Abstract
Urban slum dwellers are not only prone to develop communicable diseases but also to non-communicable disease (NCDs). The extent and magnitude of NCDs among slum dwellers is largely unknown in Nigeria. A total of 964 adults aged 20–81 years (male 330 and female 634) residing in the urban slum of Ajegunle in Lagos State, Nigeria were studied to determine the prevalence of hypertension and associated factors. The overall prevalence of hypertension was 38.2 %. Of the 368 respondents identified as having hypertension, only 50 (5.2 %) respondents were previously aware of their diagnosis. Of the 50 known hypertensive patients, 48(96 %) had poor control of their high blood pressure. The socio-demographic factors significantly associated with hypertension status were age, sex, education, religion, BMI, and marital status. The study concludes a high prevalence of hypertension among urban slums dwellers in Lagos. The need for government to develop policies for the control of hypertension, improve access to early diagnosis and provide an enabling socioeconomic environment while promoting healthy living.
Keywords: Hypertension, Prevalence, Slum, Urban poor, Nigeria
Introduction
The United Nations expert group in 2002 defined slum as “human settlement that has inadequate access to safe water, inadequate access to sanitation and other infrastructure, poor structural quality of housing, overcrowding, and insecure residential status”.1 About one billion people of the world population are estimated to be living in slum or squatter settlement.2 The explosive population growth in cities was due in part to increased industrial activities which created job opportunities for both skilled and unskilled workers and resulted in the migration of people from rural to urban areas in search of employment opportunities and a better life.3
The increase in the population of urban cities led to overstretching of the limited infrastructural facilities available in the cities due to the inability of governments to provide affordable housing and poor urban planning.4 This has led the low income segment of the population to live in crowded slum with poor sanitary conditions.5
It has been reported that in many developing countries there is an epidemiological transition from communicable to non-communicable diseases (NCDs). NCDs contributed 60.3 % of the total deaths worldwide in 2005.6 Three quarters of these deaths were in low- and middle-income countries. It is estimated that NCDs will contribute 60 % of the world’s disease burden, and contribute 53 % of total deaths by 2020.7
Urban slum dwellers are exposed not only to communicable diseases as a result of poor living condition but also to non-communicable diseases such as hypertension.8 They are equally exposed to unhealthy lifestyle factors such as potentially harmful diets, physical inactivity, obesity, alcohol and tobacco use as a result of the high unemployment rates and poverty, in addition to the limited access to essential health services.9 However, the prevalence, magnitude and risk factors of NCDs in slums are not known.
Hypertension is one of the major public health challenges in both developed and developing countries and constitutes a major risk factor for cardiovascular disease. The World Health Organization estimates a prevalence rate of 10–16 % using the cut-off of 160/95 mmHg.10 With the current revised definition of 140/90, this prevalence will be much higher. Earlier studies in Nigeria among adults 15 years and above using the cut-off of 160/95 mmHg, reported a prevalence rate of 11.2 % which ranged from 9.8 % in rural to 14.6 % in urban communities. Using the revised cut-off of 140/90 mmHg, a revised prevalence rate of 17–20 % has been reported.11 In another population-based survey, a prevalence rate of 14.5 % was observed.12 In a meta analysis of studies on prevalence of hypertension in Nigeria, prevalence rates ranges from 12.4 to 34.8 % among adults in Nigeria.13
To the best of our knowledge, no study has been done on the prevalence of hypertension among slum dwellers. Hence, this study was carried out to assess the prevalence of hypertension among slum dwellers in Lagos, Nigeria.
Methodology
According to the National population commission, Lagos state has an estimated population of 9.3 million at the 2006 population census. The study was carried out in one of the urban slum area in Ajegunle/Ifelodun Local Government Area of the State. The study subjects were adults aged 20 years and above residing in the area.
The study area was selected by random sampling. A list of all the Enumeration areas (EA) constituting the Local Government Area was received from the National Population Commission. By simple random sampling one EA was chosen. The study population consisted of the first EA and the adjoining EA until the sample size was attained. The study was conducted on a house to house basis. In each building, the total number of households was identified. Both verbal and written consent were obtained from each respondent. Information was collected from the respondents using a pre-tested questionnaire.
The diagnosis of hypertension was based on systolic blood pressure (BP) ≥ 40 mmHg or a diastolic blood pressure of ≥90 mmHg or both, and/or concomitant use of antihypertensive medications according to the WHO/ISH guidelines.14 The respondents were allowed to rest for at least 10 min before a resting blood pressure was taken using an appropriate cuff size electronic sphygmomanometer. Three readings were carried out while the mean was taken as the reading for each individual.
Body weight was measured with respondents bare footed, with no caps nor head gear. Body weight was measured in kilograms to the nearest 0.1 kg and the corresponding height of the respondents was measured in centimeter and later converted to meter. The body mass index (BMI) was calculated using weight in kilogram divided by the square of the height in meter. The BMI was classified using the WHO classification.15 BMI <18.5 kg/m2 was regarded as underweight, BMI 18.5–24.5 kg/m2 as normal, BMI 25–29.5 kg/m2 as overweight and BMI >30 kg/m2 was classified as obesity.
Data was analyzed using standard statistical procedures including the use of IBM SPSS version 15 statistical soft ware. We used chi-square test to evaluate differences in categorical variables. Fisher’s exact test was used when cell size were less than 5. The Student’s t test was used to compare continuous variables. Differences between data were considered significant where P < 0.05 or odds ratio (O.R) did not embrace unity.
Results
Overall, 964 respondents participated in this study. The males were 330 (34.2 %) while the females were 634 (65.8 %) giving a male/female ratio of 1:1.92.
The mean age of respondents was 38.41 ± 12.9 years (ranging from 20 to 81 years). The mean age in male was 40.27 ± 13.8, while that of female 37.50 ± 12.3. Majority of the respondents (30.1 %) were in the age group 20–29 years, followed closely by the age group 30–39 years (28.6 %). About half of the population (46.3 %) had secondary (both junior and senior) education while only 21.8 % had post secondary education. Majority were married (76.8 %), Christians (70.8 %), and self employed as traders (40.5 %) and artisans (26.8 %). The mean BMI among the study population was 25.32 ± 4.7 kg/m2. It ranged from a minimum of 14.34 kg/m2 to a maximum of 42.6 kg/m2. About half of the respondents (49.7 %) were of normal weight with BMI between 18.5–24.9 kg/m2, 29.7 % were overweight with BMI of 25–29.9 kg/m2 and 16.4 % were obese with BM1 ≥30 kg/m2. Only 4.6 % of respondents were underweight with BMI less than 18.5 kg/m2 as shown in Table 1.
Table 1.
Socio-demographic characteristics of respondents by gender
| Characteristics | Male N = 330 (%) | Female N = 634(%) | Total N = 964 (%) |
|---|---|---|---|
| Age | |||
| 20–29 | 88(26.7) | 202(31.9) | 290(30.1) |
| 30–39 | 78(23.6) | 198(31.2) | 276(28.6) |
| 40–49 | 86(26.1) | 132(20.8) | 218(22.6) |
| 50–59 | 36(10.9) | 62(9.8) | 98(10.2) |
| 60–69 | 38(11.5) | 26(4.1) | 64(6.6) |
| ≥70 | 4(1.2) | 14(2.1) | 18(1.9) |
| Educational status | |||
| No formal education | 24(8.3) | 56(8.9) | 80(8.2) |
| Primary | 80(24.2) | 148(23.3) | 228(23.7) |
| Junior secondary | 30(9.1) | 66(10.4) | 96(10) |
| Senior secondary | 118(35.8) | 232(36.6) | 350(36.3) |
| Post secondary | 78(23.6) | 132(20.8) | 210(21.8) |
| Religion | |||
| Christianity | 236(71.5) | 446(70.3) | 682(70.8) |
| Islam | 94(28.5) | 182(28.7) | 276(28.6) |
| Others | 0(0) | 6(0.9) | 6(0.6) |
| Marital status | |||
| Single | 86(26.1) | 92(14.5) | 178(18.5) |
| Married | 240(72.7) | 500(78.9) | 740(76.8) |
| Separated | 2(0.6) | 8(1.3) | 10(1.0) |
| Widowed | 2(0.6) | 34(5.4) | 36(3.7) |
| BMI | |||
| Underweight | 22(6.7) | 22(3.5) | 44(4.6) |
| Normal weight | 212(64.2) | 264(41.6) | 476(49.7) |
| Overweight | 80(24.2) | 206(32.5) | 286(29.7) |
| Obese | 16(4.8) | 142(22.4) | 158(16.4) |
| Ever smoked | |||
| Yes | 59 (17.8) | 2 (0.3) | 61(6.3) |
| No | 271 (82.2) | 632(99.7) | 901(93.7) |
| Occupation | |||
| Traders/business | 46(14) | 344(54.3) | 390(40.5) |
| Artisans | 152(46.1) | 106(16.7) | 258(26.8) |
| Students | 16(4.8) | 58(9.1) | 74(7.7) |
| Admin worker (e.g. clerks ) | 18(5.5) | 48(7.6) | 66(6.8) |
| Transport worker | 28(8.5) | 2(0.3) | 30(3.1) |
| Housewife/house husband | 8(2.4) | 42(6.6) | 50(5.2) |
| Farmer | 6(1.8) | 6(0.9) | 12(1.2) |
| Health care worker (nurses, auxiliary health staff) | 0(0) | 10(1.6) | 10(1.0) |
| Construction workers | 20(6.1) | 0(0) | 20(2.1) |
| Others (retired, clergy, etc.) | 36(10.9) | 18(2.8) | 54(5.6) |
The overall prevalence of hypertension in this study was 38.2 % (368/964). The prevalence of systolic hypertension was 37.1 % (358/964) while the prevalence of diastolic hypertension was 14.5 % (140/964). The mean systolic blood pressure was 136.96 ± 25.2 mmHg and it ranged from 93 mmHg to 271 mmHg. The mean diastolic blood pressure was 75.94 ± 14.42 mmHg and ranged from 39 mmHg to 165 mmHg. The proportion of males with systolic hypertension was higher compared to females (43.6 % v 33.8 %; p = 0.003). A slightly higher proportion of females had diastolic hypertension compared to males but this was not statistically significant (15.1 % v 13.3 %; p = 0.5).
Of the 368 respondents identified as having hypertension in this study, only 50 (5.2 %) respondents were previously aware of their diagnosis. Of the 50 known hypertensive patients, 48 (96 %) had poor control of their blood pressure. Of the 368 respondents diagnosed with hypertension, 318 (94.8 %) were not previously aware of their diagnosis.
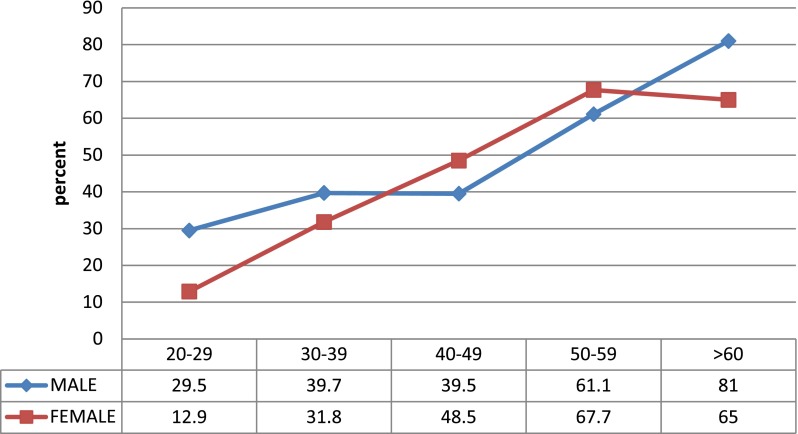
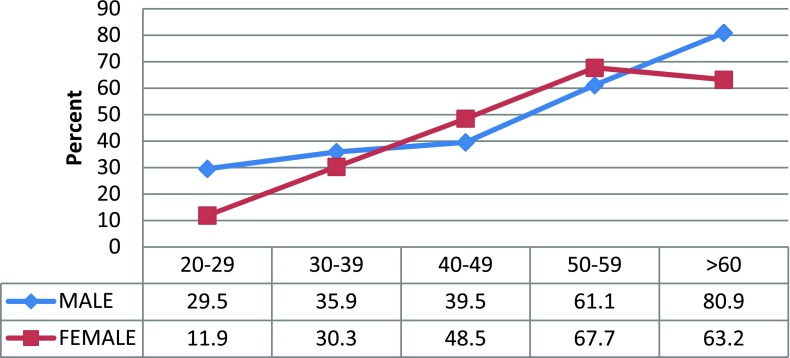
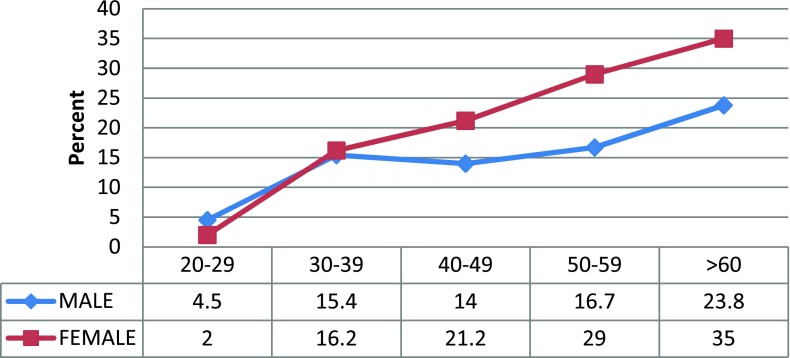
The prevalence of hypertension was found to increase steadily with age. The proportion of individuals with hypertension within each age group was found to steadily increase. The age-specific prevalence rate in males rose from 13 % in the age group 20–29 year to 80 % in the age group >60 years. In the female population however, there was a steady rise until the age 50–59 year followed by a slight decline in the age group >60 years as shown in Fig. 1. The age-specific prevalence of systolic hypertension is shown in Fig. 2. There was a steady rise with increasing age. There was also a higher prevalence of systolic blood pressure among females in the age group 40–59 years old. A similar observation was noted for the diastolic blood pressure though, from the age 30–39 years old group and above as shown in Fig. 3.
Figure 1.
Age -specific prevalence of hypertension by gender.
Figure 2.
Age-specific prevalence of systolic hypertension by gender.
Figure 3.
Age-specific prevalence diastolic pressure by gender.
The socio-demographic factors were assessed with hypertension status. In bivariate analysis, sex, education, religion, marital status, BMI and age were significantly associated with hypertension as shown in Table 2. However, in multivariate analysis, only age, BMI and sex showed significant relationship to hypertension as shown in Table 3. The logistic regression analysis of hypertension and some socio-demographic variables is shown in Table 4. It was shown that sex was the most predictive factor of hypertension followed by BMI and age.
Table 2.
Distribution of the mean systolic and diastolic pressure by age and gender
| Age group (years) | Total | Male | Females | |||
|---|---|---|---|---|---|---|
| Mean sys BP ± S.D (mmHg) | Mean dia BP ± S.D (mmHg) | Mean sys BP ± S.D (mmHg) | Mean dia BP ± S.D (mmHg) | Mean sys BP ± S.D (mmHg) | Mean dia BP ± S.D (mmHg) | |
| 20–29 | 127.01 ± 13.6 | 69.88 ± 9.8 | 132.48 ± 14.58 | 67.89 ± 11.02 | 124.62 ± 12.44 | 70.75 ± 7.25 |
| 30–39 | 132.70 ± 22.8 | 75.57 ± 13.7 | 135.85 ± 18.48 | 74.26 ± 12.17 | 131.46 ± 24.27 | 76.08 ± 14.56 |
| 40–49 | 141.53 ± 27.60 | 80.19 ± 18.10 | 138.74 ± 24.91 | 77.81 ± 17.6 | 143.35 ± 29.17 | 81.74 ± 18.31 |
| 50–59 | 152.65 ± 33.16 | 80.80 ± 11.32 | 151.11 ± 37.61 | 79.11 ± 10.82 | 153.55 ± 30.57 | 81.77 ± 11.57 |
| >60 | 155.63 ± 25.12 | 81.49 ± 13.87 | 157.38 ± 19.13 | 80.43 ± 12.39 | 153.80 ± 30.32 | 82.60 ± 15.35 |
Table 3.
Factors associated with hypertension among respondents
| Factors | Hypertensive N = 368 | Non hypertensive N = 596 | Chi square | P value |
|---|---|---|---|---|
| Age | ||||
| <40 | 146 | 420 | 87.7 | 0.0001 |
| >40 | 222 | 176 | ||
| BMI | ||||
| Underweight <18.5 kg/m2 | 8 | 36 | 30.7 | 0.0001 |
| Normal weight 18.5–24.9 kg/m2 | 154 | 322 | ||
| Overweight 25–29.9 kg/m2 | 124 | 162 | ||
| Obese >30 kg/m2 | 82 | 76 | ||
| Sex | ||||
| Male | 147 | 183 | 8.630 | 0.004 |
| Female | 221 | 413 | ||
| Education | ||||
| No formal education | 66 | 24 | 39.40 | 0.0001 |
| Primary | 86 | 142 | ||
| Secondary education | 160 | 288 | ||
| Post secondary | 66 | 144 | ||
| Religion | ||||
| Christianity | 268 | 414 | 0.78 | 0.378 |
| Islam | 100 | 176 | ||
| Marital | ||||
| Single | 37 | 141 | 44.06 | 0.0001 |
| Married | 299 | 441 | ||
| Separated | 6 | 4 | ||
| Widowed | 26 | 10 | ||
Table 4.
Logistic regression analysis of hypertension and some variables
| B | Std Error. | Sig. | Exp(B) | 95 % C.I. for EXP(B) | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Sex | 0.592 | 0.169 | 0.000 | 1.808 | 1.299 | 2.517 |
| Age | 0.051 | 0.007 | 0.000 | 1.052 | 1.037 | 1.068 |
| Education | −0.197 | 0.059 | 0.001 | 0.821 | 0.732 | 0.921 |
| Religion | −0.439 | 0.140 | 0.002 | 0.645 | 0.490 | 0.849 |
| Marital Status | −0.048 | 0.129 | 0.709 | 0.953 | 0.740 | 1.227 |
| BMI | 0.105 | 0.017 | 0.000 | 1.111 | 1.074 | 1.149 |
Discussions
The prevalence of hypertension among slum dwellers in our study was 38.2 %. This was higher than 8.6 %,16 10.7 %,17 15.4 %,8 and 21.4 %,3 respectively, reported in similar studies among slum dwellers in India. However, this observed prevalence was lower than the 69 and 73.3 % observed among elderly women in slum area of India.18,19 The highly selective population with risk factors for hypertension may be responsible for the high prevalence of hypertension in these studies.
Our study also showed a slightly higher prevalence compared with a similar study among urban dwellers in Lagos which reported a prevalence of 34.8 %.20 Studies from other parts of Nigeria showed a much lower prevalence of hypertension.10,12,13 Whether urban slum dwellers have a higher prevalence rate of hypertension needs to be further evaluated by future research.
The high prevalence rate in this study can be comparable to studies in developed countries.12 The adoption of western lifestyle by city dwellers which include lack of physical activity or exercise, increased intake of processed foods, increased salt intake, sedentary jobs and obesity may have contributed to the high prevalence of hypertension in this study as observed by other studies on hypertension.21,22 Some of these lifestyle factors are modifiable and a targeted intervention to reduce the effects of these risk factors will eventually lead to a reduction in the prevalence of hypertension in the community.
The mean systolic blood pressure of 136.96 ± 25.2 mmHg in this study was higher than the 121.5 mmHg that was observed about a decade ago in similar studies in Ghana23 and Nigeria.12 The increase can be attributed to the general increase in the rate of hypertension globally which may be related to the increase in the risk factors for the development of hypertension as a result of increasing urbanization. People living in urban slum bear the greater brunt of the recent global economic recession which poses greater stress and negative effect on their health and well being.
Our study showed that the prevalence of hypertension was higher in males than females. This observation was also reported in other sudies12,23 whereas some other studies actually found a higher prevalence in women.24 However, this study showed that women had consistently higher age-specific prevalence of diastolic hypertension. Further studies will be required to ascertain if gender play a role in the development or severity of hypertension.
Over 90 % of respondents were not aware of their hypertensive state prior to the study. This low awareness has been well described in similar studies.3,8,16,17,23 The low level of education, poverty, ignorance, lack of access to health information and health care services may be responsible for the low awareness. Hypertension is a disease that does not present with obvious signs and symptoms and therefore it is called the “silent killer”. In communities like the slum, affected individuals may not seek medical intervention early and may later present with signs of complications or organ damage. Thus, health education programs should be targeted at the urban slum dwellers to ensure early detection and management.
The study observed that majority of the diagnosed hypertensive patient on treatment had poor control of their blood pressure. Poor adherence to treatment has been identified as the most important cause of uncontrolled blood pressure.24–26 Some reasons for non-adherence to antihypertensive treatment as reported in the literatures include poor socioeconomic status, illiteracy and unemployment27,28 lack of understanding and acceptance of the disease, perception of the health risk, and the cost of treatment. These factors are more prevalent among urban poor than the general population. Strategies for improving access to drugs such as sustainable community health financing and provision of affordable medications will influence patient adherence positively.29 Non-adherence to treatment will ultimately lead to the development of long term complications of the disease, place more economic burden on the slum dwellers that are already disadvantaged economically. It is therefore imperative for the government to provide health care services which is available, accessible and affordable to all categories of people according to the principles of primary health care irrespective of their social strata in the society. This will encourage the people to seek care early and avoid the development of preventable complications.
The socio-demographic risk factors associated with hypertension was age >40 years, male, lower educational status, and higher BMI. The only modifiable risk factor predictive of hypertension in this study was obesity. Obesity could be as a result of increasing westernized diet and sedentary life style. Health interventions which include health education on healthy nutrition and how to use available resources to prepare healthy diet, increase physical exercise, and the improvement of the general living conditions of dwellers in slum environment cannot be overemphasized.
In conclusion, there is a high prevalence of hypertension in urban slums in Lagos. Policy makers should consider strategies to prevent non-communicable diseases in addition to effort by government to address communicable diseases in the country. More attention should be paid to the urban poor who are marginalized and have become a vulnerable group in the society. Targeted health intervention for early diagnosis and appropriate management of hypertension are required to forestall the development of complication from uncontrolled hypertension.
References
- 1.The challenge of slums: global report on human settlements 2003. London: Earthscan; 2003. [Google Scholar]
- 2.UN millennium project—investing in development. A practical plan to achieve the millennium development goals. London: Earthscan; 2005. [Google Scholar]
- 3.Viswanathan V, Tharkar S. Can the divide be bridged: overview of life in urban slums in India? Indian J Comm Med. 2010;35:198–199. doi: 10.4103/0970-0218.62562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giok, Lingooi and Kai Hong Phua. Urbanization and slum formation. Journal of Urban Health. Bulletin of the New York Academy of Medicine vol 84 no1. 2007. [DOI] [PMC free article] [PubMed]
- 5.Riley LW, Ko AI, Unger A, Reis MG. Slum health: diseases of neglected population. BMC Int Health Human rights. 2007;7:2.1–6. doi: 10.1186/1472-698X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strong K, Mathers C, Leeder S, Beaglehole R. Preventing chronic diseases: how many lives can we save? Lancet. 2005;366:1578–82. doi: 10.1016/S0140-6736(05)67341-2. [DOI] [PubMed] [Google Scholar]
- 7.Reddy KS, Shah B, Varghese C, Ramadoss A. Responding to the threat of chronic diseases in India. Lancet. 2005;366:1744–9. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- 8.Anand K, Shah B, Yadav K, Singh R, Mathur P, Paul E, Kapoor SK, Are the urban poor vulnerable to non communicable diseases? A survey of risk factors for non communicable diseases in urban slums of Faribad. Natl med J India 2007 May-June 20 (3) 115–20. [PubMed]
- 9.Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79(12):1139–1147. doi: 10.1097/00001888-200412000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Akinkugbe OO. Hypertension in Non communicable Diseases in Nigeria. Final Report of a national survey Lagos. Federal Ministry of Health and Social services 1997:12–41
- 11.Kadiri S, Walker O, Salako BL, Akinkugbe O. Blood pressure, hypertension and correlates in urbanized workers in Ibadan, Nigeria—a revisit. Journ Hum Hypert. 1999;13:23–27. doi: 10.1038/sj.jhh.1000722. [DOI] [PubMed] [Google Scholar]
- 12.Cooper R, Rotimi C, Ataman S, Mcgee D, Osotimehin B, Kadiri S, et al. The prevalence of hypertension in seven populations of West African origin. Am J Public Health. 1997;87:160–168. doi: 10.2105/AJPH.87.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ekwunife OI, Aguwa CN. A meta analysis of prevalence rate of hypertension in Nigerian populations. J Public Health Epidemiol. 2011;29:604–607. [Google Scholar]
- 14.Whitworth IA. World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21(11):1983–1992. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 15.“Obesity preventing and managing global epidemic”. Report of a WHO consultation on obesity. Geneva Switzerland: WHO /NUT/NCD/98.1; 1997. [PubMed] [Google Scholar]
- 16.Reddy SS, Prabhu GR. Prevalence and risk factors of hypertension in adults in an urban slum Tirupaty. Indian J Community Med. 2005;30:84–86. doi: 10.4103/0970-0218.42855. [DOI] [Google Scholar]
- 17.Patnaik L, Sahani NC, Sahu T, Sethi S.Astudy on hypertension in urban slum of Brahmapour, Orissa. Indian association of preventive and social medicine Orissa chapter accessed at http://www.jcmorisa.org/index_files/page682.htm on 17 july 2012
- 18.Hypertension study group Prevalence, awareness, treatment and control of hypertension among elderly in Bangladesh and India; a multi-centric study. Bulletin of the WHO. 2001;79(6):490–500. [PMC free article] [PubMed] [Google Scholar]
- 19.Pawar AB, Bansal RK, Bharodiya P, Panchal S, Patel HB, Padariya PK, Patel GH. Prevalence of hypertension among elderly women in slums of Surat city. Nat J Community Med. 2010;1:39–40. [Google Scholar]
- 20.Nigerian Heart Foundation. Federal Ministry of Health and social services. Health behavior monitor among Nigerian adult population. Available from URL: http://www.who.int/chp/steps/2003_STEPS_report Nigeria.pdf
- 21.Working Group on the Primary Prevention of Hypertension Report of the National High Blood Pressure Education Program Working Group on Primary Prevention of Hypertension. Arch Intern Med. 1993;153:186–208. doi: 10.1001/archinte.1993.00410020042003. [DOI] [PubMed] [Google Scholar]
- 22.Elliot P. Observational studies on salt and blood pressure. Hypertension. 1991;17(suppl 1):13–18. doi: 10.1161/01.hyp.17.1_suppl.i3. [DOI] [PubMed] [Google Scholar]
- 23.Cappuccio FP, Micah FB, Emmett L, Kerry SM, Antwi S, Martin-Peprah R. Prevalence, detection, management and control of hypertension in Ashanti West Africa. Hypertension. 2004;43:1017–1022. doi: 10.1161/01.HYP.0000126176.03319.d8. [DOI] [PubMed] [Google Scholar]
- 24.Amaoah AGB. Hypertension in Ghana: a cross sectional community prevalence study in greater Accra. Ethn Dis. 2003;13:310–315. [PubMed] [Google Scholar]
- 25.Burt VL, Cutler JA, Higgins M, Horan MJ, Larbarthe D, Whelton P, et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension. 1995;25:305–313. doi: 10.1161/01.HYP.25.3.305. [DOI] [PubMed] [Google Scholar]
- 26.Hershey JC, Morton BG, Davis JB, Reichgott MJ. Patient compliance with antihypertensive medication. Am J Public Health. 1980;70:1081–1089. doi: 10.2105/AJPH.70.10.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saounatsou M, Patsi O, Fasoi G, Stylianou M, Kavga A, Economou O, et al. The influence of the hypertensive patient’s education in compliance with their medication. Public Health Nursing. 2001;18:436–442. doi: 10.1046/j.1525-1446.2001.00436.x. [DOI] [PubMed] [Google Scholar]
- 28.Bone LR, Hill MN, Stallings R, et al. Community health survey in an urban African-American neighborhood: distribution and correlates of elevated blood pressure. Ethn Dis. 2000;10:87–95. [PubMed] [Google Scholar]
- 29.Schafheutle EI, Hassell K, Noyce PR, et al. Access to medicines: cost as an influence on the views and behaviour of patients. Health Soc Care Comm. 2002;10:187–195. doi: 10.1046/j.1365-2524.2002.00356.x. [DOI] [PubMed] [Google Scholar]