Abstract
In 2001, the Regenstrief Institute for Health Care and the Indiana University School of Medicine (IUSM) began an IAIMS planning effort to create a vision and a tactical plan for the first Integrated Advanced Information Management Systems (IAIMS) implementation to cross a large area and include unaffiliated institutions. A number of elements made this planning effort unique. Among these elements were the existence of a network infrastructure that supported the Indianapolis Network for Patient Care, the existence of a mature medical informatics program at the Regenstrief Institute, and the existence of a wide-area knowledge network fostered by the IUSM libraries. However, the leadership for a strong information technology role in the IUSM that could promote collaboration in support of education and research across the diverse Indianapolis hospital systems had been lacking. By bringing together various groups, each with a commitment to improve health care quality and public health across the Indianapolis metropolitan area, regardless of individual institutional affiliation, the strategic directions for I3–Indianapolis IAIMS Initiative have been defined and the foundations for a third generation IAIMS construct have been laid in Indianapolis, Indiana.
In 1997, over a decade and a half after the beginning of the Integrated Academic/Advanced Information Management System (IAIMS) program, Stead challenged IAIMS institutions to evolve the concept into an “area,” or interinstitutional, approach. He defined five necessary stages for this evolution as (1) focusing on critical individual applications, (2) investment in infrastructure to create a capacity for integration, (3) integration driven by new products, (4) integration driven by component-based architecture, and (5) reapplication of the first four processes across multiple institutions [1].
While the Indiana University School of Medicine (IUSM) and the Regenstrief Institute for Health Care have recently completed their IAIMS Planning Process, Stead's challenge is particularly appropriate to the I3–Indianapolis IAIMS Initiative, because stage five is now being realized.
SIGNIFICANCE
A treatise known as the Matheson-Cooper Report [2] was the product of a 1982 project of the Association of American Medical Colleges (AAMC) with support by the National Library of Medicine (NLM). This report was the genesis of NLM's IAIMS program and the catalyst for the transformation of information management across a large number of academic health centers. As stated by the principal developers of the IAIMS program at NLM a decade after its inception, “The Integrated Academic Information Management System (IAIMS) Program was, and is, the right thing to do” [3].
In the early 1980s, information systems were beginning to be recognized for their potential to manage large amounts of information key to academic health center operations. The Matheson-Cooper report noted that these information systems were being developed out of need, frequently driven by crisis, and without the benefit of enterprise-wide planning. Integration was seen as key to functionality, frequently conceptualized by the idea that all necessary information should be accessible via a single desktop computer. Further, integration was recognized as encompassing not only interfaces between dissimilar technologies but also reengineering workflows and human systems to create a more efficient and effective academic health care environment.
Because the early IAIMS initiatives were institutionally specific, the primary tangible outcomes of these projects were very different. Among the early recipients of IAIMS funding, Columbia-Presbyterian Medical Center brought to reality the concept of information at the point of need accessible from a single workstation through an integrated, best-of-breed approach, primarily in the clinical arena [4]. Georgetown University developed a Knowledge Network [5], and Baylor created its Virtual Notebook System [6]. Yale University, Oregon Health Sciences University, and the University of Washington built institutional architectures supporting access to information resources across disparate environments using standard vocabularies and unique institutional assets [7–9]. ACOGQUEST, the information network of the American College of Obstetricians and Gynecologists (ACOG), was created using the basic precepts of the IAIMS program to deliver targeted information to the ACOG membership across the nation [10].
The second generation of IAIMS institutions included Vanderbilt University, the University of Pittsburgh, the University of Missouri–Columbia, and the City of Hope National Medical Center. These institutions built on the work of the early sites and took the IAIMS concept to a much higher level. The confluence of good ideas, leadership, and technological advances resulted in significant product development and higher levels of institutional integration at these campuses. Vanderbilt deserves special mention for its fast-track implementation of IAIMS and its mature model that, in a recent AAMC study about the impact and future directions of IAIMS, was used as the “beta site for the site visit process and interview tools” [11].
During the past two decades of IAIMS, evolution has been significant. Early programmatic focus was on the development and deployment of current and new technologies to create integrated information architectures crossing multiple organizational aspects of the respective institutions. More recent IAIMS implementations have assumed the existence of significant technologies in the institutions and have focused on the development of new tools to facilitate integration and promote institutional and IAIMS branding. However, with all of the advances, evidence has been growing that IAIMS in its purest sense is not a permanent construct and needs continual reenergizing.
In his 1997 article, Stead noted three recurrent themes that cross all IAIMS institutions: each institution has undergone a paradigm shift that has enabled the emergence of a respected informatics core to lead information technology change; each has built a significant information infrastructure; and each has worked across boundaries and cultures to provide focus on an information technology plan to support the needs of distinct groups. These three elements are critical to ensuring that the IAIMS concept is viable, and analyzing them must be integral to the planning process [12].
APPROACH
The Indiana University School of Medicine (IUSM)/Regenstrief Institute for Health Care began the IAIMS planning process on July 1, 2001. The Regenstrief Institute, founded in 1969, is a joint enterprise of the Regenstrief Foundation, the IUSM, and the Health and Hospital Corporation of Marion County, Indiana. Located on the IU medical center campus in Indianapolis, the institute is comprised of full-time investigators, affiliated scientists, and fellows. Over the past forty plus years, it has become internationally recognized for conducting research to improve health care by improving the capture, analysis, content, and delivery of information needed by patients, their health care providers, and policy makers and for conducting intervention studies designed to measure the effect of the application of this research on the efficiency and quality of health care. Because of the wealth of its research in medical informatics, the Regenstrief Institute became the lead institution in the planning process.
One of the outcomes of some of the early IAIMS implementation projects was the development of a solid medical informatics program. The Regenstrief Institute was one of the few institutions to develop such a program without IAIMS funding. One of the outcomes of some of the early IAIMS implementation projects was the development of a sophisticated information infrastructure for patient care. Again, the Regenstrief Institute had already developed one. Another outcome of some of the early IAIMS implementation projects was the networking of knowledge-based information resources across the academic health center enterprise. The IUSM libraries, in partnership with the Regenstrief Institute, had been providing information at the point of decision making since the beginnings of electronic access to such resources.
Two areas were not as well developed. The first of these was internal to the medical school. While a small IUSM Office of Technology supported administrative applications and information technology support was promised from Indiana University's University Information Technology Services (UITS) group, the reality had been the development of departmentally based information services units with virtually no coordination. An integral part of the IAIMS planning initiative was the development of the IUSM Information Technology Strategic Plan.
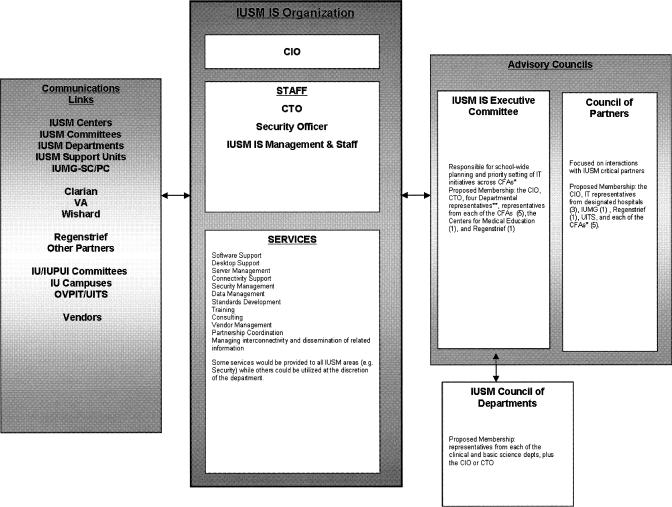
The planning process lasted over a year and resulted in the restructuring of the Office of Technology with the appointment of three new and critical positions, a chief information officer, a chief technology officer, and an information security officer. To foster greater input, three advisory groups were created: the IUSM Information Services (IS) Council (or Executive Committee), the Council of Partners, and the IUSM Council of Departments. This structure enabled input and decision making from a divergent group of key stakeholders as explained below and shown in Figure 1.
Figure 1.
Indiana University School of Medicine Information Services organization
As previously mentioned, most of the major information technology (IT) initiatives and support services had been driven by the departments. Departments with significant IT investments did not want to lose control of their IT personnel and resources, but they were willing to support an enhanced centralized resource with appropriate input. The Council of Departments, providing representation from each academic department in the IUSM, provides this input, with up to four representatives from this council serving on the IS Council.
The five core functional areas in IUSM, each led by an executive associate dean, are: finance and administration, academic affairs, research affairs, educational affairs, and clinical affairs. These areas each have representation on both the IUSM IS Council and the Council of Partners. The Regenstrief Institute also has representation on both groups. The IS Council serves as the primary advisory committee to the Office of Technology, and its members each represent key areas of the academic medical center.
The Council of Partners is necessary to provide cross communication with the primary teaching hospitals and practice groups. IUSM does not own a teaching hospital but has significant relationships with Clarian Health (Methodist Hospital, IU Hospital, Riley Children's Hospital), the VA Medical Center, and Wishard Health Services. Because these facilities are key loci of medical education and clinical research as well as the practice sites of the IUSM clinical faculty, integration of IT services and resources are essential to foster cross-campus and institutional communication.
In addition to the restructuring of the Office of Technology and its advisory committees, three other key groups provide enterprise-wide technology support and are key participants in the IUSM IS administration. In the research arena, a director of bioinformatics has been appointed to integrate bioinformatics into the fabric of the research being driven by the Indiana Genomics Initiative. The Office of Information Resources and Educational Technology was created in 2002 to oversee all educational technology including curriculum management, computer-assisted instruction, video conferencing, and mobile computing in support of learning processes. The IUSM Libraries are a key unit in this office, with responsibility for knowledge management and dissemination. The Regenstrief Institute continues to provide the primary clinical computing advances for the medical school.
The second area needing development falls outside the purview of the medical school and is central to the outreach activities of the Regenstrief Institute. Indianapolis is the largest city in Indiana. In addition to the four hospitals comprising the primary academic medical center, it has three other major hospital systems and a growing number of specialty hospitals. Given the threats of bioterrorism and emerging infectious diseases, providing information access across all institutions is not only intended to meet the “area” goal of the next generation of IAIMS but is also a strategic directive of building today's public health infrastructure.
In 1994, in collaboration with three hospital emergency departments, four health management organization (HMO) practice sites, five community health clinics, and fourteen homeless care sites, the Regenstrief Institute began to design and implement the Indianapolis Network for Patient Care and Research. Features of this early system included a secure, wide-area network; a clinical data repository; a clinician's workstation; and a focus on standard vocabularies and data exchange. This early network embodied the concept of the area-focused IAIMS and became the genesis for the current I3–Indianapolis IAIMS Initiative [13, 14].
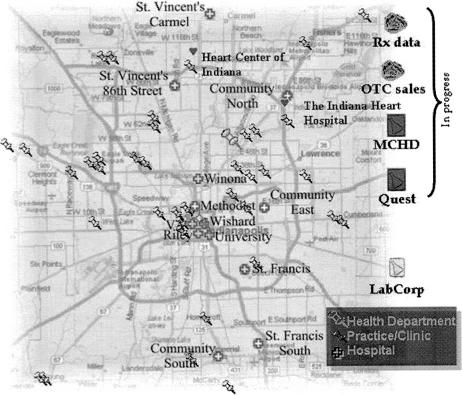
During the IAIMS planning period, the Indiana Network for Patient Care (INPC) was leveraged to enhance information transfer among the hospitals in the city and the Indiana Department of Health with facilitation from the Regenstrief Institute. The goal of the INPC was to push necessary clinical information to health care providers through a common Web interface, regardless of the source of the information or the location of the health care provider. Figure 2 is a map of the current INPC.
Figure 2.
Map of the Indiana Network for Patient Care
The conceptualization of the network is relatively simplistic and yet underscores the basis of the next generation of IAIMS, one in which institutions with different missions and organizational priorities can work together to improve health care delivery across a community. The problem is complex; the solution is simple in concept. Five different hospital information systems need to share information. To create true integration of these different systems would be a Herculean task. However, using Health Level 7 standards for data transfer, an INPC clinical data repository for each participating hospital can feed into a central, partitioned data repository. This repository is then indexed by unique patient identifiers and provides patient-specific information to any authorized health care provider, regardless of location or system, through the INPC Web interface and authentication.
A recent enhancement of the system is the creation of Docs4Docs, an automated pushing of lab results to providers, once the results become available, in the method specified by the individual provider (email, fax, etc.). This recent feature has moved the information transfer from interinstitutional to primary practice sites. To fully realize an area-wide IAIMS initiative, access to information in support of health care delivery cannot be limited by types of institutions but must be driven by end users.
Concomitant to the early development of the INPC, a second initiative, ICareConnect, was being conceptualized to support information access at the office level. While Docs4Docs can deliver patient care information to the office as well as the bedside and the INPC provides the architecture for information sharing, many providers need assistance in establishing and maintaining their initial computer connections. ICareConnect has been developed to provide this support.
While planning for the logical extension of information from the hospital to the office or clinic, it became apparent that the I3–Indiana IAIMS Initiative had addressed each of Stead's three themes. A major paradigm shift has taken place, enabling the creation of a central data repository supporting activities of health care providers across the Indianapolis Metropolitan Statistical Area (MSA). Hospital chief executive officers (CEOs) and chief information officers (CIOs) have agreed to share data to improve patient outcomes. Trust in information integrity and patient confidentiality policies and procedures, as well as a strong desire to improve the quality of care across institutions, has resulted in increasing use of the INPC.
It is frequently difficult to get institutions to work together for a common good. At the beginning of the development of INPC, this was true. However, a number of factors fell into place to enable the INPC to become a reality. The driver of the INPC effort was a distinguished physician, respected across the state but particularly by the CEOs and CIOs of the hospitals in Indianapolis. The project was pushed by the Indiana State Department of Health. Federal funds supported much of the effort. Provider workflows were not altered; all data transfer was transparent to the user. The Regenstrief Institute was viewed as a neutral partner that would protect the data of the donor institutions.
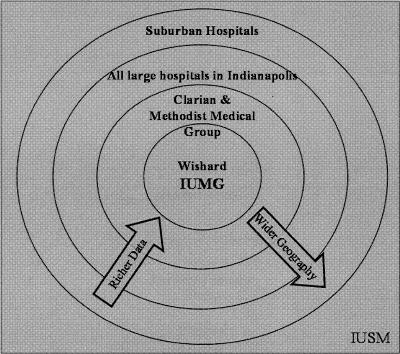
In addition to supporting the INPC concept, the hospitals have also been willing to support the telecommunications infrastructure to enable the operation of INPC; the Regenstrief Institute has provided the technological hardware and software to bring the concept to reality. INPC is the model for crossing institutional boundaries to create an area IAIMS construct. The richness of data and the geographic reach of the I3–Indianapolis IAIMS Initiative can also be pictured as concentric circles with richer data sources and Indianapolis's center moving outward to include additional participants. The IUSM cuts across many of these boundaries through its research and education missions as well as its clinical care. Figure 3 represents this idea.
Figure 3.
Data and geographical relationships in I3
The initial realization of INPC has raised several issues specific to IAIMS planning. The first of these is branding. While a single institution might be able to coordinate and consolidate information integration under the IAIMS umbrella, beyond its basic concepts, the acronym has little meaning when crossing multiple organizations. The Indianapolis Network for Patient Care and ICareConnect are two easily recognized and accepted names for information delivery in the Indianapolis area. IAIMS is not, although the IAIMS principals underpin both initiatives. When attempting to develop integrated information systems across multiple institutions, names for those systems must be based on consensus of the key stakeholders.
While it has been difficult to achieve IAIMS brand recognition across all of the units organized under the IAIMS planning efforts, plays on words and symbols have the potential to offer alternatives. Those principally involved with the IAIMS planning efforts created “I3” as a logo for the implementation phase for several reasons. It is easy to remember. It does not detract from the INPC and ICareConnect name recognition. The logo itself is appealing. Indianapolis is the network operations center for Internet 2 (I2). The area concept in IAIMS is the third iteration of the program, hence I3. The logo is found in Figure 4.
Figure 4.
I3 logo
Another issue is that of recognition of multiple information needs and limitations imposed by primary affiliations. An example of this is the desire to provide a common suite of knowledge-based information resources and the licensure issues dictated by Indianapolis hospital memberships in larger health care systems. A solution to this problem has been theorized and will be one focus of the expansion and implementation of the next generation of the I3–Indianapolis IAIMS Initiative.
Finally, the most significant factor in the adoption of the new system is human. Regardless of the apparent benefits of INPC, Docs4Docs, and ICareConnect, without both “marketing” and initial customized support, rapid widespread adoption has little likelihood of success. Further, without a solid business model that will lead to ongoing support, an area IAIMS initiative is doomed to fail, because it lacks the safety net provided by a single organization. Therefore, to institutionalize an area IAIMS across multiple organizations, significant attention must be paid to gaining a critical mass of users and to developing a business model for long-term support and fiscal viability.
NEXT STEPS
To realize the goal of establishing a common framework for collection and delivery of critical health information, which crosses virtually all hospitals and practice sites in the Indianapolis Metropolitan Statistical Area (MSA), that is used by a majority of health care providers and is supported by a solid financial model, the I3–Indianapolis IAIMS Initiative has four aims.
Aim 1: Expand and enhance the existing Indiana Network for Patient Care by adding community-identified, context-appropriate resources including additional clinical data, knowledge resources, and functionality
The first key resource is a cleaned and expanded global file of doctors that contains demographic and contact data for all providers. The file contains not only email addresses and fax numbers but also current affiliations, addresses, and other data necessary for communications. This file is the basis for authentication of users and will enable access to knowledge-based information predicated on licensure agreements in addition to serving as a key resource for the Indiana Department of Health and its information infrastructure. This file will be the basis for outreach, usage monitoring, and digital rights management. After development, maintenance of this directory is central to enhancing resources and building a community of knowledge-based practice.
Garnering buy-in to the current network requires providing members with their requested resources. A needs assessment was done in late 2002, and a number of resources were identified as desirable. These information resources were primarily clinical, including expanded access to drug resources. INPC currently stores data from Wishard Health Services pharmacies. To expand the availability of outpatient pharmacy data, judged one of the three most important data sets to add to the INPC, an agreement in principal exists with RxHub, a joint venture of the largest pharmaceutical benefit-management companies, to provide data on outpatient prescription transactions. In addition, an agreement with the RODS Laboratory in Pittsburgh, Pennsylvania, has provided access to the National Pharmaceutical Resource that includes approximately 60% of the over-the-counter sales data for Indiana.
In addition to drug information, expanded access to Ovid MEDLINE and its linked full-text resources has been requested. The hospitals of Clarian Health and Wishard have significant access through the consortium agreement negotiated by the IUSM libraries. One other hospital system in Indianapolis indicated interest in joining the consortium. However, other hospital systems are either not interested in expanding current access or are part of multi-hospital systems that support group purchasing of knowledge-based resources for affiliates. Should this interest change, a favorable consortium agreement for Ovid access for all hospitals in Indiana has recently been established between IUSM and Ovid and is open to any Indiana hospital.
To provide appropriate access to licensed knowledge and databases, network members will be given access to the greatest number of resources to which they are entitled. To facilitate this, resources will be ranked as to completeness and extensibility. Based on the affiliation agreements indicated in the global directory, each member will be given the highest level of resources, with the ability to access specifically authenticated resources on demand.
The INPC provides access to various information resources including MEDLINE through Ovid and PubMed as well as PraxisMD. MEDLINE access is simplified, because no login is required and full-text access is provided by the library through open links. Providers access PraxisMD through a search box on each results review page. The most common medical problems in the Regenstrief Medical Records System (RMRS) have been mapped to PraxisMD terminology to facilitate linkages. In addition, Infobutton linkages have been made in the system to Columbia-Presbyterian's Infobutton server for laboratory results and medications [15, 16].
Another resource to be provided is the push of knowledge-based information in response to a public health emergency. Because the system forwards reportable disease information to the health department, trends at multiple sites are easily identified. Through an agreement with the Indiana State Department of Health, indications of an emerging infectious disease or a bioterrorism event will trigger notification of the IUSM Medical Libraries. Knowledge informatics faculty will identify appropriate evidence in disease management and push the information to the network users along with information from the Indiana Department of Health alert.
While not a key part of the I3–Indianapolis IAIMS Initiative, the network will facilitate enhancements in two areas benefiting the IUSM, education and research. The first benefit will be in the area of education. IUSM uses ANGEL, a Web-based curriculum management system, for course delivery and distributed learning. Medical students rotate through all hospitals in the target area and, while they are currently able to access ANGEL, the different hospitals do not have a common interface.
Because of the need to capture clinical data in a secure environment outside of the individual hospital's clinical data repository, these data will also enhance the immense clinical data repository already available at the Regenstrief Institute, making this system the premier source of clinical data for many future research projects. A new generation of query tools has been developed based on FastRetrieval (a very fast tool for identifying cohorts and creating basic descriptions) as part of a National Cancer Institute–funded project.
In addition to supporting traditional biomedical research, the I3–Indianapolis IAIMS Initiative will provide an outstanding laboratory for studying medical informatics innovations. With the extensive data linkages and software tools, researchers will have many opportunities to study questions that cannot be studied anywhere else.
Aim 2: Promote use of these data and knowledge resources by patients, providers, researchers, educators, and policy makers
Many innovative products of medical informatics initiatives have never achieved widespread adoption, not because of their lack of utility, but because of the reticence on the part of the targeted user to adopt the innovation. This reticence comes from fear of change, difficulty in incorporating the system into current workflows, lack of initial installation support, and need for ongoing maintenance. Because the goal of this project is not to create an area IAIMS, but to achieve widespread acceptance and use, promotion and support are critical to success.
One of the first efforts of promotion is the reengineering of the extant INPC Website. Health care providers need to identify with the site and make it their primary access to their health care resources, whether they need current information about their patients or access to knowledge-based information. To facilitate this, a new Website will be designed to provide an inviting and functional locus of information, ensuring appropriate hospital and office branding based on primary affiliations while retaining the common look of the I3–Indianapolis IAIMS Initiative.
The initial focus of the INPC is to provide information in support of health care delivery in the hospital setting. However, to fully realize the proposed Indianapolis MSA IAIMS, the systems need to be expanded to clinics and offices. Partnerships with the IT groups at the hospitals will guarantee support for in-hospital access. A variety of techniques are necessary to encourage adoption and use of the systems in clinics and offices. Identification of early adopters will be the first step in taking the project beyond hospital walls. Other techniques include face-to-face meetings with health care providers to install appropriate software and assist them in reengineering their work flows. Additionally, system use will be monitored and a drop off in use will trigger a site visit and employment of academic detailing to encourage continued participation.
Logical geographic expansion paths include adding the eight community hospitals in the counties surrounding Marion County, all of which are members of the Suburban Hospital Association and some of which, such as Major Hospital in Shelbyville, are very sophisticated in terms of IT. These hospitals all use Meditech, which should limit the effort required to create interfaces for all of them.
The Indiana State Department of Health Information Services and Policy Commission has surveyed all of the hospitals throughout the state and found that 60% have high-speed (T1) Internet access in place already, but that 10% did not have any Internet connection. Building on Indiana's statewide government network and using funds available to the health department through the Centers for Disease Control and Prevention (CDC), these 10% should have high-speed Internet connections in place within the year. This work lays the foundation for further expansion throughout the state.
Aim 3: Evaluate the project through on-going data analysis and periodic qualitative research such as structured interviews or focus groups to assess usability, usefulness, and perceived impact on patient care
A variety of evaluation techniques will build upon current evaluation methods used to assess the effectiveness and adoption of the I3–Indianapolis IAIMS Initiative. The first of these is ongoing data capture. Transactions with the current system are captured, and data can be extracted granularly to determine the level of site and individual participation. Particularly important are trends in use. As mentioned in aim 2, if providers initially use the system at a high level and then their use declines, this could have a negative impact on both community-based patient care and public health monitoring. For this reason, use data capture will focus not only on absolute numbers to tease out growth in system use but also on individual use to determine potential problems.
Other data that will be monitored and reported include the transactions between the clinical data repository and the state health department for the number and types of reportable diseases, the number of Docs4Docs provided through the network, the number of accesses to knowledge-based information, and the number of Website visits. The evaluation data collected across the time of the project will be used to refine the system and provide support for both internal promotion and dissemination of the process and results of the initiative.
Aim 4: Create a sustainable, self-funding model for the resource
The I3–Indianapolis IAIMS Initiative is close to taking its first step toward financial sustainability. Through ICareConnect, the five major health systems are preparing to pay for clinical messaging services. The fee for clinical messaging, less than the amount that institutions spend now to deliver results, will support initial ICareConnect operations. This win-win approach is made possible by using Docs4Docs for electronic delivery of most of the results, with attendant savings. Clinical messages for providers that do not use Docs4Docs will be provided through fax or print and mail delivery. ICareConnect staff will provide support to providers in their offices, and the Regenstrief Institute will provide the software, manage the databases, and have responsibility for creating and maintaining interfaces for the source systems.
CONCLUSION
Every IAIMS implementation is different and generally entails a great deal of innovation for its environment. IAIMS began in the academic realm with basic infrastructure and migrated in response to the technology explosion to advanced applications, for the most part still in a single institution or organization. A few more recent initiatives have targeted loosely affiliated institutions with an attempt to insert “area” into the concept. However, no group of unaffiliated institutions has yet to integrate information technology across a wide group of clinical, research, education, and support applications. The I3–Indianapolis IAIMS Initiative, through its early development of the Indianapolis Network for Patient Care, has already laid the foundation for what promises to be the first implementation of its kind.
Most of the early IAIMS implementations involved clinical processes. This has been the cornerstone of medical informatics and has provided a platform for a more global approach to integrating disparate systems. Clinical information technology is even more important today. Not only is the medical community faced with all of the mandates of the Health Insurance Portability and Accountability Act (HIPAA) but with the need to better coordinate community health information for a variety of public health activities. The I3–Indianapolis IAIMS Initiative has already made great strides in this area.
The I3–Indianapolis IAIMS Initiative will build on the already substantial health information network in Indianapolis, coordinated by the Regenstrief Institute, to create a seamless network of results reporting that extends beyond the hospital to the primary care practice site, to link the health department and develop protocols to identify emerging infectious diseases and potential bioterrorism threats regardless of the locus of treatment, and to provide access to evidence and push information for decision support to the point of care. When this is accomplished, the I3–Indianapolis IAIMS Initiative will have met and exceeded Stead's vision for an area IAIMS and will have laid the foundation for the third generation of this enduring concept.
Footnotes
* This program was supported by NIH Grant no. G08 LM06908 from the National Library of Medicine.
Contributor Information
Julie J. McGowan, Email: jjmcgowa@iupui.edu.
J. Marc Overhage, Email: moverhage@regenstrief.org.
Mike Barnes, Email: mbarnes@regenstrief.org.
Clement J. McDonald, Email: cmcdonald@regenstrief.org.
REFERENCES
- Stead WW. The evolution of IAIMS: lessons for the next decade. J Am Inform Assoc. 1997 Mar–Apr. 4(2 suppl):S4–S9. [PMC free article] [PubMed] [Google Scholar]
- Matheson NW, Cooper JAD. Academic information in the health sciences center: roles for the library in information management. J Med Ed. 1982 Oct. 57(10 pt 2):1–93. [DOI] [PubMed] [Google Scholar]
- Lindberg DA, West RT, and Corn M. IAIMS: an overview from the National Library of Medicine. Bull Med Libr Assoc. 1992 Jul. 80(3):244–6. [PMC free article] [PubMed] [Google Scholar]
- Roderer NK, Clayton PD. IAIMS at Columbia-Presbyterian Medical Center: accomplishments and challenges. Bull Med Libr Assoc. 1992 Jul. 80(3):253–62. [PMC free article] [PubMed] [Google Scholar]
- Broering NC, Bagdoyan HE. The impact of IAIMS at Georgetown: strategies and outcomes. Bull Med Libr Assoc. 1992 Jul. 80(3):263–75. [PMC free article] [PubMed] [Google Scholar]
- Gorry GA. IAIMS development at Baylor College of Medicine. Bull Med Libr Assoc. 1992 Jul. 80(3):247–52. [PMC free article] [PubMed] [Google Scholar]
- Miller PL, Paton JA, Clyman JL, and Powsner SM. Prototyping an institutional IAIMS/UMLS information environment for an academic medical center. Bull Med Libr Assoc. 1992 Jul. 80(3):281–7. [PMC free article] [PubMed] [Google Scholar]
- Ash JS, Hersh WR, Krages KP, Morgan JE, and Schumacher R. The Oregon IAIMS: then and now. Bull Med Libr Assoc. 1999 Jul. 87(3):347–9. [PMC free article] [PubMed] [Google Scholar]
- Fuller SS. Creating the future: IAIMS planning premises at the University of Washington. Bull Med Libr Assoc. 1992 Jul. 80(3):288–93. [PMC free article] [PubMed] [Google Scholar]
- DeGeorges KM, Van Hine P, and Pearse WH. ACOGQUEST: the model phase of the IAIMS project of the American College of Obstetricians and Gynecologists. Bull Med Libr Assoc. 1992 Jul. 80(3):276–80. [PMC free article] [PubMed] [Google Scholar]
- Florance V, Masys D. Next Generation IAIMS: binding knowledge to effective action. Washington, DC: Association of American Medical Colleges, 2002:7. [Google Scholar]
- Stead WW. The evolution of IAIMS: lessons for the next decade. J Am Inform Assoc. 1997 Mar–Apr. 4(2 suppl):S5–S6. [PMC free article] [PubMed] [Google Scholar]
- Overhage JM, Tierney WM, and McDonald CJ. Design and implementation of the Indianapolis Network for Patient Care and Research. Bull Med Libr Assoc. 1995 Jan. 83(1):48–56. [PMC free article] [PubMed] [Google Scholar]
- Overhage JM, Dexter PR, Perkins SM, Cordell WH, McGoff J, McGrath R, and McDonald CJ. A randomized, controlled trial of clinical information shared from another institution. Ann Emerg Med. 2002 Jan. 39(1):14–23. [DOI] [PubMed] [Google Scholar]
- Cimino JJ, Li J, Bakken S., and Patel VL. Theoretical, empirical and practical approaches to resolving the unmet information needs of clinical information system users. Proc AMIA Symp 2002:170–4. [PMC free article] [PubMed] [Google Scholar]
- Baorto DM, Cimino JJ. An “infobutton” for enabling patients to interpret on-line Pap smear reports. Proc AMIA Symp 2000:47–50. [PMC free article] [PubMed] [Google Scholar]