Abstract
Background
The purpose of this study was to evaluate the use of short dental implants in distally reduced alveolar bone height.
Material/Methods
MedLine (PubMed and Ovid), ISI Web of Knowledge, and Cochrane databases were used for analysis. Searching was conducted using the search equation: ‘Dental Implants’ [Majr] AND (Short[TIAB] OR Shorter[TIAB]) AND (Implant[TIAB] OR Implants[TIAB]). Abstracts were screened by 2 independent reviewers. The articles included in the analysis were published in the English language and reported data on the use of implants with lengths below 10 mm in the posterior region with reduced alveolar bone height making the placement of longer implants impossible without additional surgical interventions. Articles concerning data on orthodontic implants and post-resection surgery reconstruction were excluded from analysis. Any disagreements between the 2 reviewers were resolved by a third reviewer. No time frame was used.
Results
Of the 791 articles initially found, automatic rejection of duplicates in the Endnotes X5 software resulted in 538 articles. After the selection of studies from databases, a bibliography of 32 eligible articles was searched for other publications. Through this method, 2 more studies were added.
Conclusions
The analysis of the results of different studies on the use of short dental implants showed that this treatment could be effective and comparable to the use of standard-length implants. This study revealed that rough-surfaced implants with lengths between 6–10 mm placed in the posterior mandible are the preferred solution. However, more detailed data will require additional prospective studies.
Keywords: dental implants, implant placement, prosthetic rehabilitation, success rate, survival rate, jaw, edentulous, partially/rehabilitation
Background
The use of implants and the development of surgical techniques enabling the reconstruction of reduced alveolar bone height have become a standard treatment. On the one hand, these techniques have introduced new indications to the use of implants; on the other hand, they increased the risk of complications. Nevertheless, any intervention on the bone, such as the above standard preparation for implant placement, can generate both short- and long-term complications.
These observations have led to suggestions to replace regeneration techniques with less complicated procedures that would eliminate the need for additional interventions [1]. Therefore, the aim of this study was a critical review of the literature on the use of short dental implants in distally reduced alveolar bone height as an alternative to the augmentation procedure.
Material and Methods
On April 9, 2013, MEDLINE (PubMed), MEDLINE(Ovid), ISI Web of Knowledge, and Cochrane databases were searched using the search equation: ‘Dental Implants’ [Majr] AND (Short[TIAB] OR Shorter[TIAB]) AND (Implant[TIAB] OR Implants[TIAB]). Abstracts were screened by 2 independent reviewers. The articles included in the analysis were published in the English language and reported data on the use of implants with lengths ≤10 mm in the posterior region with reduced alveolar bone height making the placement of longer implants impossible without additional surgical procedures. The articles concerning data on the use of orthodontic implants and post-resection surgery reconstruction were excluded from analysis. Any disagreements between the 2 screening reviewers were resolved by a third reviewer. No time frame was used.
To give a comprehensive topic overview, the included articles were divided into 2 categories: treatment results and factors influencing the efficacy of treatment.
Results
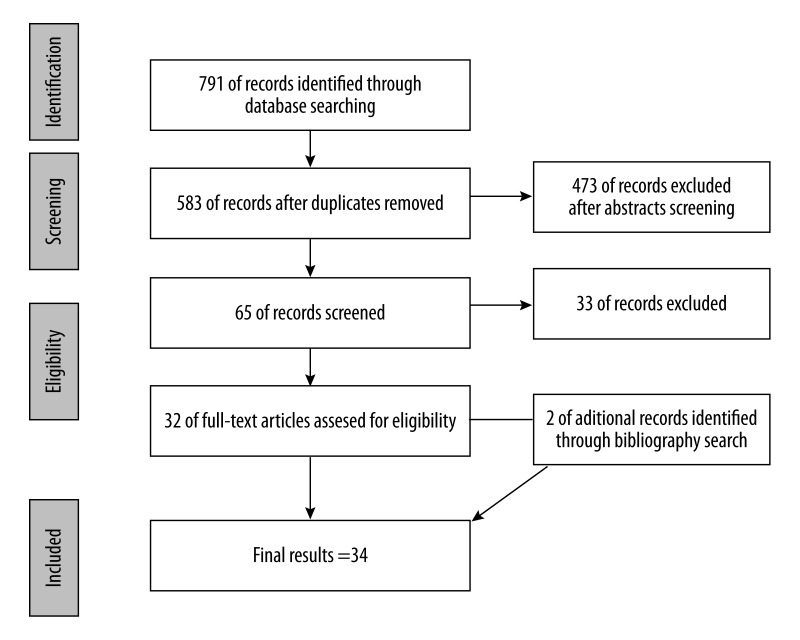
Of the 791 articles initially found, the automatic rejection of duplicates in Endnotes X5 software resulted in 538 articles. After a selection of studies from databases, a bibliography of 32 eligible articles was searched for other publications. Through this method, 2 more studies were added. The selection scheme is presented in a PRISMA flow diagram (Figure 1). Nineteen articles (56%) were included in the “treatment results” category, while the remaining 15 (44%) in were included in the “factors influencing treatment results” category.
Figure 1.
PRISMA flow diagram.
Definition of Short Implants and Indications for Their Use
The term ‘short implant’ is subjective. In most publications this is defined as an implant length between 5 and 10 mm. The first implants of this type and length of 7 mm were introduced in 1979 by the Bränemark system. Today, most implantology companies offer implants shorter than 8 mm, which has led to their common use in clinically substantiated cases.
The use of shorter implants is indicated in the lateral parts of the maxilla and the mandible. These regions are the most predisposed to atrophy because first molars are the first teeth lost [2] in most cases. After their extraction, the atrophy of bone surface develops in 30–90% of cases. The process depends on the time from the tooth extraction and coexisting pathological factors. The extraction of molars can also be the cause of further negative processes such as the mesial inclination of second molars towards the hole, which generates improper occlusal loading, leading to local bone atrophy.
It has been found that the extraction of upper teeth (particularly molars) leads to increased volume of the maxillary sinus and, in consequence, to bone atrophy beginning from the sinus surface. It is assumed that the air pressure inside the sinus and features of the mucosa that lines the sinus play important roles in this process. It has been found that in cases of Caldwell-Luc mucosectomy of the sinus due to infection, in frequent cases, the sinus was destroyed and this significant atrophy of the alveolar process was not even observed [3]. Time from extraction, age, sex, genetic predispositions, periodontal disease, and the use of dentures may also influence the degree of bone atrophy [4,5]. Additionally, the localization of the inferior alveolar nerve can also limit the potential of implantological treatment in the mandible.
Oikarinen et al. conducted a radiographic study in a population of 431 65-year-olds, it was found that the placement of an implant of at least 6 mm length was possible in the lateral part of maxilla only in 38% of cases and in only 50% of mandible cases [6] in the lateral zone. Therefore, the aim of this study was to summarize and review the possibilities for the use of short dental implants in distally reduced alveolar bone height.
Treatment Results
Thirteen clinical studies [7–19] and 6 review-type articles [20–25] fulfill inclusion criteria.
Clinical studies
To give a comprehensive overview of clinical results, the US Task Force evidence classification level was applied (Table 1). Two articles [7,8] were controlled trials (1 randomized), 9 were retrospective cohort studies, and 2 were case series. Therefore, only 2 articles [7,8] had a sufficient level of evidence to be the basis of clinical decisions.
Table 1.
US preventive services task forces hierarchy of research design.
| Level of evidence | Study design | % of clinical studies | No of articles | Bibliography numbers |
|---|---|---|---|---|
| I: | Rrandomized controlled trial | 8% | n=1 | [7] |
| II-1: | Controlled trials without randomization | 8% | n=1 | [8] |
| II-2: | Cohort or case-controlled studies | 69% | n=9 | [10–12,14–19] |
| II-3: | Case series | 15% | n=2 | [9,13] |
| III: | Case reports, opinions of authorities | 0% | n=0 |
The total number of short implants placed in the posterior region across/in all studies was 5643, from which 108 were prospectively examined. Follow-up ranged from 1 to 8 years. From individual studies, information about location, surface, and implant length were also collected (Table 2).
Table 2.
Treatment results.
| Article | Number of implants | Lenght and/or surface of implants | Follow up | Success rate % |
|---|---|---|---|---|
| Esposito [7] | 60 | 5 mm | <1 y | Not applicable |
| Deporter [8] | 48 | 7; 9 mm/rough | <50.3 m, mean 32.6 m | 100% |
| Deporter [9] | 26 | 5 mm | 1–8 y | 83.7%mx 100%md |
| Sanchez-Garces [10] | 273 | ≤10 mm/154 machined, 119 rough | 1.8–12 y | 92.67% |
| Fugazzotto [11] | 2073 | <10 mm | ≤84 m | 99.2% |
| Bruggenkate [12] | 253 (42mx/146md) | 6 mm/plasma sprayed | 1–7 y | 97% |
| Misch [13] | 745 | 7 and 9 mm | 1–5 y | 98.9% |
| Malo [14] | 409 (130mx/278md) | 7 mm; 8,5 mm/272 machined, 136 TiUnte | <5 y | 96.2% – 7mm 97.1% – 8.5 mm |
| Testori [15] | 405/158-short (282mx/123md) | 7; 8.5 and 10 mm | 3 y | 98.9% 97.5% |
| Renouard [16] | 96 | 6 and 8.5 mm/54 machined, 42 TiUnite | >2 y, average 37.6 m | 94.6% |
| Griffin [17] | 168 (89mx/79md) | 8 mm/rough | ≤68 m, mean 34.9 | 100% |
| Anitua [18] | 1287 (570mx/717md) | <8.5 mm | 1–8 y | 98.8% |
| Romeo [19] | 265 | 8; 10 mm/rough | 3–14 y | 97.9% – 8mm 97.1% – 10mm |
m – month; y – year; mx – maxilla; md – mandible.
The success rate ranged from 83.7% to 100%. Nine of the 13 studies reported a success rate above 95%. The lowest success rate was reported by Deporter [9] (83.7%) using 5-mm sintered porous-surfaced implants in posterior maxilla. Sanchez-Garces [10] found the highest failure rate for machined-surface implants (8.4%) compared to rough-surfaced (5.9%) implants. Renouard [11] reported a 94.6% success rate and results from the randomized clinical trial performed by Eposito [7] were not applicable.
From major studies we found that a greater overall success rate was achieved in the mandible [9–14] rather than in the maxilla [15], with a rough [10,14,16] rather than machined surface.
A length of 5 mm seems to be crucial to the outcome due to the highest failure rate being reported using these 5-mm implants. The follow-up period length did not influence the success rate across studies.
Review articles
Of 5 review articles, 1 was a meta-analysis [20]. Despite many existing articles on the topic of short implants in which reviews were included the analysis, one common finding accompanied all conclusions: “more scientific evidence is needed”. There are 2 reasons presented for this statement: lack of consistency in the study designs and the low number of prospective studies (high level of evidence). However, the major clinical findings across all of the articles were similar. Sun [21] reported that most (57.9%) failures occurred before prosthesis connection, finding a tendency toward higher failure rates for the maxilla- and machined-surfaced implants compared with the mandible and rough surface. No statistically significant difference between the failure rates of short and standard length implants or between implants placed in single-stage and 2-stage procedures were obtained. In a review by Annibali et al. [22], a 99.1% cumulative survival rate was reported. Similarly, Pommer found a difference between rough- and machine-surfaced implants of 99.5%/97.2% [23], respectively. The only meta-analysis showed cumulative success rates of 92.5% and 98.42% for machined- and rough-surface implants, respectively. Neldam [24] confirmed these findings and showed a general pattern of implant losses concentrated during the healing phase. Hagi [25] observed that surface geometry plays a role in performance of dental implants of 7 mm length or less and reported that threaded implants had higher failure rates compared to press-fit (non-threaded) shaped and sintered porous implants.
Factors Influencing Treatment Results
Initially, short implants were considered biomechanically unsuitable and their use was seen as simply experimental. However, finite element analysis performed by Pierrisnard et al. [26] showed that maximum stress in the implant area was largely independent of implant length. Experimental studies on animal models confirmed that the increase of implant length from 7 mm to 10 mm did not significantly improve implant anchorage in the bone [27].
Short implants not only distribute stress similarly, but also because of their length may be used in reduced bone conditions for supporting distally extended cantilever, which could reduce compressive and tensile stress by 34.7% and 19%, respectively [28].
More favourable force distribution could also be obtained by crown interlocking, in which the forces transferred to the bone are reduced because they are absorbed by prostheses, cement, or abutment screws. Yang [29] showed that the usage of two 7-mm implants decreases the strain caused by the use of the oblique force in the same degree as the connection of two 12-mm implants. Splinted implants increase functional surface area and compensate for lower bone density.
An important biomechanical rule states that in case of 2 materials with different modules of elasticity and with only 1 of them being loaded, the highest stress is found at the area of contact of these 2 materials [30]. For an implant placed in the bone, the highest stress is found in the first 5 mm, starting from the implant bearing surface, which usually covers the first 3–5 threads or more if this part of the implant has microthreads [31]. Studies showed that the surface of the implant contacting with cortical bone was the most exposed to forces triggered with mastication, and very little stress was transferred to the apical portion of the implant [32]. This data suggests that the bone area around the first 3–5 mm of the implant is the most predisposed to atrophy. The results of the studies led to an improvement in the functional part of the implant structure, transferring compressive and tensile load stress to the bone. Modifications were made, mainly involving changes in the shape of threads. The number, depth, and distances between the threads were adjusted for different bone parameters. The increased number of threads and thread depth lead to a widened implant surface at a given length and diameter of the implant.
Mistakes made during the prosthetic phase are one of the many causes of treatment failure. In a literature analysis, Das Neves et al. [33] found that 45.1% of implant failures occurred after loading, but if the first year of loading was also considered, the failure rate increased to 63.2%. In 27.2% of cases the main reason was occlusal overload.
Unfavorable crown-to-implant length ratio (C/I ratio) is one of the main factors that discourages many clinicians from the use of short implants. However, this factor only plays an important role in natural teeth, which results from another fixation of the tooth compared to a stiff implant anchorage in the bone. Tawil [34] suggests that even if the crown-to-implant ratio increased by 2–3-fold, it would not increase the biomechanical risk of implant loss and found no correlation between bone loss in the implant area and the action of occlusive forces. He concluded that the implant length should not determine the height of the prosthetic crown, but one should try to eliminate negative forces that develop due to the unfavorable crown-to-implant length ratio.
Blanes [35] analyzed 2 publications on the influence of crown-to-implant ratio and found that in cases in which C/I ratio was ≥2, the survival rate of implants was 94.1%. In both articles, there was no negative effect on bone loss in the peri-implant area. Similar results were obtained by Birdi et al/[36], who did not find a significant relationship between the increased C/I ratio and the degree of bone loss measured mesially and distally in short implants.
Bidez and Misch [37] evaluated the effect on the implant and its relationship with the height of the prosthetic crown. If the crown height is increased from 10 mm to 20 mm, the force on the implant is increased by 100%. Therefore, it seems logical to place 2 implants on the ends of any planned prosthesis.
According to Nedir [38] and Malo [14], it is unproven that factors such as crown to implant ratio, splinting, the length of cantilever, occlusal surface pattern, the type of implant system, the type of dentition in the opposing arch and bruxism influenced the outcome of any treatment. In prosthetic reconstruction, excluding biomechanical factors, it is very important to restore adequate biological width and to provide a 1–2 mm space for connective tissue [39,40].
Conclusions
Analysis of the results from different studies on the use of short implants suggests that the optimization of surface from machined to rough provides a higher survival rate. Adequate prosthetic interventions have led to an improvement in clinical outcomes in treatment using short implants. Proper surgical and prosthetic interventions lessen the treatment time with short implants and limit indications for the use of more complicated peri-implant procedures. This directly decreases the risk of complications and patient discomfort and decreases the cost of the procedure. Although currently available studies indicate the high success rate of short implants and could suggest them as an alternative, there is still no study offering a sufficient level of evidence and follow-up to be the basis for clinical decisions.
Footnotes
Statement
Conflicts of interest: No conflicts of interest declared.
Source of support: Self financing
This research was carried out without funding.
References
- 1.Esposito M, Grusovin MG, Felice P, et al. Interventions for replacing missing teeth: horizontal and vertical bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev. 2009;7:CD003607. doi: 10.1002/14651858.CD003607.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Emran S. Prevalence of tooth loss in Saudi Arabian school children: An epidemiological study of Saudi male children. Saudi Dental J. 1990;2(4):137–40. [Google Scholar]
- 3.Lawson W, Patel ZM, Lin FY. The development and pathologic processes that influence maxillary sinus pneumatization. Anat Rec (Hoboken) 2008;291(11):1554–63. doi: 10.1002/ar.20774. [DOI] [PubMed] [Google Scholar]
- 4.Bryant SR. The effects of age, jaw site, and bone condition on oral implant outcome. Int J Prosthodont. 1998;11:470–90. [PubMed] [Google Scholar]
- 5.Ulm C, Kneissel M, Schedle A. Characteristic features of trabecular bone in edentulous maxillae. Clin Oral Implants Res. 1999;10:459–67. doi: 10.1034/j.1600-0501.1999.100604.x. [DOI] [PubMed] [Google Scholar]
- 6.Oikarinen K, Raustia AM, Hartikainen M. General and local contraindications for endosseal implants--an epidemiological panoramic radiograph study in 65-year-old subjects. Community Dent Oral Epidemiol. 1995;23(2):114–18. doi: 10.1111/j.1600-0528.1995.tb00212.x. [DOI] [PubMed] [Google Scholar]
- 7.Esposito M, Grusovin MG, Rees J, et al. Interventions for replacing missing teeth: augmentation procedures of the maxillary sinus. Cochrane Database Syst Rev. 2010;17:CD008397. doi: 10.1002/14651858.CD008397. [DOI] [PubMed] [Google Scholar]
- 8.Deporter D, Pilliar RM, Todescan R, et al. Managing the posterior mandible of partially edentulous patients with short, porous-surfaced dental implants: early data from a clinical trial. Int J Oral Maxillofac Implants. 2001;16:653–58. [PubMed] [Google Scholar]
- 9.Deporter D, Ogiso B, Sohn DS, et al. Ultrashort sintered porous-surfaced dental implants used to replace posterior teeth. J Periodontol. 2008;79:1280–86. doi: 10.1902/jop.2008.070496. [DOI] [PubMed] [Google Scholar]
- 10.Sánchez-Garcés A, Costa-Berenguer X, Gay-Escoda C. Short implants: a descriptive study of 273 implants. Clin Implant Dent Relat Res. 2012;14(4):508–16. doi: 10.1111/j.1708-8208.2010.00301.x. [DOI] [PubMed] [Google Scholar]
- 11.Fugazzotto PA. Shorter implants in clinical practice: rationale and treatment results. Int J Oral Maxillofac Implants. 2008;23:487–96. [PubMed] [Google Scholar]
- 12.ten Bruggenkate CM, Asikainen P, Foitzik C, et al. Short (6-mm) nonsubmerged dental implants: results of a Multicenter clinical trial of 1 to 7 years. Int J Oral Maxillofac Implants. 1998;13:791–98. [PubMed] [Google Scholar]
- 13.Misch CE, Steignga J, Barboza E, et al. Short dental implants in posterior partial edentulism: a multicenter retrospective 6-year case series study. J Periodontol. 2006;77:1340–47. doi: 10.1902/jop.2006.050402. [DOI] [PubMed] [Google Scholar]
- 14.Maló P, de Araújo NM, Rangert B. Short implants placed onestage in maxillae and mandibles: a retrospective clinical study with 1 to 9 years of follow-up. Clin Implant Dent Relat Res. 2007;9:15–21. doi: 10.1111/j.1708-8208.2006.00027.x. [DOI] [PubMed] [Google Scholar]
- 15.Testori T, Del Fabbro M, Feldman S, et al. A multicenter prospective evaluation of 2-months loaded Osseotite implants placed in the posterior jaws: 3-year follow-up results. Clin Oral Implants Res. 2002;2:154–61. doi: 10.1034/j.1600-0501.2002.130205.x. [DOI] [PubMed] [Google Scholar]
- 16.Renouard F, Nisand D. Short implants in the severly resorbed maxilla: a 2-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;7(Suppl 1):104–10. doi: 10.1111/j.1708-8208.2005.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 17.Griffin TJ, Cheung WS. The use of short, wide implants in posterior areas with reduced bone height: a retrospective investigation. J Prosthet Dent. 2004;92:139–44. doi: 10.1016/j.prosdent.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Anitua E, Orive G. Short implants in maxillae and mandibles: a retrospective study with 1 to 8 years of follow-up. J Periodontol. 2010;81:819–26. doi: 10.1902/jop.2010.090637. [DOI] [PubMed] [Google Scholar]
- 19.Romeo E, Ghisolfi M, Rozza R, et al. Short (8-mm) dental implants in the rehabilitation of partial and complete edentulism: a 3- to 14-year longitudinal study. Int J Prosthodont. 2006;19:586–92. [PubMed] [Google Scholar]
- 20.Menchero-Cantalejo E, Barona-Dorado C, Cantero-Alvarez M, et al. Meta-analysis on the survival of short implants. Med Oral Patol Oral Cir Bucal. 2011;16(4):e546–51. doi: 10.4317/medoral.16.e546. [DOI] [PubMed] [Google Scholar]
- 21.Sun HL, Huang C, Wu YR, Shi B. Failure rates of short (≤ 10 mm) dental implants and factors influencing their failure: a systematic review. In t J Oral Maxillofac Implants. 2011;26:816–25. [PubMed] [Google Scholar]
- 22.Annibali S, Cristalli MP, Dell’Aquila D, et al. Short dental implants: a systematic review. J Dent Res. 2012;91(1):25–32. doi: 10.1177/0022034511425675. [DOI] [PubMed] [Google Scholar]
- 23.Pommer B, Frantal S, Willer J, et al. Impact of dental implant lenght on early failure rates: a meta-analysis of observational studies. J Clin Periodontol. 2011;38:856–63. doi: 10.1111/j.1600-051X.2011.01750.x. [DOI] [PubMed] [Google Scholar]
- 24.Neldam CA, Pinholt EM. State of the art of short dental implants: a systematic review of the literature. Clin Impl Dentistry Rel Resear. 2012;14(4):622–32. doi: 10.1111/j.1708-8208.2010.00303.x. [DOI] [PubMed] [Google Scholar]
- 25.Hagi D, Deporter DA, Pilliar RM, Arenovich T. A targeted review of study outcomes with short (< or =7 mm) endosseous dental implants placed in partially edentulous patients. J Periodontol. 2004;75:798–804. doi: 10.1902/jop.2004.75.6.798. [DOI] [PubMed] [Google Scholar]
- 26.Pierrisnard L, Renouard F, Renault P, Barquinis M. Influence of implant lenght and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res. 2003;5:254–62. doi: 10.1111/j.1708-8208.2003.tb00208.x. [DOI] [PubMed] [Google Scholar]
- 27.Bernard JP, Szmukler-Moncler S, Pessotto S, et al. The anchorage of Brånemark and ITI implants of diffrent lenghts.I. An experimental study in the canine mandible. Clin Oral Implants Res. 2003;14:593–600. doi: 10.1034/j.1600-0501.2003.120908.x. [DOI] [PubMed] [Google Scholar]
- 28.Akça K, Iplikçioğlu H. Finite element stress analysis of the effect of short implant usage in place of cantilever extensions in mandibular posterior edentulism. J Oral Rehabil. 2002;29(4):350–56. doi: 10.1046/j.1365-2842.2002.00872.x. [DOI] [PubMed] [Google Scholar]
- 29.Yang TC, Maeda Y, Gonda T. Biomechanical rationale for short implants in splinted restorations: an in vitro study. Int J Prosthodont. 2011;24(2):130–32. [PubMed] [Google Scholar]
- 30.Von Recum A. Handbook of Biomaterials Evaluation: Scientific, Technical and Clinical Testing of Implant Materials. New York, NY: McMilian; 1986. [Google Scholar]
- 31.Sevimay M, Turhan F, Kiliçarslan MA, Eskitascioglu G. Three-dimensional finite element analysis of the effect of different bone quality on stress distribution in an implant-supported crown. J Prosthet Dent. 2005;93(3):227–34. doi: 10.1016/j.prosdent.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 32.Lum LB. A biomechanical rationale for use of short implants. J Oral Implantol. 1991;17(2):126–31. [PubMed] [Google Scholar]
- 33.das Neves FD, Fones D, Bernardes SR, et al. Short Implants – An analysis of longitudinal studies. Int J Oral Maxillofac Implants. 2006;21:86–93. [PubMed] [Google Scholar]
- 34.Tawil G, Aboujaoude N, Younan R. Influence of prosthetic parametres on the survival and complication rates of short implants. Int J Oral Maxillofac Implants. 2006;21:360–70. [PubMed] [Google Scholar]
- 35.Blanes RJ. To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin Oral Implants Res. 2009;20(Suppl,4):67–72. doi: 10.1111/j.1600-0501.2009.01762.x. [DOI] [PubMed] [Google Scholar]
- 36.Birdi H, Schulte J, Kovacs A, et al. Crown-to-implant ratios of short-length implants. J Oral Implantol. 2010;36(6):425–33. doi: 10.1563/AAID-JOI-D-09-00071. [DOI] [PubMed] [Google Scholar]
- 37.Bidez MW, Misch CE. Force transfer in implant dentistry: Basic concepts and principles. J Oral Implantol. 1992;18:264–74. [PubMed] [Google Scholar]
- 38.Nedir R, Bischof M, Briaux JM, et al. A 7-year life table analysis from a prospective study on ITI implants with specjal emphasis on the use of short implants. Results from a private practice. Clin Oral Implants Res. 2004;2:150–57. doi: 10.1111/j.1600-0501.2004.00978.x. [DOI] [PubMed] [Google Scholar]
- 39.Deporter DA, Al-Sayyed A, Pilliar RM, Valiquette N. „Biologic Width” and crestal bone remodeling with sintered porous-surfaced dental implants: A study in dogs. Int J Oral Maxillofac Implants. 2008;23:544–50. [PubMed] [Google Scholar]
- 40.Lazzara RJ, Porter SS. Platform-switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26(1):9–17. [PubMed] [Google Scholar]