Abstract
Objectives
To describe the prevalence and pattern of traumatic experiences, to assess the prevalence of posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS), to identify risk factors for PTSD and PTSS, and to analyse the association of PTSD and PTSS with concomitant anxiety and depressive symptoms in women requesting induced abortion.
Methods
A Swedish multi-centre study of women requesting an induced abortion. The Screen Questionnaire – Posttraumatic Stress Disorder was used for research diagnoses of PTSD and PTSS. Anxiety and depressive symptoms were evaluated by the Hospital Anxiety and Depression Scale (HADS).
Results
Of the 1514 respondents, almost half reported traumatic experiences. Lifetime- and point prevalence of PTSD were 7% (95% confidence interval [CI]: 5.8–8.5) and 4% (95% CI: 3.1–5.2), respectively. The prevalence of PTSS was 23% (95% CI: 21.1–25.4). Women who reported symptoms of anxiety or depression when requesting abortion were more likely to have ongoing PTSD or PTSS. Also single-living women and smokers displayed higher rates of ongoing PTSD.
Conclusions
Although PTSD is rare among women who request an induced abortion, a relatively high proportion suffers from PTSS. Abortion seeking women with trauma experiences and existing or preexisting mental disorders need more consideration and alertness when counselled for termination.
Keywords: Abortion, Posttraumatic stress disorder, Posttraumatic stress, Depression, Anxiety
INTRODUCTION
Most women cope well with an induced abortion1 and the strongest predictor of mental health problems after induced abortion is the pre-existing mental health2–4. However, although induced abortion generally does not cause mental health problems2,5, the concern that it may has been raised repeatedly6.
Every fifth woman in the US who experiences a trauma will develop a posttraumatic stress disorder (PTSD), and the most common trauma exposures in women are rape and sexual molestation7. Lifetime population prevalence of PTSD in women is 7% and 10% in Sweden and the US, respectively7,8.
Pre-existing anxiety and depression disorders may increase the vulnerability to PTSD following a traumatic exposure9. Personality traits and an avoidant coping style are other factors that predispose for PTSD, and co-morbidities with major depression, anxiety disorders, social phobia and substance abuse are common4,9–11. For individuals who only partly meet the diagnostic criteria of the disorder, the terms sub-threshold PTSD, partial PTSD or posttraumatic stress symptoms (PTSS) have been used12. The relevance of sub-threshold PTSD has been discussed, particularly as a broadening of diagnostic criteria hypothetically could dissolve the border between disease and n ormal stress reactions13. However, sub-threshold PTSD is often exhibited by Vietnam veterans14, and since it is associated with impaired work and school functioning12,15, clinical attention is often required for it16.
Sexual abuse and intimate violence are exposures associated with mental health problems following abortion3. A new trauma may be a reminder of an earlier traumatic experience and trigger posttraumatic reactions16, and some researchers have suggested that abortion can function as a traumatic stressor capable of causing PTSD and PTSS17. Thus far, data regarding induced abortion and PTSD are few and yield imprecise estimates. A study by US researchers that compared American women with their Russian counterparts revealed that about 14% of the 217 American women and 1% of the 331 Russian women were diagnosed with PTSD, while posttraumatic reactions were present in 65% of the American women and 13% of the Russian women18. The large differences in prevalence rates between the two countries might be due to the cultural differences of the acceptance of abortion within each of these nations.
Together with positive feelings, emotional distress is part of the mix of contradictory emotions expressed by the majority of abortion-seeking women1. However, those with ongoing PTSD or PTSS are hypothetically a vulnerable group in need of targeted efforts during the abortion process. Hence, these are first results from a longitudinal study addressing PTSD and PTSS among women wanting to have an abortion. The paper describes the prevalence and pattern of traumatic experiences, assesses the prevalence of PTSD and PTSS, identifies risk factors for PTSD and PTSS and examines the association of PTSD and PTSS with concomitant anxiety and depressive symptoms among women seeking an induced abortion in clinics in Sweden.
MATERIALS AND METHODS
Between September 2009 and June 2010, a multi-centre study targeting women who requested an induced abortion was conducted at the outpatient clinics of the Departments of Obstetrics and Gynaecology of six public hospitals in Sweden. All those who requested an abortion before the end of the 12th week of gestation were approached for participation in the survey. They were informed about the study by research nurses or midwives, when registering for the first abortion visit. Women who agreed to participate received written information together with a questionnaire, coded with a study-specific ID number. They were asked to sign an informed consent form, and to fill out the questionnaire. Completed questionnaires were deposited in a locked mail-box. The only exclusion criterion for the study was inability to read and understand the questionnaire because of language difficulties.
Ethics
The study was approved by the Independent Research Ethics Committee at Uppsala University, dnr 2009/012.
Questionnaire
The questionnaire contained questions on socio- demographic variables including age, relationships, education, ethnicity, tobacco and alcohol use. In addition, the following research instruments were employed: the Screen Questionnaire – Posttraumatic Stress Disorder (SQ-PTSD) and the Hospital Anxiety and Depression Scale (HADS).
The SQ-PTSD is based on the diagnostic criteria for PTSD, according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV)8,19. The reliability, validity, sensitivity and specificity of the SQ-PTSD have been tested with satisfactory results8. Only women who met all DSM-IV criteria from A to F were classified as having a research diagnosis of PTSD. The criteria are: A1: confrontation with the stressor should involve actual or threatened death or serious injury, or a threat to the physical integrity of self or others; A2: the response to the confrontation should involve fear, helplessness or horror; B: persistent re-experiencing of the traumatic event in intrusive thoughts, nightmares or flashbacks; C: persistent avoidance of stimuli associated with the event and emotional numbing symptoms, described as an inability to experience any positive feelings such as love, contentment, satisfaction and happiness; D: hyper-arousal symptoms such as difficulties in sleeping, concentrating and controlling anger; E: duration of the disturbance (symptoms of criteria B, C, and D) for more than one month; and F: the disturbance causes clinically significant distress or impairment in social and occupational, or other important areas of functioning19. PTSS was defined as prevalence of A1 and A2 criteria together with one or more of the re-experiencing, avoidance or hyper arousal symptoms (B-C-D criteria). Controls were defined as women with neither PTSD nor PTSS.
The Hospital Anxiety and Depression scale (HADS) measures anxiety and depressive symptoms and contains seven items evaluating anxiety and seven more assessing depressive symptoms20. The instrument has been validated in several clinical populations with satisfactory results21 and for Swedish circumstances22. Depressive and anxiety symptoms are defined by the HADS questionnaire as: none (score 0–6), depressive mood/ mild or moderate anxiety (score 7–10), and risk for depression/possible anxiety disorder (score > 10)20.
Statistical analyses
In the sample size calculation a prevalence of 8.9% was assumed, based on a previous population-based study on prevalence of PTSD among women 20–39 years performed by Frans et al.8. We wanted the standard error (SE) of the two-sided 95% confidence interval (CI; calculated by use of the large sample normal approximation) for the prevalence not to exceed (±) 0.014. Simulations based on the above assumptions showed that if N = 1,500, the SE will exceed 0.014 with a probability of 0.12; i.e., the power was 0.88.
Socio-demographic data were classified accordingly: age groups, according to the Official Statistics of Induced Abortion in Sweden23, and duration of education, as less than 12 years (high school not completed) or 12 years or more. ‘Single living’ is defined as ‘not partnered’. Alcohol use was categorised as no use, moderate drinking or heavy drinking, where moderate drinking was defined as less than 1.5 bottles of wine (1 bottle of wine = 75cl) or seven beers (1 beer = 35cl) per week or the equivalent, and heavy drinking was defined as more than 1.5 bottles of wine or seven beers per week or the equivalent. Those limits are defined as hazardous alcohol use according to Alcohol Use Disorders Identification Test developed by WHO.
Country of birth was categorised into high-income countries and low- and middle-income countries and from that perspective classified into three groups: (i) Native-born Swede, (ii) EU-countries/Norway/Australia, (iii) Other countries; two non EU-countries that were part of the former Yugoslavia were categorised as low and middle-income countries alongside countries from Asia, Africa and South America. Anxiety and depressive scores on the HADS were dichotomised as none (0–7) or present (8–21), to clarify whether anxiety and depression symptoms were present or not.
The chi-square test was used to analyse the associations between socio-demographic factors and PTSD and PTSS, respectively. The 95% confidence intervals [CIs] for the lifetime- and point prevalence were calculated using the normal approximation. Logistic regression analyses were performed to assess the risk factors of PTSD, PTSS as well as the association of depressive and anxiety symptoms to PTSD. Dependent variables were PTSD and PTSS, respectively, and adjustments were made for socio-demographic variables that were significant in the bivariate analyses. The statistical software package IBM SPSS version 20 was used for all statistical analyses.
RESULTS
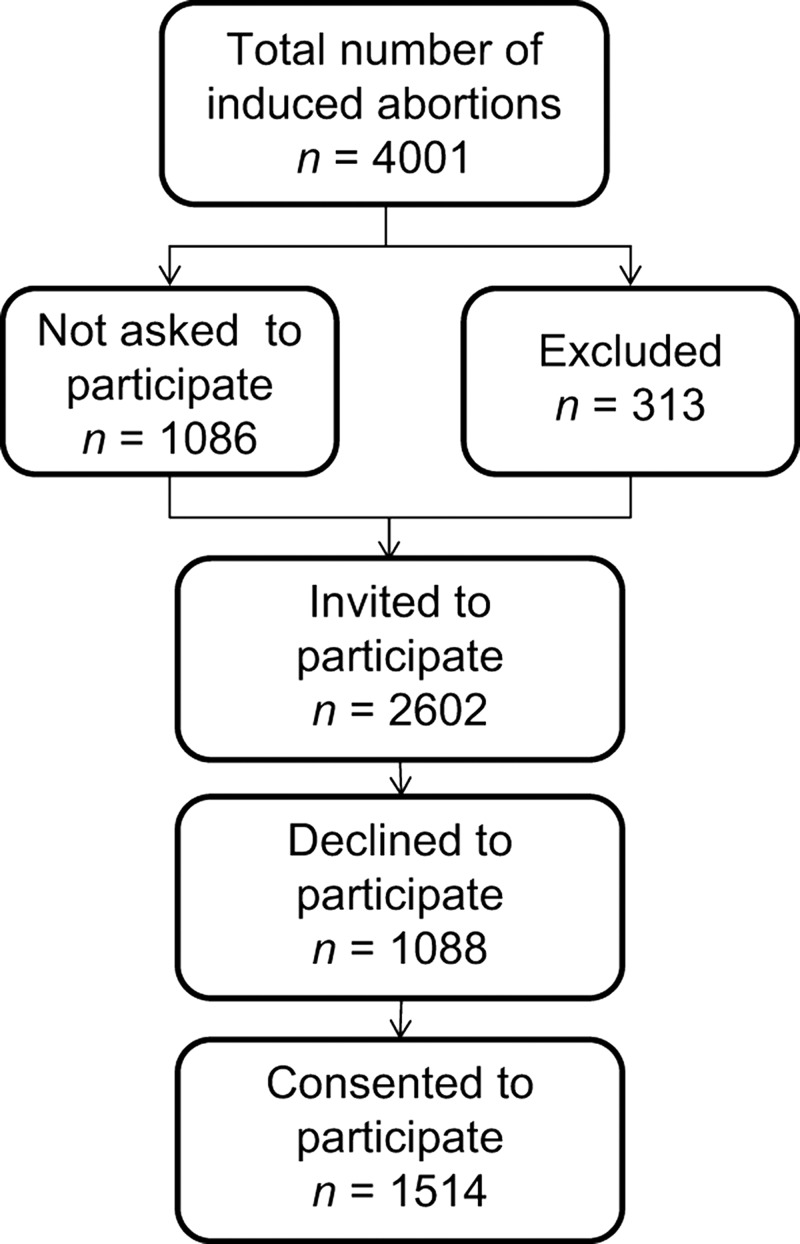
During the study period 4001 abortions were induced at the six out-patient clinics. Because the study inclusion depended on specific study personnel who were not always present, and because the patient-flow sometimes was too intense, 1086 women were never approached for the study. A total of 313 women were excluded, the reasons for exclusion reported by the clinics being: not mastering the Swedish language (n = 96), wishing to continue the pregnancy (n = 13), miscarriage (n = 14), and not pregnant (n = 11); for 179 of the women no reasons were disclosed by the clinics. In all, 2602 women were invited for participation and 1514 women consented and completed the questionnaire (overall response rate 58%; response rate per clinic 45–77%; Figure 1). Forty-four of these 1514 women had not filled out the entire SQ-PTSD, leaving 1470 women available for evaluation of PTSD or PTSS research diagnoses.
Figure 1.
Flowchart of the recruitment of patients during the study period.
Distribution across age groups differed significantly between responders and non-responders (p < 0.01; Table 1). Also, the age distribution of the study responders differed from the population-based Official Statistics of Induced Abortions in Sweden23 (p < 0.001). Both of these findings were driven by a lower proportion of women younger than 20 years among the responders (Table 1).
Table 1.
Women requesting induced abortion before the end of gestational week 12, age distribution between responders, non responders and the Official Statistics of Induced Abortion in Sweden23.
|
Responders
|
Non responders
|
Official Statistics of Induced Abortion in Sweden, year 2010
|
||||
|---|---|---|---|---|---|---|
| Age, years | n | % | n | % | n | % |
| < 19 | 140 | 9 | 152 | 14 | 5930 | 17 |
| 20–24 | 463 | 31 | 303 | 28 | 9438 | 27 |
| 25–29 | 350 | 23 | 231 | 21 | 7025 | 20 |
| 30–34 | 238 | 16 | 177 | 16 | 5678 | 16 |
| 35–39 | 187 | 12 | 139 | 13 | 4675 | 13 |
| > 40 | 136 | 9 | 86 | 8 | 2350 | 7 |
| Total | 1514 | 100 | 1088 | 100 | 35,096 | 100 |
Of the participants, 92% were born in Sweden and 5% were born outside Europe. Age varied from 15 to 52 years, with a mean age of 28 years and a median age of 27 years. The overall prevalence of prior trauma was 41%, and as many as 4% had experience of war. Having been subjected to severe physical threat, psychological threat and severe physical injury were the most commonly reported trauma experiences. In addition, 12% and 18% of women had experiences of sexual assault and robbery, respectively (Table 2).
Table 2.
Reported trauma experiences among women requesting induced abortion (N = 1514).
| n | % | |
|---|---|---|
| Self-experience or witness of severe physical threat | 659 | 43 |
| Self-experience or witness of severe psychological threat | 588 | 39 |
| Self-experience or witness of severe physical injury | 544 | 36 |
| Self-experience or witness of a traffic accident | 370 | 24 |
| Self-experience or witness of death threat | 366 | 24 |
| Death of a relative or close friend by accident, homicide or suicide | 332 | 22 |
| Robbery | 275 | 18 |
| Sexual assault | 183 | 12 |
| War | 61 | 4 |
Multiple responses possible, frequencies reported for each item.
Lifetime- and point prevalence of PTSD were 104 (7%; 95% CI: 5.8–8.5) and 60 (4%; 95% CI: 3.1–5.2), respectively. The overall reporting of PTSS was 340 (23%; 95% CI: 21.1–25.4). Rates of ongoing PTSD and PTSS did not differ between the participating clinics (5–9% and 15–28%, respectively). Most women with PTSD had concomitant anxiety (90%) and depressive symptoms (76%), but also those with PTSS displayed much higher rates of anxiety (60%) and depressive symptoms (38%) than controls (Table 3).
Table 3.
Associations between socio-demographic factors, anxiety and depressive symptoms and on-going posttraumatic stress disorder (PTSD), point prevalence, as well as posttraumatic stress symptoms (PTSS) among women requesting abortion.
|
Ongoing PTSD (n = 60)
|
PTSS (n = 340)
|
Controls (n = 1026)
|
||||||
|---|---|---|---|---|---|---|---|---|
| n | % | p-value | n | % | p-value | n | % | |
| Age | ||||||||
| < 19 years | 7 | 12 | < 0.05 | 37 | 11 | 0.3 | 89 | 9 |
| 20–24 years | 23 | 38 | 101 | 30 | 301 | 29 | ||
| 25–34 years | 26 | 43 | 137 | 40 | 392 | 38 | ||
| > 35 years | 4 | 7 | 65 | 19 | 244 | 24 | ||
| Education | ||||||||
| < 12 years | 45 | 76 | 0.2 | 250 | 74 | < 0.05 | 688 | 67 |
| > 12 years | 14 | 24 | 88 | 26 | 332 | 32 | ||
| Cohabiting | 36 | 62 | < 0.05 | 237 | 73 | 0.8 | 734 | 74 |
| Smoking | 31 | 52 | < 0.001 | 103 | 30 | 0.5 | 291 | 29 |
| Snuff use | 8 | 15 | 0.3 | 44 | 14 | 0.2 | 112 | 10 |
| Alcohol | ||||||||
| No | 22 | 37 | < 0.001 | 73 | 21 | 0.5 | 195 | 19 |
| Moderate drinking | 33 | 56 | 255 | 75 | 801 | 78 | ||
| Heavy drinking | 4 | 7 | 11 | 3 | 27 | 3 | ||
| Anxiety symptoms | 53 | 90 | < 0.001 | 199 | 60 | < 0.001 | 343 | 34 |
| Depressive symptoms | 45 | 76 | < 0.001 | 127 | 38 | < 0.001 | 259 | 25 |
| Country | ||||||||
| Sweden | 52 | 87 | 0.3 | 309 | 91 | 0.8 | 939 | 92 |
| European countries, Australia | 2 | 3 | 4 | 1 | 15 | 1 | ||
| Other countries | 6 | 10 | 25 | 7 | 65 | 6 | ||
Anxiety and depressive symptoms according to HADS. Frequencies are reported according to number of responders for each item.
p-values refer to the comparison with the control group, Chi-square test.
In Table 3 the association between socio- demographic factors, anxiety and depressive symptoms, and ongoing PTSD as well as PTSS, are displayed. Women who were living with their partner (62%; p < 0.05), who were smokers (52%; p < 0.001), used no alcohol (37%; p < 0.001) or were heavy drinkers (7%; p < 0.001) displayed higher rates of ongoing PTSD, whereas women with PTSS more often had a low level of education (74%, p < 0.05). In addition, women who reported high levels of anxiety or depression at the time of the induced abortion were also more likely to fulfil criteria for ongoing PTSD or PTSS. In the multivariate regression model, anxiety and depressive symptoms, smoking and no alcohol use remained significantly associated with PTSD. PTSS was significantly associated with anxiety symptoms and low educational level, following adjustment for socio-demographic variables (Table 4).
Table 4.
The association between socio-demographic factors, posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) among women requesting abortion.
| OR | 95% CI | p-value | |
|---|---|---|---|
| Ongoing PTSD (n = 60) | |||
| Anxiety symptoms | 8.1 | 2.9–22.2 | < 0.001 |
| Depressive symptoms | 4.1 | 2.0–8.5 | < 0.001 |
| Smoking | 2.4 | 1.3–4.4 | < 0.001 |
| Alcohol | |||
| Moderate drinking | 1 | ||
| No | 2.1 | 1.1–4.0 | < 0.05 |
| Heavy drinking | 1.8 | 0.5–6.4 | 0.4 |
| PTSS (n = 340) | |||
| Anxiety symptoms | 2.8 | 2.1–3.8 | < 0.001 |
| Education | |||
| > 12 years | 1 | ||
| < 12 years | 1.41 | 1.06–1.9 | < 0.05 |
OR, odds ratio; CI, confidence interval. All socio-demographic variables in Table 4 were considered and those with significant regression coefficients were entered in the model. Only significant associations in the multivariate model are presented in the table. Anxiety and depression symptoms according to the Hospital Anxiety and Depression Scale (HADS).
DISCUSSION
Findings
The main findings of the study were that women who requested an induced abortion had a point prevalence of PTSD and PTSS of 4% and 23%, respectively. Women with PTSD or PTSS displayed higher rates of anxiety and depressive symptoms than controls.
Strengths and weaknesses of the study
The study is strengthened by the use of standardised and validated instruments, the size of the study population, and the multi-centre nationwide design. The major limitation of our study was the relatively low response rate (58%). One explanation could be the practical aspects of the recruitment process, where women were asked to fill out the questionnaire at the clinic. Some women might have been under a time constraint or felt too stressed by the overall situation of requesting an abortion. Another reason for this outcome was the substantial variation in response rate by clinic due to factors such as continuity of field supervision and organisation of the recruitment at each site. The best response rates were obtained at the hospitals where only one study coordinator was responsible for the recruitment.
The prevalence of PTSD and PTSS was, however, similar between sites. The non-responders were characterised by a different age distribution, with a higher proportion of women under 20 years. Previous analyses of drop-outs in abortion studies have suggested that non-responders are younger, have a lower level of education and more often live alone than responders24. As all of these factors are of importance for PTSD, it is thus possible that the prevalence of the disorder is underestimated in this study.
Differences in results and conclusions in relation to other studies
The lifetime prevalence of PSTD of 7% in this study is the same as in the general female population (7%). The corresponding figure for Swedish women, aged 20–39 years, is 9% (reanalysed prevalence rates)8. By comparison, the US population-based prevalence rate of lifetime PTSD in women is 10%, and by age-group the corresponding rates are 16%, 10% and 5% in women aged 15–24 years, 25–34 years and 35–44 years, respectively7.
In line with previous studies, we found that young age, single living, smoking, and heavy drinking were associated with a higher risk of PTSD, at least in the bivariate analyses7,8,25,26. Previous studies have suggested a declining PTSD prevalence with advancing age8, and that was similar to our finding that women aged 35 years or more had a lower prevalence of PTSD compared to those who were younger.
Smoking rates are high among individuals with PTSD25. Studies imply that smoking reduces negative affect, thus individuals who meet the criteria for PTSD may be more likely to smoke for this reason25–27. The Swedish National Board of Health and Welfare28 has reported a decrease of smoking among Swedish women, except in groups with a low level of education. Women with limited education and smokers are overrepresented among women seeking abortion and they more often display symptoms of emotional distress29,30. Tobacco use and a low level of education are also risk factors for repeat abortions31. In Sweden, both a low educational background and smoking are strongly linked to low socio-economic status28.
Heavy drinking was also associated with PTSD in the bivariate analysis, which is consistent with earlier findings that alcohol and substance abuse often are co-morbid with PTSD7. Nevertheless, an even higher percentage (37%) of women with PTSD reported no alcohol use. No reasonable explanation for the association between PTSD and alcohol abstinence has been found, but reasons for not consuming alcohol could be a wish for self-control, negative experiences of alcohol use in the family, medication with antidepressants, religious beliefs or a goal of being healthy. Furthermore, alcohol use may also be underreported due to the design of the question, where only three response alternatives were given.
Anxiety and depressive symptoms were common among women with PTSD, far more so than in those not having PTSD or PTSS, i.e., beyond normal negative feelings reported by abortion seeking women1. Psychiatric co-morbidity is often observed in PTSD7,32, with the most frequent disorders being major depression and generalised anxiety disorder, followed by alcohol abuse or dependence32. Earlier findings suggested that ethnicity may be a risk factor for PTSD as those born abroad may have had a higher exposure to traumatic events8. The present study did not confirm any association with ethnicity, but we did note that 4% of the women in the study had experiences of war. Although more than half of the latter were born in Sweden, it is reasonable to assume that some of these had visited war zones in their parents’ countries.
Traumatic experiences were common in the study population. Nearly half of the women reported trauma experience of severe physical threat and 12% had experience of sexual violence or threats. The high rate of trauma exposure in this survey is in line with what has been found in earlier studies8,33,34: exposure to violence appears to be more prevalent in women who seek an abortion than among those who choose to give birth4.
Relevance of the findings: Implications for clinicians and policy makers
PTSS was more common than PTSD in our population, with an estimated prevalence of 23%. While these women did not fulfil criteria for PTSD, a great proportion of them had co-morbid depressive and anxiety symptoms. Anxiety and depressive symptoms, smoking and alcohol abstinence were associated with a risk for PTSD, whereas PTSS was significantly associated with anxiety symptoms and low educational level. The results indicate that women who are asking for an induced abortion should be questioned about the aforementioned risk factors and subjects presenting these risk factors should be counselled about stress symptoms and related management. From a clinical point of view, it is possible that women with PTSS are as susceptible as those with PTSD to trauma events after an abortion.
Unanswered questions and future research
Further studies are needed to address possible long-term consequences of PTSD/PTSS in abortion care. In addition, future research should clarify and compare the mental well-being, including PTSD and PTSS, of the women who already had an induced abortion with that of those who are planning to have an induced abortion. Results of studies of PTSD following a traumatic experience at childbirth demonstrate, among other factors, an association with low levels of support from staff and partners, intolerable pain, and unanticipated complications35–39. So far, this has not been addressed in longitudinal studies of abortion care.
CONCLUSION
Although PTSD is rare (7%) among women who request an induced abortion, a relatively high proportion (23%) suffers from PTSS. Women who seek abortions who have had trauma experiences in the past and/or have had symptoms of mental distress need more consideration and alertness from the medical personnel when they are counselled for termination.
Acknowledgments
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and the writing of the paper.
Funding for this project was provided by the Marianne and Marcus Wallenberg Foundation, the Medical Faculty of Uppsala Universities, the Family Planning Foundation at Uppsala University, the Regional Research Committees of Uppsala and Örebro Counties Councils, and the Sophiahemmet Foundation.
REFERENCES
- 1.Kero A, Hogberg U, Lalos A. Wellbeing and mental growth – long-term effects of legal abortion. Soc Sci Med. 2004;58:2559–69. doi: 10.1016/j.socscimed.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Munk-Olsen T, Munk Laursen T, Pedersen CB, et al. Induced first-trimester abortion and risk of mental disorder. N Engl J Med. 2011;364:332–9. doi: 10.1056/NEJMoa0905882. [DOI] [PubMed] [Google Scholar]
- 3.Robinson GE, Stotland NL, Russo NF, et al. Is there an ‘abortion trauma syndrome’? Critiquing the evidence. Harv Rev Psychiatry. 2009;17:268–90. doi: 10.1080/10673220903149119. [DOI] [PubMed] [Google Scholar]
- 4.Steinberg J, Russo NF. Abortion and anxiety: What's the relationship? Soc Sci Med. 2008;67:238–52. doi: 10.1016/j.socscimed.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 5.Pedersen W. Abortion and depression: A population-based longitudinal study of young women. Scand J Publ Health. 2008;36:424–8. doi: 10.1177/1403494807088449. [DOI] [PubMed] [Google Scholar]
- 6.Major B, Appelbaum B, Beckman L, et al. Report of the APA Task Force on Mental Health and Abortion: American Psychological Association 2008. http://www.en.federa.org.pl/dokumenty_pdf/podrzednegora/abortion-report.pdf [Google Scholar]
- 7.Kessler R, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 8.Frans Ö, Rimmo PA, Aberg L, Fredrikson M. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatr Scand. 2005;111:291–9. doi: 10.1111/j.1600-0447.2004.00463.x. [DOI] [PubMed] [Google Scholar]
- 9.Breslau N, Davis GC, Peterson EL, Schultz L. Psychiatric sequelae of posttraumatic stress disorder in women. Arch Gen Psychiatry. 1997;54:81–7. doi: 10.1001/archpsyc.1997.01830130087016. [DOI] [PubMed] [Google Scholar]
- 10.Chung MC, Easthope Y, Farmer S, et al. Psychological sequelae: Post-traumatic stress reactions and personality factors among community residents as secondary victims. Scand J Caring Sci. 2003;17:265–70. doi: 10.1046/j.1471-6712.2003.00224.x. [DOI] [PubMed] [Google Scholar]
- 11.Willebrand M, Andersson G, Ekselius L. Prediction of psychological health after an accidental burn. J Trauma. 2004;57:367–74. doi: 10.1097/01.ta.0000078697.69530.0e. [DOI] [PubMed] [Google Scholar]
- 12.Breslau N, Lucia VC, Davis GC. Partial PTSD versus full PTSD: An empirical examination of associated impairment. Psychol Med. 2004;34:1205–14. doi: 10.1017/s0033291704002594. [DOI] [PubMed] [Google Scholar]
- 13.McNally RJ. Progress and controversy in the study of posttraumatic stress disorder. Annu Rev Psychol. 2003;54:229–52. doi: 10.1146/annurev.psych.54.101601.145112. [DOI] [PubMed] [Google Scholar]
- 14.Weiss DS, Marmar CR, Schlenger WE, et al. The prevalence of lifetime and partial post-traumatic stress disorder in Vietnam theater veterans. J Traumatic Stress. 1992;5:365–76. [Google Scholar]
- 15.Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry. 1997;154:1114–9. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- 16.Friedman MJ, Keane T M, Resick PA. Science and practice. New York: The Guilford Press; 2007. Handbook of PTSD. [Google Scholar]
- 17.Speckhard AC, Rue VM. Postabortion syndrome: An emerging public health concern. J Soc Issues. 1992;48:95–119. [Google Scholar]
- 18.Rue V, Coleman PK, Rue JJ, Reardon DC. Induced abortion and traumatic stress: A preliminary comparison of American and Russian women. Med Sci Monit. 2004;10:SR516. [PubMed] [Google Scholar]
- 19.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th edn. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 20.Zigmond A, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 21.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 22.Lisspers J, Nygren A, Soderman E. Hospital Anxiety and Depression Scale (HAD): Some psychometric data for a Swedish sample. Acta Psychiatr Scand. 1997;96:281–6. doi: 10.1111/j.1600-0447.1997.tb10164.x. [DOI] [PubMed] [Google Scholar]
- 23.The Swedish National Board of Health and Welfare. Statistics – Health and Medical Care. Socialstyrelsen/Official Statistics of Sweden 2010. Induced abortions 2010. http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/18330/2011-6-1.pdf
- 24.Soderberg H, Andersson C, Janzon L, Sjoberg NO. Selection bias in a study on how women experienced induced abortion. Eur J Obstet Gynecol Reprod Biol. 1998;77:67–70. doi: 10.1016/s0301-2115(97)00223-6. [DOI] [PubMed] [Google Scholar]
- 25.Feldner MT, Babson KA, Zvolensky MJ. Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clin Psychol Rev. 2007;27:14–45. doi: 10.1016/j.cpr.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feldner MT, Babson KA, Zvolensky MJ, et al. Posttraumatic stress symptoms and smoking to reduce negative affect: an investigation of trauma-exposed daily smokers. Addict Behav. 2007;32:214–27. doi: 10.1016/j.addbeh.2006.03.032. [DOI] [PubMed] [Google Scholar]
- 27.Marshall EC, Zvolensky MJ, Vujanovic AA, et al. Evaluation of smoking characteristics among community-recruited daily smokers with and without posttraumatic stress disorder and panic psychopathology. J Anxiety Disord. 2008;22:1214–26. doi: 10.1016/j.janxdis.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The Swedish National Board of Healthand Welfare. Folkhälsorapport: Socialstyrelsen, Stockholm, 2009. http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/ 8495/2009-126-71_200912671.pdf
- 29.Larsson M, Aneblom G, Odlind V, Tyden T. Reasons for pregnancy termination, contraceptive habits and contraceptive failure among Swedish women requesting an early pregnancy termination. Acta Obstet Gynecol Scand. 2002;81:64–71. doi: 10.1046/j.0001-6349.2001.00169.x. [DOI] [PubMed] [Google Scholar]
- 30.Söderberg H, Janzon L, Sjöberg N-O. Emotional distress following induced abortion: A study of its incidence and determinants among abortees in Malmö, Sweden. Eur J Obstet Gynecol Reprod Biol. 1998;79:173–78. doi: 10.1016/s0301-2115(98)00084-0. [DOI] [PubMed] [Google Scholar]
- 31.Makenzius M, Tyden T, Darj E, Larsson M. Repeat induced abortion – a matter of individual behaviour or societal factors? A cross-sectional study among Swedish women. Eur J Contracept Reprod Health Care. 2011;16:369–77. doi: 10.3109/13625187.2011.595520. [DOI] [PubMed] [Google Scholar]
- 32.Brown TA, Campbell LA, Lehman CL, et al. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol. 2001;110:585–99. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- 33.Meltzer-Brody S, Hartmann K, Miller WC, et al. A brief screening instrument to detect posttraumatic stress disorder in outpatient gynecology. Obstet Gynecol. 2004;104:770–6. doi: 10.1097/01.AOG.0000140683.43272.85. [DOI] [PubMed] [Google Scholar]
- 34.Söderquist J, Wijma B, Thorbert G, Wijma K. Risk factors in pregnancy for post-traumatic stress and depression after childbirth. BJOG. 2009;116:672–80. doi: 10.1111/j.1471-0528.2008.02083.x. [DOI] [PubMed] [Google Scholar]
- 35.Czarnocka J, Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol. 2000;39:35–51. doi: 10.1348/014466500163095. [DOI] [PubMed] [Google Scholar]
- 36.Ayers S, Pickering AD. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth. 2001;28:111–8. doi: 10.1046/j.1523-536x.2001.00111.x. [DOI] [PubMed] [Google Scholar]
- 37.Stramrood CA, Paarlberg KM, Huis In 't Veld EM, et al. Posttraumatic stress following childbirth in homelike- and hospital settings. J Psychosom Obstet Gynaecol. 2011;32:88–97. doi: 10.3109/0167482X.2011.569801. [DOI] [PubMed] [Google Scholar]
- 38.Soderquist J, Wijma K, Wijma B. Traumatic stress after childbirth: The role of obstetric variables. J Psychosom Obstet Gynaecol. 2002;23:31–9. doi: 10.3109/01674820209093413. [DOI] [PubMed] [Google Scholar]
- 39.Olde E, van der Hart O, Kleber R, van Son M. Posttraumatic stress following childbirth: A review. Clin Psychol Rev. 2006;26:1–16. doi: 10.1016/j.cpr.2005.07.002. [DOI] [PubMed] [Google Scholar]