Abstract
Objective:
To search the English-language literature for original research addressing the effect of cryotherapy on return to participation after injury.
Data Sources:
We searched MEDLINE, the Physiotherapy Evidence Database, SPORT Discus, the Cochrane Reviews database, and CINAHL from 1976 to 2003 to identify randomized clinical trials of cryotherapy. Key words used were cryotherapy, return to participation, cold treatment, ice, injury, sport, edema, and pain.
Data Synthesis:
Original research, including outcomes-assessment measures of return to participation of injured subjects, was reviewed using the Physiotherapy Evidence Database (PEDro) Scale. Four studies were identified and reviewed by a panel of certified athletic trainers. The 4 articles' scores ranged from 2 to 4 on the PEDro scale, which has a maximum of 10 points. Two of the articles suggested that cryotherapy speeds return to participation after ankle sprains. However, these authors failed to provide in-depth statistical analysis of their results. A confounding factor of compression as part of the treatment prevented interpretation of the effects of cryotherapy in 1 article.
Conclusions:
After critically reviewing the literature for the effect of cryotherapy on return-to-participation measures, we conclude that cryotherapy may have a positive effect. Despite the extensive use of cryotherapy in the management of acute injury, few authors have actually examined the effect of cryotherapy alone on return-to-participation measures. The relatively poor quality of the studies reviewed is of concern. Randomized, controlled clinical studies of the effect of cryotherapy on acute injury and return to participation are needed to better elucidate the treatment responses.
Keywords: modalities, cold treatment, outcomes assessment, evidence-based practice
One goal of all certified athletic trainers is to return athletes to play as quickly and safely as possible after injury. To facilitate this goal, numerous rehabilitation techniques pertaining to the treatment of athletic injuries have been studied. These studies typically focus on the effect of a particular modality or treatment on a particular aspect of the rehabilitative process.1–3 Examples include range of motion, strength, and balance measurements. Increasingly, the effects of therapeutic interventions are being assessed through functional and self-report outcomes measures.4,5 Investigators are starting to address such questions as whether individuals treated with a particular modality or medication return to work or sport more rapidly, have a lower incidence of reinjury, or achieve a desired outcome at a lower cost.4,5 Certified athletic trainers have developed practice guidelines in the form of National Athletic Trainers' Association position statements on lightning, fluid replacement, and heat illness.6 These have offered an excellent starting point; however, to date, no guidelines have addressed the efficacy of assessment, treatment, and rehabilitation techniques. The continued development of the profession and the need for better patient care require that all aspects of clinical practice, including prevention, assessment, treatment, and rehabilitation, be examined and critically appraised.
The need for better patient care has lead to evidence-based medical practice.7 Evidence-based practice (EBP) is the integration of the best research evidence with clinical expertise and patient values.7 It combines practitioners' clinical expertise at treating a condition with research of the literature on the treatments of a certain condition. The focus is on patient values or on the outcomes of patients treated with a certain modality or rehabilitative technique.
Evidence-based practice starts with a question regarding a patient problem—for example, “Is iontophoresis effective in the treatment of lateral epicondylalgia?” Clinicians can then use past experiences with iontophoresis and begin to search and critically appraise the literature. Once the articles are appraised and reviewed, conclusions based on the effectiveness of the treatment can be drawn. The knowledge gained from these sources must be applied to the patient problem.8 Evidence-based practice is a constantly changing process; new research is continually conducted, and different results may be reported. The evidence for the effect of iontophoresis in the treatment of lateral epicondylalgia may change as new research is published. In addition, reviewing the literature may not answer all questions. Depending upon the evidence, such a review may lead to more questions than answers, which can be a starting point for future research to examine outcomes and develop an EBP guideline. As new research is conducted, EBP guidelines must be updated and revised.
Cryotherapy is one of the most commonly applied treatments in the management of acute, athletic-related musculoskeletal injuries. Even though cryotherapy is typically applied clinically along with elevation and compression, we felt it was important to determine the effect of cryotherapy in isolation without any confounding variables. This way, the true effect of cryotherapy could be determined. Numerous studies have been conducted examining the effect of cryotherapy on tissue temperature,1,2,9–15 blood flow,1–3,9,16–20 pain,1,2,9,21–24 and swelling.1,2,9,25–29 Although it is important to determine the effect of cryotherapy on various physiologic responses, the bigger question is, “What is the effect of cryotherapy on treatment outcome?” Does treatment with cryotherapy affect return to participation? Does speed of return to participation affect reinjury rate? Is cryotherapy cost effective? When treatment benefits are identified, the mechanisms responsible can be further explored. Our purpose was to search the English-language literature for original research addressing the effect of cryotherapy on return to participation after injury.
DATA SOURCES
A search of the English-language literature was performed using MEDLINE, the Physiotherapy Evidence Database, SPORT Discus, the Cochrane Reviews database, and CINAHL from 1976 to 2003 for literature related to cryotherapy application. Key words used were cryotherapy, return to participation, cold treatment, ice, injury, sport, edema, and pain.
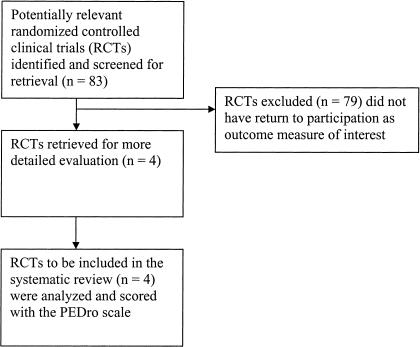
Research specific to treatment outcomes after cryotherapy were identified. All randomized, controlled clinical trials assessing the effect of cryotherapy were initially examined. (Figure). All articles were read and the outcomes measures for each article were recorded. The references of identified articles were examined to identify additional articles that may have been missed during the original search. The majority of researchers examined the effect of cryotherapy on the following outcomes measures: tissue temperature,11–15 blood volume,16–19 swelling,25–29 pain,22–24 functional performance,1,2 and postoperative measures.1,2 These articles were retained for review and referenced as appropriate in the discussion section. However, these articles were not used as part of the analysis, because they did not examine return to participation. We were specifically searching for articles that examined the effect of cryotherapy on return to participation. Return to participation was defined as return to sport participation (athletes) or return to work (typical population) for this study. Articles by authors who had examined the effect of cryotherapy on return to participation were retained for further review.
Criteria for selection of articles for review.30
Physiotherapy Evidence Database Scale
Once we identified the 4 articles, we used the Physiotherapy Evidence Database (PEDro) scale to rate the articles. The PEDro Scale is an evaluation instrument developed for the Physiotherapy Evidence Database by the Centre for Evidence- Based Physiotherapy.31 The database provides access to controlled clinical trials and systematic reviews in physiotherapy. The trials in the database are rated to help users identify studies of highest methodologic quality. The PEDro scale is a checklist that examines the “believability” (internal validity) and the “interpretability” of trial quality. The Scale “grades” the believability of a research report by considering aspects of study design, such as random allocation; concealment of allocation; comparability of groups at baseline; blinding of patients, therapists, and assessors; analysis by intention to treat; and adequacy of follow-up. The Scale measures the interpretability of the trials by examining between-group statistical comparisons and descriptions of both point estimates and measures of variability. The 11-item checklist (Table 1) yields a maximum score of 10 points if all criteria are satisfied. (No points are awarded for the first criterion.)
Table 1.
PEDro* Scale31
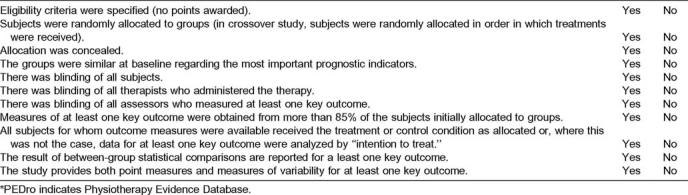
We chose the PEDro Scale because it has tested reliability data and was specifically developed for physiotherapy studies. Maher et al32 investigated the reliability of the 11 items of the PEDro Scale as well as the total score. Raters were volunteer physical therapists who had been trained in the use of the Scale. The reliability estimates of the PEDro Scale (intraclass correlation coefficient = .56 for total score for individual ratings and .68 for panel ratings) are similar to those reported for 3 other commonly used quality scales (Chalmers Scale, Jadad Scale, and Maastricht List).32 The panel ratings tend to be more reliable than the individual ratings. When using the PEDro Scale, it would be more beneficial to have a panel of reviewers than to rely on the judgment of one individual.32 However, a panel of reviewers is not part of the PEDro Scale guidelines.
We independently evaluated the 4 randomized, controlled trials that met the criteria of return-to-participation measures using the PEDro Scale. All 3 certified athletic trainers read the 4 articles separately and assessed them for each of the 11 criteria specified by the PEDro Scale. Scores were recorded, and then we met to review the scores. Full consensus was achieved over the scores given to the 4 articles.
DATA SYNTHESIS
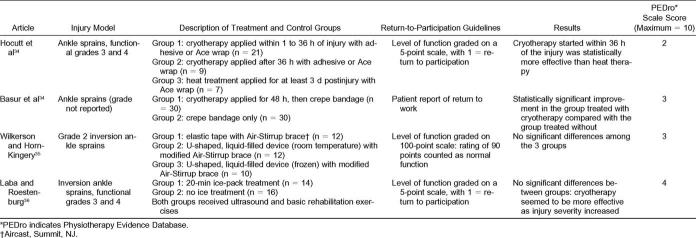
Scores on the PEDro Scale ranged from 2 to 4 of a maximum 10 points (Table 2). Authors of two of the 4 articles33,34 reported patients returned to play or full function faster with immediate cryotherapy when compared with late cryotherapy or no cryotherapy. The third set of authors35 also reported quicker return to participation; however, they attributed this result to the application of external compression rather than cryotherapy. The fourth set36 reported no statistical differences in return to participation, but a closer look at the data demonstrated that the greater the severity of ankle sprain, the better the effect of cryotherapy on return to participation.
Table 2.
Reviewed Articles
Hocutt el al33 compared the effects of cryotherapy applied immediately after injury, 1 to 36 hours after injury, and 48 hours after injury and thermotherapy in the treatment of ankle sprains. Grade of ankle injury was based on level of function at the start of the study. Grades ranged from 1 (functional) to 5 (requiring surgery). All participants in the study were classified as having grade 3 or 4 ankle function. When a subject reached grade 1, we considered that returning to participation. The study reported that cryotherapy started within 36 hours after the injury was statistically more effective than heat therapy.
This article scored 2/10 on the PEDro Scale. The eligibility criteria were specified by including subjects with grade 3 and 4 ankle sprains and excluding those with fractures. The groups were similar at baseline with regard to the most important prognostic indicators (degree of ankle sprain). All subjects received some form of treatment, even though there was no true control group. This article was awarded 1 point for having the intention to treat all subjects. An intention-to-treat analysis means that, when subjects did not receive treatment as allocated (or were part of the control condition) and when measures of outcome were available, the analysis was performed as if subjects received the treatment or control condition allocated to them.31
Basur et al34 compared crepe-bandaging treatment with treatment with cryotherapy and crepe bandaging for 48 hours postinjury. Subjects were given a severity-of-ankle-injury score (0 to 6) based on their signs and symptoms when they visited the emergency room. They were assigned to treatment with cryotherapy, crepe bandaging, and a layer of tubular compression bandage or to a control group treated with the crepe bandaging only. Although a significant difference between groups was reported, the results of the specific statistical analyses were not provided. Of the subjects treated with cryotherapy, 42.1% recovered by the second day and 84.2% by the 7th day of follow-up. In the control group, recovery rates were 29.1% and 60.6%, respectively.34
This paper was graded 3/10 on the PEDro Scale. The investigators measured at least 1 key outcome from more than 85% of the subjects initially allocated to the groups. Thus, of the subjects initially enrolled in the study, 85% received treatment, and the dependent variable of interest (return to participation) was measured. All 60 subjects initially placed in the treatment group received treatment. Inclusion criteria based on this point system were not specified. Full function was defined as the number of days to return to work.
Wilkerson and Horn-Kingery35 examined the treatment of grade II inversion ankle sprains with different modes of compression and cryotherapy. Subjects were randomly assigned to 1 of 3 treatment groups, which differed based on the type of compression they received. The authors assessed ankle function with an 11-item, 100-point scale.35 A score of 100 points was considered “full functional capacity,” which we equate with return to participation. The reliability of the scale is not currently known. We felt that this was a good objective method for determining ankle level of function and should be examined in future research studies. Wilkerson and Horn-Kingery35 reported no significant differences among the groups. The lack of significant between-group differences may be attributable to low statistical power (1 − β = .58).35
This paper scored 3/10 on the PEDro Scale. The authors specified the eligibility criteria, measured at least 1 key outcome (return to participation) in more than 85% of the subjects initially allocated to the groups, reported the results of between-group variability, and provided point estimates and associated variability. Ten of the 34 subjects were unavailable at some point during data collection, so measurements were not available for all subjects at all time points.
Laba and Roestenburg36 examined the effect of cryotherapy on return to participation in a group treated with cryotherapy and a group treated with no cryotherapy. Ankle grading was based on a level-of-function scale similar to that used by Hocutt et al.33 All subjects in the study were classified as grade 3 or 4 ankle function level. For subjects who were classified as having a grade 4 injury and treated with cryotherapy, time to recovery averaged 7.3 days, versus those treated without cryotherapy, whose recovery time averaged 10.2 days. However, subjects with less severe injuries (grade 3) treated with cryotherapy averaged 4.6 days to recovery, whereas those treated without cryotherapy recovered in 3.0 days.36 It may be that severity of injury plays a role in the effect of cryotherapy. Yet, there were no statistical differences in the level of pain, amount of swelling, or speed of return to participation in those treated with or without cryotherapy.36
This article had the highest score (4/10) of all the articles reviewed on the PEDro Scale. Subjects were randomly allocated to the 2 groups, and the authors provided baseline comparability for all subjects, adequate follow-up, and measures of variability (standard deviations).
DISCUSSION
Our review of the 4 randomized, controlled clinical trials suggests that cryotherapy may be effective in reducing the time to return to participation; however, the extremely low quality of the studies reviewed is of concern. Despite the extensive use of cryotherapy in the management of acute musculoskeletal injury, few investigators33–36 have actually examined the effect of cryotherapy alone on return to participation. The results of 233,34 of the 4 papers reviewed suggest that cryotherapy instituted soon after injury may be effective in speeding return to work or sport activity. One of the potential limitations of this systematic review is the fact that only 4 articles were reviewed. However, our initial purpose was to examine the effect of cryotherapy on return to participation. Numerous studies have been conducted examining the effect of cryotherapy on various outcomes measures, such as pain, swelling, and functional activities. We felt it was necessary to examine return to participation. The small number of articles reviewed is evidence of how little research is available that examines the effect of cryotherapy on return to participation.
The major flaw with the study by Hocutt el al33 is the lack of detail in reporting the statistical analysis. The authors provided the mean number of days for subjects to return to participation, which was defined as being able to stand, walk, climb stairs, and run without pain. They stated that all values were significant to a .05 confidence level by the Scheffé method.33 We were unsure whether an analysis of variance was performed before the analysis with the Scheffé method. In addition, we questioned which post hoc pairwise comparisons were tested. Also, subjects were not evenly distributed among groups. The total number of subjects in the immediate cryotherapy group was greater than the number in the heat therapy and late cryotherapy groups combined.
In the study by Basur et al,34 the type of work to which the patients returned was not described. In addition, the patients in the study were not athletes, unlike the subjects in the Hocutt et al33 and Wilkerson and Horn-Kingery35 investigations. We wanted to include any study that examined return to work or sport. We felt that this helped to widen the scope of the project. In clinics, athletes are not the only people being treated with cryotherapy. Although the results of the Basur et al34 study are difficult to compare due to the differences in population, we felt that it was important to include the study in our analysis.
Although cryotherapy was examined by Wilkerson and Horn-Kingery,35 compression appeared to be the primary focus of the study. All subjects received some form of cryotherapy at least once per day during the acute phase of injury. Group 1 received uniform compression, whereas groups 2 and 3 received focal compression. Group 2 (U-shaped, liquid-filled device at room temperature with modified Air-Stirrup brace [Aircast, Summit, NJ]) took an average of 11.67 days to return to participation, compared with 12.30 days for group 3 (U- shaped, liquid-filled, frozen device with modified Air-Stirrup brace). The authors stated that the small difference between group 2 and 3 mean values suggests that the mode of compression had a greater effect on return to participation than did cryotherapy. However, both groups had U-shaped, liquid-filled devices with modified Air-Stirrup braces. The only difference between the groups was that group 3's liquid-filled device was frozen. The subjects in group 3 were instructed to exchange a thawed device for a frozen one at 4-hour intervals throughout the day during the acute phase. Groups 1 and 2 were both instructed to ice at least once per day for 20 to 30 minutes. It may be that the long duration of cryotherapy application was actually detrimental to return to participation. However, group 3 did return to participation more quickly than group 1, which led the authors to believe that the focal compression applied to groups 2 and 3 resulted in quicker return to play than the cryotherapy treatment. Groups 2 and 3 attained function levels 60 through 90 in approximately 25% fewer days then Group 1.35 The confounding effect of compression makes it difficult to draw definite conclusions on the effect of cryotherapy.
Laba and Roestenburg36 reported no significant differences in return to participation between groups treated and not treated with cryotherapy after acute inversion ankle sprains. However, subjects with grade 4 injuries treated with cryotherapy returned to participation an average of 2.9 days faster then those not treated with cryotherapy. One limitation of this study is that subjects underwent other forms of rehabilitation in addition to either receiving or not receiving cryotherapy. All subjects received ultrasound treatments and performed basic range-of-motion and strengthening exercises depending on the severity of injury.36 Some variability was noted between the groups with regard to sets, repetitions, and types of exercises (resisted versus active). All of these additional variables confound the potential effects of cryotherapy. It is difficult to determine whether cryotherapy was indeed responsible for the recovery rates of the subjects.
Mechanisms for the Efficacy of Cryotherapy
Because cryotherapy was reported effective in returning subjects to participation in 3 of the 4 articles, we felt that it was important to examine the mechanisms for effectiveness. Two potential mechanisms may be better pain control or reduced secondary tissue injury.
The analgesic effect of cryotherapy is one of the primary reasons clinicians use it in the management of acute musculoskeletal injuries. Slowing of nerve conduction velocity is the likely mechanism for the analgesic response to cold. Ice reduces nerve conduction velocity and slows the stretch reflex. The greatest effect of reduced nerve conduction velocity is shown in superficial nerves,21 and the effect of cold on nerve conduction velocity may last up to 30 minutes after application. When pain is effectively managed, the patient may be able to begin and progress rehabilitation sooner to address range-of-motion and strength deficits as well as progress to full weightbearing and functional activities more rapidly.21
Retarding secondary injury is an important theoretic benefit of cryotherapy.37–39 Secondary tissue death has been attributed to secondary enzymatic injury and secondary hypoxic injury. Knight37 proposed that secondary hypoxic injury is a significant problem after injury. Cryotherapy reduces tissue temperature, slowing the rate of chemical reactions and, therefore, the demand for adenosine triphosphate (ATP).37 Decreased cellular ATP demand decreases the demand for oxygen, which leads to longer tissue survival during hypoxia.39 By decreasing the amount of damaged and necrotic tissue, the healing process can be shortened.
Merrick39 authored an extensive review of secondary tissue injury. The purpose of the paper was to review the secondary injury model and incorporate new theories into the model that will guide further research. It is not currently possible to clearly distinguish primary and secondary tissue damage. No data are available on the time frame for secondary injury.
Merrick39 also addressed the question, “Is the efficacy of short-term cryotherapy explained by reduction or prevention of secondary injury in cells not initially damaged by primary trauma, or is the efficacy explained by rescuing or delaying the death of the cells that were primarily injured but not initially destroyed?” He also questioned the use of the term “secondary hypoxic injury.” Based on the definitions of hypoxia and ischemia, it is appropriate to use the term “secondary ischemic injury.” Hypoxia presents the single challenge of inadequate oxygen, whereas ischemia presents 3 different inadequacies: oxygen, fuel substrates, and waste removal.39–41 All 3 of these problems may contribute to secondary injury. Short- term cryotherapy through mechanisms described earlier may lessen tissue ischemia and, therefore, secondary injury.
Physiotherapy Evidence Database Scale
We chose the PEDro Scale to help us appraise the quality of relevant articles. It identifies research that is unbiased, interpretable, and valid in an effort to discriminate higher and lower quality studies. In addition, the quality of an article gives us an estimate of the likelihood that the results are a valid estimate of the truth.42 At present, more than 50 quality scales are available to review the methodologic quality of research articles, and for most, the reliability is unknown.32 A comprehensive list of scales and checklists for assessing quality of articles has been published by Moher et al.42 This paper is a helpful guide for clinicians who wish to learn about assessing the quality of articles.
The studies we reviewed were conducted as long ago as 27 years, with the most recent having been conducted 10 years ago. During the last decade, research methods in this field have evolved significantly. The mean PEDro quality scores of clinical trials published between 1955 and 1959 was 2.8, whereas trials published between 1995 and 1999 scored on average 5.0.43 The fact that the 4 articles we reviewed scored poorly on the PEDro Scale does not mean that the results and conclusions are invalid. They reflect limitations in the research methods available at the time the studies were conducted. Further investigation into the efficacy of cryotherapy in the treatment of musculoskeletal injuries through randomized, controlled clinical trials is, however, clearly warranted.
CONCLUSIONS
The first question an athlete asks after injury is, “When can I return to play?” Clinicians should use treatments that maximize recovery and minimize both the risk of reinjury and the cost of care. Most research related to cryotherapy has focused on the physiologic response to cold application; thus, a void exists in the area of clinically relevant treatment outcomes. Randomized, controlled clinical trials need to be conducted to examine return to participation. Investigators should randomly allocate participants to groups, conceal allocation, specify eligibility criteria, ensure similar baseline measures of subjects, and report outcome measures from more than 85% of the subjects initially enrolled. Intention-to-treat analysis methods should be used to evaluate data.
Based on the 4 studies we examined critically for this study, we conclude that cryotherapy had a positive effect on return to participation. Even though 2 sets of authors35,36 did not report a significant difference between groups in return to participation, they did display a trend in improvement. In the study by Wilkerson and Horn-Kingery,35 all 3 groups received cryotherapy, with the group receiving the longest duration of cryotherapy improving faster then 1 group but not faster than the other. Laba and Roestenburg36 reported the greater the severity of ankle sprain, the better the effect of cryotherapy on return to participation. The confounding effects of compression and different rehabilitation techniques may have concealed the positive effect of cryotherapy. Therefore, further research is necessary before the effect of cryotherapy on return to participation can be fully elucidated.
REFERENCES
- 1.MacAuley DC. Ice therapy: how good is the evidence? Int J Sports Med. 2001;22:379–384. doi: 10.1055/s-2001-15656. [DOI] [PubMed] [Google Scholar]
- 2.Swenson C, Sward L, Karlsson J. Cryotherapy in sports medicine. Scand J Med Sci Sports. 1996;6:193–200. doi: 10.1111/j.1600-0838.1996.tb00090.x. [DOI] [PubMed] [Google Scholar]
- 3.Stockle U, Hoffmann R, Schutz M, von Fournier C, Sudkamp NP, Haas N. Fastest reduction of posttraumatic edema: continuous cryotherapy or intermittent impulse compression? Foot Ankle Int. 1997;18:432–438. doi: 10.1177/107110079701800711. [DOI] [PubMed] [Google Scholar]
- 4.Philadelphia Panel. Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for low back pain. Phys Ther. 2001;81:1641–1674. [PubMed] [Google Scholar]
- 5.Runeson L, Haker E. Iontophoresis with cortisone in the treatment of lateral epicondylalgia (tennis elbow): a double-blind study. Scand J Med Sci Sports. 2002;12:136–142. doi: 10.1034/j.1600-0838.2002.02142.x. [DOI] [PubMed] [Google Scholar]
- 6.Denegar CR, Hertel J. Clinical education reform and evidence-based clinical practice guidelines. J Athl Train. 2002;37:127–128. [PMC free article] [PubMed] [Google Scholar]
- 7.Sackett DL, Straus SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-Based Medicine: How to Practice and Teach EBM. 2nd ed. Philadelphia, PA: Churchill Livingstone; 2000. [Google Scholar]
- 8.Cormack JC. Evidence-based practice…what is it and how do I do it? J Orthop Sports Phys Ther. 2002;32:484–487. doi: 10.2519/jospt.2002.32.10.484. [DOI] [PubMed] [Google Scholar]
- 9.MacAuley DC. Do textbooks agree on their advice on ice? Clin J Sport Med. 2001;11:67–72. doi: 10.1097/00042752-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Merrick MA, Knight KL, Ingersoll CD, Potteiger JA. The effects of ice and compression wraps on intramuscular temperature at various depths. J Athl Train. 1993;28:236–245. [PMC free article] [PubMed] [Google Scholar]
- 11.Zemke JE, Anderson JC, Guion WK, McMillan J, Joyner AB. Intramuscular temperature responses in the human leg to two forms of cryotherapy: ice massage and ice bag. J Orthop Sports Phys Ther. 1998;27:301–307. doi: 10.2519/jospt.1998.27.4.301. [DOI] [PubMed] [Google Scholar]
- 12.Enwemeka CS, Allen C, Avila P, Bina J, Konrade J, Munns S. Soft tissue thermodynamics before, during, and after cold pack therapy. Med Sci Sports Exerc. 2002;34:45–50. doi: 10.1097/00005768-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Myrer JW, Measom G, Fellingham GW. Temperature changes in the human leg during and after two methods of cryotherapy. J Athl Train. 1998;33:25–29. [PMC free article] [PubMed] [Google Scholar]
- 14.Myrer JW, Myrer KM, Measom GJ, Fellingham GW, Evers SL. Muscle temperature is affected by overlying adipose when cryotherapy is administered. J Athl Train. 2001;36:32–36. [PMC free article] [PubMed] [Google Scholar]
- 15.Martin SS, Spindler KP, Tarter JW, Detwiler K, Petersen HA. Cryotherapy: an effective modality for decreasing intraarticular temperature after knee arthroscopy. Am J Sports Med. 2001;29:288–291. doi: 10.1177/03635465010290030501. [DOI] [PubMed] [Google Scholar]
- 16.Karunakara RG, Lephart SM, Pincivero DM. Changes in forearm blood flow during single and intermittent cold application. J Orthop Sports Phys Ther. 1999;29:177–180. doi: 10.2519/jospt.1999.29.3.177. [DOI] [PubMed] [Google Scholar]
- 17.Curl WW, Smith BP, Marr A, Rosencrance E, Holden M, Smith TL. The effect of contusion and cryotherapy on skeletal muscle microcirculation. J Sports Med Phys Fitness. 1997;37:279–286. [PubMed] [Google Scholar]
- 18.Ho SSW, Illgen RL, Meyer RW, Torok PJ, Cooper MD, Reider B. Comparison of various icing times in decreasing bone metabolism and blood flow in the knee. Am J Sports Med. 1995;23:74–76. doi: 10.1177/036354659502300112. [DOI] [PubMed] [Google Scholar]
- 19.Thorsson O, Lilja B, Ahlgren L, Hemdal B, Westlin N. The effect of local cold application on intramuscular blood flow at rest and after running. Med Sci Sports Exerc. 1985;17:710–713. doi: 10.1249/00005768-198512000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Weston M, Taber C, Casagranda L, Cornwall M. Changes in local blood volume during cold gel pack application to traumatized ankles. J Orthop Sports Phys Ther. 1994;19:197–199. doi: 10.2519/jospt.1994.19.4.197. [DOI] [PubMed] [Google Scholar]
- 21.Lee JM, Warren MP, Mason SM. Effects of ice on nerve conduction velocity. Physiotherapy. 1978;64:2–6. [PubMed] [Google Scholar]
- 22.Ingersoll CD, Mangus BC. Sensations of cold reexamined: a study using the McGill pain questionnaire. J Athl Train. 1991;26:240–245. [Google Scholar]
- 23.Brandner B, Munro B, Bromby LM, Hetreed M. Evaluation of the contribution to postoperative analgesia by local cooling of the wound. Anaesthesia. 1996;51:1021–1025. doi: 10.1111/j.1365-2044.1996.tb14995.x. [DOI] [PubMed] [Google Scholar]
- 24.Benson TB, Copp EP. The effects of therapeutic forms of heat and ice on the pain threshold of the normal shoulder. Rheumatol Rehabil. 1974;13:101–104. doi: 10.1093/rheumatology/13.2.101. [DOI] [PubMed] [Google Scholar]
- 25.Dolan MG, Thornton RM, Fish DR, Mendel FC. Effects of cold water immersion on edema formation after blunt injury to the hind limbs of the rats. J Athl Train. 1997;32:233–237. [PMC free article] [PubMed] [Google Scholar]
- 26.McMaster WC, Liddle S. Cryotherapy influence on posttraumatic limb edema. Clin Orthop. 1980;150:283–287. [PubMed] [Google Scholar]
- 27.Matsen FA, 3rd, Questad K, Matsen AL. The effect of local cooling on postfracture swelling: a controlled study. Clin Orthop. 1975;109:201–206. doi: 10.1097/00003086-197506000-00029. [DOI] [PubMed] [Google Scholar]
- 28.Deal DN, Tipton J, Rosencrance E, Curl WW, Smith TL. Ice reduces edema: a study of microvascular permeability in rats. J Bone Joint Surg Am. 2002;84:1573–1578. [PubMed] [Google Scholar]
- 29.Meeusun R, van der Venn P, Joos E, Roeykens J, Bossuyt A, De Meirleir K. The influence of cold and compression on lymph flow at the ankle. Clin J Sport Med. 1998;8:266–271. doi: 10.1097/00042752-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 31.PEDro Scale. Available at: http://www.pedro.fhs.usyd.edu.au/. Accessed April 1, 2003.
- 32.Maher C, Sherrington C, Herbert R, Moseley A, Elkins M. Reliability of the PEDro rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 33.Hocutt JE, Jr, Jaffe R, Rylander CR, Beebe JK. Cryotherapy in ankle sprains. Am J Sports Med. 1982;10:316–319. doi: 10.1177/036354658201000512. [DOI] [PubMed] [Google Scholar]
- 34.Basur RL, Shephard E, Mouzas GL. A cooling method in the treatment of ankle sprains. Practitioner. 1976;216:708–711. [PubMed] [Google Scholar]
- 35.Wilkerson GB, Horn-Kingery HM. Treatment of the inversion ankle sprain: comparison of different modes of compression and cryotherapy. J Orthop Sports Phys Ther. 1993;17:240–246. doi: 10.2519/jospt.1993.17.5.240. [DOI] [PubMed] [Google Scholar]
- 36.Laba E, Roestenburg M. Clinical evaluation of ice therapy for acute ankle sprain injuries. N Z J Physiother. 1989;17:7–9. [Google Scholar]
- 37.Knight KL. Cryotherapy in Sports Injury Management. Champaign, IL: Human Kinetics; 1995. pp. 3–98. [Google Scholar]
- 38.Knight KL. Effects of hypothermia on inflammation and swelling. Athl Train J Natl Athl Train Assoc. 1976;11:7–10. [Google Scholar]
- 39.Merrick MA. Secondary injury after musculoskeletal trauma: a review and update. J Athl Train. 2002;37:209–217. [PMC free article] [PubMed] [Google Scholar]
- 40.Kotter M, Osguthorpe S. Alterations in oxygen transport. In: Copstead LC, Banasik JL, editors. Pathophysiology: Biological and Behavioral Perspectives. 2nd ed. Philadelphia, PA: WB Saunders; 2000. pp. 292–331. [Google Scholar]
- 41.Majno G, Joris I. Cells, Tissues, and Disease: Principles of General Pathology. Cambridge, MA: Blackwell Scientific; 1996. [Google Scholar]
- 42.Moher D, Jadad AR, Nichol G, Penman M, Tugwell P, Walsh S. Assessing the quality of randomized controlled trials: an annotated bibliography of scales and checklists. Control Clin Trials. 1995;16:62–73. doi: 10.1016/0197-2456(94)00031-w. [DOI] [PubMed] [Google Scholar]
- 43.Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro) Aust J Physiother. 2002;48:43–49. doi: 10.1016/s0004-9514(14)60281-6. [DOI] [PubMed] [Google Scholar]