might and might not work. And, it got her involved in problem solving. I want my patients to be active participants, not just people doing something because I told them to. |
At the end of each section of the program, physicians were asked to set goals. In the MI section, physicians were asked to choose between focusing on open-ended questions, reflective listening, or praise. At the end of the Behaviors to Avoid section, physicians were asked to choose an unhelpful habit to avoid in upcoming patient encounters: giving unsolicited advice, expressing disapproval, or confronting. At the end of the 5 A’s section, physicians were asked to write in their own words how they might use each of the 5 A’s that they were not already consistently using (as indicated by their baseline data).
Interactive exercises gave physicians the opportunity to type in communication ideas. For example, physicians were presented a closed-ended question “Did you stop drinking soda for breakfast, like we talked about?” and were then asked to rewrite it as an open-ended question and enter this into a text box. At the end of the program, take-home messages were summarized; Figure 2 is a screen shot of these take home messages. Each physician’s performance was also summarized and presented graphically in relation to the other physicians. Figure 3 (available online) shows a screen shot illustrating the percentage of questions asked that were open ended both by the individual physician and others in the study. After completion of the online program, physicians were sent automated emails weekly for four weeks to remind them of the goals they had set.
Figure 2.
Screen shot of educational module summary
Figure 3.
Screen shot summary of use of open-ended questions
3 Results
3.1 Characteristics of participating physicians
Forty-six physicians were recruited from seven primary care pediatrics practices and four family medicine practices. Twenty-two physicians were randomized to view the intervention website and 24 to the control group. The average age of the physicians was 39 years, and 63% were female.
3.2 Use of online modules
The 22 physicians in the intervention arm were notified via an email that included their personal sign-on code, instructions for use of the website, and a hypertext link to the site. Fifteen of the physicians viewed the program within in the first 1–2 days after they were sent the link to the site, and most physicians had signed on to the site within 1 week. Ten physicians completed the module in one sitting and did not login again, whereas one physician logged in 4 different times before completing the module. Time utilization was available for 19 of the 22 physicians. The educational module took an average of 54 minutes to complete, with a range of 31 minutes to 115 minutes. All physicians viewed the pages that included their personalized audio clips.
3.3 Feedback regarding online modules
After viewing the website, all physicians received follow up emails from and met with the PI (KP) to review the content and to review any website issues or questions about using the website that physicians may have had. Positive comments included “I have had the opportunity to use the technique on at least 3 teens and have also started using on adults as well. It has been well-received and has facilitated good discussion.” “I have had one teen who was quite surprised that I was asking for permission to give advice!” “Implementing the goal and practicing it in multiple setting is helping it to be a more natural part of the discussion.” One physician did note that “the time crunch of getting it all done looms over my head, and I dare say I neglect to use these skills but (am) continuing to try.”
Physicians also completed a 67-item survey regarding their own perceived counseling skills and the usefulness of various components of the intervention. Written survey data were available for all 22 physicians in the intervention group. Responses were ranked on a 5 point Likert scales: “not helpful at all”, “a little helpful”, “somewhat helpful”, “fairly helpful”, and “very helpful.” All 22 remembered receiving email reminders, and 77% found these emails to be somewhat, fairly, or very helpful. As shown in Table 4, many of the physicians found the website to be fairly or very helpful in learning how to ask open-ended rather than closed-ended questions, and to use reflections rather than questions. Fewer physicians found the website useful in learning to communicate confidentiality to adolescents. 43% of physicians thought that the website would impact their communication effectiveness “a good amount” or “a great deal” and would assist with challenging conversations. 62% indicated that they were likely to increase the use of the skills presented on the website. 67% thought that the website was worth their time, and 76% were likely to recommend the web site to a colleague. Physicians were also asked to list the most useful aspects of the website, and examples included “helping to give direction on open ended questions”, “patient scenarios, hearing my own examples”, “very helpful to hear myself say certain things”, “ideas on how to use reflection” and “seeing different strategies for communicating”. When asked how they would improve the website, suggestions included “more interactive, more recorded examples”, “make the online training more concise”, “too basic”, and “make useable on tablet or iPad—some things didn’t transfer.”
Table 4.
How helpful did you find the website in…
| % answering “fairly helpful or “very helpful” | |
|---|---|
| Understanding the importance of counseling about nutrition and physical activity | 67 |
| Learning how to ask open ended rather than closed ended questions | 81 |
| Learning how to use reflections instead of questions | 81 |
| Learning how to praise | 76 |
| Learning to avoid giving advice without permission | 71 |
| Learning to avoid showing disapproval | 57 |
| Learning to avoid confronting patients when the disagree | 48 |
| Learning to “ask” patients what they think about their weight | 76 |
| Learning to “advise” patients to attain a healthy weight | 62 |
| Learning to “assess” patients’ willingness to work on their weight | 67 |
| Learning how to “assist” patients in making weight-related changes | 57 |
| Learning to “arrange” a follow up visit to discuss weight | 67 |
| Learning how to ask parents to leave the room and allow you to talk to the adolescent in private | 33 |
| Learning to communicate confidentiality to adolescents | 38 |
4 Discussion and Conclusion
4.1 Discussion
The Teen CHAT intervention is a theory-driven model for physician education applied in a multi-media, personalized, and interactive format used to enhance doctor-patient communication regarding nutrition and physical activity with overweight and obese adolescents seen for preventive health visits. Although many physicians acknowledge the need for effective office-based counseling for child and adolescent obesity, and many are eager to improve their communication skills, intensive MI training remains impractical for many primary care providers. The Teen CHAT program offers many advantages. Compared to a traditional workshop or mentored training, it requires a less time commitment by the provider, is easily accessed by providers regardless of their geographical location, can be delivered to a large number of providers with cost efficiency, and can be delivered with fidelity and without the need for skilled facilitators who are in short supply. Compared to other web-based trainings, it offers individually tailored feedback built around providers’ own real-world encounters. Although this tailored feedback offers many potential advantages, it does make large-scale dissemination more difficult but remains easier than face-to-face training, which, though effective, is expensive and time-consuming for both trainer and trainee. The use of training sessions that include personalized audio clips may be a useful way for physicians to pursue periodic reflective learning, allowing them to build on their developing MI skills. As we continue to collect data on utilization, it may be that certain themes and similar statements from physicians become apparent, and future versions of the intervention may include content selected from a library that match individual physicians’ self-identified educational goals.
Use of and satisfaction with the Teen CHAT program provides the base for evaluation of clinical effectiveness. Previous studies of computerized medical education interventions have shown widely varying utilization rates, ranging from 29% of pediatric emergency department physicians (26) to 87% of medical students. (27) However, because most web-based educational programs are accessible to the general population, the potential “eligible population” is usually unknown, making accurate calculation of utilization rates impossible.
As more computerized medical education becomes available, it has become apparent that not all educational programs are created equal. While almost all programs contain some text, fewer include audio or video, and most that do include these media elements simply present “talking heads” explaining the content that the physician could just as easily read. Fewer still include interactive components. (28) The participants in the Teen CHAT program endorsed the use of the video vignettes and the interactive components, emphasizing the need for such educational interventions to be more than online textbooks, as well as the value that the video case vignettes provide in demonstrating the real-world use of the communication skills covered in other sections.
In general, physicians were satisfied with Teen CHAT, and found it particularly helpful in a number of areas, most prominently regarding the use of open-ended rather than closed-ended questions, and using reflective statements. This is encouraging, given that these are key components of patient-centered interviewing, a concept that has been linked with improved health outcomes, improved patient satisfaction, and improved physician satisfaction. (29) Some participants were concerned about the time that using the MI techniques described in our educational intervention, however, there is little evidence that using open-ended questions and reflective listening skills takes more time, and it is likely that utilizing these MI skills will in fact save time overall. (30)
4.2 Conclusion
Given the importance of physician counseling, effective interventions are needed that can be easily disseminated and implemented to busy practicing physicians. Teen CHAT shows promise for improving physician communication and had high penetration. The Teen CHAT online educational intervention shows potential for enhancing physician MI skills in an acceptable and time-efficient manner.
4.3 Practice Implications
If shown to be effective, the Teen CHAT program can be widely disseminated to practicing physicians who want to improve their office-based counseling skills with adolescent patients.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity. Rockville, MD: Public Health Service, Office of the Surgeon General; 2001. [PubMed] [Google Scholar]
- 2.Koplan JP, Liverman CT, Kraak VI. Preventing Childhood Obesity: Health in the Balance. Washington, DC: Institute of Medicine of the National Academies; 2005. [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 4.Luttikhuis HO, Baur L, Jansen H, Shrewsbury VA, O’Malley C, Stolk RP, et al. Interventions for treating obesity in children: Cochrane Databse of Systematic Reviews. 2009. [DOI] [PubMed] [Google Scholar]
- 5.Wang LY, Denniston M, Lee S, Galuska D, Lowry R. Long-term health and economic impact of preventing and reducing overweight and obesity in adolscence. Journal of Adolescent Health. 2010;46(5):467–73. doi: 10.1016/j.jadohealth.2009.11.204. [DOI] [PubMed] [Google Scholar]
- 6.Broder KR, Cohn AC, Schwartz B, Klein JD, Fisher MM, Fishbein DB, et al. Adolescent Immunizations and Other Clinical Preventive Services: A Needle and a Hook? Pediatrics. 2008;121(Supplement 1):S25–S34. doi: 10.1542/peds.2007-1115D. [DOI] [PubMed] [Google Scholar]
- 7.Barlow SE Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: a summary report. Pediatrics. 2007;120(Suppl):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 8.Erickson SJ, Gerstle M, Feldstein SW. Brief interventions and motivational interviewing with children, adolescents, and their parents in pediatric health care settings. Archives of Pediatrics & Adolescent Medicine. 2005;159:1173–80. doi: 10.1001/archpedi.159.12.1173. [DOI] [PubMed] [Google Scholar]
- 9.Pollak KI, Alexander SC, Ostbye T, Luna P, Tulsky JA, Dolor RJ, et al. Primary care physicians’ discussions of weight-related topics with overweight and obese adolescents: results from the Teen CHAT pilot study. Journal of Adolescent Health. 2009;45(2):205–7. doi: 10.1016/j.jadohealth.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emmons KM, Rollnick S. Motivational interviewing in health care settings: opportunities and limitations. American Journal of Preventive Medicine. 2001;20(1):68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 11.Pollak KI, Alexander SC, Coffman C, Tulsky JA, Luna P, Dolor RJ, et al. Physician communication techniques and weight loss in adults: Project CHAT. American Journal of Preventive Medicine. 2010;39(4):321–8. doi: 10.1016/j.amepre.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwartz P, Hamre R, Dietz W, Wasserman R, Slora E, Myers E, et al. Office-based motivational interviewing to prevent childhood obesity. Arch Pediatr Adolesc Med. 2007;161:495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 13.Rubak S, Sandbaek A, Lauritzen T, Borch-Johnsen K, Christensen B. An education and training course in motivational interviewing influence: GPs’ professional behaviour--ADDITION Denmark. British Journal of General Practice. 2006 Jun;56(527):429–36. [PMC free article] [PubMed] [Google Scholar]
- 14.Doherty Y, Hall D, James PT, Roberts SH, Simpson J. Change counselling in diabetes: the development of a training programme for the diabetes team. Patient Education & Counseling. 2000 Jun;40(3):263–78. doi: 10.1016/s0738-3991(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 15.Patrick K, Sallis JF, Prochaska JJ, Lydston DD, Calfas KJ, Zabinski MF, et al. A multicomponent program for nutrition and physical activity change in primary care: PACE+ for adolescents. Archives of Pediatrics & Adolescent Medicine. 2001 Aug;155(8):940–6. doi: 10.1001/archpedi.155.8.940. [DOI] [PubMed] [Google Scholar]
- 16.Schermer CR, Moyers TB, Miller WR, Bloomfield LA. Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. Journal of Trauma-Injury Infection & Critical Care. 2006 Jan;60(1):29–34. doi: 10.1097/01.ta.0000199420.12322.5d. [DOI] [PubMed] [Google Scholar]
- 17.CSS, Pollak KI, Farrell D, Olsen MK, Jeffreys AS, Tulsky JA. Use of and reactions to a tailored CD-ROM designed to enhance oncologist-patient communication: The SCOPE trial intervention. Patient Education and Counseling. 2009;77:90–6. doi: 10.1016/j.pec.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tulsky JA, Arnold RM, Alexander SC, Olsen MK, Jeffreys AS, Rodriguez KL, et al. Enhancing communication between oncologists and patients with a computer-based training program: a randomized trial. Annals of Internal Medicine. 2011;155(9):593–601. doi: 10.1059/0003-4819-155-9-201111010-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bandura A. Social foundations of thought and action: A social cognition theory. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1986. [Google Scholar]
- 20.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 21.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. American Journal of Preventive Medicine. 2002;22(4):267–84. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 22.Alexander SC, Cox ME, Boling Turer CL, Lyna P, Ostbye TA, Dolor RJ, et al. Do the five A’s work when physicians counsel about weight loss? Family Medicine. 2011;43(3):179–84. [PMC free article] [PubMed] [Google Scholar]
- 23.Andrews JO, Tingen MS, Waller JL, Harper RJ. Provider feedback improves adherence with AHCPR smoking cessaiont guidelines. Preventive Medicine. 2001;33(5):415–21. doi: 10.1006/pmed.2001.0907. [DOI] [PubMed] [Google Scholar]
- 24.Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28(1):19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 25.Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat. 2005;28(1):19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 26.Pusic MV. Pediatric residents: are they ready to use computer-aided instruction? Archives of Pediatrics & Adolescent Medicine. 1998;152(54):494–8. doi: 10.1001/archpedi.152.5.494. [DOI] [PubMed] [Google Scholar]
- 27.Schultze-Mosgau S, Zielinski T, Lochner J. Web-based, virtual course units as a didactic concept for medical teacing. Medical Teacher. 2004;26(4):336–42. doi: 10.1080/01421590410001679028. [DOI] [PubMed] [Google Scholar]
- 28.Cook DA, Garside S, Levinson AJ, Dupras DM, Montori VM. What do we mean by web-based learning? A systematic review of the variability of interventions. Medical Education. 2010;44(8):765–74. doi: 10.1111/j.1365-2923.2010.03723.x. [DOI] [PubMed] [Google Scholar]
- 29.Lyles JS, FCS, Lein C, Smith RC. Evidence-based patient-centered interviewing. Journal of Clinical Outcomes Management. 2001;8(7):28–34. [Google Scholar]
- 30.Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. Journal of General Internal Medicine. 1999;14:S34–S40. doi: 10.1046/j.1525-1497.1999.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]