Abstract
Background
Radiotherapy may lead to side-effects undermining patients’ quality of life (QOL). While mind-body practices such as qigong appear to improve QOL in cancer survivors, little is known about benefits for patients undergoing radiotherapy. Thus, this RCT examined the efficacy of a qigong intervention on QOL in women with breast cancer during and after treatment.
Methods
Ninety-six women with breast cancer were recruited from a cancer center in Shanghai, China, and randomized to the qigong (N=49) or waitlist control (N=47) group. Women in the qigong group attended 5 weekly classes over 5–6 weeks of radiotherapy. QOL outcomes (i.e., depressive symptoms, fatigue, sleep disturbance, and overall QOL) and cortisol slopes were assessed at baseline, during and at the end of treatment, and 1 and 3 months later.
Results
The mean age of the women was 46 years (range 25–64); stage 0 (7%) stage I (25%), stage II (40%) and stage III (28%); with over half (54%) having undergone mastectomy surgery. Multilevel analyses revealed that women in the qigong group reported less depressive symptoms over time than in the control group (P=.05). Women with elevated depressive symptoms at radiotherapy onset reported less fatigue (P<.01) and better overall QOL (P<.05) in the qigong compared to the control group. Findings were clinically significant. No significant differences were found for sleep disturbance and cortisol slopes.
Conclusion
Qigong may have therapeutic effects in the management of QOL in women receiving radiotherapy for breast cancer. Benefits were particularly evident for patients with pre-intervention elevated levels of depressive symptoms.
INTRODUCTION
Despite incredible medical advances in cancer treatment, patients are faced with treatment side effects undermining their quality of life (QOL). Patients with breast cancer are at particularly high risk because they tend to receive multimodal treatment including surgery, chemotherapy, and/or radiotherapy over an extended period of time,1,2 leading to an accumulation of related morbidity. Side effects may include pain, fatigue, pulmonary symptoms, radiation burns, nausea, vomiting, insomnia, infertility, and sexual dysfunction among others.3 Not surprisingly, patients are also at risk of experiencing anxiety and depression.4–7 Psychological distress is problematic because it contributes to hypothalamic-pituitary-adrenal (HPA) axis dysregulation,8,9 which may impact tumor progression, overall recovery, and possibly even survival.10–12 A reliable measure of HPA axis dysregulation is to assess the diurnal cortisol pattern, a stress hormone and an end-product of the HPA axis.13 Studies have revealed that both elevated levels of cortisol and flattened high levels or erratic diurnal fluctuations of cortisol cause down-regulation of the immune response and are associated with worse survival in women with breast cancer.14,15
Growing evidence suggests that stress-reduction techniques (e.g., meditation, progressive relaxation, diaphragmatic breathing, guided imagery, and physical movements) improve QOL and reduce physiological stress (i.e., HPA axis dysregulation).16–19 Even though practicing these techniques individually appears to be successful in reducing psychological distress, a mind-body intervention such as the ancient Chinese practice of qigong (“qi” energy flow; “gong” skill or achievement)20 that combines many of these techniques may be particularly effective in addressing the multi-faceted needs of breast cancer patients undergoing active treatment. Through mind-body integration of specific movements, breathing techniques, meditation, and a mindful focus on the body, the primary goal of qigong is to manipulate one’s energy (qi) for the benefit of one’s physical, psychological, and spiritual health. A recent review of clinical trials examining the effects of qigong in cancer patients receiving chemotherapy revealed generally positive findings.21 For instance, in a sample of 81 patients with mixed cancer diagnoses, patients participating in a 10-week qigong program experienced better overall QOL and less inflammation compared to those receiving usual care.22 Yet, little is known about benefits for patients undergoing radiotherapy (RT) and potential long-term effects as none of the previous studies in cancer patients include follow-up assessments beyond the intervention period. Thus, we were interested in the effects of practicing qigong on QOL and biological indices of stress (i.e., cortisol function) during and after completing RT. Because QOL is a broad, multidimensional construct,23 we focused on the most frequently reported long-term QOL concerns in this population including depressive symptoms, fatigue, and sleep disturbances as well as overall QOL.24
We hypothesized that patient who practice qigong would report better QOL (i.e., fewer depressive symptoms, less fatigue and sleep disturbance, and improved overall QOL) compared to patients in a wait-list control (WLC) during and after treatment. We also hypothesized that women in the qigong group would have less cortisol dysregulation as reflected in a steeper diurnal cortisol slope and a smaller cortisol awakening response than the WLC group. As a secondary goal, we examined the effectiveness of the qigong program as a function of women’s baseline depressive symptoms. A recent meta-analysis25 of 61 trials demonstrated that pre-intervention depressive symptoms/psychological distress moderates the efficacy of psychosocial/behavioral treatment for cancer patients suggesting that psychosocial/behavioral interventions may be most beneficial for cancer patients with elevated depressive symptoms. Consequently, we hypothesized that patients with high baseline depressive symptoms would benefit more from the qigong intervention compared to patients with low baseline depressive symptoms.
PATIENTS AND METHODS
Study Population
The trial was conducted at the Fudan University Shanghai Cancer Center, Shanghai, China between 2005 and 2007 in collaboration with faculty from the MD Anderson Cancer Center, Houston, Texas. Women with stage 0–III breast cancer who were at least 18 years old, able to read, write, and speak Mandarin, had undergone breast surgery, and were scheduled to receive 5–6 weeks of RT were eligible to participate in the study. Patients who were unable to legally provide consent and those who reported prior regular qigong or tai chi practice (self-defined) within the past year were excluded from the study.
Procedures
During pretreatment clinic visits, right after the treating radiation oncologist had briefly introduced the study to potentially eligible patients, research nurses approached patients, confirmed study eligibility, and obtained written informed consent prior to data collection. Before the start of RT and randomization, patients underwent a baseline (T1) assessment of questionnaires and provided saliva samples at four time points per day for two consecutive days to assess cortisol rhythm according to procedures described elsewhere.13,26 Participants undergoing RT as outpatients were then randomly assigned to either the qigong or WLC group by a form of adaptive randomization called minimization27 so that the groups were evenly balanced according to stage of disease, age, time since diagnosis, type of surgery (mastectomy vs. breast conserving surgery), and prior chemotherapy. Participants undergoing RT as inpatients were assigned to cohorts to minimize bias and contamination of the control group since all inpatient participants resided on the same floor during treatment. Every inpatient participant in a given cohort was assigned to the same group as determined by a coin flip. Once everyone in the cohort had finished her treatment, the next cohort received the alternate condition. Participants in the qigong group followed the qigong program as described below. Women in the WLC group received the standard of care.
Participants in both conditions completed four additional assessments including questionnaires and saliva sample collection similar to baseline: middle of RT (T2); during the last week of RT (T3); and 1 month (T4) and 3 months (T5) after the end of RT. Patients were given a small gift (a $20 value) for completing each assessment. If the patients were not coming for a follow up visit or were unable to travel, a questionnaire and saliva kit were mailed to them. Women who were assigned to the WLC group were given the option of attending the qigong program after the completion of the last assessment but no additional data were collected. The Institutional Review Boards of both MD Anderson and Fudan University Shanghai Cancer Center approved the protocol.
Qigong Program
Women in the qigong group attended five 40-minute qigong classes each week during their 5–6 weeks of RT. All qigong sessions were taught by the same instructor who was a government licensed traditional Chinese medicine doctor and qigong master, trained at the Shanghai University of Traditional Chinese Medicine with 30 years of clinical experience. Session attendance ranged from 1 to 10 participants. Participants were given a DVD with a recording of the qigong program and some printed materials with similar instructions and encouraged to practice qigong on their own on the days when they did not meet with the qigong master and after they had completed RT.
The program involved a modified version of a Chinese medical qigong therapy developed by Guo Lin (Goulin New Qigong), often referred to as “walking qigong,”20 frequently prescribed in China for medical conditions including cancer and consisted of several breathing and moving exercises. After a brief course introduction, each session was separated into three parts: 1) Preparation Exercise: relaxation (gentle breathing and meditation; 4 min.), synchronizing the breath with slow shallow squatting movements (3 min.), and synchronizing the breath with gentle arm movements in front of the abdomen (opening and closing of the dantian; 3–6 min); 2) Main Exercise: participants walked in a circle synchronizing their breathing, arm movements, and steps focusing on the movement of their body with the goal of calming one’s mind, relaxing various parts of the body and the mind, and revitalizing the “life-force,” i.e., qi. This was first done slowly and then fast using wind-like breathing (18 min); and 3) Ending Exercise: breathing exercises, opening and closing of the dantian, and self-massage (3–6 min). Participants practiced in a standing position.
Measures
All questionnaires were administered in Chinese using validated translated versions of the original instruments.28–31
Symptoms of depression were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D),28 a 20-item self-report measure of depression that focuses on depressive feelings and behaviors over the past week, with higher scores representing worse symptoms. A cutoff score of ≥16 indicates “caseness” warranting further psychological evaluation for clinical depression.
Fatigue was assessed using the Brief Fatigue Inventory (BFI),31 a nine-item questionnaire asking participants to rate the severity of their fatigue at that moment and how much it interfered with their lives during the previous 24 hours. Higher scores represent worse fatigue.
Sleep disturbances were assessed using the Pittsburgh Sleep Quality Index (PSQI),29 an 18-item self-rated questionnaire that assesses sleep disturbances over the past month. The instrument includes seven subscales: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction. The current study reports on the total score. Higher scores represent greater sleep disturbances.
Overall QOL was assessed with the 28-item Functional Assessment of Cancer Therapy-General (FACT-G)30 to assess health-related QOL including physical, functional, social, and emotional well-being dimension. Research indicates that a total difference score of ≥7 on the Fact-G is clinically significant.32
Cortisol Rhythm
To determine the circadian nature of cortisol, four saliva samples per day (waking, 45 minutes later, 8 hours later, and at bedtime) were obtained for two consecutive days.33 Levels of cortisol were determined using a time resolved immunoassay with fluorescence detection.
Demographic and Medical Factors and Tracking Data
Some demographic items (e.g., age, marital status) were included in the baseline questionnaires. Medical data were extracted from patients’ charts. Tracking data were kept regarding study attrition, qigong class attendance, and frequency of home practice. Participants in the qigong group completed a brief evaluation of the class and their home practice each week when they attended the qigong classes and with their questionnaires at later assessments (T4 and T5).
Data Analyses
The primary outcome was the 1-month QOL indices (i.e., fewer depressive symptoms, less fatigue and sleep disturbance, and improved overall QOL). A sample size of approximately 50 patients per group provided 80% power (2-sided alpha P=.05) to detect effect sizes between .56 and .63 assuming 10% attrition. We calculated descriptive statistics and examined if demographic and medical factors (e.g., age, income, stage, time since surgery, and type of surgery) were significantly related to the outcomes at P<.05. If so, these factors were included as control variables in the main analyses along with inpatient/outpatient status. Main analyses were performed with multilevel modeling (MLM) analyses using Proc MIXED (SAS, 9.2.2 version) accounting for the nested data structure of our repeated measure design for each outcome variable. To evaluate the general effectiveness of the qigong intervention, we examined the group by time interaction effect while controlling for main effects and baseline scores of the outcome variable. For significant group by time interactions, we compared least squared means (LSM) for each group at each time point using the general linear model (GLM) analysis controlling for baseline levels of the outcome variable and illustrated the interaction by plotting LSM. Due to non-normal distribution of cortisol data, the raw levels were log-transformed. Cortisol circadian slopes were calculated by regressing log-transformed cortisol levels on the saliva collecting time (hours after waking up in the morning) for each participant at each assessment point. Cortisol awakening response was calculated by examining the difference between cortisol levels at wakening and 45 min. later. To evaluate if the intervention was more effective for participants scoring high (i.e., scoring 1 standard deviation above the sample mean) in baseline depressive symptoms, we examined the group by time by baseline depression interaction effect for QOL outcomes. Because less than five comparisons were performed and comparisons involved complementary constructs, we did not use a multiple comparison adjustment.34,35 Further, because our analyses involved the testing of interaction terms, all significance tests were highly conservative.36
RESULTS
Baseline Characteristics of Sample
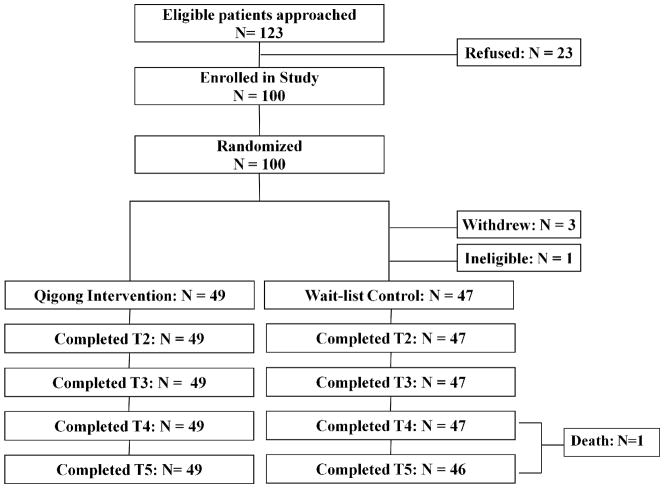
We approached 123 eligible women of which 100 consented to participate in the study. While 14 patients failed to provide a reason for study refusal, others expressed a lack of interest (n=3), physical symptoms (n=3), spousal concerns (n=2), or time constraints (n=1) preventing participation. After randomization and before the start of radiotherapy, one patient become ineligible (discontinued RT) and three withdrew from the study (lack of interest, spouse’s wish, and medical complications) leaving 49 patients in the qigong and 47 patients in the WLC group. All participants completed all assessments except one patient in the WLC group who died after the T4 assessment (Figure 1).
Figure 1.
Consort flow diagram.
The baseline characteristics of the participants assigned to each condition were analyzed using chi-square tests for categorical variables (e.g., inpatient vs. outpatient, income, type of surgery, prior chemotherapy) and t-tests for continuous variables (e.g., age, time since surgery). There were no significant group differences in patient characteristics (see Table 1). The sample mean of CES-D scores was 12.64 (SD±9.01) with 39.2 % of the sample meeting the CES-D criterion for caseness. Importantly, there were no group differences at baseline in any of the outcome variables (depressive mood, fatigue, sleep disturbance, overall QOL, and cortisol slope).
Table 1.
Participant Demographics and Clinical Characteristics by Group
| Variable | Qigong (n=49) | WLC (n=47) | p-value |
|---|---|---|---|
| Mean age, years ±SD, (range) | 45.3±6.3 (29–58) | 44.7±9.7 (25–62) | 0.73 |
| Marital Status | |||
| Married | 46 (93.9%) | 40 (87.0%) | 0.25 |
| Highest Level of Education | |||
| Some college or higher | 26 (55%) | 23 (50%) | 0.17 |
| Income+ | |||
| <1,500 | 2 (4.1%) | 4 (8.7%) | 0.12 |
| 1,500–7,900 | 20 (40.8%) | 21 (45.7%) | |
| 8,000–15,800 | 10 (20.4%) | 12 (26.1%) | |
| >15,800 | 7 (14.3%) | 4 (8.7%) | |
| Refused to answer | 10 (20.4%) | 5 (10.9%) | |
| Stage | |||
| 0 | 2 (4.3%) | 3 (6.7%) | 0.20 |
| I | 8 (17.4% | 14 (31.1%) | |
| II | 17 (34.7%) | 17 (36.2%) | |
| III | 17 (34.7%) | 7 (14.9%) | |
| Time since surgery, weeks ±SD, (range) | 16.5±5.5 (2.14–23.86) | 14.7±5.7 (0–25.1) | 0.24 |
| Surgery Type | |||
| Mastectomy | 18 (36.7%) | 26 (56.5%) | 0.07 |
| Lumpectomy | 31 (63.3%) | 20 (43.5%) | |
| RT fractions | |||
| 25 | 39 (78.3%) | 35 (77.8%) | 0.90 |
| 30 | 9 (19.6%) | 10 (22.2) | |
| 35 | 1 (2.2%) | 0 | |
Abbreviations: WLC, Wait-list control receiving usual care; SD, Standard deviation;
Income converted to US dollars from Chinese Yuan.
Adherence to Qigong Program
Adherence was high with 30.4% of women having attended 100% of the sessions, 65.2% attended at least 80% of the session, and 78.3% attended at least 50% of the sessions with only 13.0% attending less than 20% (mean 22.0 sessions (SD 6.1), and range of 5–30).
Main Effect of Intervention
Depressive Symptoms
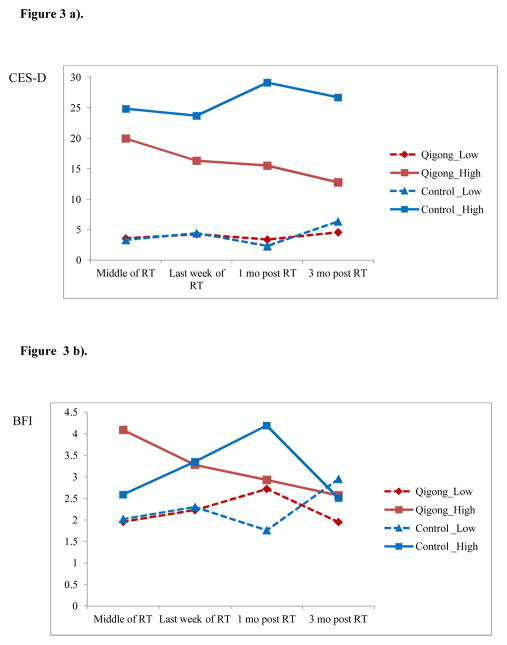
Multilevel modeling analyses revealed a significant main effect of time (F(4,367)=10.91, p=.001) indicating that depression scores decreased over time. However, this effect was moderated by group (F(3,281)= 2.62, P=0.05) indicating significant group differences in changes in depression over time. Figure 2 illustrates a reduction in depressive symptoms over time for the qigong group with no changes in the WLC group. Follow-up analyses at specific time points revealed marginally significant group difference at T4 (F(1, 92) =2.97, p=.09; adjusted means: qigong 10.01 vs. WLC 12.14).
Figure 2.
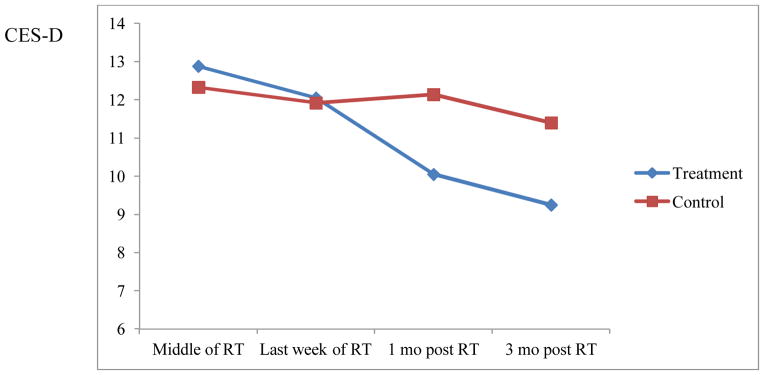
Least square means (adjusted for baseline level) of a multilevel modeling analysis for depressive symptoms over time. Higher scores represent greater symptoms.
No significant group differences were found for fatigue, overall QOL, sleep disturbance, and cortisol circadian slope or cortisol awakening response (see Table 2 for means by group over time for each variable).
Table 2.
Raw Means of Outcome Measures by Group at Each Assessment Point
| Measure | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||||
| Baseline | Middle of RT | Last week of RT | 1-month post RT | 3-months post RT | ||||||||||||||||
|
| ||||||||||||||||||||
| Qigong | WLC | Qigong | WLC | Qigong | WLC | Qigong | WLC | Qigong | WLC | |||||||||||
|
| ||||||||||||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
|
| ||||||||||||||||||||
| CES-D | 13.1 | 8.9 | 12.2 | 9.2 | 13.1 | 8.6 | 12.1 | 9.1 | 12.3 | 8.2 | 11.6 | 8.1 | 10.3 | 7.0 | 11.9 | 10.3 | 9.5 | 6.6 | 11.2 | 9.8 |
| BFI | 3.0 | 2.6 | 2.4 | 2.2 | 3.2 | 2.3 | 2.6 | 2.0 | 3.1 | 2.0 | 2.7 | 2.1 | 2.9 | 1.9 | 2.4 | 2.0 | 2.6 | 1.8 | 2.3 | 1.8 |
| PSQI | 12.0 | 3.7 | 11.7 | 4.0 | 12.0 | 4.3 | 10.9 | 3.5 | 12.0 | 4.1 | 11.3 | 3.7 | 11.0 | 3.3 | 10.3 | 3.3 | 10.1 | 3.1 | 9.6 | 2.9 |
| FACT-G | 75.8 | 17.3 | 80.5 | 15.1 | 76.6 | 17.2 | 79.5 | 16.7 | 76.6 | 16.4 | 80.8 | 15.7 | 79.9 | 15.4 | 80.8 | 18.7 | 82.1 | 15.4 | 82.8 | 15.9 |
| Slope | −.10 | .05 | −.10 | .05 | −.12 | .04 | −.10 | .05 | −.12 | .04 | −.11 | .05 | −.11 | .05 | −.09 | .06 | −.11 | .05 | −.09 | .05 |
| CAR | −.19 | .44 | −.06 | .48 | −.18 | .53 | −.01 | .64 | −.11 | .61 | −.15 | .45 | −.17 | .66 | −.14 | .48 | −.24 | .63 | .01 | .62 |
Abbreviations: WLC, Wait-list control; CES-D, Center for Epidemiologic Studies Depression Scale; BFI, Brief Fatigue Inventory; PSQI, Pittsburgh Sleep Quality Index; FACT-G, Functional Assessment of Cancer Therapy-General; Slope, cortisol circadian slope; CAR, cortisol awakening response
Depression as a Moderator of Intervention Effectiveness
Depressive Symptoms
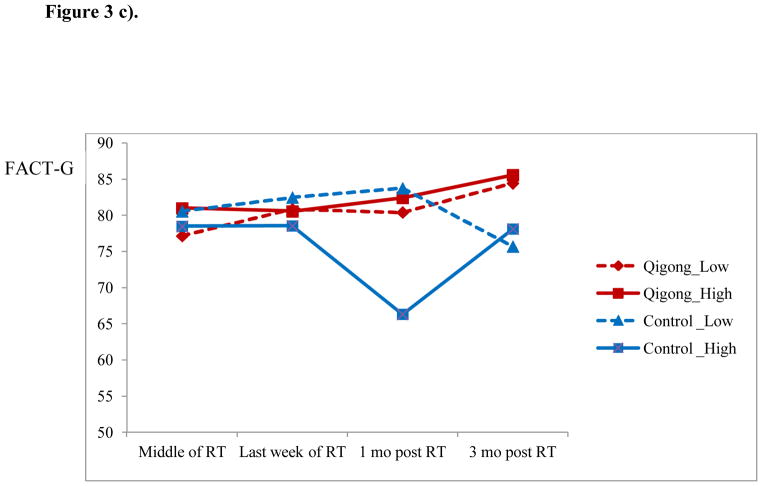
There was a significant group x time x baseline depression interaction effect (F(4,368)=3.98; P=.004) for depressive symptoms. We decomposed the interaction by high and low (mean±1SD) baseline depressive symptoms and plotted the LSM for each group across time (Figure 3a). There were no significant group differences for those low in baseline depressive symptoms at any assessment point. For women with high baseline depressive symptoms, there were marginally significant group difference at T3 (F(1,92)=3.78, P=.06; qigong 16.36 vs. WLC 23.6), and significant group differences at T4 (F(1,92) =13.32, P<.001; qigong 15.5 vs. WLC 29.1) and T5 (F(1,90)=6.48, P<.05; qigong 12.74 vs. WLC 26.51).
Figure 3.
Least square means (adjusted for baseline level) of a multilevel modeling analysis by group for those with high and low baseline depressive symptoms (mean±1SD) over time for a) depressive symptoms (CES-D); b) fatigue (BFI); and c) overall QOL (FACT-G); Higher scores represent greater symptoms and fatigue and better overall OQL.
Fatigue
Controlling for stage at diagnosis (which was associated with fatigue levels), there was a significant group x time x baseline depression interaction effect (F(3,275) = 4.25; P=.01) for fatigue. To illustrate the overall effect of the significant interaction, we decomposed the interaction by high and low of baseline depressive symptoms and plotted the LSM for each group across time (Figure 3b). There were no significant group differences for those low in baseline depressive symptoms at any assessment point. For women with high baseline depressive symptoms, there were significant group differences at T4 (F(1,90) =5.36, P<.05; qigong 2.93 vs. WLC 4.19).
Overall QOL
Controlling for stage at diagnosis and type of resection (which were associated with overall QOL), there was a significant group x time x baseline depression interaction effect (F(3,275) = 3.03; P=.02) on overall QOL. To illustrate the overall effect of the significant interaction, we decomposed the interaction by high and low of baseline depressive symptoms and plotted the LSM for each group across time (Figure 3c). There were no significant group differences for those low in baseline depressive symptoms at any assessment point. For women with high baseline depressive symptoms, there were significant group differences at T4 (F(1,90) =7.71, P<.01.; qigong 82.44 vs. WLC 66.31). Importantly, the group differences were also clinically significant (7 point between-group difference).32 At T5, there was a clinically but not statistically significant difference (qigong 85.55 vs. WLC 78.11) for women high baseline depressive symptoms.
Sleep Disturbances and Cortisol Outcomes
Baseline depressive symptoms did not significantly moderate the group x time interaction effect on sleep disturbances, cortisol circadian slope or cortisol awakening response.
Treatment Adherence
Class attendance and home practice were not significantly associated with any of the outcomes.
DISCUSSION
The current RCT found that qigong may reduce depressive symptoms in women with breast cancer undergoing RT. Qigong may be particularly helpful for women who reported elevated levels of depressive symptoms at RT initiation. When baseline symptoms of depression were taken into account, group differences revealed lower depressive symptoms, fatigue and better overall QOL for the qigong versus WLC group. This finding may have important implications given the association between depression and survival in prospective studies.10 The observed benefits exceeded the threshold for clinically significant differences in overall QOL32 at 1 and 3 month post RT. Generally, observed significant differences in outcomes (depressive symptoms, fatigue, and overall QOL) emerged after but not during treatment suggesting that qigong may prevent delayed symptom burden or expedite the RT recovery process for women with elevated levels of depressive symptoms at the start of RT.
This research supports the promising findings of previously reported qigong trials;21,22 however, it is the first trial that enrolled women while on active RT treatment and included a follow-up period. Because no adverse events were reported in the study participants, qigong appears to be a safe therapy for patients on active treatment that is well accepted with 65% of women adhering to at least 80% of the qigong sessions. Our findings also support the findings of a recent, large meta-analysis25 suggesting that behavioral interventions are most efficacious for participants with increased baseline levels of depressive symptoms or distress. Consequently, even though our trial showed reduced depressive symptoms over time for the qigong group with no changes in the WLC group, the findings suggest that patients with depressive symptoms may benefit the most from a qigong intervention. Nevertheless, these findings are too preliminary to offer clinical recommendations and further research is needed to examine differential effects for all-comers versus at-risk patients and compare the benefits of qigong with other mind-body interventions (e.g., yoga37). Future research is also needed to uncover psychosocial and biological mechanisms by which qigong affects symptom relief. We examined one mechanism, cortisol rhythm, which yielded no significant group differences.
Our study had some limitations. We did not include an active control intervention. Thus, we cannot rule out that the effects of the intervention were not influenced by patients’ expectancies of the qigong practice and the attention and social support participants in the qigong group received over the 5–6 week intervention period. We are currently addressing these concerns in a three-arm, single-blinded qigong trial. Also, the homogenous nature of our sample that was specifically Chinese women at a single-site in Shanghai, China, limits the generalizability of our results. Consequently, it would be prudent to further explore the benefits of qigong in culturally and ethnically diverse samples of breast cancer patients and patients with other cancer types including non-gender specific disease sites. The finding for the benefits of qigong based on pre-RT depressive symptoms needs to be interpreted with caution as the patients were not recruited based on depressive symptoms. Finally, we followed participants for only 12 weeks post RT, so the long-term effectiveness of qigong in patients with breast cancer remains to be determined.
In conclusion, this randomized clinical trial found that qigong may lead to reductions in depressive symptoms over time and may be especially useful for women reporting high symptoms of depression at baseline. Studies involving a blinded design with an active control group, enriched for high levels of baseline depressive symptoms, and longer-term follow-up are necessary to examine generalizablity of our findings and to deepen our understanding of this promising therapeutic approach.
Acknowledgments
Grant Support:
Support was provided in part by the United States National Cancer Institute (NCI) grants R21CA108084 and U19CA121503 (principal investigator, Lorenzo Cohen), the NCI Cancer Center Support Grant CA016672.
We thank Drs. Peiying Yang, Joseph Chiang, and Qingyi Wei for all their support with language, culture, and politics.
Footnotes
Financial disclosure: None of the authors have any conflict of interests to disclose.
References
- 1.Overgaard M, Hansen PS, Overgaard J, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. New England Journal of Medicine. 1997;337:949–955. doi: 10.1056/NEJM199710023371401. [DOI] [PubMed] [Google Scholar]
- 2.Ragaz J, Jackson SM, Le N, et al. Adjuvant radiotherapy and chemotherapy in node-positive premenopausal women with breast cancer. New England Journal of Medicine. 1997;337:956–962. doi: 10.1056/NEJM199710023371402. [DOI] [PubMed] [Google Scholar]
- 3.Society AC. Breast Cancer Facts & Figures 2011–2012. Atlanta: 2011. [Google Scholar]
- 4.Wengstrom Y, Haggmark C, Strander H, et al. Perceived symptoms and quality of life in women with breast cancer patients receiving radiation therapy. Eur J Oncol Nurs. 2000;4:78–88. doi: 10.1054/ejon.1999.0052. [DOI] [PubMed] [Google Scholar]
- 5.Spiegel D. Psychosocial aspects of breast cancer treatment. Seminars in Oncology. 1997;24:36–47. [PubMed] [Google Scholar]
- 6.Redd WH, Silberfarb PM, Andersen BL, et al. Physiologic and psychobehavioral research in oncology. Cancer. 1991;67:813–822. doi: 10.1002/1097-0142(19910201)67:3+<813::aid-cncr2820671411>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 7.Aaronson NK, Meyerowitz BE, Bard M, et al. Quality of life research in oncology. Past achievements and future priorities. Cancer. 1991;67:839–843. doi: 10.1002/1097-0142(19910201)67:3+<839::aid-cncr2820671415>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 8.Vedhara K, Tuinstra J, Miles JN, et al. Psychosocial factors associated with indices of cortisol production in women with breast cancer and controls. Psychoneuroendocrinology. 2006;31:299–311. doi: 10.1016/j.psyneuen.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Thornton LM, Andersen BL, Carson WE., 3rd Immune, endocrine, and behavioral precursors to breast cancer recurrence: a case-control analysis. Cancer Immunol Immunother. 2008;57:1471–81. doi: 10.1007/s00262-008-0485-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer. 2009;115:5349–61. doi: 10.1002/cncr.24561. [DOI] [PubMed] [Google Scholar]
- 11.Giese-Davis J, Collie K, Rancourt KM, et al. Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer: a secondary analysis. J Clin Oncol. 2011;29:413–20. doi: 10.1200/JCO.2010.28.4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Antoni MH, Lutgendorf SK, Cole SW, et al. The influence of bio-behavioural factors on tumour biology: pathways and mechanisms. Nat Rev Cancer. 2006;6:240–8. doi: 10.1038/nrc1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kirschbaum C, Hellhammer DH. Salivary cortisol in psychoneuroendocrine research: recent developments and applications. Psychoneuroendocrinology. 1994;19:313–33. doi: 10.1016/0306-4530(94)90013-2. [DOI] [PubMed] [Google Scholar]
- 14.Sephton SE, Sapolsky RM, Kraemer HC, et al. Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst. 2000;92:994–1000. doi: 10.1093/jnci/92.12.994. [DOI] [PubMed] [Google Scholar]
- 15.Filipski E, King VM, Li X, et al. Host circadian clock as a control point in tumor progression. J Natl Cancer Inst. 2002;94:690–7. doi: 10.1093/jnci/94.9.690. [DOI] [PubMed] [Google Scholar]
- 16.Carlson LE, Speca M, Patel KD, et al. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65:571–81. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- 17.Phillips KM, Antoni MH, Lechner SC, et al. Stress management intervention reduces serum cortisol and increases relaxation during treatment for nonmetastatic breast cancer. Psychosom Med. 2008;70:1044–9. doi: 10.1097/PSY.0b013e318186fb27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krischer MM, Xu P, Meade CD, et al. Self-administered stress management training in patients undergoing radiotherapy. Journal of Clinical Oncology. 2007;25:4657–62. doi: 10.1200/JCO.2006.09.0126. [DOI] [PubMed] [Google Scholar]
- 19.Antoni MH, Carver CS, Boyers A, et al. Cognitive behavioral stress management intervention increases positive adaptation to breast cancer. Psychosomatic Medicine. 1999;61:94. [Google Scholar]
- 20.Cohen KS. The way of qigong: the art and science of Chinese energy healing. 1. New York: Ballentine Books; 1997. [Google Scholar]
- 21.Oh B, Butow P, Mullan B, et al. A Critical Review of the Effects of Medical Qigong on Quality of Life, Immune Function, and Survival in Cancer Patients. Integr Cancer Ther. 2011 doi: 10.1177/1534735411413268. [DOI] [PubMed] [Google Scholar]
- 22.Oh B, Butow PN, Mullan BA, et al. Effect of medical Qigong on cognitive function, quality of life, and a biomarker of inflammation in cancer patients: a randomized controlled trial. Support Care Cancer. 2011 doi: 10.1007/s00520-011-1209-6. [DOI] [PubMed] [Google Scholar]
- 23.Cella DF, Tulsky DS. Quality of life in cancer: definition, purpose, and method of measurement. Cancer Invest. 1993;11:327–36. doi: 10.3109/07357909309024860. [DOI] [PubMed] [Google Scholar]
- 24.Bower JE, Ganz PA, Irwin MR, et al. Inflammation and behavioral symptoms after breast cancer treatment: do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol. 2011;29:3517–22. doi: 10.1200/JCO.2011.36.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schneider S, Moyer A, Knapp-Oliver S, et al. Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: a meta-analysis. J Behav Med. 2010;33:1–14. doi: 10.1007/s10865-009-9227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pruessner JC, Wolf OT, Hellhammer DH, et al. Free cortisol levels after awakening: a reliable biological marker for the assessment of adrenocortical activity. Life Sci. 1997;61:2539–49. doi: 10.1016/s0024-3205(97)01008-4. [DOI] [PubMed] [Google Scholar]
- 27.Pocock SJ. Clinical trials: A practical approach. New York: John Wiley & Sons; 1983. [Google Scholar]
- 28.Cheng ST, Chan ACM. The Center for Epidemiologic Studies Depression Scale in older Chinese: thresholds for long and short forms. International Journal of Geriatric Psychiatry. 2005;20:465–470. doi: 10.1002/gps.1314. [DOI] [PubMed] [Google Scholar]
- 29.Tsai PS, Wang SY, Wang MY, et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14:1943–52. doi: 10.1007/s11136-005-4346-x. [DOI] [PubMed] [Google Scholar]
- 30.Yu CL, Fielding R, Chan CL, et al. Measuring quality of life of Chinese cancer patients: A validation of the Chinese version of the Functional Assessment of Cancer Therapy-General (FACT-G) scale. Cancer. 2000;88:1715–27. [PubMed] [Google Scholar]
- 31.Mendoza T, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, Huber SL. The Rapid Assessment of Fatigue Severity in Cancer Patients: Use of the Brief Fatigue Inventory. Cancer. 1999;85:1186–96. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 32.Cella DF, Zagari MJ, Vandoros C, et al. Epoetin alfa treatment results in clinically significant improvements in quality of life in anemic cancer patients when referenced to the general population. J Clin Oncol. 2003;2:366–73. doi: 10.1200/JCO.2003.02.136. [DOI] [PubMed] [Google Scholar]
- 33.Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: a systematic review and meta-analysis. Biol Psychol. 2009;80:265–78. doi: 10.1016/j.biopsycho.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 34.Saville DJ. Multiple Comparison Procedures: The Practical Solution. The American Statistician. 1990;44:174–180. [Google Scholar]
- 35.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–6. [PubMed] [Google Scholar]
- 36.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 37.Chandwani KD, Thornton B, Perkins GH, et al. Yoga improves quality of life and benefit finding in women undergoing radiotherapy for breast cancer. J Soc Integr Oncol. 2010;8:43–55. [PubMed] [Google Scholar]