Abstract
This study was designed to estimate the relationship between exposure to tobacco retail outlets and smoking initiation in a racially diverse urban setting. Using data from the 2011 NYC Youth Risk Behavior Survey, multivariable logistic regression analyses were conducted to estimate the exposure–initiation relationship and test for effect modification, while controlling for covariates. The predicted probability of smoking initiation from the multivariable model increased from 7.7 % for zero times a week exposed to tobacco retailers to 16.0 % for exposure seven times or more per week. The odds of initiation were significantly higher among adolescents exposed to tobacco retail outlets two times or more a week compared with those exposed less often (AOR = 1.41; 95 % CI: 1.08, 1.84). Risk-taking behavior modified the relationship between exposure and initiation, with the odds of initiation highest among those low in risk-taking (AOR = 1.78; 95 % CI: 1.14, 1.56). These results are consistent with past research, showing that frequent exposure to tobacco marketing in retail settings is associated with increased odds of initiation. Reducing exposure to tobacco retail marketing could play an important role in curtailing smoking among adolescents, especially those less prone to risk-taking.
Keywords: Adolescent tobacco use, Smoking initiation, Tobacco marketing
Introduction
Following the Master Settlement Agreement in 1998 banning billboard advertisements of tobacco products, tobacco companies shifted a large portion of their promotional resources to point-of-sale (PoS) tobacco marketing.1,2 Retail promotion includes PoS displays and print materials, as well as placement of cigarettes in “friendly familiar” locations behind the cashier, near candy and other staple items.3,4 In 2010, tobacco companies spent an estimate of $477 million promoting tobacco products in the retail environment.5
Research has begun examining the impact of this marketing shift on adolescents' smoking behaviors.6 Weekly or more frequent visits to tobacco retailers have been associated with a 50 % increase in the odds of ever smoking,7,8 and incidence of smoking initiation has been observed to be significantly higher among teens visiting retail outlets at least twice per week.9 Teen smokers are more likely to prefer the brands that are marketed in stores near their schools,7 and exposure to brand promotion in retail outlets has been associated with teens overestimating the prevalence of peer smoking and the social acceptability of smoking.4,7 Furthermore, high tobacco retailer outlet density has been associated with an elevated smoking prevalence at nearby schools,10 higher odds of smoking initiation11 and more positive perceptions of smoking.12 Based on these findings, it has been suggested that the strength of the association between exposure to PoS tobacco marketing and smoking initiation is comparable to exposure to smoking in the home.6
Many previous studies have focused on pre- and young teens (11–14 years old). Smoking uptake typically occurs during the high school years (14–17 years);5 thus, studies of young adolescents may not sufficiently represent the relationship between exposure to PoS tobacco marketing and adolescent smoking behaviors. Much of the research in the US has been conducted in the same small semirural community comprised primarily of whites and Hispanics.7,8,13 Differences in smoking behaviors have been documented between rural and urban youth.14 Furthermore, predictors of smoking experimentation and uptake differ by race/ethnicity.15,16 African-American adolescents typically smoke at lower rates than their white and Hispanic peers.17,18 Thus, including older adolescents and African-Americans within PoS studies is important for accurately estimating the strength of the relationship between exposure and key outcomes.
New York City (NYC) presents an advantageous environment for studying exposure to retail tobacco product promotion and smoking behaviors among adolescents. NYC is one of the most diverse cities in the US, and a high number of NYC tobacco retailers are located near schools and playgrounds, increasing the likelihood of incidental exposure to tobacco products among NYC adolescents as compared to adolescents living in rural or suburban areas.19 We explored the relationship between exposure and key outcomes among a large and diverse sample of NYC public high school students. We modeled the shape of the relationship to test for dose–response effects, and we examined whether race or other respondent characteristics moderated the relationship between exposure and initiation.
Methods
Data Collection and Sample
We used data from the 2011 NYC Youth Risk Behavior Survey (YRBS), a population-based, self-administered survey of NYC public high school students. The YRBS is adapted from the Centers for Disease Control and Prevention's Youth Risk Behavioral Surveillance System and contains modules assessing tobacco, alcohol and drug use, behaviors that contribute to injury, sexual behaviors, mental health, dietary behaviors, and physical activity.
The NYC YRBS uses a stratified two-stage cluster sample to produce a representative sample of public high school students, grades 9 through 12. Post-stratification weights are applied to the data to adjust for nonresponse and represent the gender, race/ethnicity, and grade distributions of the NYC public high school population. A total of 11,570 surveys were completed in 2011, representing a school cooperation rate of 93 % and a student response rate of 79 %.
Measures
Smoking Initiation
Students who indicated they had tried cigarette smoking for the first time in the previous 12 months were classified as initiators.9,15 This measure is based on the definition of initiation used in the National Survey on Drug Use and Health and similar to the definition used in Henriksen et al.9 It includes those who tried cigarettes once (i.e., experimenters), as well as those who continued to smoke regularly. Students who never smoked or who tried smoking more than 12 months ago were classified as non-initiators.
Exposure to Retail Tobacco Marketing
We estimated exposure to retail tobacco marketing by asking students how many times per week they shopped at pharmacies, delis, or bodegas. Bodegas are individually-owned small grocery stores, usually with no more than two registers. They are distinct from convenience stores, in that they offer a wider variety of food items.20 Responses could range from 0 to 7 times or more (M = 2.38; SD = 3.97). Research has documented that the frequency of shopping at store types most likely to sell tobacco products is comparable to the frequency of visiting stores known to sell tobacco.8,9 Licensing data from the New York City Department of Consumer Affairs showed that in 2011, pharmacies, delis, and bodegas represented 75 % of the tobacco retailers in NYC.
Social Influences on Smoking Behaviors
Measures of social norms were included to account for beliefs about prevalence and acceptability of smoking among peers. To measure descriptive norms, respondents were asked, “Out of every ten students in your grade at school, how many do you think smoke?” Response categories ranged from zero students to eight to ten students. The median response of two out of ten students overestimates the actual prevalence of current smoking among NYC public high school students, which is 8.4 %.21 Following previous studies, a dichotomous variable representing overestimation of smoking among peers was created using a median split (1 = overestimated; 0 = not overestimated).22,23 Setting the threshold at 20 % is conservative and allows for variation between schools and within schools between grades. Subjective norms were assessed by asking students to rate whether their friends approve of smoking on a five-point scale ranging from strongly approve to strongly disapprove. Responses were collapsed to create a dichotomous variable representing approval of smoking (1 = approve; 0 = neutral/disapprove). An additional item assessed whether respondents currently live with a smoker.
Risk-taking Behaviors
A variable was created to capture variation in risk-taking, a trait associated with smoking uptake among adolescents.24 Based on previous research,25 ten items associated with risk-taking were screened using principle components analysis: (1) excessive drinking; (2) driving while intoxicated; (3) ever smoking marijuana; (4) ever using cocaine; (5) ever using heroin; (6) ever using methamphetamine; (7) ever using ecstasy; (8) ever using prescription medication recreationally; (9) ever using inhalants; (10) having unprotected sex. These items all loaded on a single factor and were summed to form a unit-weighted composite that ranged from zero to ten (M = .83; SD = 2.84)
Sociodemographic Characteristics
Sociodemographic variables used in the analyses were age, sex, race/ethnicity, and borough of residence. To account for household poverty level, we created a variable based on three items: students were asked if they had seen (1) cockroaches, (2) rats, or (3) mold on the walls and ceilings of their home in the past 30 days. Responses were coded as 1 (yes) or 0 (no), analyzed using principle components and summed to create a unit-weighted composite that ranged from 3 (high poverty) to 0 (low poverty) (M = .74; SD = 1.60).
Statistical Analyses
Bivariate analyses were conducted to identify variables associated with the frequency of exposure to tobacco retailers and variables associated with smoking initiation. Wald χ2 tests were used to identify significant associations (α = .05).
We next conducted a series of multivariable logistic regression analyses to estimate the relationship between exposure to tobacco retailers and smoking initiation while controlling for covariates. Variables associated with either retail exposure or smoking initiation in the bivariate analyses were included in the models and retained if significant at p < .25. Risk-taking and household poverty measures were treated as continuous variables; borough and race were treated as categorical variables; measures of descriptive norms, injunctive norms, and living with a smoker were treated as dichotomous variables. The first model estimated included linear and quadratic terms for retail exposure to test for dose–response and curvilinear effects. Based on the results of this analysis, the second model was estimated with a dichotomous exposure variable, which was created using a median split (two times or more vs. one or no times per week). Interaction tests were next conducted using the dichotomous exposure variable to assess if race or any other covariates moderated the exposure–initiation relationship. Significant interactions were followed up by calculating the conditional odds ratio for the relationship between exposure and initiation at select levels of the moderator variable.26
All analyses were performed using the survey procedures in SAS v.9.2 (SAS Institute Inc., Cary, NC) to account for the complex survey design of the YRBS. School-level clustering is accounted for in all analyses using the cluster statement. The final sample was limited to underage students (17 years or younger) who provided a response to the retail exposure item (N = 8,633).
Results
Bivariate Analyses
Sample characteristics and bivariate associations with exposures to tobacco retailers are displayed in Table 1. The dichotomous exposure variable (two times or more vs. one or no times per week) was used for ease of presentation. Race/ethnicity, borough of residence, overestimating smoking among peers, living with a smoker, risk-taking, and household poverty were all associated with more frequent exposure to tobacco retail outlets.
Table 1.
Characteristics of NYC public high school students and associations with exposure to tobacco retailers
| Infrequent exposure | Frequent exposure | p-value | |||||
|---|---|---|---|---|---|---|---|
| (<2 times/week) | (≥2 times/week) | ||||||
| N | % | 95 % CI | N | % | 95 % CI | ||
| Sample Distribution (row %) | 3,835 | 48.1 | (46.3, 49.9) | 4,798 | 50.1 | (50.1, 53.7) | – |
| Age | 0.27 | ||||||
| < = 14 years old | 1,006 | 27.7 | (22.6, 32.7) | 1,137 | 25.3 | (21.6, 28.9) | |
| 15 years old | 1027 | 28.0 | (22.6, 33.4) | 1,213 | 26.0 | (20.4, 31.7) | |
| 16 years old | 974 | 23.8 | (21.3, 26.3) | 1,322 | 26.2 | (22.7, 29.7) | |
| 17 years old | 828 | 20.6 | (17.5, 23.7) | 1,126 | 22.6 | (17.9, 27.2) | |
| Sex | 0.87 | ||||||
| Female | 2,148 | 53.1 | (48.3, 57.9) | 2,690 | 52.8 | (48.9, 56.7) | |
| Male | 1,673 | 46.9 | (42.1, 51.7) | 2,095 | 47.2 | (43.3, 51.1) | |
| Race | <.0001 | ||||||
| White | 565 | 16.8 | (13.5, 20.0) | 570 | 16.7 | (12.1, 21.3) | |
| African-American | 929 | 31.1 | (23.3, 38.9) | 1,109 | 29.3 | (23.5, 35.2) | |
| Hispanic | 1,310 | 26.3 | (22.4, 30.2) | 2,428 | 42.1 | (37.7, 46.3) | |
| Asians | 609 | 24.9 | (19.7, 30.2) | 278 | 10.9 | (8.0, 13.9) | |
| Others | 228 | 0.9 | (.8, 1.1) | 247 | 0.9 | (.7, 1.1) | |
| Borough | <.0001 | ||||||
| Bronx | 713 | 14.6 | (11.7, 17.4) | 1,232 | 20.4 | (17.0, 23.7) | |
| Brooklyn | 950 | 31.9 | (26.6, 37.1) | 997 | 26.9 | (21.1, 32.8) | |
| Manhattan | 626 | 15.4 | (12.3, 18.6) | 1,318 | 24.6 | (19.0, 30.3) | |
| Queens | 766 | 29.7 | (24.7, 34.8) | 630 | 21.5 | (17.6, 25.5) | |
| Staten Island | 780 | 8.4 | (7.2, 9.6) | 621 | 6.6 | (5.5, 7.6) | |
| Friends approve of smoking (subjective norm) | 589 | 15.0 | (12.7, 17.4) | 739 | 15.3 | (13.2, 17.4) | 0.83 |
| Overestimate smoking among peers (descriptive norm) | 2,444 | 64.6 | (60.4, 68.8) | 3,331 | 73.0 | (70.0, 76.0) | <.0001 |
| Lives with a smoker | 1,161 | 30.9 | (28.7, 33.1) | 1,598 | 34.6 | (32.0, 37.2) | 0.031 |
| Risk-taking (1+ behaviors) | 1,267 | 31.6 | (28.9, 34.4) | 2,397 | 50.0 | (47.3, 52.7) | <.0001 |
| Household poverty level (high) | 151 | 3.9 | (3.2, 4.7) | 227 | 5.0 | (3.8, 6.1) | 0.004 |
Data from the New York City 2011 YRBS. Analyses limited to respondents 17 years old and younger. Frequent exposure = visiting retailers 2 days or more a week; infrequent exposures = visiting retailers 1 or 0 days per week
The overall prevalence of smoking initiation among students was 11.9 %. Table 2 presents the prevalence and odds ratios for smoking for the first time in the past year as a function of respondent characteristics. The odds of initiation increased with the number of times visiting retailers up to four times a week and plateaued between five and seven times per week. Perceived pro-smoking norms, living with a smoker, risk-taking, and high household poverty were also associated with higher odds of smoking initiation. Compared to White students, the odds of smoking initiation were lower among Black and Asian students.
Table 2.
Prevalence and odds ratios for smoking initiation among NYC public HS students as a function of retail exposure, social influences, and sociodemographic characteristics
| N | % | 95 % CI | OR [95 % CI] | |
|---|---|---|---|---|
| Smoking initiation prevalence overall | 998 | 11.9 | (10.7, 13.1) | – |
| Exposure to tobacco retailers* | ||||
| 0 times per week | 237 | 8.8 | (7.3, 10.3) | ref. |
| 1 times per week | 119 | 10.0 | (7.5, 12.4) | 1.1 [.8–1.6] |
| 2 times per week | 119 | 12.1 | (9.5, 14.7) | 1.4 [1.1–1.8] |
| 3 times per week | 131 | 13.6 | (10.5, 16.7) | 1.6 [1.3–2.1] |
| 4 times per week | 91 | 16.1 | (12.1, 20.1) | 2.0 [1.5–2.7] |
| 5 times per week | 90 | 15.1 | (10.3, 19.8) | 1.8 [1.3–2.5] |
| 6 times per week | 47 | 17.7 | (10.3, 25.0) | 2.2 [1.3–3.9] |
| 7 times or more per week | 164 | 15.4 | (12.7, 18.0) | 1.9 [1.4–2.5] |
| Age | ||||
| <= 14 years old | 216 | 11.2 | (8.4, 14.0) | ref. |
| 15 years old | 254 | 10.7 | (8.4, 12.9) | 0.9 [0.7–1.3] |
| 16 years old | 301 | 13.8 | (11.6, 15.9) | 1.3 [0.9–1.7] |
| 17 years old | 227 | 12.2 | (9.8, 14.7) | 1.1 [0.7–1.7] |
| Sex | ||||
| Female | 548 | 11.4 | (9.7, 13.1) | ref. |
| Male | 439 | 12.2 | (10.5, 13.9) | 1.1 [0.9–1.4] |
| Race/Ethnicity*** | ||||
| White | 160 | 15.1 | (11.8, 18.4) | ref. |
| Black | 175 | 9.2 | (7.4, 11.0) | 0.6 [0.4–0.7] |
| Hispanic | 481 | 14.4 | (12.6, 16.2) | 0.9 [0.7–1.3] |
| Asian | 75 | 8.0 | (6.1, 9.8) | 0.5 [0.3–0.7] |
| Others | 58 | 14.6 | (9.1, 20.2) | 1.0 [0.6–1.5] |
| Borough | ||||
| Bronx | 206 | 10.8 | (9.4, 12.2) | 0.8 [0.6–1.0] |
| Brooklyn | 214 | 12.2 | (9.0, 15.3) | 0.9 [0.6–1.3] |
| Manhattan | 238 | 12.6 | (10.2, 15.1) | 1.0 [0.7–1.3] |
| Queens | 162 | 11.5 | (9.6, 13.4) | 0.9 [0.7–1.1] |
| Staten Island | 178 | 13.1 | (10.7, 15.5) | ref. |
| Subjective norms*** | ||||
| Friends approve of smoking | 256 | 19.4 | (15.9, 22.9) | 2.1 [ 1.6–2.6] |
| Friends neutral/disapprove of smoking | 705 | 10.4 | (9.3, 11.5) | ref. |
| Descriptive norms*** | ||||
| Overestimate peer smoking | 787 | 13.9 | (12.5, 15.3) | 2.0 [ 1.6–2.6] |
| Do not overestimate peer smoking | 199 | 7.3 | (6.0, 8.7) | ref. |
| Lives with a smoker*** | ||||
| Yes | 393 | 14.8 | (12.5, 17.1) | 1.6 [1.3–2.0] |
| No | 550 | 9.8 | (8.8, 10.9) | ref. |
| Risk-taking*** | ||||
| 1 or more behaviors | 780 | 21.5 | (19.9, 23.1) | 4.9 [3.9–6.2] |
| none | 218 | 5.2 | (4.1, 6.5) | ref. |
| Household poverty level*** | ||||
| High | 70 | 21.9 | (17.0, 26.7) | 2.2 [1.6–3.1] |
| middle and low | 879 | 11.1 | (9.9, 12.4) | ref. |
Data from New York City 2011 YRBS. Analyses limited to respondents 17 years old and younger. †p < .10
*p = <.05; **p = <.01; ***p = <.001
Logistic Regression Models
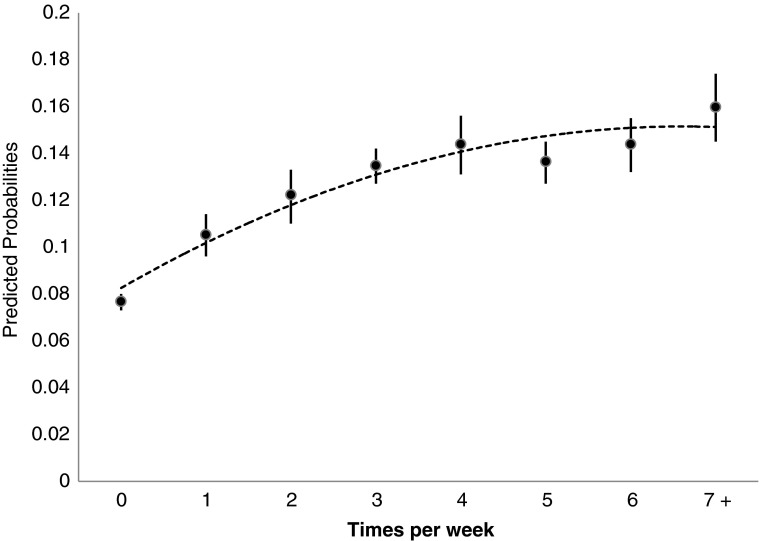
Results for the three regression models are presented in Table 3. Model 1 revealed significant linear and quadratic trends in the smoking initiation–retail exposure relationship. The predicted probabilities of initiation (Fig. 1) show that the prevalence of initiation increases up to about four times per week and then decelerates between five and seven or more times per week.
Table 3.
Multivariable logistic regression analysis of smoking initiation among NYC public high school students, 2011
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| AOR | 95 % CI | AOR | 95 % CI | AOR | 95 % CI | |
| Exposure to tobacco retail outlets | ||||||
| Linear trend | 1.26** | (1.08, 1.48) | – | – | – | – |
| Quadratic trend | 0.97* | (0.95, .99) | – | – | – | – |
| Dichotomous (2+ days vs. 1 or less) | – | – | 1.41** | (1.08, 1.84) | 1.78*** | (1.31, 2.43) |
| Race | ||||||
| White | ref. | ref. | ref. | |||
| Black | 0.6** | (0.42, .87) | 0.6*** | (0.42, .86) | 0.6*** | (0.41, .86) |
| Hispanic | 0.85 | (0.58, 1.27) | 0.85 | (0.57, 1.26) | 0.85 | (0.58, 1.25) |
| Asian | 0.63* | (0.4, .98) | 0.63* | (0.41, .98) | 0.65* | (0.42, .99) |
| Other | 1.09 | (0.7, 1.67) | 1.08 | (0.7, 1.66) | 1.07 | (0.7, 1.65) |
| Borough | ||||||
| Bronx | 0.96 | (0.69, 1.34) | 0.96 | (0.69, 1.33) | 0.96 | (0.69, 1.34) |
| Brooklyn | 1.2 | (0.85, 1.71) | 1.2 | (0.85, 1.71) | 1.2 | (0.85, 1.69) |
| Manhattan | 1.09 | (0.77, 1.52) | 1.09 | (0.78, 1.52) | 1.09 | (0.78, 1.52) |
| Queens | 1.25 | (.94, 1.65) | 1.25 | (.95, 1.64) | 1.25 | (0.95, 1.65) |
| Staten Island | ref. | ref. | ref. | |||
| Friends approve of smoking | 1.48** | (1.09, 2.02) | 1.47* | (1.08, 2.01) | 1.44* | (1.06, 1.95) |
| Overestimate smoking among peers | 1.72*** | (1.3, 2.26) | 1.72*** | (1.3, 2.27) | 1.73*** | (1.31, 2.27) |
| Living with a smoker | 1.38** | (1.1, 1.75) | 1.37** | (1.09, 1.73) | 1.37** | (1.08, 1.73) |
| Risk-taking | 1.34*** | (1.26, 1.42) | 1.33*** | (1.25, 1.42) | 1.54*** | (1.36, 1.74) |
| Household poverty | 1.12† | (1.0, 1.26) | 1.12† | (1.0, 1.26) | 1.11† | (0.98, 1.26) |
| Exposure (dichotomous)*Risk-takinga | – | – | – | – | 0.81** | (0.72, .93) |
AOR adjusted odds ratio. †p<.10
*p = <.05; **p = <.01; ***p = <.001
aThe value for the interaction term is a ratio of odds ratios
Figure 1.
Predicted probability of smoking initiation as a function of times per week exposed to tobacco retailers, adjusted for covariates.
Given the curvilinear relationship, we reestimated the model using the dichotomous exposure variable (model 2) and tested for effect modification. We found only a significant interaction between retail exposure and risk-taking (model 3). The odds ratio for the exposure–initiation relationship changes by a factor of .81 with each 1 unit increase in risk-taking.26 Among students with no history of risky behaviors (risk-taking = 0), frequent retail exposure was associated with 78 % higher odds of smoking initiation (AOR = 1.78; 95 % CI: 1.31, 2.43); at 1 on the risk-taking scale, frequent retail exposure was associated with 45 % higher odds of smoking initiation (AOR = 1.45; 95 % CI: 1.11, 1.89); at 2 on the risk-taking scale, frequent retail exposure was not significantly associated with higher odds of smoking initiation (AOR = 1.18; 95 % CI: 0.87, 1.60).
Discussion
Visiting tobacco retailers two or more times per week was significantly associated with smoking initiation. The predicted probability of initiating among students visiting retailers seven times or more a week (16 %) was double that of students who never visit retailers (8 %) in a typical week. This relationship was strongest among students who were lowest in risk-taking tendencies—a group that is otherwise at low risk for smoking experimentation and uptake.24 The strength of the association between initiation and frequent exposure overall was comparable to that of the association between initiation and living with a smoker.
These results are consistent with past research, showing that frequent exposure to tobacco marketing in retail settings is associated with smoking experimentation.7,8 Previous research has also found evidence of a curvilinear relationship between retailer exposure and smoking initiation. However, Henriksen et al.,9 who conducted a longitudinal study, found that the risk of smoking initiation accelerated as visits per week increased. This pattern could stem from differences in the way retail exposure was measured and the outcome used. The possible range of exposure was much greater than our study, and the primary outcome was the incidence of smoking initiation, as opposed to odds. Nevertheless, both studies found clear evidence of a graded relationship between frequency of shopping at tobacco retailers and odds of initiation.
Our study has several limitations. The cross-sectional design limits our ability to make causal inferences. As noted above, we did find evidence of a dose–response relationship between exposure and initiation, which is consistent with causation. The measures of risk-taking and household poverty we used have limitations also. Data were not available to incorporate thrill-seeking tendencies into the risk-taking measure, and we were not able to measure household poverty directly. There could be residual confounding as a result. Additionally, the exposure measure did not allow us to disentangle the unique influence of exposure to different store types or distinguish the influence of product display from advertising. Recent experimental work suggests that the display of tobacco products may be more influential than advertising in shaping responses to tobacco retail environments.27 Additional longitudinal research using different measures of exposure that can distinguish the influence of store type would be an important direction for future work. Given the unique characteristics of NYC, studies in municipalities of different sizes and densities would also be useful in order to establish the generalizability of our results.
This study is one of the few to examine exposure to tobacco retailers among a racially-balanced sample of older teens and to estimate effects of exposure within that sample using population-level data. Previous research including diverse urban-based populations has relied on ecological methods that use retailer density as a proxy for exposure (e.g., Novak et al.).11 Although Loomis et al.12 recently found that retailer density was associated with perceived awareness of retail tobacco marketing among NYC adolescents, the generalizability of this study is difficult to determine because perceived awareness may measure a distinct aspect of PoS exposure that is different from frequency of exposure.8 Our results provide evidence that mere exposure to tobacco retail outlets is a significant correlate of smoking initiation in the population. This study is also one of the few to examine moderating variables. The finding that exposure is most strongly related to initiation among teens least prone to engage in risky behaviors is novel and points to the potency of retail tobacco marketing among youth. Future research using other measures of risk-taking is needed to confirm the reliability of this finding.
Several countries have recently banned PoS display of tobacco products based on accumulating evidence of the risks associated with exposure to retail tobacco marketing.23,28–30 Evaluations of these restrictions provide evidence for the potential benefits of keeping PoS displays out of sight. For example, following a ban on PoS display in Ireland in 2009, the number of youths overestimating how many of their peers smoke regularly declined by nearly 30 %. In New Zealand, after the implementation of a PoS display ban in 2003, youth smoking declined significantly between 2003 and 2008.29 Researchers studying compliance have suggested that the display ban could produce even larger decreases in youth smoking with better enforcement.30
Although much progress has been made both nationally and in NYC, smoking persists at significant levels among teens. Implementation and enforcement of polices that reduce the impact of tobacco product promotion in retail settings could play an important role in efforts to curtail smoking among this vulnerable population.
Acknowledgments
The authors certify that there are no conflicts of interest to disclose.
References
- 1.Chung PJ, Garfiled CF, Rathouz PJ, Lauderdale DS, Best D, Lantos J. Youth targeting by tobacco manufacturer since the Master Settlement Agreement. Health Aff (Millwood) 2002;21(2):254–263. doi: 10.1377/hlthaff.21.2.254. [DOI] [PubMed] [Google Scholar]
- 2.Wakefield MA, Terry-McElrath YM, Chaloupka FJ, et al. Tobacco industry marketing at point of purchase after the 1998 MSA billboard advertising ban. Am J Public Health. 2002;92(6):937–940. doi: 10.2105/AJPH.92.6.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dewhirst T. POP goes the power wall? Taking aim at tobacco promotional strategies utilized at retail. Tob Control. 2004;13:209–210. doi: 10.1136/tc.2004.009043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paynter J, Edwards R, Schluter PJ, McDuff I. Point of sale tobacco displays and smoking among 14–15 year olds in New Zealand: a cross-sectional study. Tob Control. 2009;18:268–274. doi: 10.1136/tc.2008.027482. [DOI] [PubMed] [Google Scholar]
- 5.Federal Trade Commission. Cigarette Report for 2009 and 2010. Washington, D.C.: Federal Trade Commission, 2012. http://www.ftc.gov/os/2012/09/120921cigarettereport.pdf. Accessed April 25, 2013
- 6.Paynter J, Edwards R. The impact of tobacco promotion at the point of sale: a systematic review. Nicotine Tob Res. 2009; 11(1): 25–35. doi:10.1093/ntr/ntn002. Epub 2009 Jan 27. [DOI] [PubMed]
- 7.Henriksen L, Feighery EC, Wang Y, Fortmann SP. Association of retail tobacco marketing with adolescent smoking. Am J of Pub Health. 2004;94(12):2081–2083. doi: 10.2105/AJPH.94.12.2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feighery EC, Henriksen L, Wang Y, Schleicher NC, Fortmann SP. An evaluation of four measures of adolescents' exposure to cigarette marketing in stores. Nicotine Tob Res. 2006;8(6):751–759. doi: 10.1080/14622200601004125. [DOI] [PubMed] [Google Scholar]
- 9.Henriksen L, Schleischer NC, Feighery EC, Fortmann SP. A longitudinal study of exposure to retail cigarette advertising and smoking initiation. Pediatrics. 2010;126(2):232–238. doi: 10.1542/peds.2009-3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henriksen L, Feighery EC, Schleicher NC, Cowling DW, Kline RS, Fortmann SP. Is adolescent smoking related to the density and proximity of tobacco outlets and retail cigarette advertising near schools? Prev Medicine. 2008;47:210–214. doi: 10.1016/j.ypmed.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Novak SP, Reardon SF, Raudenbusch SD, Buka SL. Retail tobacco outlet density and youth cigarette smoking: a propensity modeling approach. Am J Public Health. 2006;96(4):670–676. doi: 10.2105/AJPH.2004.061622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loomis BR, Kim AE, Busey AH, Farrelly MC, Willett JG, Juster HR. The density of tobacco retailers and its association with attitudes toward smoking, exposure to point-of-sale tobacco advertising, cigarette purchasing, and smoking among New York youth. Prev Med. 2012;55(5):468–474. doi: 10.1016/j.ypmed.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 13.Henriksen L, Feighery EC. Reaching youth at point of sale: cigarette marketing is more prevalent in stores, where adolescents shop more frequently. Tob Control. 2004;13:315–318. doi: 10.1136/tc.2003.006577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarvela PD, Cronk CE, Isberner FR. A secondary analysis of smoking among rural and urban youth using the MTF data set. J Sch Health. 1997;67(9):372–374. doi: 10.1111/j.1746-1561.1997.tb07178.x. [DOI] [PubMed] [Google Scholar]
- 15.Griesler PC, Kandel DB, Davies M. Ethnic differences in predictors of initiation and persistence of adolescent cigarette smoking in the National Longitudinal Survey of Youth. Nicotine Tob Res. 2002;4:79–93. doi: 10.1080/14622200110103197. [DOI] [PubMed] [Google Scholar]
- 16.Gritz ER, Prokhorov AV, Hudmon KS, et al. Predictors of susceptibility to smoking and ever smoking: a longitudinal study in a tri-ethnic sample of adolescents. Nicotine Tob Res. 2003;5(4):493–506. doi: 10.1080/1462220031000118568. [DOI] [PubMed] [Google Scholar]
- 17.Anderson C, Burns DM. Patterns of adolescent smoking initiation rates by ethnicity and sex. Tob Control. 2000;9(Suppl 2):ii4–ii8. doi: 10.1136/tc.9.suppl_2.ii4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ordein T, Foulds J. Causes of the decline in cigarette smoking among African-American youths from 1970s to the 1990s. Am J Public Health. 2011;101(10):e4–e14. doi: 10.2105/AJPH.2011.300289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luke DA, Ribisl KM, Smith C, Sorg AA. Family smoking prevention and tobacco control act: banning outdoor tobacco advertising near schools and playgrounds. Am J Prev Med. 2011;40(3):295–302. doi: 10.1016/j.amepre.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 20.North American Industry Classification System. North American Industry Classification System Code Search. http://www.census.gov/eos/www/naics/index.html. Accessed April 29, 2013
- 21.New York City Department of Health and Mental Hygiene. Epiquery: NYC Interactive Health Data System—Youth Risk Behavior Survey 2011. http://nyc.gov/health/epiquery. Accessed April 29, 2013
- 22.Spanopolous D, Britton J, McNeill A, Ratschen E, Szatkowski L. Tobacco display and brand communication at the point of sale: implications for adolescent smoking behavior. Tob Control. Published online first: 28 February 2013 doi:10.1136/tobaccocontrol-2012-050765B [DOI] [PMC free article] [PubMed]
- 23.McNeill A, Lewis S, Quinn C, et al. Evaluation of the removal of point-of-sale tobacco displays in Ireland. Tob Control. 2011;20(2):137–143. doi: 10.1136/tc.2010.038141. [DOI] [PubMed] [Google Scholar]
- 24.Burt RD, Dinh KT, Peterson AV, Saranson IG. Predicting adolescent smoking: a prospective study of personality variables. Prev Med. 2000;30:115–125. doi: 10.1006/pmed.1999.0605. [DOI] [PubMed] [Google Scholar]
- 25.Gullone E, Moore S, Moss S, Boyd C. The adolescent risk-taking questionnaire: development and psychometric evaluation. J of Adol Research. 2000;15(2):231–250. doi: 10.1177/0743558400152003. [DOI] [Google Scholar]
- 26.Jaccard J. Interaction Effects in Logistic Regression. Newbury Park: Sage; 2001. [Google Scholar]
- 27.Kim AE, Nonnemaker, JM, Loomis, BR, et al., 2012. Influence of tobacco displays and ads on youth: a virtual store experiment. Pediatrics. 2013;131(1):1–8. doi:10.1542/peds.2012-0197. Epub 2012 Dec 3. [DOI] [PubMed]
- 28.Scheffels J, Lavik R. Out of sight, out of mind? Removal of point-of-sale tobacco displays in Norway. Tob Control. Epub 2012 Jun 7. doi:10.1136/tobaccocontrol-2011-050341 [DOI] [PMC free article] [PubMed]
- 29.Paynter J. National Year 10 ASH Snapshot Survey, 1999–2008: Trends in tobacco use by students aged 14–15 years. Report for the Ministry of Health, Health Sponsorship Council and Action on Smoking and Health. Auckland, New Zealand 2009.
- 30.Quedley M, Ng B, Sapre N, et al. In sight, in mind: retailer compliance with legislation on limiting retail tobacco displays. Nicotine Tob Res. 2008;10(8):1347–1354. doi: 10.1080/14622200802238860. [DOI] [PubMed] [Google Scholar]