Abstract
Patient: Female, 14
Final Diagnosis: Multiple pituitary hormone deficiency
Symptoms: Hyponatremia
Medication: —
Clinical Procedure: Endovascular embolectomy
Specialty: Endocrinology and Metabolic
Objective: Patient complains/malpractice
Background:
Hyponatremia is one of the most common electrolyte disorders. Depending on the patient’s hydration status, hyponatremia can be classified as hypovolemic, hypervolemic, or normovolemic. The last type is caused by the syndrome of ‘inappropriate’ secretion of antidiuretic hormone (SIADH), and more rarely by SIADH-like syndrome, in which oversecretion of ADH is caused by adrenal or thyroid insufficiency.
Case Report: This report presents the case of a girl who, at the age of 14 years and 4 months, presented with severe normovolemic hyponatremia (Na 110 mmol/L) due to decompensation of previously undiagnosed secondary adrenal insufficiency due to a respiratory tract infection. Hyponatremia was worsened by concomitant hypothyroidism and valproic acid therapy. This case is a rare example in clinical practice of multiple pituitary hormone deficiency, that despite typical symptoms such as short stature, adrenal insufficiency (hypoglycemia, hyponatremia, and low blood pressure), or delayed puberty, was diagnosed only after the development of adrenal crisis (severe symptomatic hyponatremia and hypoglycemia).
Conclusions:
In prepubertal pediatric patients with severe hyponatremia, multiple pituitary hormone deficiency must be considered. Patients with hypothyroidism, as well as concomitant epilepsy treated with valproic acid, are at risk of severe hyponatremia, which may cause symptoms mimicking an epileptic attack.
Keywords: hyponatremia, secondary adrenal insufficiency, multiple pituitary hormone deficiency, pituitary stalk interruption syndrome
Background
Hyponatremia is one of the most common electrolyte disorders. It can cause many different clinical signs and symptoms, including neurological symptoms such as headache, confusion, lethargy, fatigue, irritability, spasm, and the most serious, seizures and coma. Depending on the patient’s hydration status, hyponatremia can be classified as hypovolemic, hypervolemic, or normovolemic. The last type is not caused by actual lack of sodium, but rather by water retention due to the syndrome of ‘inappropriate’ secretion of antidiuretic hormone (SIADH), and, more rarely, by SIADH-like syndrome, in which oversecretion of ADH is caused by adrenal or thyroid insufficiency.
Case Report
A girl age 14 years and 4 months was admitted to the hospital due to seizures during an acute respiratory tract infection with fever and vomiting. The child was born at 40 weeks gestation, birth body weight was 3800 g, and length was 56 cm. The growth was linear, with height at about (–) 3 SDS (standard deviation score) below the mid-parental height, which was 151 cm (–2.4 SDS). At ages 6, 8, and 12 years, in the course of infections, generalized tonic-clonic seizures occurred, accompanied by hyponatremia (Na ≤130 mmol/L). After the second episode, due to the ongoing presence of epileptiform discharges in the electroencephalography, valproic acid therapy was started. On admission to the hospital the general condition of the child was good. Acute pharyngitis and tonsillitis were diagnosed. Furthermore, skin pallor and growth retardation (–) 3.3 SDS were found, with body weight appropriate for the height and no signs of sexual maturation (thelarche I, pubarche I according to the Tanner scale, and axillary hair absent) (Figure 1.) The laboratory studies showed low serum sodium levels (124.9 mmol/L), increased markers of inflammation (C reactive protein: 77.6 mg/dL), and microcytic anemia. In spite of treatment with antibiotics and intravenous infusions of sodium chloride, the child’s condition deteriorated sharply on the fourth day of hospitalization; the girl was pale, lethargic, and weak, she reported having anxiety, and was temporarily disoriented. The blood pressure was low: 85/57 mmHg (50th percentile for height and sex: 106/77 mmHg) [1]. The serum sodium level was decreasing: from 113 to 110 mmol/L. Laboratory tests showed low levels of cortisol (48.9 ng/mL N: 50–230 ng/mL), lack of a compensatory increase of ACTH (adrenocorticotropin) (14.4 pg/mL, N: 10–60 pg/mL), and the glucagon stimulation test showed inadequate adrenal reserve (max. cortisol concentration 17.7 ng/mL). Normal concentrations of aldosterone (217.4 pg/mL N: 35–310 pg/mL) and plasma renin activity (0.41 ng/mL/ h N: 1.5–5.7 mg/mL/h) with normokalemia (4.48 mmol/L) led to the exclusion of aldosterone deficiency. Secondary adrenal insufficiency was diagnosed and hydrocortisone therapy was started (initial dose 30 mg/m2), obtaining a gradual improvement in the general condition of the child and an increase in the concentration of sodium. MRI revealed the pituitary gland measured 8×12×4 mm, an ectopic posterior pituitary lobe measuring 3×3.6 mm located medially and adhering to the dorsal surface of the optic chiasm, and the pituitary stalk was difficult to trace (Figure 2A, 2B). Additional tests revealed secondary hypothyroidism, growth hormone (GH) deficiency, and hypogonadotropic hypogonadism. The introduction of multiple hormonal replacement therapy (hydrocortisone, L-thyroxine, human recombinant GH, estradiol) normalized the metabolic and laboratory parameters and improved the general condition and growth of the child. Subsequently, the girl was reconsulted neurologically and valproic acid therapy was gradually withdrawn without causing any convulsions. The convulsions were earlier mistaken for seizure attacks and most probably were due to hyponatremia and/or low blood glucose, which had been repeatedly observed in the laboratory tests of the child during these attacks.
Figure 1.

Female patient (age 14 years and 4 months) with no signs of sexual maturation (thelarche I, pubarche I according to the Tanner scale and axillarche absent).
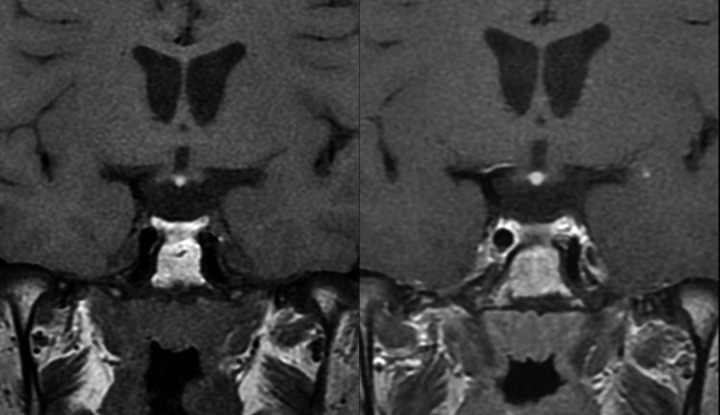
Figure 2.
MRI of the pituitary gland. Sequences FSET1 and FSET1 after enhacement, coronal images. The pituitary stalk is difficult to trace, in unenhanced and enhanced images too. The enlargment of the hiperintensive structure, corresponding the ectopic posterior pituitary lobe, in FSTE1 after enhacement suggests the presence of the vascular structures of the pituitary stalk in adherence to the ectopic lobe, what indirectly confirms the lack of continuity of the further section of pituiatry stalk.
Discussion
Hyponatremia, which is defined as the lowering of serum sodium concentration values below 135 mmol/l, is one of the most commonly observed electrolyte disorders and occurs in almost 15% of patients hospitalized for various causes [2,3]. Normovolemic hyponatremia is most often caused (in over 60% of cases) by SIADH, which is diagnosed when the following criteria have been met: urine osmolality >100 mOsm/KgH2O, urine sodium concentration >30 mmol/L, no edema or other signs of water retention, with the preservation of normal renal, adrenal, and thyroid function [2,4]. The most common causes of SIADH are central nervous system diseases: tumors, abscesses, meningitis, head injury or surgery, and certain medications such as anticonvulsants, antipsychotics, antidepressants, angiotensin-converting-enzyme inhibitors, and cytostatics. A rare, yet important, cause of normovolemic hyponatremia is SIADH-like syndrome, which has the same clinical symptoms and metabolic changes as SIADH, yet increased secretion of ADH is caused by secondary adrenal insufficiency or hypothyroidism (primary or secondary) [3,5]. In the presented case, 3 independent causes of normovolemic hyponatremia occurred: previously undiagnosed secondary adrenal insufficiency, hypothyroidism, and chronic valproic acid therapy. This caused adrenal crisis decompensation in the course of a respiratory tract infection and severe life-threatening hyponatremia. The main cause of hyponatremia during secondary adrenal insufficiency is the increased secretion of ADH due to the lack of inhibiting action of cortisol. In addition, overexpression of aquaporin-2 channels leads to increased water retention by the kidneys [6]. This causes water retention and a significant drop in serum sodium levels, which even increased secretion of aldosteron is not able to compensate [7]. Additional factors that increase ADH secretion are present in adrenal insufficiency hypoglycemia and stimulation of the vomiting centers of the brain [7]. Moreover, concomitant hypothyroxinemia causes a reduction in cardiac output and the volume of blood, which in turn leads to a reduction in the glomerular filtration rate (GFR) in the kidney, and, in consequence, to an increase in the reabsorption of water in the proximal tubule of the kidney. Furthermore, a reduction in circulating blood volume directly stimulates the secretion of ADH [3,8].
Conclusions
In this case report, the least known of all the described causes of hyponatremia is valproic acid therapy. Based on previously described cases, it is believed that the most important factor is its direct action on the tubules of the kidneys and their increased sensitivity to ADH [9].
Acknowledgments
The authors would like to thank: Dr. Agata Zygmunt-Górska, Dr. Anna Kalicka-Kasperczyk, Dr. Dorota Roztoczynska, Dr. Katarzyna Tyrawa, and Dr. Anna Wędrychowicz for clinical assistance, and Dr. Karolina Popławska for translation of the manuscript.
Abbreviations:
- ACTH
adrenocorticotropin;
- ADH
antidiuretic hormone;
- EEG
electroencephalography;
- fT3
free triiodothyronine;
- fT4
free thyroxine;
- GH
growth hormone;
- LH-RH
lutropine releasing hormone;
- MRI
magnetic resonance imaging;
- N
normal value;
- SDS
standard deviation score;
- SIADH
syndrome of ‘inappropriate’ secretion of antidiuretic hormone;
- TSH
thyroid-stimulating hormone
Footnotes
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
Conflict of interest
The authors have no conflicts of interest to disclose.
References:
- 1.National High Blood Pressure Education Program Working Group on High Blood Pressure Education Program in Children and Adolescents. The fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76. [PubMed] [Google Scholar]
- 2.Baylis PH. The syndrome of inappropriate antidiuretic hormone secretion. Int J Biochem Cell Biol. 2003;35:1495–99. doi: 10.1016/s1357-2725(03)00139-0. [DOI] [PubMed] [Google Scholar]
- 3.Parenti G, Ricca V, Zogheri A, et al. A case of hyponatremia caused by central Hypocortisolism. Nat Clin Pract Endocrinol Metab. 2007;3:369–75. doi: 10.1038/ncpendmet0459. [DOI] [PubMed] [Google Scholar]
- 4.Bartter FC, Schwartz WB. The syndrome of inappropriate secretion of antidiuretic hormone. Am J Med. 1967;42:790–806. doi: 10.1016/0002-9343(67)90096-4. [DOI] [PubMed] [Google Scholar]
- 5.Smyczyńska J, Lewiński A, Hilczer M. Disorders of Water-electrolyte Balance During Endocrine Diseases in Children Part I – Disorders of Vasopressin Secretion and Action Endokrynol Ped. 2010;4:49–62. [Google Scholar]
- 6.Saito T, Ishikawa SE, Ando F, et al. Vasopressin-dependent upregulation of aquaporin-2 gene expression in glucocorticoid-deficient rats. Am J Physiol Renal Physiol. 2000;279:F502–8. doi: 10.1152/ajprenal.2000.279.3.F502. [DOI] [PubMed] [Google Scholar]
- 7.Tuuri R, Zimmerman D. Adrenal Insufficiency in the Pediatric Emergency Department. Clin Pediatr Emerg Med. 2009;10:260–71. [Google Scholar]
- 8.Larsen PR, Davies TF.Hypothyroidism Larsen PR, et al.(eds.)Williams Textbook of Endocrinology WB Saunders; Philadelphia: 200210423–55. [Google Scholar]
- 9.Branten AJW, Wetzels JFM, Weber AM, Koene RAP. Hyponatremia due to sodium valproate. Ann Neurol. 1998;43:265–67. doi: 10.1002/ana.410430219. [DOI] [PubMed] [Google Scholar]