Abstract
Paraduodenal hernia is an uncommon cause of acute abdominal pain; however, it is the commonest of internal herniation. Computer tomography of the abdomen is diagnostic. Although it is a rare cause of intestinal obstruction, it is estimated that more than half of paraduodenal hernias develop symptoms. We present a case of left paraduodenal hernia that presented with acute abdominal pain and a left upper abdominal mass. Symptoms resolved spontaneously and a planned Laparoscopic repair was performed. The malpositioned small intestine was reduced from the hernia sac and the hernial orifice was closed. The patient made a rapid recovery with no recurrence of symptoms at 3-year follow-up.
INTRODUCTION
Paraduodenal hernia is a rare congenital abnormality caused by a malrotation of the midgut; it is the commonest type of internal herniation (53%). Left-sided paraduodenal hernia is more common than right side (75%:25%). It is an uncommon cause of intestinal obstruction (0.2–0.9%). Pre-operative CT scan of the abdomen is usually diagnostic; however, the diagnosis is often made intra-operatively [1].
We present a case of planned laparoscopic repair of a left-sided paraduodenal hernia presenting with abdominal symptoms that initially resolved spontaneously.
CASE REPORT
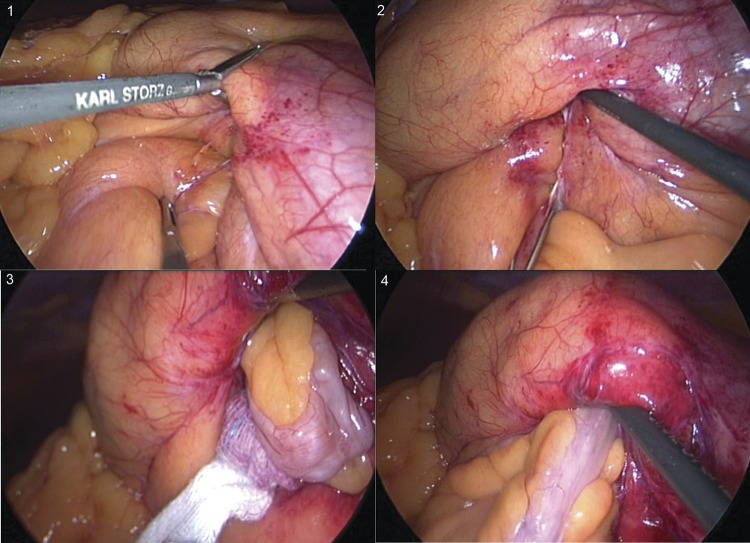
A 35-year-old male presented to accident and emergency with left upper abdominal pain, nausea and loss of appetite for 3 days. On retrospective questioning, he admitted to a propensity to vomit occasionally after large meals dating back to his childhood. On examination his abdomen was mildly distended with tenderness and a mass in his left upper quadrant. Chest and abdominal X-ray were normal. CT scan of the abdomen and pelvis with oral and i.v. contrast showed a left paraduodenal hernia (Fig. 1). Within 24 h his symptoms had resolved spontaneously and he was able to eat freely without pain and was discharged. He had mild left upper quadrant pain on a few occasions over the next 2 weeks and the option of surgical repair was discussed. As 50% or more paraduodenal hernias develop partial or complete small intestinal obstruction, surgical treatment was recommended. The patient decided to proceed to surgical treatment and a minimal access approach was planned.
Figure 1:
CT scan of the abdomen demonstrating left paraduodenal hernia.
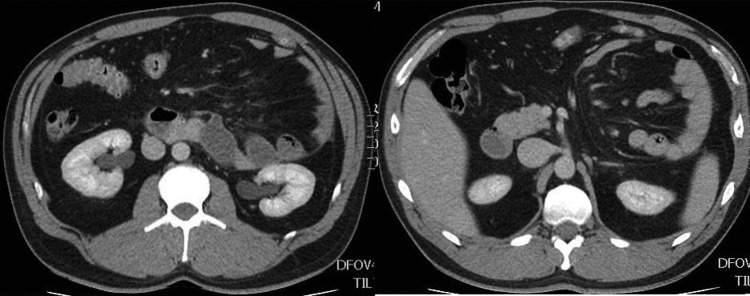
Hasson's insufflations technique was used for an initial infra-umbilical port insertion. Two further operating ports were place in the right lower quadrant under direct vision. Laparoscopy confirmed the radiological findings; the majority of the small intestine was found to lie inside the paraduodenal hernial sac. The sac lay behind the mesentery of the descending colon extending cranially behind the transverse colon and splenic flexure and lesser sac in front of the structures of the left retro-peritoneum. The neck of the hernia neck was formed anteriorly by free edge of descending colonic mesentery containing inferior mesenteric vein and posteriorly by retro-peritoneum. The neck lay to the left and caudal to the duodeno-jejunal junction with the ligament of Treitz fusing with the superior boarder. The proximal Jejunum directly distal to the DJ flexure entered the sac, the terminal ileum was identified within the abdomen, the caecum lay in the right iliac fossa, the remainder of the small intestine was within the hernia (Fig. 2 1 and 2). There were peritoneal adhesions at the neck of the hernia to the viscera entering the sac which prevented spontaneous reduction. Operative reduction of the hernia commenced with sharp dissection of these adhesions, followed by sharp and blunt dissection, the neck of the sac was cleared and mobilized. Once this procedure was complete the small intestine was easily reduced to the abdominal cavity, occasional adhesions to the hernial sac were divided to complete this process (Fig. 2 3 and 4). The hernial neck was closed with a continuous suture opposing the peritoneum of the free boarder of the descending colonic mesentery to the peritoneum below the D-J flexure to the left of the aorta. Post-operative recovery was uncomplicated and discharge was within 23 h. The patient made good recovery and to date has had no recurrence of symptoms over 3 years of follow-up.
Figure 2:
(1–4) Identification and laparoscopic reduction of paraduodenal hernia in the sequence.
DISCUSSION
Paraduodenal hernia is a rare congenital abnormality caused by an error of rotation of the midgut and/or failure of the ascending colonic mesentery to fuse to the parietal peritoneum. Commonly, it will cause few symptoms and be identified incidentally; it may, however, present with small intestinal obstruction, strangulation or perforation. Paraduodenal hernia can be left- or right-sided depending on the relationship of mesenteric vessels of small intestine. Left-sided paraduodenal hernia is more common than right and the prevalence is slightly higher in males [2, 3].
Right-sided paraduodenal hernia is a result of midgut malrotation and failure of fusion of mesentery to parietal peritoneum creating hernial defect. The development of left paraduodenal hernia occurs when midgut rotates, initially behind and then left to the superior mesenteric artery and comes to lie in the left side of the abdomen behind the mesentery of the descending colon. In a left paraduodenal hernia, the peritoneal defect lies to the left of the fourth part of the duodenum (Fossa of Landzert) and the anterior border of the hernial orifice is formed by the inferior mesenteric vein [3, 4].
The majority of historical reports was from post-mortem examinations or incidental findings at laparotomy. With the advent of abdominal imaging, the condition can be recognized and the anatomy evaluated and it is the investigation of choice for this condition.
Minimally, invasive surgery for this condition potentially results in reduced post-operative pain, reduced hospital stay and early return to normal activity. This case was admitted on the day of the operation and was discharged at 23 h. He returned to normal activity at a week and has been symptom free for 3 years. Had he presented acutely with bowel obstruction or strangulation, an open approach would have been considered, similarly if he had remained symptom free, no surgical intervention would have been required. There is no evidence to suggest fewer adhesions lead to further recurrence through a laparoscopic approach as the defect is closed intra-operatively with sutures and the aetiology differs in that it is not affected by intra-abdominal pressure.
Laparoscopic paraduodenal hernia repair is a relatively new technique. The first laparoscopic repair of paraduodenal hernia was reported in 1998 by Uematsu et al. [5]. It is recommended for uncomplicated cases (no suspicion of strangulation or perforation). We would recommend a similar approach for other internal hernias including post-surgical, transmesenteric and foramen of Winslow hernias—if the patient presents with an acute complication we would adopt an open approach, if the symptoms resolve but recur a planned minimal access approach would be favoured.
AUTHORS’ CONTRIBUTIONS
A.S.: preparation of manuscript and management of case; A.C.: revision of manuscript; T.P.: management of case and revision of manuscript.
REFERENCES
- 1.Dayananda L, Sreekumar KP, Moorthy S, Prabhu NK. Paraduodenal hernias: a pictorial essay. Ind J Radiol Imag. 2006;16:469–71. doi:10.4103/0971-3026.32248. [Google Scholar]
- 2.Yun MY, Choi YM, Choi SK, Kim SJ, Ahn SI, Kim KR. Left paraduodenal hernia presenting with atypical symptoms. Yonsei Med J. 2010;51:787–9. doi: 10.3349/ymj.2010.51.5.787. doi:10.3349/ymj.2010.51.5.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartlett MK, Wang C, Williams WH. The surgical management of paraduodenal hernia. Ann Surg. 1968;168:249–54. doi: 10.1097/00000658-196808000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callander LC, Rusk GY, Nemir A. Mechanisms, symptoms and treatment of hernia into the descending mesocolon: left duodenal hernia. Surg Gynecol Obstet. 1935;60:1052–71. [Google Scholar]
- 5.Uematsu T, Kitamura H, Iwase M, Yamashita K, Ogura H, Nakamuka T, et al. Laparoscopic repair of a paraduodenal hernia. Surg Endosc. 1998;12:50–2. doi: 10.1007/s004649900591. doi:10.1007/s004649900591. [DOI] [PubMed] [Google Scholar]